Abstract
High unpredictability has emerged as a dimension of early-life adversity that may contribute to a host of deleterious consequences later in life. Early-life unpredictability affects development of limbic and reward circuits in both rodents and humans, with a potential to increase sensitivity to stressors and mood symptoms later in life. Here, we examined the extent to which unpredictability during childhood was associated with changes in mood symptoms (anhedonia and general depression) after two adult life stressors, combat deployment and civilian reintegration, which were assessed ten years apart. We also examined how perceived stress and social support mediated and /or moderated links between childhood unpredictability and mood symptoms. To test these hypotheses, we leveraged the Marine Resiliency Study, a prospective longitudinal study of the effects of combat deployment on mental health in Active-Duty Marines and Navy Corpsman. Participants (N = 273) were assessed for depression and anhedonia before (pre-deployment) and 3–6 months after (acute post-deployment) a combat deployment. Additional assessment of depression and childhood unpredictability were collected 10 years post-deployment (chronic post-deployment). Higher childhood unpredictability was associated with higher anhedonia and general depression at both acute and chronic post-deployment timepoints (βs ≥ 0.16, ps ≤.007). The relationship between childhood unpredictability and subsequent depression at acute post-deployment was partially mediated by lower social support (b = 0.07, 95% CI [0.03, 0.15]) while depression at chronic post-deployment was fully mediated by a combination of lower social support (b = 0.14, 95% CI [0.07, 0.23]) and higher perceived stress (b = 0.09, 95% CI [0.05, 0.15]). These findings implicate childhood unpredictability as a potential risk factor for depression in adulthood and suggest that increasing the structure and predictability of childhood routines and developing social support interventions after life stressors could be helpful for preventing adult depression.
Keywords: Depression, Veterans, Anhedonia, Early-life adversity, Deployment, Social support
1. Introduction
There is clear evidence that early-life adversity impacts neurodevelopment and subsequent risk for mood and anxiety disorders (Hughes et al., 2017; Scott et al., 2011). While research into the deleterious effects of early-life adversity has typically focused on the impact of objectively negative and traumatic life events (e.g., child abuse, parental divorce; e.g., Anda et al., 2020; Chapman et al., 2004), a growing body of evidence suggests that high levels early-life unpredictability represents a distinct form of adversity with long-term negative impact on emotion and cognition in adulthood (Baram et al., 2012; Davis et al., 2022). In contrast to other forms of early-life adversity that pertain to the frequency/severity of stressors early in life, early-life unpredictability refers to the extent to which one’s home, caregivers, and environment are predictable (Molet et al., 2016; Glynn & Baram, 2019). For instance, in both rats and humans, unpredictability can be quantified by the rate at which mothers transition between different behavioral patterns and sensory signals (i.e., changes in visual, auditory, and tactile signals) regardless of whether those signals are positive or negative (Davis et al., 2017) as well as predictability of household events and routines (Glynn et al. 2019; Lindert et al. 2022). Unpredictability during development is associated with a number of poor functional outcomes in adulthood including increased anxiety and depression (Spadoni et al., 2022), increased risk for intimate partner violence (Szepsenwol et al., 2019), cognitive dysfunction (Davis et al., 2022), and poorer physical health (Maner et al., 2023). Hence, more research into the mechanisms underlying the negative impacts of early-life unpredictability is necessary to better understand how such impacts come about and can be prevented.
In rodents, fragmented and unpredictable maternal care is linked specifically to disrupted reward-seeking (Bolton et al., 2017, 2018; Kangas et al., 2022; Molet et al., 2016) and aberrant development of pleasure-reward circuitry (Bolton et al., 2018; Birnie et al., 2020, 2023). In humans, there are preliminary indications that unpredictability in early life is associated with alterations in neural circuits that subserve emotional salience, emotional regulation and memory and are also disrupted in major depressive disorder (Granger et al. 2021; Davis et al. 2017; Jirsaraie et al. 2023; Xu et al. 2023; Arnone et al. 2012; Brandl et al. 2022). Indeed, exposure to childhood unpredictability is linked to greater symptoms of depression and anhedonia in both adolescents and adults (Glynn et al., 2019; Spadoni et al., 2022). There is also a preliminary link with maternal depression and negative affect: Greater variability in maternal mood during the prenatal period predicts the development of negative affectivity in young children and depressive symptoms in adolescents (Glynn et al., 2018). Taken together these cross-species findings lead to the question whether in humans early-life unpredictability and later mental health problems may be linked specifically to anhedonia – defined as deficit in the subjective in the ability to experience pleasure or reward (Ho & Summers, 2013; Pizzagalli, 2014) -- as well as to broader depression symptoms.
One factor that may play a critical role in how early-life unpredictability leads to later reward disruption and mood symptoms is prior stress exposure. Neurobiological models contend that exposure to early-life unpredictability can disrupt the development of the stress-response system, as observed through improper maturation of the hippocampus (Davis et al., 2019, 2017), disrupted reward circuits (Birnie et al., 2020, 2023; Granger et al., 2021) and blunted release of cortisol in response to stress (Noroña-Zhou et al., 2020). For this reason, the consequences of an aberrant stress-response system should emerge following stressful life events, particularly through the development or worsening of mental health problems – as summarized by the stress-sensitization hypothesis (Harkness et al., 2006; McLaughlin et al., 2010; Rousson et al., 2020). As applied to the current investigation, this model would suggest that childhood unpredictability might create a latent predisposition that either interacts with later stressors to produce mood symptoms like depression or anhedonia.
At the same time, there is also evidence that the negative consequences of an aberrant stress-response system can partially be mitigated through social support (Ditzen & Heinrichs, 2014). Indeed, social support remains one of the strongest predictors of symptom severity across a range of mental health disorders (Harandi et al., 2017), including those in which depression symptoms and disruptions of reward processes feature prominently (Ozer et al., 2003; Corrigan & Phelan, 2004; Gariepy et al., 2016). Hence, in the same way that stress may interact with early-life unpredictability to produce mood symptoms in adulthood, high social support might buffer against increases in these symptoms among adults who experienced an unpredictable childhood.
A third possibility is that stress and reduced social support do not interact with early-life unpredictability but are rather consequences of unpredictability, which in turn increase risk for mood symptoms. In other words, individuals with unpredictable childhoods may be at increased risk for experiencing subsequent stressors are also more likely to withdraw from social support systems later in life, both of which may lead to greater symptoms of depression in adulthood. In this way, perceived stress and social support may act as mediators that help explain the relationships between unpredictable early-life experiences and later mood symptoms, rather than moderators that alter it. Indeed, social support has been found to act as a mediator (rather than a moderator) of the relationship between early-life risk factors for depression (e.g., childhood maltreatment) and subsequent depression symptoms (Li et al., 2022; Struck et al., 2022), and similar mediational results have been found for perceived stress levels (Pereira-Morales et al., 2019). However, lack of empirical data has left the roles of perceived stress and social support in the relationship between early-life unpredictability and mood symptoms ambiguous. Such work is important for clarifying the mechanisms by which childhood unpredictability might contribute to increased levels of neuropsychiatric symptoms later in life.
Here we examined the extent to which childhood unpredictability was associated with increases in both anhedonia and general depression symptoms before and after significant life stressors. We also investigated social support and perceived stress as potential moderators and mediators of the relation between childhood unpredictability and increases in these symptoms after significant life stressors. To test these questions, we leveraged the Marine Resiliency Study, a prospective longitudinal study of combat deployment effects on mental health at acute (within 3–6 months of deployment) and chronic (~10 yrs after deployment) time points. Owing to the variety of stressful and life-threatening events that can occur on military deployment, this event is frequently utilized as a subsequent life stressor through which to test a stress-sensitization model of mental illness stemming from earlier life adversity (Smid et al., 2013; Bandoli et al., 2017; Davis et al., 2022). Moreover, reintegrating into Civilian society following military service has its own set of occupational, social, and logistical challenges that renders this period distinctly stressful as well (Elnitsky et al., 2017).
Given extant cross-species evidence implicating early-life unpredictability as a contributor to anhedonia, we hypothesized that Marine and accompanying Navy service members reporting greater unpredictability in childhood would experience greater increases in anhedonia and depression between a) pre-deployment and 3–6 months following return from deployment b) between acute post-deployment and 8 – 10 years following return from deployment. We also explored the roles of perceived stress and social support in explaining the relationship between childhood unpredictability and mood symptoms (anhedonia, general depression symptoms) by testing these factors as mediators and moderators across both time periods. Together, these analyses should provide important verification of childhood unpredictability as a risk factor for adult mood symptoms and provide initial insight into mechanisms by which unpredictable childhood experiences might contribute to increases in anhedonia and depression in adulthood.
2. Materials and Method
2.1. Participants and Procedures
Participants were prior enrollees of the Marine Resiliency Study (Baker et al., 2012), a longitudinal study of Marines and accompanying Navy Corpsmen. Study enrollees were assessed longitudinally: prior to deployment (pre-deployment timepoint), three to six months after deployment (acute post-deployment timepoint), and approximately eight to ten years after returning from the original index deployment (chronic post-deployment timepoint). Participants were invited to complete the chronic post-deployment assessment if they had consented to be re-contacted and had completed at least one acute post-deployment assessment. All study procedures were approved by the VA San Diego Healthcare System and University of California, San Diego Institutional Review Boards.
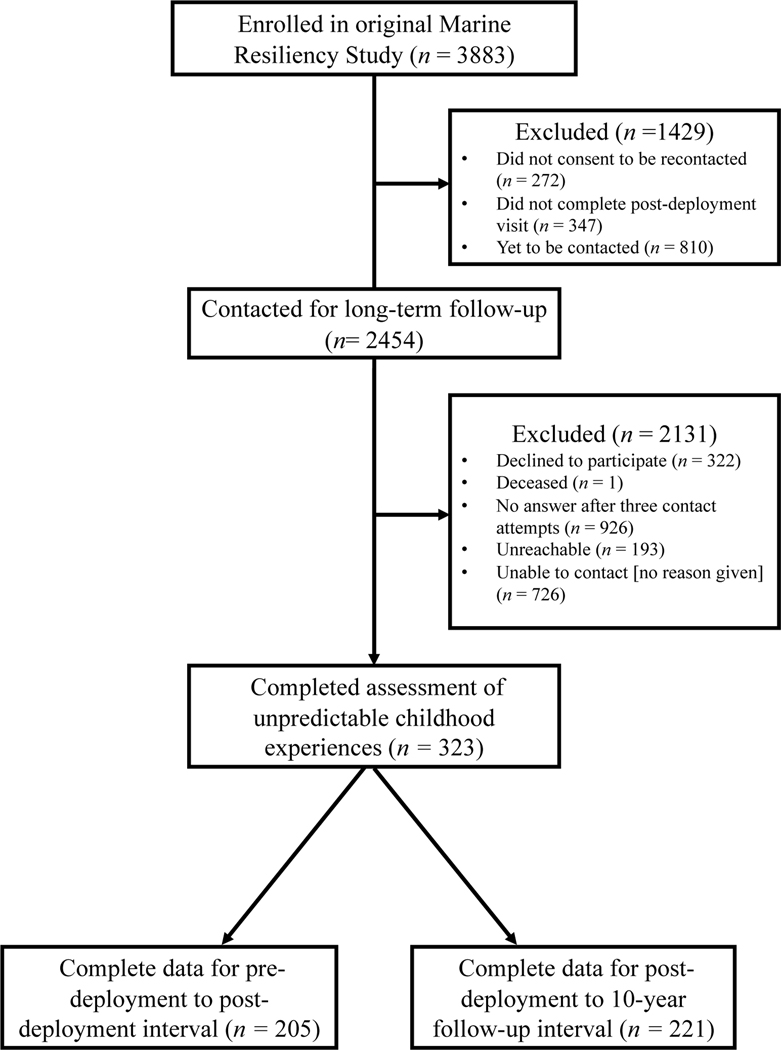
Of the 3883 participants who were enrolled in the original Marine Resiliency Study, N = 323 met eligibility criteria, consented to the long-term follow-up interview and completed our measure of unpredictable childhood experiences. Of these participants, N = 205 had the complete data necessary for longitudinal analyses involving pre-deployment and acute post-deployment while N = 221 had the complete data necessary for analyses of acute post-deployment to chronic post-deployment. Full information on participant recruitment flow can be found in Figure 1 and full demographic details of the final sample can be found in Table 1. Participants who completed the interview at chronic post-deployment were slightly older than those who did not, Mdiff = 0.61 years, t(353.033) = 2.43, p = .016, as well as being slightly more educated, Mdiff = 0.11, t(365.97) = 2.15, p = .032. Completers and non-completers did not differ in terms of race/ethnicity, depression or anhedonia symptoms at pre- or post-deployment, or in terms of perceived combat stress, perceived unit support, or perceived social support at post-deployment (ps > .134). Full statistics for these comparisons can be found in Table 1S of the Supplement.
Figure 1.
Participant flow and recruitment diagram. The Marine Resiliency Study refers to the parent investigation that collected data at pre-deployment and acute post-deployment. The long-term follow-up interview occurred approximately 8 – 10 years after participation in the original Marine Resiliency Study had concluded.
Table 1.
Demographic and clinical characteristics of the sample
| Variable | % | Mean (SD) |
|---|---|---|
| Sex | ||
| % Men | 100 | -- |
| % Women | 0 | -- |
| Ethnicity | -- | |
| % Black/African American | 3.2 | -- |
| % Native American | 2.3 | -- |
| % Asian | 4.0 | -- |
| % Pacifier Islander | 1.2 | -- |
| % Hispanic/Latino | 18.4 | -- |
| % White/Caucasian | 66.9 | -- |
| Education | ||
| % Some High School | 1.5 | -- |
| % GED | 1.5 | -- |
| % High School Diploma | 61.5 | -- |
| % Some College | 24.4 | -- |
| % Associate degree | 1.5 | -- |
| % 4-Year College Degree | 4.2 | -- |
| % Masters Degree | 0.4 | -- |
| % Doctoral Degree | 0.4 | -- |
| Parental Education Level* | ||
| % Parent with 4-Year College Degree | 39.6 | -- |
| % Parent without 4-Year College Degree | 60.4 | -- |
| Mean Age (SD) | -- | 23.13 (4.38) |
| Mean QUIC (SD) | -- | 10.48 (8.70) |
| Mean DRRI DCON (SD) | -- | 35.25 (10.58) |
| Mean DRRI PDS (SD) | -- | 3.92 (2.86) |
| BDI-A | ||
| Mean Pre-deployment (SD) | -- | 0.80 (1.27) |
| Mean Acute post-deployment (SD) | -- | 1.06 (1.54) |
| Mean Chronic post-deployment (SD) | -- | 2.42 (2.33) |
| BDI-D | ||
| Mean Pre-deployment (SD) | -- | 2.27 (3.14) |
| Mean Acute post-deployment (SD) | -- | 2.54 (3.90) |
| Mean Chronic post-deployment (SD) | -- | 5.65 (6.23) |
| BDI-2 | ||
| Mean Pre-deployment (SD) | -- | 6.25 (6.79) |
| Mean Acute post-deployment (SD) | -- | 7.46 (8.12) |
| Mean Chronic post-deployment (SD) | -- | 13.41 (11.97) |
| DRRI US | ||
| Mean Acute post-deployment (SD) | -- | 33.60 (11.48) |
| Mean Chronic post-deployment (SD) | -- | 47.97 (10.31) |
| DRRI GPDS | ||
| Mean Acute post-deployment (SD) | -- | 54.70 (10.16) |
| Mean Chronic post-deployment (SD) | 38.28 (8.04) |
Note. All demographic variables were assessed at pre-deployment except for parental education level, which as assessed at the chronic post-deployment timepoint. DRRI DCON was assessed at acute post-deployment, DRRI PDS was assessed at chronic post-deployment, and QUIC was assessed at chronic post-deployment. Acute post-deployment refers to the interval from 3–6 months after returning from deployment; chronic post-deployment refers to the interval between 8 – 10 years following return from deployment. GED = General education degree; QUIC = Questionnaire of Unpredictability in Childhood; BDI-A = Beck Depression Inventory Anhedonia Items; BDI-D = Beck Depression Inventory Depression items; BDI-2 = Beck Depression Inventory Two; DRRI = Deployment Risk and Resilience Inventory; DCON = Deployment Concerns subscale; PDS = Post-deployment stressors subscale; US = Unit support subscale; GPDS = General post-deployment support subscale. N = 221 for chronic post-deployment; N = 205 for acute post-deployment.
2.2. Measures
2.2.1. Questionnaire of Unpredictability in Childhood
The Questionnaire of Unpredictability in Childhood (QUIC; Glynn et al., 2019) is a 38-item self-report measure of exposure to social, emotional and environmental unpredictability in childhood. The QUIC asks respondents specifically about their life prior to age 18 years, with a subset of questions focused on events more likely to occur prior to age 12 years. A higher QUIC score indicates greater exposure to childhood unpredictability. Internal consistency for the QUIC in the current study was excellent (Cronbach’s alpha = .91). The QUIC was administered during the chronic post-deployment period (8–10 years following deployment). A subset of participants (n = 53) completed the QUIC multiple times during this period (n = 34 two completions, n = 19 three completions). The intraclass correlation coefficient for these multiple completions was .91, indicating excellent test-retest reliability.
2.2.2. Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996) is a 21-item self-report measure of depressive symptoms in the past two weeks, with a higher score indicating greater severity of depressive symptoms. In addition to the total BDI-2 score, two subscales were calculated from BDI-2: The BDI-2 anhedonia items (BDI-A) and the BDI-2 depression items (BDI-D). These subscales were computed by summing items relevant to anhedonia and general depression, respectively, as guided by results of a principal components analysis conducted in the full data set of the Marine Resiliency Study (see Acheson et al. 2022). Participants completed the BDI-II at the pre-deployment, acute post-deployment and chronic post-deployment timepoints. Reliability of the BDI-2 and its subscales ranged from good to very good across the three timepoints (Cronbach’s alpha = .739 - .838).
2.2.4. Deployment Risk and Resiliency Inventory (DRRI; King et al., 2006).
The DRRI is a self-report scale that assesses key psychosocial risk and resilience factors for military personnel deployed to war zones or other hazardous environments. The full DRRI yields 14 distinct constructs related to pre-deployment, deployment, and post-deployment factors. The DRRI and its subscales have demonstrated strong evidence of validity and reliability (King et al., 2006) including in samples of soldiers deployed to Iraq and Afghanistan like those examined in the present study (Vogt et al., 2008).
Of the available DRRI subscales, the following were analyzed in the present investigation. First, the Deployment Concerns subscale (DRRI DCON) was used as a measure of perceived stress during deployment (e.g., “I thought I would never survive”), and was administered during the acute post-deployment timepoint. Second, the General Post-deployment Support subscale (DRRI GPDS) was used as a measure of general social support following deployment (e.g., “The American people made me feel at home when I returned”), and was administered during both the acute and chronic post-deployment timepoints. Third, the Unit Support subscale (DRRI US) was used as a measure of support from the respondent’s military comrades within their unit both during deployment and after returning from deployment (e.g., “My unit is like a family to me.”), and was administered during both the acute and chronic post-deployment timepoints. Finally, the post-deployment stressors (DRRI PDS) subscale was used to assess the perceived stress during the reintegration period following deployment (e.g., “Since returning home I have experienced serious financial problems.”), and was administered at the chronic post-deployment timepoint.
For perceived stress during deployment (DRRI DCON), participants were directed to respond according to their experiences on deployment. For DRRI PDS, GPDS, and US, participants were directed to respond to the time period since their last deployment. Thus, when administered at acute post-deployment, DRRI GPDS and US measures reflected perceived levels of support in the 3 – 6 months since returning from deployment. When DRRI GPDS, US, and PDS were administered at chronic post-deployment, they reflected perceived levels of stress/support in the 8 – 10 years since returning from deployment.
2.2.4. Childhood Socioeconomic Status
In addition to our main outcomes, we also assessed participants’ parental education levels during childhood as a proxy for childhood socioeconomic status, which was used to gauge general levels of adversity during childhood. Specifically, participants reported the education level and occupation of both their parents when the participant was 8 years old and 16 years old. Participants reported parental education during visits from the chronic post-deployment timepoint. Parental education was coded as a dichotomized variable related to the highest parental education level at age 16 years wherein participants with a parent who earned a bachelor’s degree or higher were coded as ‘1’ and all others were coded as ‘0’.
2.3. Analytical Plan
2.3.1. Data processing.
Scores for all questionnaires (QUIC, BDI-A, DRRI subscales) were computed by taking an average of all completed items and multiplying by the total number of items on the scale, which allowed us to derive inferred total scores for participants in the case of missing items. If multiple assessments of depression (BDI-2) or stress (DRRI DCON, DRRI PDS) had been completed within a given post-deployment timeframe (i.e., acute or chronic), the highest score was used to capture the most severe clinical state or highest perceived stress level of the participant during the time period. If multiple assessments of the DRRI support measures (i.e., DRRI US, DRRI GPDS) had been completed within given post-deployment timeframe, the lowest score was used to capture the lowest perceived support during the interval. If multiple assessments of the QUIC or parental education were completed during the chronic post-deployment timeframe, the earlier score was used to minimize the temporal gap between childhood and the current assessment.
2.3.2. Testing longitudinal relations between childhood unpredictability and depression change.
To investigate the relationship between childhood unpredictability and changes in mood symptoms (anhedonia and general depression), we first conducted hierarchical regression for each interval (i.e., pre-deployment to acute post-deployment, acute post-deployment to chronic post-deployment). For the acute post-deployment interval, each BDI-2 measure (BDI-A, BDI-D, BDI-2 total) was tested as an outcome in separate regression models. For predictors, the corresponding depression measure from pre-deployment was entered first, followed by total scores from the QUIC, which tested whether higher childhood unpredictability would predict higher depression symptomology after controlling for the same measure of depression symptomology from pre-deployment (i.e., change in depression symptomology from pre-deployment to acute post-deployment). An identical set of models was tested for the interval from acute post-deployment to chronic post-deployment, with the depression measure from chronic post-deployment serving as the outcome variable and the same measure from the acute post-deployment being entered in the first step, followed by QUIC in the second step.
Next, we further examined the specificity of childhood unpredictability as a predictor of anhedonia or depression change by testing whether any effect of QUIC remained significant after accounting for parental education, which served as a proxy for childhood socioeconomic status (CSES). Children from low SES backgrounds are at heightened risk for a variety of environmental stressors during childhood (Merrick et al., 2018; Domornay et al., 2023), so controlling for CSES can help establish whether the effect of childhood unpredictability on mood symptoms is distinct from other forms of early-life adversity. In these models, the BDI measure at the earlier timepoint were entered first (i.e., pre-deployment BDI for acute post-deployment models; acute post-deployment BDI for chronic post-deployment models), followed by parental education, and finally the QUIC total score, which tested whether the relationship between childhood unpredictability and depression symptom change was independent of childhood SES. Of note, these analyses were conducted with a reduced sample as only a subset of participants completed the parental education measure (N = 189).
2.3.3. Testing potential moderators and mediators of the relationship between childhood unpredictability and depression change.
Finally, to help better understood the mechanisms by which childhood unpredictability might lead to increases in mood symptoms, we tested perceived levels of stress and social support as potential moderators and mediators of the longitudinal QUIC-BDI relationship. Examination of potential moderators and mediators was conducted separately for each interval (i.e., pre-deployment to acute post-deployment; acute post-deployment to chronic post-deployment). For analyses predicting acute post-deployment mood symptoms, deployment stressors DRRI US, DRRI GPDS, and DRRI DCON from the acute post-deployment timepoint were tested as potential moderators/mediators. For analyses predicting chronic post-deployment mood symptoms, post-deployment stressors DRRI US, DRRI GPDS, and DRRI PDS were tested as potential moderators/mediators.
To reduce redundancy in these analyses, we utilized an analytic framework guided by the MacArthur approach, which helps unambiguously categorize variables as potential moderators or mediators (Chmura Kraemer et al., 2008). In this framework, zero-order associations are tested between the X variable (i.e., QUIC), and the Y variable (i.e., the BDI measure), and the potential moderators/mediators of interest. Variables that are not associated with X (i.e., independent of X) are considered candidate moderators, variables that associated with both X and Y are considered candidate mediators, and variables that are only associated with X are not considered further.
Potential moderators were then tested by examining whether the interaction between the X (i.e., QUIC) and the moderator predicted additional, significant variance in the outcome variable (i.e., BDI measure at the later timepoint) in a regression model that included the BDI measure from the earlier timepoint (step 1), the main effect of QUIC (step 2), the main effect of the potential moderator (step 3), and finally the QUIC x Moderator interaction (step 4). Potential mediators were tested using the model 1 of the PROCESS Macro for SPSS (Preacher & Hayes, 2004), which yields an indirect effect of the mediator on the outcome variable by testing it across k samples of the data’s sample size with replacement (k = 10000 for the study study) and computing a 95% confidence interval (CI). The indirect effect of the mediator is considered significant if the 95% bootstrapped CI does not contain zero. Here, the outcome variable again was the BDI measure of interest at the later timepoint, QUIC was X variable, and the corresponding BDI measure from the earlier timepoint was entered as a control variable. Thus, these models tested whether a significant proportion of the effect of QUIC on the BDI measure at the later timepoint could be accounted for by the candidate mediator. In cases where multiple mediators were found, they were tested simultaneously in a parallel mediation model to determine whether their mediating effects were unique or redundant.
All predictors were z-scored to aid interpretability. All reported regression coefficients are taken from the regression model in which they were first entered. Alpha was set at .05 (two-tailed) for all tests. Analyses were conducted in SPSS Version 28.
3. Results
3.1. Associations between Childhood Unpredictability and Post-Deployment Depression Symptoms
As hypothesized, levels of QUIC significantly predicted higher BDI-A scores at both acute post-deployment, β = 0.16, 95% CI[0.05, 0.29], p = .007, and chronic post-deployment, β = 0.25, 95% CI[13, 0.39], p < .001, after controlling for levels of BDI-A at the earlier timepoint. Thus, participants who reported greater unpredictability during childhood tended to experience greater increases in anhedonia from both pre-deployment to acute post-deployment and from acute post-deployment to chronic post-deployment. QUIC was also a significant predictor of general depression symptoms as measured by the BDI-D subscale and total BDI-2 at both times timepoints. Specifically, higher QUIC significantly predicted greater acute post-deployment scores on the BDI-D, β = 0.22, 95% CI[0.10, 0.34], p < .001, and total BDI-2, β = 0.21, 95% CI[0.09, 0.32], p < .001 as well as greater chronic post-deployment scores on the BDI-D, β = 0.17, 95% CI[0.05, 0.31], p = .009, and total BDI-2, β = 0.20, 95% CI[0.08, 0.33], p = .002. Thus, participants reporting greater unpredictability in childhood appeared to experience larger increases in more general symptoms of depression, not specifically anhedonia. Accordingly, only models involving the total BDI-2 scale were considered in subsequent analyses for the purposes of parsimony.
3.2. Testing the Specificity of Childhood Unpredictability Relative to Childhood SES
Results of regression models used to predict post-deployment BDI-2 scores at acute and chronic post-deployment from QUIC after controlling for childhood socioeconomic status (i.e., parental education) can be found in Table 2. Parental education did not significantly predict BDI-2 scores at either acute post-deployment (p = .122) or chronic post-deployment (p = .095). Moreover, the effect of QUIC remained significant at both post-deployment timepoints even after controlling for parental education and (ps < .003). Thus, the association of retrospectively reported childhood unpredictability with changes in post-deployment depression symptoms was independent of parental education.
Table 2.
Hierarchical regression analyses predicting depression symptoms from childhood unpredictability adjusting for parental education level.
| Outcome variable | Step | Predictor | ΔR2 | β (95% CI) | t | p |
|---|---|---|---|---|---|---|
| BDI-2 at acute post-deployment | 1 | BDI-2 at pre-deployment | .296 | 0.54 (0.43 – 0.70) | 8.29 | < .001 |
| 2 | Parent Edu | .010 | −0.10 (−0.23 – 0.03) | −1.56 | .122 | |
| 3 | QUIC Total | .057 | 0.25 (0.12 – 0.39) | 3.81 | < .001 | |
|
| ||||||
| BDI-2 at chronic post-deployment | 1 | BDI-2 at acute post-deployment | .086 | 0.29 (0.18 – 0.49) | 4.20 | <.001 |
| 2 | Parent Edu | .014 | −0.12 (−0.25 – 0.02) | −1.68 | .095 | |
| 3 | QUIC Total | .042 | 0.22 (0.07 – 0.37) | 3.00 | .003 | |
Note. Coefficients displayed for each variable are taken from the regression model in which they were first entered. Parent Edu was coded such that 0 = neither parent achieved a 4-year college degree and 1 = at least one parent achieved a 4-year college degree. Acute post-deployment refers to the interval between 3–6 months after returning from deployment; chronic post-deployment refers to the interval between 8 – 10 years following return from deployment. QUIC = Questionnaire of Unpredictability in Childhood; BDI-2 = Beck Depression Inventory-II; Parent Edu = Parental education level. N = 189.
3.3. Testing mediators and moderators of relationship between childhood unpredictability and depression change
3.3.1. Acute Post-deployment.
Associations between QUIC, acute post-deployment BDI-2, and the three candidate moderators/mediators at acute-post-deployment (i.e., DRRI DCON, DRRI US, DRRI GPDS) can be found in Table 3. While perceived stress during deployment (DRRI DCON) was positively associated with acute post-deployment BDI-2 (p < .001), it was unrelated to QUIC (p = .278). Therefore, perceived deployment stress was tested as a potential moderator of the relationship between QUIC and acute post-deployment depression symptoms. In contrast, DRRI US and DRRI GPDS were negatively associated with both QUIC and total BDI-2 scores (ps < .001), suggesting that general social support (DRRI GPDS) and unit support (DRRI US) at acute post-deployment were potential mediators of the relationship between childhood unpredictability and acute post-deployment depression symptoms.
Table 3.
Associations between childhood unpredictability, depression symptoms, and potential moderator and mediator variables at acute post-deployment time point.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. QUIC Total | 1 | .28** | .07 | -.20** | -.33** |
| 2. BDI-2 Total | 1 | .31** | −.31** | −.46** | |
| 3. DRRI DCON | 1 | −.08 | −.07 | ||
| 4. DRRI US | 1 | .55** | |||
| 5. DRRI GPDS | 1 |
Note. QUIC was assessed at chronic post-deployment; all other variables were assessed at acute post-deployment. Acute post-deployment refers to the interval from 3–6 months after returning from deployment; chronic post-deployment refers to the interval between 8 – 10 years following return from deployment. QUIC = Questionnaire of Unpredictability in Childhood; BDI-2 = Beck Depression Inventory-II;. DRRI = Deployment Risk and Resilience Inventory; DCON = Deployment concerns subscale; US = Unit support subscale; GPDS = General post-deployment support subscale.
p ≤ .01. N = 205.
To test perceived stress during deployment DRRI DCON as a moderator, we ran an additional regression in which the QUIC x DRRI DCON interaction was tested as a predictor of acute post-deployment BDI-2 scores. Although the main effect of DRRI DCON was significant, β = 0.25, 95% CI [.15, .37], p < .001, the DRRI DCON x QUIC interaction was not, β = 0.08, 95% CI [−0.03, .19], p = .146. Thus, while perceived stress during deployment was predictive of higher depression symptoms following deployment, it did not moderate the relationship between childhood unpredictability and depression symptoms following deployment.
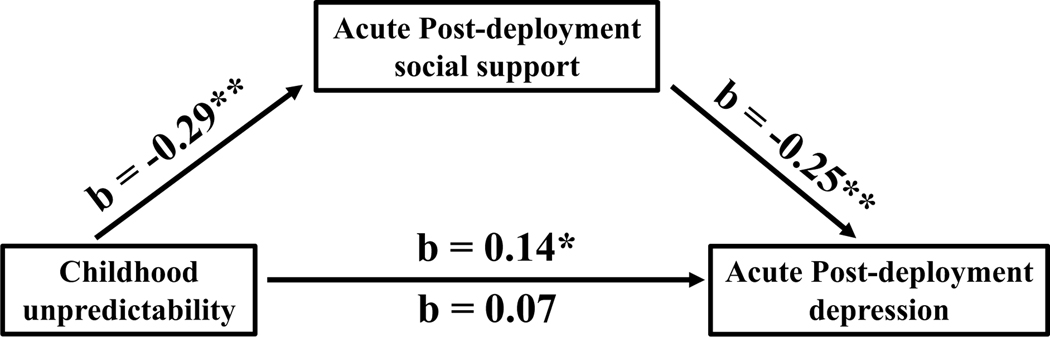
To test whether general social support (DRRI GPDS) and unit support (DRRI US) mediated the relationship between QUIC and BDI-2 at acute post-deployment, we input these variables as mediators in model 1 of the SPSS PROCESS macro, with QUIC serving as the X variable, acute post-deployment BDI-2 as the Y variable, and pre-deployment BDI-2 as a control variable. These tests revealed that while the indirect effect of DRRI US was not significant, b = 0.01, 95% CI [−0.002, 0.05], the indirect effect of DRRI GPDS was significant, b = 0.07, 95% CI [0.03, 0.15], and explained approximately 34% of the effect of QUIC on acute post-deployment BDI-2 scores. Notably, the direct effect of QUIC on post-deployment BDI-2 remained significant after accounting for DRRI GPDS, b = 0.14, 95% CI [0.02, 0.26], p = .023, suggesting that DRRI GPDS is a partial mediator of this relationship (see Figure 2 for a full illustration of the mediating model). Thus, the relationship between childhood unpredictability and increased depression symptoms at acute post-deployment is partially attributable to lower levels of general social support at acute post-deployment, and independent of support from one’s military unit.
Figure 2.
Effect of childhood unpredictability on depression symptoms 3–6 months post deployment as mediated by general social support at acute post-deployment. Acute post-deployment refers to the interval from 3–6 months after returning from deployment. Childhood unpredictability was measured by the QUIC, post-deployment social support by the DRRI GPDS, and depression with the BDI-2. Pre-deployment BDI-2 was entered as a covariate to control for depression symptoms at pre-deployment. QUIC = Questionnaire of unpredictability in childhood; DRRI GPDS = Deployment risk and resilience inventory general post-deployment support subscale; BDI-2 = Beck Depression Inventory II. *p < .05; **p < .001.
3.3.2. Chronic post-deployment.
Associations between QUIC, chronic post-deployment BDI-2, and the three candidate moderators/mediators at chronic post-deployment (i.e., DRRI PDS, DRRI US, DRRI GPDS) can be found in Table 4. In contrast to results from acute post-deployment, all three candidate variables were significantly associated with both QUIC scores and BDI-2 total scores (ps < .001). Thus, levels of perceived stress (DRRI PDS), unit support (DRRI US), and general social support (DRRI GPDS) were all tested as mediators of the relationship between childhood unpredictability and depression symptoms at chronic post-deployment.
Table 4.
Associations between childhood unpredictability, depression symptoms, and potential moderator and mediator variables at chronic post-deployment
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. QUIC Total | 1 | .33** | .37** | -.22** | -.44** |
| 2. BDI-2 Total | 1 | .46** | −.29** | −.46** | |
| 3. DRRI PDS | 1 | −.23** | −.25** | ||
| 4. DRRI US | 1 | .44** | |||
| 5. DRRI GPDS | 1 |
Note. All variables were assessed at chronic post-deployment. Chronic post-deployment refers to the interval between 8 – 10 years following return from deployment. QUIC = Questionnaire of Unpredictability in Childhood; BDI-2 = Beck Depression Inventory-II; DRRI = Deployment Risk and Resilience Inventory; PDS = Post-deployment stressors subscale; US = Unit support subscale; GPDS = General post-deployment support subscale.
p ≤ .001. N = 221.
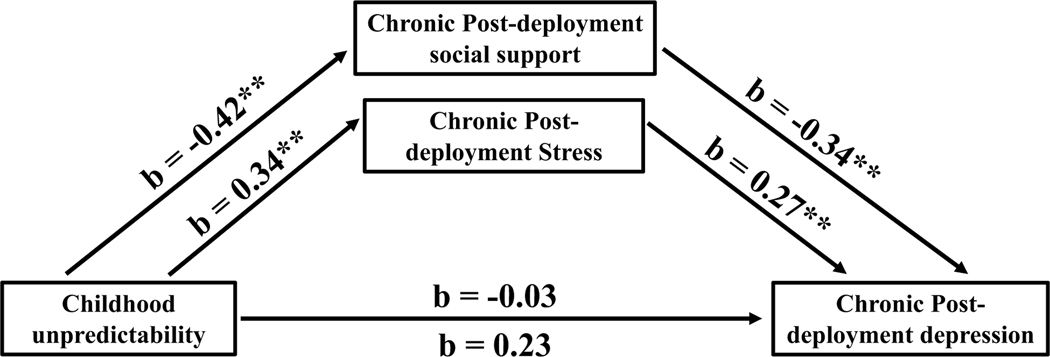
Next, all three variables were tested in separate models as mediator variables using the SPSS PROCESS macro, with QUIC serving as the X variable, chronic post-deployment BDI-2 as the Y variable, and acute post-deployment BDI-2 as a control variable These tests revealed significant indirect effects for all three variables: DRRI PDS, b = 0.10, 95% CI [0.05, 0.17], DRRI US, b = 0.03, 95% CI [0.0003, 0.08], and DRRI GPDS, b = 0.15, 95% CI [0.07, 0.24]. Since indirect effects for all three variables were significant, we next entered them all into a parallel mediation model to determine whether they reflected unique or redundant mediating pathways. In this overall model, the indirect effect of DRRI PDS remained significant, b = 0.09, 95% CI [0.05, 0.15], as did the indirect effect of DRRI GPDS, b = 0.14, 95% CI [0.07, 0.23]. In contrast, the indirect effect of DRRI US was no longer significant, b = −0.003, 95% CI [−0.03, 0.02]. In the overall mediation model, indirect effects accounted for 90% of the total effect of QUIC on chronic post-deployment BDI-2, and the direct effect of QUIC on chronic post-deployment BDI-2 was no longer significant, b = −0.03, 95% CI [−0.16, 0.10], p = .691. An illustration of the complete mediation model for chronic post-deployment can be found in Figure 3.
Figure 3.
Effect of childhood unpredictability on chronic post-deployment depression symptoms as mediated by general social support and post-deployment stressors chronic post-deployment. Chronic post-deployment measures were assessed between 8 – 10 years following return from deployment. Childhood unpredictability was measured by the QUIC, post-deployment social support by the DRRI GPDS, post-deployment stress with the DRRI PDS, and depression with the BDI-2. Pre-deployment BDI-2 was entered as a covariate to control for depression symptoms at pre-deployment. QUIC = Questionnaire of childhood unpredictability; DRRI = Deployment risk and resilience inventory; GPDS = General post-deployment support subscale; PDS = Post-deployment stressors subscale; BDI-2 = Beck Depression Inventory II. **p < .05; **p < .001.
4. Discussion
Consistent with past work linking early-life unpredictability to the development of diminished reward response across species (Bolton et al., 2017, 2018; Kangas et al., 2022; Molet et al., 2016; Glynn et al., 2018), we tested the hypothesis that greater unpredictability during childhood increases risk for symptoms of depression across distinct periods of stress. We examined the longitudinal association between childhood unpredictability as measured by the QUIC and the increases in mood symptoms (anhedonia and general depression symptoms) in the aftermath of both combat deployment (~3–6 mo post-deployment; referred to as ‘acute post-deployment’) and the period of reintegration into Civilian society (~8–10 yrs later; referred to as ‘chronic post-deployment’). Participants reporting higher childhood unpredictability experienced larger increases in depression symptoms across both periods. This association remained significant after controlling for an indicator of childhood socioeconomic status (CSES), suggesting that the effect of unpredictable childhood experiences was not merely a proxy for greater childhood adversity. The relationship between higher childhood unpredictability and increased depression symptoms at acute post-deployment was partially mediated by lower levels of general social support during the acute post-deployment period. The association between unpredictability and increased depression at chronic post-deployment was fully mediated by the combination of lower levels of general social support and higher perceived stress during the chronic post-deployment period – as indexed disruptions in psychosocial functioning and adjustment. Overall, these findings support the notion that childhood unpredictability might play a role in increasing depression symptoms following stressful transitionary periods and suggest that disruptions in psychosocial adjustment and social support in early adulthood my serve as critical links in the relationship between childhood unpredictability and depression later in life.
Our study complements existing cross-sectional studies demonstrating an association between early-life unpredictability and adult psychopathology by demonstrating that childhood unpredictability also predicts longitudinal increases in mental health symptoms – namely depression – over time (Glynn et al., 2018; Spadoni et al., 2022). Importantly, the longitudinal relationship between childhood unpredictability and depression was demonstrated across two distinct timespans (i.e., pre-deployment to post-deployment, acute post-deployment to chronic post-deployment), each with their own distinct challenges (i.e., deployment and civilian reintegration). The prospective, longitudinal nature of our design not only helps further implicate childhood unpredictability as a risk factor for adult psychopathology but suggests that childhood unpredictability continues to confer risk for increasing mental health symptoms across different phases of the lifespan after exposure to certain kinds of stressors.
Foundational rodent studies indicate that early-life unpredictability disrupts circuits associated with both reward (e.g. striatal circuit connectivity) as well as emotional regulation and stress responding (e.g. hippocampal circuit function and hypothalamic-pituitary-axis responses), suggesting unpredictability modulates multiple neural circuits implicated in anhedonia and depression (Walker et al., 2017; Davis et al., 2017; Noroña-Zhou et al., 2020; Birne et al., 2020; Bolton et al., 2018; Molet et al., 2016). Consistent with these animal data, our study is the first to link childhood unpredictability to increased levels of depression symptoms in adulthood. Contrary to expectations however, childhood unpredictability did not interact with levels of perceived stress to predict depression, as would be hypothesized based on a stress-sensitization model (Stroud et al., 2011). In the case of depression symptoms experienced in the acute post-deployment period, childhood unpredictability and deployment stress appeared to exert independent effects: Higher levels of both were predictive of depression symptoms following return from deployment and were not related to each other. In the case of chronic post-deployment, higher perceived stress during the reintegration period mediated the effect of childhood unpredictability on depression symptoms at chronic post-deployment. This finding suggests that higher childhood unpredictability could increase risk for experiencing stressors during the Civilian reintegration period, which would in turn increase risk for depression symptoms. The discrepancy in the effect of perceived stress at the acute versus chronic post-deployment periods may be due to differences in the controllability of these stressors: Whereas deployment stress may be heavily dictated by experiences outside the individual’s control (e.g., combat events) stressors in the civilian reintegration represent psychosocial disruptions that are relatively more controllable (e.g., financial problems), perhaps allowing individual differences in previous developmental experiences (e.g., childhood unpredictability) to exert greater influence. How an unpredictable childhood might increase risk for psychosocial disruption during civilian reintegration is unclear, though previous studies have found links between childhood unpredictability and impairments related to the same reintegration stressors that mediated the association between childhood unpredictability and adult depression in our investigation. For example, greater unpredictability during childhood has been linked to greater impairment in social and romantic relationships in adulthood (Maranges et al., 2021; Barbaro & Shackelford, 2019; Szepsenwol et al., 2019) and to greater difficulty making career decisions in adulthood (Xu et al., 2022) – similar to the relationship- and employment-related stressors that composed our measure of perceived stress in this study.
This study also demonstrates that social support is a potential mediating variable in the relationship between childhood unpredictability and adult psychopathology. Lower social support in both the months following return from deployment and approximately a decade later explained a large proportion of the effect of childhood unpredictability on increased depression symptoms over both intervals. One possible interpretation of this finding is that unpredictable childhood environments negatively influence interpersonal functioning in a way that makes individuals more likely to withdraw from or underutilize support networks. Conversely, predictable childhood may strengthen support expectations in later relationships, thereby enhancing engagement with social support networks that buffer against development of mood symptoms after significant life stressors. In support, predictability during childhood is associated with prosocial behavior in adulthood (Maranges et al., 2021; Ren et al., 2022) and ocial support has been found to mediate a broad range of evidence-based treatment effects on symptom change in depression, suggesting that factors that influence social support may consequently influence depression symptoms (Dour et al., 2014). Alternatively, social support following deployment may have partially included the same support network that existed in childhood, with unpredictable networks and predictable networks mediating increased and decreased risk of depression respectively. These explanations are not mutually exclusive: predictable care in childhood could render individuals more likely to seek additional support and also contribute to a stronger support network. Future research may clarify the relevance of these two explanations by conducting a more granular examination of the specific aspects of a support network mediating the relationship between childhood unpredictability and later depression.
In terms of what circuits might mediate the associations reported here, early-life unpredictability disrupts maturation of striatal (Bolton et al., 2017, 2018; Kangas et al., 2022; Molet et al., 2016) and hippocampal circuits (Davis et al., 2017). Disruption of both circuits are linked to anhedonia and depression symptoms (Campbell & MacQueen, 2004), and these circuits are sensitive to early-life adversity effects across species (Tartt et al., 2022; Jiang et al., 2023; Tang et al., 2022; ). These circuits are also important for social behavior and reward (Solomonov et al., 2023), suggesting they could contribute to the observed relationship between childhood adversity, social support and risk for depression and anhedonia. Hippocampal volume is also inversely related to social support in adults who had experienced other forms of childhood adversity (Förster et al., 2021), and hippocampal abnormalities have been linked to disruptions in a range of social processes (e.g., tracking dynamic social behavior, remembering social rules) that could lead to diminished engagement in support networks (Montagrin et al., 2017). Further research is needed to understand if these (or other) circuits or others mediate the observed links between childhood unpredictability and depression symptoms.
4.1. Limitations
Results of the present study must be considered in light of several important limitations. First, childhood unpredictability was assessed retrospectively and could be subject to self-report biases that skewed the accuracy of reported experiences. Test-retest reliability of the QUIC was high across a two-year period (albeit in a small sample), suggesting that participants’ perceptions of their childhood unpredictability were stable and thus unlikely to have been dictated by factors that shift across time (e.g., life circumstances, mood states at the time of administration). The QUIC was also associated with anhedonia and depression over three timepoints spanning more than a decade, suggesting its relationship to anhedonia is not state specific. Moreover, the QUIC has been shown to prospectively predict longitudinal changes in unpredictability within the family and home environment in developmental samples, offering further evidence that the instrument validly assesses unpredictability despite its retrospective assessment method (Glynn et al., 2019). Nonetheless, greater validity would undoubtedly be achieved by assessing childhood unpredictability during or closer to childhood, which should be a priority for future studies looking to verify the relationship between this construct and mental health symptoms later in life.
Second, our study did not examine the relationship between childhood unpredictability and depression change in individuals who did not experience a stressful life event (i.e., participants who did not go on military deployment). For this reason, it is difficult to determine the extent to which stressful life experiences contribute to increased depression among those who had unpredictable childhoods, as we do not know the ‘normative’ trajectories of depression symptoms among individuals of similar backgrounds who did not experience such stressful periods. Notably, there was no interaction between childhood unpredictability and perceived stress levels during either time interval in predicting later depression. Thus, it appears that at minimum, greater stress exposure does not amplify the effect of childhood unpredictability on later mental health symptoms.
Finally, our sample was all men, which necessarily limits our ability to generalize these findings to women. Early-life adversity has different effects on reward circuits and behaviors in male versus female rodents and humans (Anisman & Matheson, 2005; Harkness et al., 2021; Levis et al., 2022), which may contribute to higher rates of depression observed among women (Parker & Brotchie, 2010). Thus, future research is needed to compare longitudinal associations between childhood unpredictability and depression across men versus women.
5. Conclusions
The purpose of this study was to examine the association between childhood unpredictability and the development of depression symptoms following military deployment and civilian reintegration, as well as evaluate the roles of perceived stress and social support in these associations. Participants who reported greater unpredictability during childhood experienced a greater increase in both general depression symptoms and anhedonia, from before to after military deployment and from immediately after military deployment to approximately a decade later. The effect of childhood unpredictability on depression symptoms was mediated by lower perceived social support in both the short-term and long-term following return from deployment, as well as by greater disruptions in psychosocial functioning during the civilian reintegration period. Overall, this study offers further evidence that childhood unpredictability contributes to the development of depression symptoms and builds upon the results of previous investigations by shedding light on the possible psychosocial factors through which childhood unpredictability confers risk for later depression. Future research should aim to replicate this work with prospective measures of childhood unpredictability, examine mediating brain circuitry, and compare the effect of childhood unpredictability on depression development between men and women. Clinically, these results could ultimately inform novel strategies for preventing depressive disorders that involve increasing the structure and predictability of childhood routines as well as developing social support interventions after life stressors.
Supplementary Material
6. Acknowledgements
Support for this work includes NIMH P50MH096889 (DGB, VBR), the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs (MV, CH), BLR&D VA Research Career Scientist Award (VBR), and the Center of Excellence for Stress and Mental Health (MV, CH, BC, DGB, VBR).
References
- Acheson DT, Vinograd M, Nievergelt CM, Yurgil KA, Moore TM, Risbrough VB, & Baker DG (2022). Prospective examination of pre-trauma anhedonia as a risk factor for post-traumatic stress symptoms. European Journal of Psychotraumatology, 13(1), 2015949. doi: 10.1080/20008198.2021.2015949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Porter LE, & Brown DW (2020). Inside the adverse childhood experience score: strengths, limitations, and misapplications. American Journal of Preventive Medicine, 59(2), 293–295. [DOI] [PubMed] [Google Scholar]
- Anisman H, & Matheson K. (2005). Stress, depression, and anhedonia: caveats concerning animal models. Neuroscience & Biobehavioral Reviews, 29(4–5), 525–546. 10.1016/j.neubiorev.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Arnone D, McIntosh AM, Ebmeier KP, Munafò MR, & Anderson IM (2012). Magnetic resonance imaging studies in unipolar depression: systematic review and meta-regression analyses. European Neuropsychopharmacology, 22(1), 1–16. [DOI] [PubMed] [Google Scholar]
- Baker DG, Nash WP, Litz BT, Geyer MA, Risbrough VB, Nievergelt CM, O’Connor DT, Larson GE, Schork NJ, Vasterling JJ, Hammer PS, & Webb-Murphy JA (2012). Predictors of Risk and Resilience for Posttraumatic Stress Disorder Among Ground Combat Marines: Methods of the Marine Resiliency Study. Preventing Chronic Disease, 9(5). 10.5888/pcd9.110134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandoli G, Campbell-Sills L, Kessler RC, Heeringa SG, Nock MK, Rosellini AJ, ... & Stein MB (2017). Childhood adversity, adult stress, and the risk of major depression or generalized anxiety disorder in US soldiers: a test of the stress sensitization hypothesis. Psychological Medicine, 47(13), 2379–2392. doi: 10.1017/S0033291717001064, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baram TZ, Davis EP, Obenaus A, Sandman CA, Small SL, Solodkin A, & Stern H. (2012). Fragmentation and unpredictability of early-life experience in mental disorders. American Journal of Psychiatry, 169(9), 907–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaro N, & Shackelford TK (2019). Environmental unpredictability in childhood is associated with anxious romantic attachment and intimate partner violence perpetration. Journal of Interpersonal Violence, 34(2), 240–269. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown G. (1996). Beck Depression Inventory–II (BDI-II) [Database record]. APA PsycTests. 10.1037/t00742-000. [DOI] [Google Scholar]
- Birnie MT, Kooiker CL, Short AK, Bolton JL, Chen Y, & Baram TZ (2020). Plasticity of the reward circuitry after early-life adversity: mechanisms and significance. Biological Psychiatry, 87(10), 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnie MT, Short AK, de Carvalho GB, Taniguchi L, Gunn BG, Pham AL, ... & Baram TZ (2023). Stress-induced plasticity of a CRH/GABA projection disrupts reward behaviors in mice. Nature Communications, 14(1), 1088. 10.1038/s41467-023-36780-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton JL, Molet J, Regev L, Chen Y, Rismanchi N, Haddad E, Yang DZ, Obenaus A, & Baram TZ (2017). Anhedonia following early-life adversity involves aberrant interaction of reward and anxiety circuits and is reversed by partial silencing of amygdala corticotropin-releasing hormone gene. Biological Psychiatry. 10.1016/j.biopsych.2017.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton JL, Molet J, Regev L, Chen Y, Rismanchi N, Haddad E, Yang DZ, Obenaus A, & Baram TZ (2018). Anhedonia Following Early-Life Adversity Involves Aberrant Interaction of Reward and Anxiety Circuits and Is Reversed by Partial Silencing of Amygdala Corticotropin-Releasing Hormone Gene. Biological Psychiatry, 83(2), 137–147. 10.1016/j.biopsych.2017.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandl F, Weise B, Mulej Bratec S, Jassim N, Hoffmann Ayala D, Bertram T, ... & Sorg C. (2022). Common and specific large-scale brain changes in major depressive disorder, anxiety disorders, and chronic pain: a transdiagnostic multimodal meta-analysis of structural and functional MRI studies. Neuropsychopharmacology, 47(5), 1071–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S, & MacQueen G. (2004). The role of the hippocampus in the pathophysiology of major depression. Journal of Psychiatry and Neuroscience, 29(6), 417–426. [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217–225. [DOI] [PubMed] [Google Scholar]
- Chmura Kraemer H, Kiernan M, Essex M, & Kupfer DJ (2008). How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology, 27(2S), S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, & Phelan SM (2004). Social support and recovery in people with serious mental illnesses. Community Mental Health Journal, 40, 513–523. [DOI] [PubMed] [Google Scholar]
- Davis EP, Korja R, Karlsson L, Glynn LM, Sandman CA, Vegetabile B, Kataja EL, Nolvi S, Sinervä E, Pelto J, Karlsson H, Stern HS, & Baram TZ (2019). Across continents and demographics, unpredictable maternal signals are associated with children’s cognitive function. EBioMedicine, 46, 256–263. 10.1016/j.ebiom.2019.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, Stout SA, Molet J, Vegetabile B, Glynn LM, Sandman CA, Heins K, Stern H, & Baram TZ (2017). Exposure to unpredictable maternal sensory signals influences cognitive development across species. Proceedings of the National Academy of Sciences of the United States of America, 114(39), 10390–10395. 10.1073/pnas.1703444114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, McCormack K, Arora H, Sharpe D, Short AK, Bachevalier J, ... & Baram TZ (2022). Early life exposure to unpredictable parental sensory signals shapes cognitive development across three species. Frontiers in Behavioral Neuroscience, 16, 960262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditzen B, & Heinrichs M. (2014). Psychobiology of social support: the social dimension of stress buffering. Restorative Neurology and Neuroscience, 32(1), 149–162. [DOI] [PubMed] [Google Scholar]
- Dour HJ, Wiley JF, Roy-Byrne P, Stein MB, Sullivan G, Sherbourne CD, ... & Craske MG (2014). Perceived social support mediates anxiety and depressive symptom changes following primary care intervention. Depression and Anxiety, 31(5), 436–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elnitsky CA, Blevins CL, Fisher MP, & Magruder K. (2017). Military service member and veteran reintegration: A critical review and adapted ecological model. American Journal of Orthopsychiatry, 87(2), 114–128. 10.1037/ort0000244 [DOI] [PubMed] [Google Scholar]
- Förster K, Danzer L, Redlich R, Opel N, Grotegerd D, Leehr EJ, ... & Dannlowski U. (2021). Social support and hippocampal volume are negatively associated in adults with previous experience of childhood maltreatment. Journal of Psychiatry and Neuroscience, 46(3), 328–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gariepy G, Honkaniemi H, & Quesnel-Vallee A. (2016). Social support and protection from depression: systematic review of current findings in Western countries. The British Journal of Psychiatry, 209(4), 284–293. [DOI] [PubMed] [Google Scholar]
- Glynn LM, Howland MA, Sandman CA, Davis EP, Phelan M, Baram TZ, & Stern HS (2018). Prenatal maternal mood patterns predict child temperament and adolescent mental health. Journal of Affective Disorders, 228(November 2017), 83–90. 10.1016/j.jad.2017.11.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn LM, & Baram TZ (2019). The influence of unpredictable, fragmented parental signals on the developing brain. Frontiers in Neuroendocrinology, 53, 100736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn LM, Stern HS, Howland MA, Risbrough VB, Baker DG, Nievergelt CM, Baram TZ, & Davis EP (2019). Measuring novel antecedents of mental illness: the Questionnaire of Unpredictability in Childhood. Neuropsychopharmacology, 44(5), 876–882. 10.1038/s41386-018-0280-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn LM, Davis EP, Luby JL, Baram TZ, & Sandman CA (2021). A predictable home environment may protect child mental health during the COVID-19 pandemic. Neurobiology of Stress, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granger SJ, Glynn LM, Sandman CA, Small SL, Obenaus A, Keator DB, ... & Davis EP (2021). Aberrant maturation of the uncinate fasciculus follows exposure to unpredictable patterns of maternal signals. Journal of Neuroscience, 41(6), 1242–1250. 10.1523/JNEUROSCI.0374-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harandi TF, Taghinasab MM, & Nayeri TD (2017). The correlation of social support with mental health: A meta-analysis. Electronic Physician, 9(9), 5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness KL, Bruce AE, & Lumley MN (2006). The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology, 115(4), 730–741. 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Lamontagne SJ, & Cunningham S. (2021). Environmental contributions to anhedonia. Anhedonia: Preclinical, Translational, and Clinical Integration, 81–108. 10.1016/j.neubiorev.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Ho N, & Sommers M. (2013). Anhedonia: a concept analysis. Archives of Psychiatric Nursing, 27(3), 121–129. 10.1016/j.apnu.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, ... & Dunne MP (2017). The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2(8), 356–366. [DOI] [PubMed] [Google Scholar]
- Jirsaraie RJ, Palma AM, Small SL, Sandman CA, Davis EP, Baram TZ, ... & Yassa MA (2023). Prenatal Exposure to Maternal Mood Entropy is Associated with a Weakened and Inflexible Salience Network in Adolescence. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kangas BD, Short AK, Luc OT, Stern HS, Baram TZ, & Pizzagalli DA (2022). A cross-species assay demonstrates that reward responsiveness is enduringly impacted by adverse, unpredictable early-life experiences. Neuropsychopharmacology, 47(3), 767–775. 10.1038/s41386-021-01250-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, & Samper RE (2006). Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology, 18(2), 89–120. 10.1207/s15327876mp1802_1. [DOI] [Google Scholar]
- Levis SC, Birnie MT, Bolton JL, Perrone CR, Montesinos JS, Baram TZ, & Mahler SV (2022). Enduring disruption of reward and stress circuit activities by early-life adversity in male rats. Translational Psychiatry, 12(1), 251. 10.1038/s41398-022-01988-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M, O’Donnell KJ, Caron J, Meaney MJ, Kobor M, D’Arcy C, ... & Meng X. (2022). To what extent do social support and coping strategies mediate the relation between childhood maltreatment and major depressive disorder: A longitudinal community-based cohort. Development and Psychopathology, 1–12. [DOI] [PubMed] [Google Scholar]
- Lindert NG, Maxwell MY, Liu SR, Stern HS, Baram TZ, Poggi Davis E, ... & Glynn LM (2022). Exposure to unpredictability and mental health: Validation of the brief version of the Questionnaire of Unpredictability in Childhood (QUIC-5) in English and Spanish. Frontiers in Psychology, 13, 971350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maner JK, Hasty CR, Martinez JL, Ehrlich KB, & Gerend MA (2023). The role of childhood unpredictability in adult health. Journal of Behavioral Medicine, 46(3), 417–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maranges HM, Hasty CR, Maner JK, & Conway P. (2021). The behavioral ecology of moral dilemmas: Childhood unpredictability, but not harshness, predicts less deontological and utilitarian responding. Journal of Personality and Social Psychology, 120(6), 1696. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, & Gilman SE (2010). Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine, 40(10), 1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molet J, Heins K, Zhuo X, Mei YT, Regev L, Baram TZ, & Stern H. (2016). Fragmentation and high entropy of neonatal experience predict adolescent emotional outcome. Translational Psychiatry, 6(November 2015). 10.1038/tp.2015.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagrin A, Saiote C, & Schiller D. (2018). The social hippocampus. Hippocampus, 28(9), 672–679. [DOI] [PubMed] [Google Scholar]
- Noroña-Zhou AN, Morgan A, Glynn LM, Sandman CA, Baram TZ, Stern HS, & Davis EP (2020). Unpredictable maternal behavior is associated with a blunted infant cortisol response. Developmental psychobiology, 62(6), 882–888. 10.1002/dev.21964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Parker G, & Brotchie H. (2010). Gender differences in depression. International Review of Psychiatry, 22(5), 429–436. 10.3109/09540261.2010.492391. [DOI] [PubMed] [Google Scholar]
- Pereira-Morales AJ, Adan A, & Forero DA (2019). Perceived stress as a mediator of the relationship between neuroticism and depression and anxiety symptoms. Current Psychology, 38, 66–74. [Google Scholar]
- Pizzagalli DA (2014). Depression, stress, and anhedonia: toward a synthesis and integrated model. Annual Review of Clinical Psychology, 10, 393–423. 10.1.146/annurev-clinpsy-050212-185606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren M, Zou S, Ding S, & Ding D. (2022). Childhood Environmental Unpredictability and Prosocial Behavior in Adults: The Effect of Life-History Strategy and Dark Personalities. Psychology Research and Behavior Management, 1757–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risbrough V, Glynn L, Davis E, Sandman C, Obenaus A, Stern H, Keator D, Yassa M, Baram T, Baker D. (2018) Does Anhedonia Presage Increased Risk of Posttraumatic Stress Disorder? : Adolescent Anhedonia and Posttraumatic Disorders. Curr Top Behav Neurosci, 38, 249–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rousson AN, Fleming CB, & Herrenkohl TI (2020). Childhood maltreatment and later stressful life events as predictors of depression: A test of the stress sensitization hypothesis. Psychology of Violence, 10(5), 493–500. 10.1037/vio0000303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, De Girolamo G, ... & Kessler RC (2011). Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Archives of General Psychiatry, 68(8), 838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smid GE, Kleber RJ, Rademaker AR, Van Zuiden M, & Vermetten E. (2013). The role of stress sensitization in progression of posttraumatic distress following deployment. Social Psychiatry and Psychiatric Epidemiology, 48, 1743–1754. 10.1007/s00127-013-0709-8. [DOI] [PubMed] [Google Scholar]
- Solomonov N, Victoria LW, Lyons K, Phan D, Alexopoulos GS, Gunning FM, & Flückiger C. (2023). Social Reward Processing in Depressed and Healthy Individuals Across the Lifespan: A Systematic Review and a Preliminary Coordinate-based Meta-analysis of fMRI Studies. Behavioural Brain Research, 114632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spadoni AD, Vinograd M, Glynn LM, Davis EP, Baram TZ, Baker DG, Nievergelt CM, & Risbrough VB (2022). Contribution of early - life unpredictability to neuropsychiatric symptom patterns in adulthood. Depression and Anxiety, October 2021, 1–12. 10.1002/da.23277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Struck N, Krug A, Feldmann M, Yuksel D, Stein F, Schmitt S, ... & Brakemeier EL (2020). Attachment and social support mediate the association between childhood maltreatment and depressive symptoms. Journal of Affective Disorders, 273, 310–317. [DOI] [PubMed] [Google Scholar]
- Szepsenwol O, Zamir O, & Simpson JA (2019). The effect of early-life harshness and unpredictability on intimate partner violence in adulthood: A life history perspective. Journal of Social and Personal Relationships, 36(5), 1542–1556. [Google Scholar]
- Walker CD, Bath KG, Joels M, Korosi A, Larauche M, Lucassen PJ, ... & Baram TZ (2017). Chronic early life stress induced by limited bedding and nesting (LBN) material in rodents: critical considerations of methodology, outcomes and translational potential. Stress, 20(5), 421–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Ajdacic-Gross V, Müller M, Buadze A, Seifritz E, Kleim B, ... & Vandeleur CL(2022). Childhood adversity patterns differentially cluster with mental disorders and socioeconomic indicators in a large Swiss community sample. Comprehensive Psychiatry, 112, 152282. [DOI] [PubMed] [Google Scholar]
- Xu EP, Nguyen L, Leibenluft E, Stange JP, & Linke JO (2023). A meta-analysis on the uncinate fasciculus in depression. Psychological Medicine, 53(7), 2721–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.