Surgeons, or rather male surgeons, are always addressed as Mr in the United Kingdom and the Republic of Ireland, sometimes but not always in Australia and New Zealand, and rarely in Canada or the United States. This curious British tradition is such a mystery to doctors in other countries as well as to the British public, that even a work as erudite as the 1996 edition of The New Fowler's Modern English Usage seems to have got it wrong.1 Is it therefore a tradition that should be perpetuated indefinitely, or should it be abandoned?
To understand how the tradition arose it is necessary to go back to the beginning of the 18th century, when physicians were distinguished by the possession of a university medical degree: an MD. Although many had acquired their MDs abroad with minimal effort or bought them for about £20 (about £800 today) from the Universy of Aberdeen or of St Andrews, the possession of a medical doctorate entitled physicians and no other medical practitioner to be addressed as “doctor.” Eighteenth century surgeons, who were of course addressed as Mr, seldom had any formal qualification except in the case of the few who were Members of the Company of Surgeons. After the founding of the Royal College of Surgeons of London in 1800, however, it was customary for surgeons to take the examination for Membership of the Royal College of Surgeons and put MRCS after their name.2
Summary points
(Male) surgeons are always addressed as Mr in the United Kingdom and the Republic of Ireland
The tradition arose before 1800 when physicians were by definition doctors who possessed a university medical degree (an MD); surgeons seldom had any formal qualifications
The growth of voluntary hospitals in the 18th century brought high status to surgeons
After the founding of the Royal College of Surgeons of London in 1800, surgeons had a formal qualification (the MRCS)
Surgeons became so proud to be distinguished from physicians that the title of Mr became a badge of honour
Physicians were gentlemen with a university education who dealt with internal diseases, arrived at a diagnosis on the basis of the history and external appearance of the patient, and prescribed in Latin. In theory, but seldom in practice, their supposedly superior knowledge gave them a monopoly over the practice of physic and the authority to supervise the work of surgeons.2 It was the extraordinarily rapid growth of the number of voluntary hospitals between the 1730s and 1800 that brought this hierarchical division to an end. It is only a slight oversimplification to say that because of the rules regarding medical admissions medicine stagnated and surgery leapt ahead within the new world of these hospitals. The brilliant work of men such as John Hunter (1728-93), of whom a contemporary said that he had “made gentlemen of us all,” highlights the rapid advance in the status of surgery so that John Abernethy (1764-1837), honorary surgeon at St Bartholomew's Hospital, was able to say in 1812:
There was a time when surgeons were considered as mere appendages of physicians, the mere operators to be put in motion by their directors: but times have changed and surgeons are changed too . . . and in consequence have got a kind of information which puts them on a par with others of the profession.3
Some of his colleagues went further, claiming that surgery was actually superior to medicine. G J Guthrie, president of the Royal College of Surgeons (PRCS), (1785-1856) told a parliamentary select committee in 1834 that “Surgery in Great Britain is at the highest point of elevation of surgery in any part of Europe.”4 This is just one indication of the striking self confidence of the surgeons at the London teaching hospitals who by the early years of the 19th century were earning the highest medical incomes and saw themselves as being at the very top of the medical tree. Surgeons had become so pleased with themselves that being addressed as Mr ceased to be a put-down and became a badge of honour and distinction. Although surgeons in 1730 had no right to be called Dr, hospital surgeons in 1830 had no wish to be.
But the situation was complicated by the rapid rise of the 18th century general practitioner in the form of the surgeon-apothecary or, as they were soon to be called, the general practitioner. The Apothecaries' Act of 1815 made it compulsory for all new entrants to general practice to acquire the Licence of the Society of Apothecaries (LSA). A large majority of general practitioners, however, also acquired the MRCS so that the dual qualification MRCS LSA, known colloquially as the “College and Hall” (that is, the college of surgeons and the licence granted at Apothecaries' Hall), was the hallmark of the general practitioner who was qualified to practise surgery as well as physic, midwifery, and pharmacy.5,6 It was not until 1884 that the Licence of the Royal College of Physicians (LRCP) was joined with the MRCS to form the “conjoint” qualification for general practitioners, thereby liberating them from the “degrading connection with the Society of Apothecaries.”7
FRCS: hallmark of the pure surgeon
After 1815, however, when for the first time it had become customary for all orthodox medical practitioners to have a formal qualification and letters after their name, it was galling for the elite hospital surgeons to have the same qualification (MRCS) as the general practitioners who, to make matters worse, often called themselves surgeons. The elite's reaction was to create a new, unofficial category of “pure surgeons” who differed from the general practitioner with an MRCS not only by possessing greater surgical skill and an appointment at a hospital but also on the negative grounds that under no circumstances would a pure surgeon dispense drugs or practise midwifery. Out of 8000 practitioners who held the MRCS in 1834 there were just 200 “pure surgeons,” almost all in London.8 Only the latter were eligible for election to council and allowed to use the front door of their college: the general practitioners with an MRCS had to go round to the back. When a new charter in 1843 changed the Royal College of Surgeons of London into the Royal College of Surgeons of England, the opportunity was taken to introduce the rank of fellow (FRCS), which became the hallmark of the pure surgeon and was firmly linked to the convention of addressing surgeons as Mr.2
The other problem with Mr and Dr was midwifery, which was outlawed by members of the Council of the Royal College of Surgeons. Thus, from the late 18th century to the late 19th century almost all of the growing number of obstetricians appointed to teaching hospitals were physicians. Indeed, most were Fellows of the Royal College of Physicians, called themselves “physician-accoucheurs,” and were addressed as Dr.9 Conflict arose at the end of the 19th century, however, with the growth of operative gynaecology. This is a complex story, but the root of it is the argument made by surgeons that gynaecology belonged to them because it was operative; the physician-accoucheurs claimed that obstetrics and gynaecology belonged together. As we know, the surgeons won the argument. By the 20th century the obstetrician-gynaecologist (who often, but not necessarily, possessed the FRCS) became another kind of doctor who was always addressed as Mr. And this is more or less the position today; but is the persistence of this tradition sensible?
Fifty years ago it was relatively simple. Physicians treated medical diseases and surgeons operated. Today, the treatment of surgical disorders is often undertaken by teams of doctors any of whom may “intervene” in a technical or surgical manner (the interventional radiologists are an example), whether they are titled Dr or Mr, Miss, Mrs, or Ms. Thus patients with cancer who happen to be sticklers for addressing people correctly may well be puzzled when they are referred by Dr A, their general practitioner, to Dr B, an oncologist, and Dr C, a radiologist, before seeing Mr or Ms D, a surgeon. An operation is performed under an anaesthetic administered by Dr E after which the patient is referred to Dr F for radiotherapy and back to Dr B for chemotherapy depending, perhaps, on the findings of a pathologist, Dr G. Further, the patient may enter a controlled trial run by a medical statistician, Dr H, who is not medically qualified but has a PhD.
That is eight “Drs” to one “Mr (or Miss or Mrs or Ms).” Note that any of these doctors, including Mr B, might possess an MD or a DM, which often puzzles American doctors who are not always aware that in the United Kingdom these are postgraduate degrees. But whether or not they have been awarded a university doctorate (an MD, DM, DPhil, or PhD) is irrelevant to how they are addressed. Only the surgeon is addressed as Mr (or Miss or Mrs or Ms), together with his or her registrar; but the house surgeon is not, for it is (or used to be) considered bad form if Dr John Jones who was a house physician yesterday insists on being called Mr Jones when taking up the house surgeon post tomorrow.
Medical qualifications in the United Kingdom have been in an unholy muddle ever since the Medical Act of 1858 when no less than 18 independent medical institutions offered a range of bachelorships, licences, diplomas, memberships, fellowships, and doctorates all officially recognised by the General Medical Council. This cannot be altered. Now, however, so much of surgery is teamwork that it seems to me that the original and rather trivial reasons for “mistering” surgeons have disappeared. Would surgeons be willing to abandon this pretentious anachronism so that all who possess a medical qualification that is recognised by the General Medical Council, regardless of the specialty and the letters after their name, are simply addressed as Dr? It is at least worth considering.
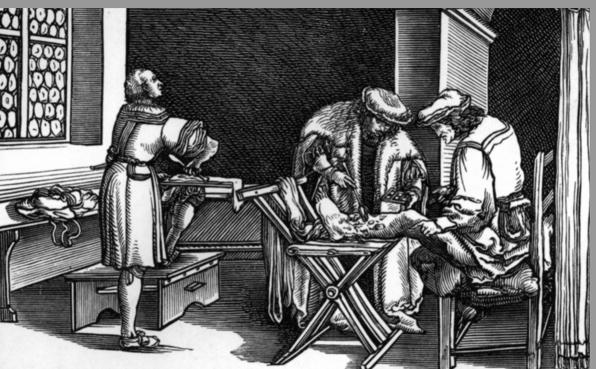
Figure.
Before the 18th century, surgeons seldom had any formal qualifications
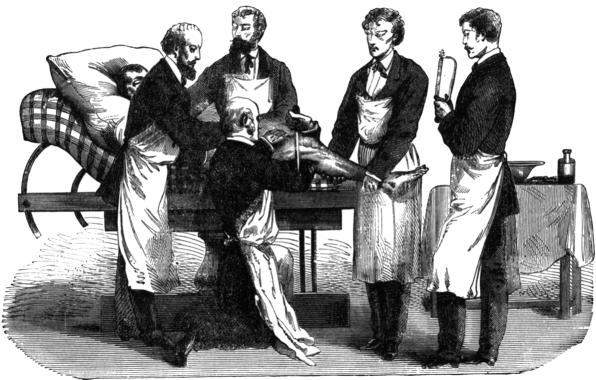
Figure.
After the founding of the Royal College of Surgeons of London in 1800, surgeons could be MRCS
Footnotes
Competing interests: None declared.
References
- 1.Aronson J. Modern English abusage. BMJ. 2000;320:357. doi: 10.1136/bmj.320.7231.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cope Z. The Royal College of Surgeons of England: a history. London: Anthony Blond; 1959. [Google Scholar]
- 3.Royal Society of Medicine London. The notebooks of John Greene Crosse of Norwich. MS. 1812. p. 285. :g.11. (Manuscript collection.) [Google Scholar]
- 4.Report of the Select Committee on Medical Education. Evidence of G J Guthrie, PRCS. Parliamentary Papers 1834;XIII (part 2):Q.4842.
- 5.Loudon I. Medical care and the general practitioner, 1750-1850. Oxford: Clarendon Press; 1986. pp. 152–170. [Google Scholar]
- 6.Loudon I. Medical education and medical reform. In: Nutton V, Porter R, editors. The history of medical education in Britain. Amsterdam: Rodopi; 1995. pp. 229–249. [Google Scholar]
- 7.Cooke AM. A History of the Royal College of Physicians. Vol. 3. Oxford: Clarendon Press; 1972. pp. 844–860. [Google Scholar]
- 8.Report of the Select Committee on Medical Education. Evidence of G J Guthrie, PRCS. Parliamentary Papers 1834;XIII (part 2):Q.4731.
- 9.Loudon I. Death in childbirth: an international study of maternal care and maternal mortality, 1750-1850. Oxford: Clarendon Press; 1992. p. 183. [Google Scholar]