Abstract
A case of a 32-year-old patient who presented with vaginal bleeding 2 years after undergoing laparoscopic radical trachelectomy and vaginal cerclage was noted to have Mersilene tape erosion. Subsequent management includes the removal of displaced Mersilene tape and a repeat cerclage through a new technique of laparoscopic abdominal cerclage to avoid repeat tape erosion. The novel technique of laparoscopic abdominal cerclage to lower the incidence of preterm delivery among pregnant patients who underwent laparoscopic radical trachelectomy for early-stage cervical cancer is described.
Keywords: Laparoscopic abdominal cerclage, Mersilene tape erosion, novel technique, radical trachelectomy
INTRODUCTION
Fertility-sparing surgery for early-stage cervical cancer has been practiced for more than two decades and the first radical laparoscopic radical trachelectomy for early-stage cervical cancer was performed by Lee et al.[1,2,3] Although cervical cancer is the fourth leading cause of cancer among women, the majority of cases are noted during the reproductive years. Empowered women tend to prioritize establishing their careers over early marriage and pregnancy. This situation led to the development of fertility-sparing surgery among women who were diagnosed with cancer. In the advent of regular papanicolaou smear and Human Papilloma Virus (HPV) test, patients who choose to undergo vaginal, abdominal, or laparoscopic radical trachelectomy can have a close follow-up of cervical cancer recurrence; hence, giving them the chance for future fertility. In some patients who underwent vaginal cerclage or laparoscopic abdominal cerclage after radical trachelectomy, tape erosion is one of the reported complications. We discuss a modified technique of laparoscopic transabdominal cerclage with the aim of preventing repeat Mersilene™ tape erosion in a patient who underwent laparoscopic radical trachelectomy with vaginal cerclage.
CASE REPORT
A 32-year-old nulligravid woman underwent an annual health examination 2 years before admission wherein a pap smear revealed squamous cell carcinoma. The patient underwent conization in a tertiary hospital and was diagnosed with squamous cell carcinoma of the cervix stage IB1. The patient had no regular pap smear or HPV vaccination. Since the patient is desirous of pregnancy, the consult was done with another gynecologist and underwent laparoscopic radical trachelectomy, sentinel lymph node biopsy, and vaginal cerclage. Histopathologic examination revealed: cervix, radical laparoscopic trachelectomy specimen–ulcer; vaginal, laparoscopic trachelectomy–negative for malignancy; bilateral pelvic lymph node (Indocyanine Green (ICG) positive for detection)–negative for malignancy. The patient underwent regular follow-ups until 6 months before admission, and irregular vaginal bleeding was noted prompting a consult with a gynecologist. Upon speculum examination, there was noted protrusion of 2 cm tape into the vaginal canal, as shown in Figure 1a. The patient underwent the removal of the protruded Mersilene™ tape vaginally [Figure 1b] and repair [Figure 1c].
Figure 1.
Mersilene Tape Erosion: (a) Mersilene tape erosion, (b) Removed Mersilene tape, (c) Patent internal OS after removal of vaginal cerclage
Four months after the removal of the eroded Mersilene tape, the patient was readmitted for repeat laparoscopic transabdominal cerclage [Figure 2a and b].
Figure 2.
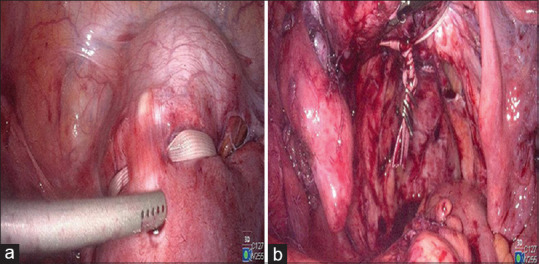
Laparoscopic abdominal cerclage: (a) Postoperative picture after laparoscopic abdominal cerclage (anterior view), (b) Postoperative Picture after laparoscopic abdominal cerclage (posterior view)
The technique in the repeat laparoscopic abdominal cerclage is described as follows: (a) A primary port is placed in the Lee-Huang Point and three accessory ports were made,[4] (b) Pelvic inspection and lysis of previous adhesions, (c) Inspection and identification of bilateral ureter, (d) Creation of bilateral broad ligament window, (e) Mersilene tape is passed thru the created right broad ligament window embedding the Mersilene tape in the anterior myometrium of the lower uterine segment and passed thru the left broad ligament window to avoid displacement and repeat erosion because of the absence of the cervico-uterine junction, (f) Both ends of the Mersilene tape are tied at the lower posterior uterine wall and secured with laparoscopic clips to avoid slippage.
In the current technique, the Mersilene tape is passed through the tunneled or dissected vesico-uterine peritoneum while in this modified technique, the Mersilene tape is embedded in the myometrium to avoid the complications of urinary bladder erosion and displacement to other surrounding pelvic structures.
The patient was discharged improved with no complications after 6 months of follow-up.
DISCUSSION
Vaginal mesh erosion is one of the reported complications of vaginal/laparoscopic placement of mesh for pelvic organ prolapse.[5] Only a few cases were reported regarding complications after vaginal or laparoscopic abdominal cerclage using Mersilene tape following radical trachelectomy.[6,7,8,9,10] Placement of foreign body such as Mersilene tape can be a risk factor for poor wound healing; hence, prone to infection which is seen in the index patient as vaginal mersilene tape erosion. Dissection of the pelvic floor spaces may contribute to the disruption of the integrity of the pelvic floor.
Placement of a laparoscopic transabdominal cerclage in patients after trachelectomy is challenging because of the absence of the cervico-uterine junction.[11] In this case, since the patient had previous cerclage placed vaginally during laparoscopic radical trachelectomy that resulted in a cerclage erosion, the surgeon opted to embed the Mersilene tape in the anterior myometrium of the neo-cervix or lower uterine segment, avoiding slippage, and possible erosion. Obstetric outcomes of patients who underwent radical trachelectomy include preterm prelabor rupture of membrane, preterm delivery, and spontaneous abortion.[6]
Mersilene tape erosion among patients who underwent cerclage after laparoscopic radical trachelectomy is rare but can cause additional psychological stress to patients. Determining the appropriate and standardized technique of laparoscopic abdominal cerclage among postradical trachelectomy patients is challenging but necessary to avoid repeat cerclage erosion and to attain improved obstetrical outcomes.[12,13]
Most published literature regarding placement of vaginal or abdominal cerclage focuses on the pregnancy outcome as well as complications but rare to find published literature on the prevention of tape complications such as erosion. Long-term follow-up as to the outcome of this modified technique is highly suggested.
Author contributions
JSP and KGH: Involved in concept, design, manuscript preparation, manuscript editing. CLL: Involved in concept, design, manuscript preparation, manuscript editing. GPG, MEM, and ZML: Involved in design, and manuscript preparation
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Financial support and sponsorship
Nil.
Conflicts of interest
This study was financially supported by Prof. Chyi-Long Lee, Editor-in-Chief of Gynecology and Minimally Invasive Therapy, had no role in the peer-review process or decision to publish this article. The other authors declared no conflicts of interest in writing this paper.
Acknowledgment
The authors, namely JP, GPG, and MEM would like to thank Professor Kuan-Gen Huang and Professor Chyi-Long Lee for their mentorship.
REFERENCES
- 1.Lee CL, Huang KG, Wang CJ, Yen CF, Lai CH. Laparoscopic radical trachelectomy for stage Ib1 cervical cancer. J Am Assoc Gynecol Laparosc. 2003;10:111–5. doi: 10.1016/s1074-3804(05)60244-7. [DOI] [PubMed] [Google Scholar]
- 2.Lee CL, Huang KG. Prospect of laparoscopy in treating early-stage cervical cancer. Taiwan J Obstet Gynecol. 2004;43:5–9. [Google Scholar]
- 3.Yang FC, Huang W, Yang W, Liu J, Ai G, Luo N, et al. Cervical cancer surgery: Current state of affairs. Gynecol Minim Invasive Ther. 2021;10:75–83. doi: 10.4103/GMIT.GMIT_81_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thepsuwan J, Huang KG, Wilamarta M, Adlan AS, Manvelyan V, Lee CL. Principles of safe abdominal entry in laparoscopic gynecologic surgery. Gynecol Minim Invasive Ther. 2013;2:105–9. [Google Scholar]
- 5.Jaili SB, Lo TS, Wijaya T, Wu PY. Intravesical midurethral sling mesh erosion secondary to transvaginal mesh reconstructive surgery. Gynecol Minim Invasive Ther. 2015;4:41–3. [Google Scholar]
- 6.Burger NB, Abdulrahman N, DE Boer MA, Fons G, Huirne JA. Cerclage related complications after trachelectomy: A retrospective case series. Arch Obstet Gynecol. 2021;2:64–75. [Google Scholar]
- 7.Xu J, Wang L, Yang W, Zhang Y. Intravesical invasion of a mersilene tape and secondary stone formation. Int Urogynecol J. 2019;30:1775–7. doi: 10.1007/s00192-019-03971-4. [DOI] [PubMed] [Google Scholar]
- 8.Alani S, Wang J, Suarthana E, Tulandi T. Complications associated with cervical cerclage: A systematic review. Gynecol Minim Invasive Ther. 2023;12:4–9. doi: 10.4103/gmit.gmit_61_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alas QM, Lee CL, Kuo HH, Huang CY, Yen CF. Interval laparoscopic transabdominal cervical cerclage (ILTACC) using needleless mersilene tape for cervical incompetence. Gynecol Minim Invasive Ther. 2020;9:145–9. doi: 10.4103/GMIT.GMIT_90_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tulandi T, Eiley D, Abenhaim H, Ziegler C. Complete erosion of abdominal cerclage into the bladder. J Obstet Gynaecol Can. 2021;43:1083–5. doi: 10.1016/j.jogc.2021.03.017. [DOI] [PubMed] [Google Scholar]
- 11.Shibata RK, Waters CH, Nimaroff ML. Laparoscopic abdominal cerclage after prior radical trachelectomy. J Minim Invasive Gynecol. 2022;29:S53–4. [Google Scholar]
- 12.Lee CL, Huang KG, Chua PT, Mendoza MC, Lee PS, Lai SY. Standardization and experience may influence the survival of laparoscopic radical hysterectomy for cervical cancer. Taiwan J Obstet Gynecol. 2021;60:463–7. doi: 10.1016/j.tjog.2021.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Lee CL. Minimally invasive therapy for cancer: It is time to take actions for training system in minimally invasive therapy after LACC report. Gynecol Minim Invasive Ther. 2019;8:1–3. doi: 10.4103/GMIT.GMIT_132_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.



