Abstract
Sleeping problems are prevalent among children and adolescents, often leading to frequent consultations with pediatricians. While cognitive-behavioral therapy has shown effectiveness, especially in the short term, there is a lack of globally endorsed guidelines for the use of pharmaceuticals or over-the-counter remedies in managing sleep onset insomnia. An expert panel of pediatric sleep specialists and chronobiologists met in October 2023 to develop practical recommendations for pediatricians on the management of sleep onset insomnia in typically developing children. When sleep onset insomnia is present in otherwise healthy children, the management should follow a stepwise approach. Practical sleep hygiene indications and adaptive bedtime routine, followed by behavioral therapies, must be the first step. When these measures are not effective, low-dose melatonin, administered 30–60 min before bedtime, might be helpful in children over 2 years old. Melatonin use should be monitored by pediatricians to evaluate the efficacy as well as the presence of adverse effects.
Conclusion: Low-dose melatonin is a useful strategy for managing sleep onset insomnia in healthy children who have not improved or have responded insufficiently to sleep hygiene and behavioral interventions.
|
What is Known: • Pediatric insomnia is a common disorder and impacts children's emotional, behavioral, and cognitive functioning, as well as parents' sleep and daytime functioning. • There is no consensus in Europe on the management of sleep onset insomnia and the use of melatonin in typically developing children. | |
|
What is New: • A group of European experts has compiled a set of recommendations for the management of insomnia, developing a step-by-step approach. • Sleep hygiene, behavioral strategies, and finally low-dose melatonin represent valid strategies for managing sleep onset insomnia. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-024-05556-w.
Keywords: Insomnia, Melatonin, Children, Adolescents, Pediatricians
Introduction and problem statement
Sleep disorders are very common in children and adolescents and represent a frequent reason for pediatric consultation [1]. Although a relatively small number of children suffer from intrinsic sleep disorders that require specialist medical care (such as sleep apnea, restless legs syndrome, or narcolepsy) and in a more considerable number of cases sleep problems occur in children suffering from chronic health conditions or mental distress (e.g., depression and anxiety), most children experience insomnia and problems falling asleep linked to chronic insomnia, evening chronotype, and circadian misalignment during changes in daily routine, schedule, or stressful situations such as exams and competitions. These situations might be difficult to manage since most pediatricians and nurse practitioners are not trained about behavioral sleep problems [2, 3].
The International Classification of Sleep Disorders, ICSD-3 [4] has included the “paediatric insomnia” into a single entity of the chronic insomnia disorder; however, it still includes three subtypes: sleep-onset association insomnia, limit-setting insomnia, and a combined type.
The chronic insomnia disorder may be diagnosed as early as 6 months of age, and its occurrence in the first years of life is very high. In European countries, the prevalence of pediatric insomnia is estimated to be around 15–30% in toddlers (3–5 years), 11–15% in school age (6–12 years), and 20–30% in adolescents [5, 6]. These percentages are quite alarming if we consider the consequences of insufficient sleep in these particularly vulnerable age groups. Insufficient sleep could be the result of inadequate sleep duration, poor sleep quality, or both [7]. Sleep quality refers to the subjective indices of how sleep is experienced including the feeling of being rested when waking up and satisfaction with sleep [8], but this feeling is not reliably reported by children [9, 10]. While the impact of sleep quality on children functioning seems to be more important than that of sleep quantity [8], there is little research that focuses specifically on the quality of sleep in children, due to their limited expressive capacity and the difficulty to perform polysomnography in children suffering from insomnia.
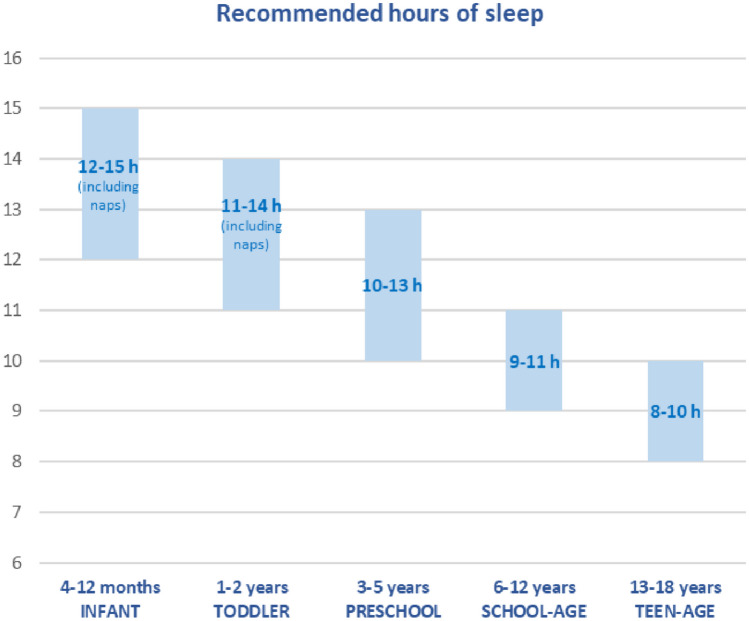
Figure 1 shows the recommendations developed by the National Sleep Foundation for sleep duration within a 24-h cycle for children and adolescents [11]. Even 30–60 min less of sleep per night significantly reduces children’s health-related quality of life [12] and impacts children’s emotional, behavioral, and cognitive functioning [13]. Insomnia has an impact on brain activity and connectivity, resulting in a wide range of disruptions in human cognition and affect [14]. This seems especially valid for insomnia that persists from childhood to adolescence [15], which seems to happen in 56% of cases [16]. The peak period of incidence of insomnia in childhood constitutes, in fact, a period of particular susceptibility of the prefrontal cortex, responsible for executive functioning and regulatory behavior. Besides poor sleep, other factors such as mental health, stress, and abuse might have detrimental effects on the prefrontal cortex, affecting the development of executive functioning and regulatory behavior, with important long-term implications [17–19].
Fig. 1.
Hours of sleep for children and adolescents recommended by the National Sleep Foundation.
Modified from Hirshkowitz et al. [11]
The effects of inadequate sleep and poor sleep quality can therefore extend from impaired neurocognitive development, expressed by thought problems and difficulties in crystallized intelligence, to behavioral and emotional problems, as externalizing behaviors, depression, and anxiety [16, 20, 21]. Clearly, insufficient sleep may be both a cause and a consequence of psychopathologic conditions; this is confirmed by the fact that sleep disorders in adolescence have been bidirectionally linked to mental health problems, leading to a vicious unhealthy circle [22].
Poor sleep impacts not only mental health and cognitive functions already in the first years of life [23] but also children’s global health. In adolescents, insufficient sleep duration has been associated with higher blood pressure [24], insulin resistance [25], obesity [26], and increased cardiometabolic risk [27]. In children, it has been linked with excessive screen time, unhealthy dietary habits, and obesity [28, 29].
The effects of a child’s disturbed sleep do not only affect physical and psychosocial health but expand to the whole family’s functioning and well-being [30, 31]. Sleep problems in children and adolescents are associated with poor sleep quality, stress, fatigue, and reduced physical health in parents [30, 32]. Insomnia in children is also associated with an increased risk of infant/child abuse by exhausted parents [33–36]. Reciprocal relations between marital or familiar conflict and sleep disruptions in children and adolescents have been highlighted [37, 38].
The management and treatment of sleep problems in childhood and adolescence are therefore fundamental, as it may lead to an improvement not only in the child/adolescent’s sleep but also in the parents’ sleep and daytime functioning.
Cognitive behavioral therapy for insomnia (CBT-I) is the first-line treatment for adults, and existing studies show promising effects also for children and adolescents [39]. Although there is considerable evidence of the effectiveness of CBT-I, at least in the short term, there are currently no internationally approved recommendations for the pharmacological or over-the-counter (OTC) management of sleep onset or sleep maintenance insomnia in children.
Study findings indicate developmental shifts in the prevalence of sleep behaviors and sleep problems, as well as how caregivers characterize sleep problems by child’s age. Waking overnight is the most common sleep behavior during infancy and early childhood, reflecting normative patterns of child sleep consolidation. Waking overnight decreases with age and after the age of 4 years, the main complaint is the difficulty sleeping independently and namely sleep onset insomnia [40]. These problems correspond with manifestations of insomnia disorder in early development, including problematic sleep onset associations (e.g., feeding or parental presence at bedtime) and the common emergence of nighttime fears and bedtime refusal in early childhood. Unlike in earlier development, difficulty falling asleep is more prevalent between ages 6 and 11 years [40]. Based on this evidence, the more prevalent problem in preschool and school children is the sleep onset insomnia.
The role of melatonin in management of sleep onset insomnia in children
Melatonin is an endogenous hormone, primarily synthesized by the pineal gland at night. Its rhythmic secretion is regulated by the circadian clock located in the suprachiasmatic nucleus in the hypothalamus which is influenced by the daily alternation of darkness and light. It is also influenced by numerous signals originating from various sources and brain structures [41], and it is strongly inhibited by light, even at relatively low intensities [42, 43]. Through its chronobiological effect, melatonin plays a key role in regulating the sleep–wake cycle, but it also has antioxidant, anti-inflammatory, and free radical scavenging properties [44]. The effect of melatonin on sleep is believed to be a consequence of its actions on MT2 and MT1 receptors, which are involved in NREM and REM sleep, respectively [45].
Melatonin is considered a “dietary supplement” by the FDA and a “natural health product” by the Health Products and Food Branch in Canada [46]. Low doses are also considered food supplement in most of the European countries [47]. In the United States, melatonin is the second most commonly used product among all children evaluated in a US National Health Interview Survey [48]. Caregivers commonly associate melatonin with “naturalness” and “safety,” and for many of them, melatonin treatment is a “life-saver” and “like a miracle”, “chang[ing] the life of the entire family” [49].
Although there are several data from scientific literature [50, 51] on the efficacy and safety of long-term melatonin for insomnia in children and adolescents with neurodevelopmental disorders, few data are available in the typically developing pediatric population. A recent systematic review and meta-analysis on melatonin use in children with idiopathic chronic sleep onset insomnia [52] found a moderate increase in total sleep time of 30 min and a moderate decrease in sleep latency of 18 min. The studies reviewed did not provide information on serious adverse events associated with melatonin use; there were only non-serious adverse events, such as headaches, nausea, red eyes, drowsiness, changes in mood and cognition, and gastrointestinal problems. Another recent systematic review on short-term and long-term adverse effects of melatonin in children and adolescents with chronic insomnia [53] found that melatonin treatment was not associated with serious adverse events and reported some level of uncertainty regarding the extent to which melatonin leads to non-serious adverse events. A recent meta-analysis study showed that in non-comorbid insomnia and comorbid insomnia melatonin had a significant effect on sleep onset latency and total sleep time in the children and adolescents group [54].
Although there are no internationally accepted guidelines on use of melatonin in normally developing children with sleep onset insomnia, management algorithms have been developed and published independently by experts in Canada [55] and Spain [56], along with a consensus paper produced during a conference in Rome [57] and a clinical recommendation based on systematic review and meta-analysis [52]. All these recommendations are very similar in the steps for treating sleep onset insomnia: the Canadian one includes sleep hygiene as first step and CBT-I with or without melatonin as second step [55]; the Spanish one suggests sleep hygiene and CBT-I as first step then addition of melatonin [56]; the consensus in Rome suggested to use melatonin as sleep inducer or chronobiotic [57]; the systematic review provided no algorithms but formulated the recommendation for melatonin only if sleep hygiene and non-pharmacological interventions have proven inadequate [52].
While recommendations from previous studies were directed to non-European countries, single European country, or to all pediatric population (typically developed children and not), this paper aims to support European primary care pediatricians in their clinical practice summarizing the views expressed by European experts in a recent Consensus Panel meeting, convened in October 2023, on the management of sleep onset insomnia and the use of melatonin in normally developing children.
Methods
Selection of the experts
To identify potential experts, an initial literature review was conducted to identify European key researchers, practitioners, and thought leaders in the field. Additionally, recommendations were sought from reputable organizations and professional networks related to the study’s topic. These sources provided a pool of candidates who were considered for inclusion in the expert panel. The selection process involved multiple stages. Initially, around 20 identified experts were invited to participate based on their expertise and contributions in the field. They were asked to submit their credentials, including their educational background, professional experience, and relevant publications. Once the initial pool of potential experts was established, a selection committee, comprising individuals with expertise in the subject matter and research methodology, reviewed the credentials of each candidate. The committee assessed their expertise, experience, and diversity in terms of geographical location and professional background. The aim was to ensure a balanced representation of perspectives and to minimize bias. Following the committee’s evaluation, the final panel of experts was selected. Invitations were sent to the chosen experts.
Nominal group technique
For the purpose of the study, we used the nominal group technique (NGT) that is a structured method for group brainstorming that consists of 5 steps: (1) introduction, (2) silent idea generation, (3) idea sharing, (4) group discussion, and (5) voting. The nominal group technique can be used by small groups to reach consensus on the identification of key problems or in the development of solutions that can be tested using rapid-change cycles.
Before, the meeting the group leader (O.B) sent a document that clarified the objective of the meeting and outlined individual roles and the voting method. Each participant was asked to collect and read the main important papers on the melatonin use in typically developing children, with the priority for topical and systematic reviews and meta-analysis. Specific questions for the purpose of the meeting were prepared and presented by the group leader. During the meeting, the group leader welcomed the participants and explained to them the purpose and procedure of the meeting. After step 2, the group leader collected the different ideas and opinions of the participants on the role of melatonin in typically developing children and shared with the others. The group discussion was devoted to the clarification of any disagreements recording the differences of opinion of the participants. The group leader finally assembled the statements and asked the participants to vote or rank. Based on the votes, a final consensus was reached.
Recommendations
Sleep problems are frequently underreported by parents if the issue does not create significant negative consequences on family functioning. Sleep and circadian rhythmicity should be assessed by primary care pediatricians during the periodic child health visit, as recommended also by the American Academy of Pediatrics [58]. A thorough assessment by pediatricians should encompass an examination of the child’s current sleep patterns, typical daytime and nighttime sleep duration and its regularity/variability, sleep/wake schedule (timing of sleep within the 24-h day and its regularity/variability), evening routines prior to bedtime, and daytime symptoms (sleepiness, alertness level, behavioral disturbances, etc.).
It is important to check that the child’s sleep duration respects the recommendations exposed in Fig. 1 [11] and to ensure that the quality of sleep is adequate by asking questions about daytime functioning and sleepiness and about subjective assessment of “good” or “poor” sleep and investigating the presence of any abnormal behavior during the night (e.g., excessive movements, bruxism, snoring, open mouth breathing, night terrors, and enuresis).
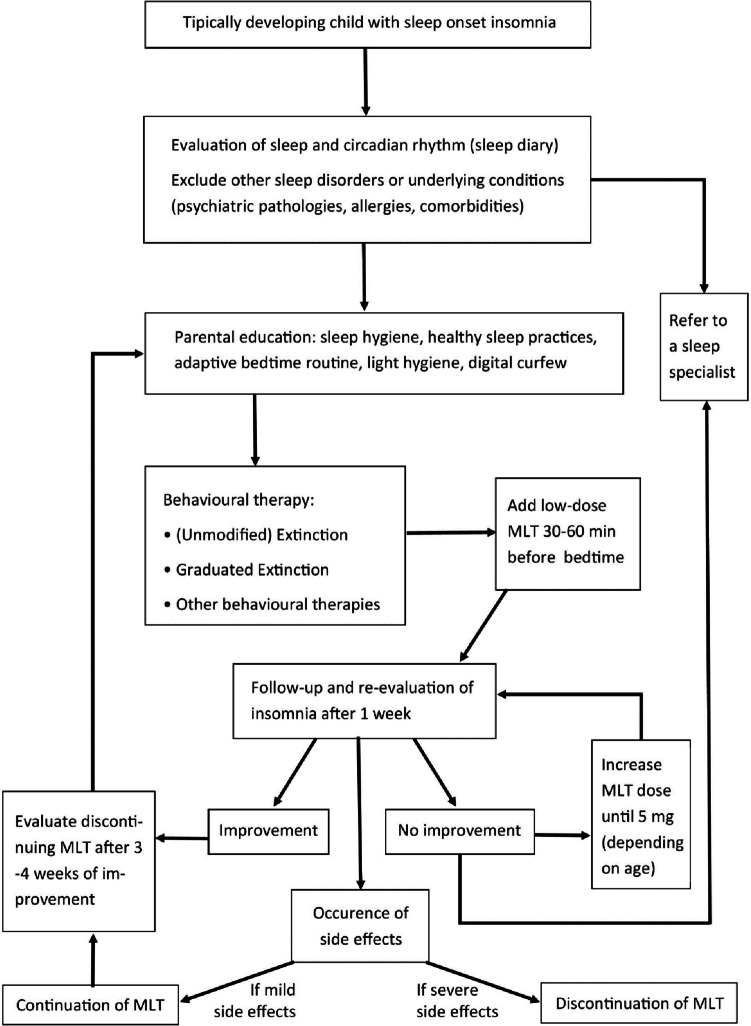
When the sleep problem occurs in comorbidity with other health problems (chronic diseases, psychiatric, or neurological disorders), comorbidity should be assessed and treated separately. When sleep onset insomnia is present in otherwise healthy children, the management should follow a stepwise approach. A simple flowchart is exposed in Fig. 2. The first step should be a comprehensive evaluation of the child’s sleep pattern, sleeping arrangement, bedtime routine, and parental behaviors and responses to the child both at bedtime and after night waking. This is often best achieved using a sleep diary, where parents record the child’s daily sleep behaviors over an extended period of time (usually around 2 weeks).
Fig. 2.
Flowchart for management of sleep onset insomnia. MLT, melatonin
Pediatricians should inquire about the presence of other sleep disorders (e.g., sleep apnea, narcolepsy, or restless legs syndrome); if suspected, they should request a consultation with a sleep specialist. Furthermore, if there are other underlying conditions that can explain the sleep problem, such as allergies, comorbidities, and potential factors causing pain (e.g., ear infections and reflux), or psychiatric diseases, the healthcare provider should treat the underlying condition or, if necessary, request a consultation with a specialist. After having excluded other possible causes of sleep onset insomnia, pediatricians should manage the problem through parental education on sleep hygiene, healthy sleep practices, and adaptive bedtime routines. Practical sleep hygiene indications to be given to parents are reported in Table 1. Since the role of circadian synchronization is crucial, particular attention should be given to light exposure. Daily sunlight/natural exposure, especially in the morning but also throughout the entire day, and a lowering of light intensity before bedtime permit the proper synchronization of the circadian clock and favor a quicker sleep onset after bedtime. Bedroom should be free from screens and bright light sources, and a “digital curfew” should be observed at least 1–2 h before bedtime (no electronics/screens). If a child requests a nightlight, choose a low light intensity and orange/red light and place it as far as possible from the head of the bed.
Table 1.
Practical sleep hygiene advices
| - Respect the recommended sleep duration for age |
|---|
| - Promote exposure to natural light (sunlight) and physical activity during the day, it helps circadian synchronization |
| - Remove screens or other light sources in the bedroom before bedtime, if the child requests a nightlight, choose a low light intensity and orange/red light |
| - Turn off screens 1–2 h before bedtime (digital curfew) |
| - Create an adaptive bedtime routine, tailored to the individual child and family |
| - Put the child to bed when he/she is still awake and then leave the child’s bedroom |
| - Promote stability of the sleep/wake cycle during the week and maintain similar sleep/wake times and bedtime routines on weekdays and weekends |
| - After a specific age ranging from 3 to 5 years, limit naps early in the afternoon to allow adequate sleep pressure to accumulate by bedtime |
| - Pay attention to a diet that promotes sleep (prefer a Mediterranean diet; avoid soft drinks, fast food, and snacks instead of meals; and do not skip breakfast) |
| - Daytime exercise promotes sleep but not too close to bedtime (no exercise within the last 2 h before bedtime) |
Attention should also be paid to children’s diet. Following a Mediterranean diet and consuming foods abundant in fiber, fruits, vegetables, and anti-inflammatory nutrients, while minimizing intake of saturated fats, appears to enhance the quality of sleep [59]. Even in toddlers, an increased intake of soft drinks, snacks, and fast foods is linked to shorter, more fragmented sleep patterns, while higher consumption of vegetables is correlated with a more stable sleep [60]. Skipping breakfast, consuming late-night snacks, or substituting meals with snacks are linked to lower overall sleep quality in students [61, 62].
Creating an adaptive bedtime routine should always be recommended as a key factor in the promotion of not only healthy sleep but also of child development and well-being as well as family functioning and caregiver–child bonding [63]. Adaptive bedtime routine includes several activities (such as reading, singing/lullabies, quiet games, bathing and/or brushing teeth, massaging, and cuddling) before lights out. Choosing adaptive bedtime activities, tailored to the individual child and family and to the cultural environment, can promote nurturing care [63] and help the child relax and feel ready for sleep. Many families have a bedtime routine but find difficulties in using it regularly or in having the same bedtime routine on weekdays and weekends [64, 65]. Stability in bedtime routines and sleep/wake time is important to ensure consolidation of sleep/wake rhythmicity and sleep quality [66]. As a conclusion of the bedtime routine, parents should put the child to bed when he/she is still awake, briefly comfort the child, turn the lights out, and leave the child’s bedroom. Worse sleep patterns (reduced night sleep duration and night awakenings) have been associated to the presence of parents while the child is falling asleep, especially if there is active physical comforting [67–69] It is important to promote the development of independence and self-regulation at bedtime and during night awakenings. To help the child to self-sooth, few familiar objects can be placed in child’s bed (avoiding plushies or dangerous objects) [70].
When sleep hygiene and changes in bedtime routines are inefficient, behavioral therapies are recommended. The most used behavioral therapies are unmodified and graduated extinction. Although effective, parental resistance remains the biggest obstacle to these approaches, most of them find extinction too difficult and stressful to implement [71], perhaps due to low parental cry tolerance and high infant distress-attribution cognitions [72]. When behavioral therapies alone are not resolutive or there is parental resistance in implementing them, low-dosage melatonin could be used in combination. Melatonin supplementation can be administered starting with a minimal dose of 0.5 mg, 30–60 min before desired bedtime. Parents should be informed regarding potential adverse events of melatonin use and lack of long-term safety data. They should also be advised to consult with a healthcare professional before using melatonin in children and not use for longer than 14 days without doctor’s recommendation. The bedtime should ensure the recommended sleep duration for the child and therefore depend on his/her age; timing should not be based on the wishes of the child or the parents. In case melatonin is inefficient after 1 week, dosage can be increased step-by-step/gradually, by 0.5 mg at a time, for a week, up to 5 mg, depending on age. Based on the different consensus in the literature, it seems reasonable to consider a dosage of 0.5 to 1 mg in infants 1 to 3 years of age; 1–2 mg in preschoolers, up to 3 mg in school-age children and up to 5 mg in adolescents [52, 55–57]. When a dose is effective, it is recommended to try a lower dose. If side effects occur, it is indicated to discontinue the administration. Although it has been reported that children who use melatonin are likely to experience non-serious adverse events, pediatricians should be aware that common side effects include headache, nausea, red cheeks, red earlobes, sore/red eyes, fatigue/drowsiness, dizziness, vomiting, influenza symptoms/infections, change in mood/cognition, musculoskeletal pain, and gastrointestinal problems [53]. The use of melatonin should not replace general good sleep practices in terms of sleep routines and good sleep hygiene. If using melatonin, importance must be given to circadian synchronization and light exposure, since the effects of light are stronger than that of melatonin on the circadian system and sleep: reduced light exposure and digital curfew are essential before bedtime. Melatonin should be used for 3–4 weeks to stabilize sleep timing and duration, along with continuous sleep hygiene and behavioral corrections; then, it is suggested to suspend it. In rare cases when these techniques do not help, referral to a sleep specialist may be considered. Also, occasional melatonin use (even for a few days) may be beneficial to help in special occasions like changes in the normal routine, flights, and return from vacation, in order to rapidly normalize the sleep–wake pattern.
While there is a wide array of products available, it is crucial to prioritize melatonin sourced from manufacturers with established, high-quality manufacturing standards. A study examining 31 melatonin-containing products and supplements from the US market and not in European market revealed considerable variability in melatonin content, ranging from − 83% to + 478% of the labeled amount. Additionally, 26% of the tested products in the US market contained serotonin, a biosynthetic precursor of melatonin and neurotransmitter associated with various neurological disorders [73]. It is also of utmost importance that the food supplements for children come in the packaging with child-resistant closure to avoid the risk of accidental exposure. Considerate manufacturers of food supplements must also have diligent post-marketing adverse events monitoring system [74].
Expert advices
An expert panel of pediatric sleep specialists and chronobiologists elaborated a consensus on the use of melatonin in otherwise healthy children.
Although no specific data are available on the safety of melatonin use in otherwise healthy children or children with neurodevelopmental disabilities under 2 years of age, some evidence showed the efficacy and safety of melatonin in older children and adolescents with sleep onset insomnia or delayed sleep phase syndrome [70, 75–77].
Advise parents or caregivers on sleep hygiene measures (including light hygiene, nutrition, and digital curfew measures) and behavioral strategies as a first line approach to improve sleep habits
If sleep hygiene and behavioral strategies are not effective, melatonin use is recommended in otherwise healthy children with sleep onset insomnia in association with behavioral strategies
Melatonin might be helpful for sleep onset insomnia at least in the short-term use
Melatonin for sleep induction should be administered 30–60 min before the desired bedtime
Start with a minimal dose of 0.5 mg; if no effect after 1 week and then increase the dose with possible titration to 1 mg or more if needed until a maximum of 5 mg depending on age. Consider a dosage of 0.5 to 1 mg in infants 1 to 3 years of age; 1–2 mg in preschoolers, up to 3 mg in school-age children, and up to 5 mg in adolescents
Parents should be informed regarding potential adverse events of melatonin use and lack of long-term safety data and advised to consult with healthcare professional before using melatonin in children and not use for longer than 14 days without doctor’s recommendation
Melatonin use should be monitored by pediatricians to evaluate the presence of adverse effects
Theoretically, since there are no studies in infants and children, melatonin should be avoided in children below the age of 2 years
No relevant adverse effects have been reported in different studies for at least 2 years in children with NDDs and specifically no effect on growth or pubertal development; we could expect the same in neurotypical children
Supplementary Information
Below is the link to the electronic supplementary material.
Authors’ contributions
OB, MB, LN, IF, ORSC, and CG contributed to the study conception and design. The first draft of the manuscript was written by MB, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. The guidance was developed following the Sleep Medicines Experts Round Table in October 2023 sponsored by Procter & Gamble.
Declarations
Competing interests
All authors have received speaker and consultant honoraria from Procter & Gamble. Dr. Maria Breda received honorarium for medical writing service including consultant honorarium.
Disclaimer
The views expressed in the submitted article are his or her own.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Glaze DG, Rosen CL, Owens JA. Toward a practical definition of pediatric insomnia. Curr Ther Res. 2002;63:B4–B17. doi: 10.1016/S0011-393X(02)80100-X. [DOI] [Google Scholar]
- 2.Meaklim H, Jackson ML, Bartlett D, Saini B, Falloon K, Junge M, Slater J, Rehm IC, Meltzer LJ. Sleep education for healthcare providers: addressing deficient sleep in Australia and New Zealand. Sleep Health. 2020;6:636–650. doi: 10.1016/j.sleh.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 3.Corkum P, Weiss S, Hall W, Brown C, Chambers C, Constantin E, Godbout R, Hanlon-Dearman A, Ipsiroglu O, Reid GJ, Shea S, Smith IM, Stremler R, Witmans M. Assessment and treatment of pediatric behavioral sleep disorders in Canada. Sleep Med. 2019;56:29–37. doi: 10.1016/j.sleep.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Sleep Medicine . International classification of sleep Disorders: Diagnostic and coding manual. 3. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 5.Breda M, Belli A, Esposito D, Di Pilla A, Melegari MG, DelRosso L, Malorgio E, Doria M, Ferri R, Bruni O. Sleep habits and sleep disorders in Italian children and adolescents: a cross-sectional survey. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2023 doi: 10.5664/jcsm.10400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewien C, Genuneit J, Meigen C, Kiess W, Poulain T. Sleep-related difficulties in healthy children and adolescents. BMC Pediatr. 2021;21:82. doi: 10.1186/s12887-021-02529-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadzil A. Factors affecting the quality of sleep in children. Child Basel Switz. 2021;8:122. doi: 10.3390/children8020122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14:179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Blunden S, Galland B. The complexities of defining optimal sleep: empirical and theoretical considerations with a special emphasis on children. Sleep Med Rev. 2014;18:371–378. doi: 10.1016/j.smrv.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Phillips SR, Johnson A, Shirey MR, Rice M. Sleep quality in school-aged children: a concept analysis. J Pediatr Nurs. 2020;52:54–63. doi: 10.1016/j.pedn.2020.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, Hillard PJA. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health J Natl Sleep Found. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Taylor RW, Haszard JJ, Jackson R, Morrison S, Beebe DW, Meredith-Jones KA, Elder DE, Galland BC. Effect of sleep changes on health-related quality of life in healthy children: a secondary analysis of the DREAM crossover trial. JAMA Netw Open. 2023;6:e233005. doi: 10.1001/jamanetworkopen.2023.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74:444–455. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 14.Krause AJ, Ben Simon E, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, Walker MP. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18:404–418. doi: 10.1038/nrn.2017.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong JM, Ruttle PL, Klein MH, Essex MJ, Benca RM. Associations of child insomnia, sleep movement, and their persistence with mental health symptoms in childhood and adolescence. Sleep. 2014;37:901–909. doi: 10.5665/sleep.3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandez-Mendoza J, Bourchtein E, Calhoun S, Puzino K, Snyder CK, He F, Vgontzas AN, Liao D, Bixler E. Natural history of insomnia symptoms in the transition from childhood to adolescence: population rates, health disparities, and risk factors. Sleep. 2021;44:zsaa187. doi: 10.1093/sleep/zsaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruni O, Melegari MG, Esposito A, Sette S, Angriman M, Apicella M, Caravale B, Ferri R. Executive functions in preschool children with chronic insomnia. J Clin Sleep Med. 2020;16:231–241. doi: 10.5664/JCSM.8172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Semin Pediatr Neurol. 1996;3:44–50. doi: 10.1016/s1071-9091(96)80028-3. [DOI] [PubMed] [Google Scholar]
- 19.Yoo S-S, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep–a prefrontal amygdala disconnect. Curr Biol CB. 2007;17:R877–878. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Shimizu M, Zeringue MM, Erath SA, Hinnant JB, El-Sheikh M. Trajectories of sleep problems in childhood: associations with mental health in adolescence. Sleep. 2021;44:zsaa190. doi: 10.1093/sleep/zsaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang FN, Xie W, Wang Z. Effects of sleep duration on neurocognitive development in early adolescents in the USA: a propensity score matched, longitudinal, observational study. Lancet Child Adolesc Health. 2022;6:705–712. doi: 10.1016/S2352-4642(22)00188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uccella S, Cordani R, Salfi F, Gorgoni M, Scarpelli S, Gemignani A, Geoffroy PA, De Gennaro L, Palagini L, Ferrara M, Nobili L. Sleep deprivation and insomnia in adolescence: implications for mental health. Brain Sci. 2023;13:569. doi: 10.3390/brainsci13040569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou J, Zhu L, Teng Y, Tong J, Gao G, Yan S, Tao F, Huang K. Early sleep duration trajectories and children’s cognitive development: a prospective cohort study. Eur J Pediatr. 2023;182:5353–5365. doi: 10.1007/s00431-023-05195-7. [DOI] [PubMed] [Google Scholar]
- 24.Meininger JC, Gallagher MR, Eissa MA, Nguyen TQ, Chan W. Sleep duration and its association with ambulatory blood pressure in a school-based, diverse sample of adolescents. Am J Hypertens. 2014;27:948–955. doi: 10.1093/ajh/hpt297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Javaheri S, Storfer-Isser A, Rosen CL, Redline S. The association of short and long sleep durations with insulin sensitivity in adolescents. J Pediatr. 2011;158:617–623. doi: 10.1016/j.jpeds.2010.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sunwoo J-S, Yang KI, Kim JH, Koo DL, Kim D, Hong SB. Sleep duration rather than sleep timing is associated with obesity in adolescents. Sleep Med. 2020;68:184–189. doi: 10.1016/j.sleep.2019.12.014. [DOI] [PubMed] [Google Scholar]
- 27.Sehn AP, Gaya AR, Dias AF, Brand C, Mota J, Pfeiffer KA, Sayavera JB, Renner JDP, Reuter CP. Relationship between sleep duration and TV time with cardiometabolic risk in adolescents. Environ Health Prev Med. 2020;25:42. doi: 10.1186/s12199-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Insufficient sleep duration is associated with dietary habits, screen time, and obesity in children. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2018;14:1689–1696. doi: 10.5664/jcsm.7374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cappuccio FP, Taggart FM, Kandala N-B, Currie A, Peile E, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuwen W, Chen ML, Cain KC, Ringold S, Wallace CA, Ward TM. Daily sleep patterns, sleep quality, and sleep hygiene among parent-child dyads of young children newly diagnosed with juvenile idiopathic arthritis and typically developing children. J Pediatr Psychol. 2016;41:651–660. doi: 10.1093/jpepsy/jsw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dubois-Comtois K, Pennestri M-H, Bernier A, Cyr C, Godbout R. Family environment and preschoolers’ sleep: the complementary role of both parents. Sleep Med. 2019;58:114–122. doi: 10.1016/j.sleep.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Merrill RM, Slavik KR. Relating parental stress with sleep disorders in parents and children. PLoS ONE. 2023;18:e0279476. doi: 10.1371/journal.pone.0279476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bayer JK, Hiscock H, Hampton A, Wake M. Sleep problems in young infants and maternal mental and physical health. J Paediatr Child Health. 2007;43:66–73. doi: 10.1111/j.1440-1754.2007.01005.x. [DOI] [PubMed] [Google Scholar]
- 34.Mansolf M, Blackwell CK, Chandran A, Colicino E, Geiger S, Harold G, McEvoy C, Santos HP, Sherlock PR, Bose S, Wright RJ. Caregiver perceived stress and child sleep health: an item-level individual participant data meta-analysis. J Child Fam Stud. 2023;32:2558–2572. doi: 10.1007/s10826-023-02624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin J, Hiscock H, Hardy P, Davey B, Wake M. Adverse associations of infant and child sleep problems and parent health: an Australian population study. Pediatrics. 2007;119:947–955. doi: 10.1542/peds.2006-2569. [DOI] [PubMed] [Google Scholar]
- 36.Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol JFP J Div Fam Psychol Am Psychol Assoc Div. 2007;43(21):67–73. doi: 10.1037/0893-3200.21.1.67. [DOI] [PubMed] [Google Scholar]
- 37.Kelly RJ, El-Sheikh M. Marital conflict and children’s sleep: reciprocal relations and socioeconomic effects. J Fam Psychol JFP J Div Fam Psychol Am Psychol Assoc Div. 2011;43(25):412–422. doi: 10.1037/a0023789. [DOI] [PubMed] [Google Scholar]
- 38.Maratia F, Bacaro V, Crocetti E. Sleep is a family affair: a systematic review and meta-analysis of longitudinal studies on the interplay between adolescents’ sleep and family factors. Int J Environ Res Public Health. 2023;20:4572. doi: 10.3390/ijerph20054572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dewald-Kaufmann J, de Bruin E, Michael G. Cognitive behavioral therapy for insomnia (CBT-i) in school-aged children and adolescents. Sleep Med Clin. 2019;14:155–165. doi: 10.1016/j.jsmc.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 40.Williamson AA, Mindell JA, Hiscock H, Quach J. Child sleep behaviors and sleep problems from infancy to school-age. Sleep Med. 2019;63:5–8. doi: 10.1016/j.sleep.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simonneaux V, Ribelayga C. Generation of the melatonin endocrine message in mammals: a review of the complex regulation of melatonin synthesis by norepinephrine, peptides, and other pineal transmitters. Pharmacol Rev. 2003;55:325–395. doi: 10.1124/pr.55.2.2. [DOI] [PubMed] [Google Scholar]
- 42.Prayag AS, Münch M, Aeschbach D, Chellappa SL, Gronfier C. Light modulation of human clocks, wake, and sleep. Clocks Sleep. 2019;1:193–208. doi: 10.3390/clockssleep1010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prayag AS, Najjar RP, Gronfier C. Melatonin suppression is exquisitely sensitive to light and primarily driven by melanopsin in humans. J Pineal Res. 2019;66:e12562. doi: 10.1111/jpi.12562. [DOI] [PubMed] [Google Scholar]
- 44.Mauriz JL, Collado PS, Veneroso C, Reiter RJ, González-Gallego J. A review of the molecular aspects of melatonin’s anti-inflammatory actions: recent insights and new perspectives. J Pineal Res. 2013;54:1–14. doi: 10.1111/j.1600-079X.2012.01014.x. [DOI] [PubMed] [Google Scholar]
- 45.Comai S, Ochoa-Sanchez R, Gobbi G. Sleep-wake characterization of double MT1/MT2 receptor knockout mice and comparison with MT1 and MT2 receptor knockout mice. Behav Brain Res. 2013;243:231–238. doi: 10.1016/j.bbr.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 46.Skrzelowski M, Brookhaus A, Shea LA, Berlau DJ. Melatonin use in pediatrics: evaluating the discrepancy in evidence based on country and regulations regarding production. J Pediatr Pharmacol Ther JPPT Off J PPAG. 2021;26:4–20. doi: 10.5863/1551-6776-26.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.EFSA Panel on Dietetic Products. Nutrition and Allergies (NDA) Scientific opinion on the substantiation of a health claim related to melatonin and reduction of sleep onset latency (ID 1698, 1780, 4080) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA J. 2011;9:2241. doi: 10.2903/j.efsa.2011.2241. [DOI] [Google Scholar]
- 48.Black LI, Clarke TC, Barnes PM, Stussman BJ, Nahin RL. Use of complementary health approaches among children aged 4–17 years in the United States: National Health Interview Survey, 2007–2012. Natl Health Stat Rep. 2015;78:1–19. [PMC free article] [PubMed] [Google Scholar]
- 49.Lee SKM, Smith L, Tan ECK, Cairns R, Grunstein R, Cheung JMY. Melatonin use in children and adolescents: a scoping review of caregiver perspectives. Sleep Med Rev. 2023;70:101808. doi: 10.1016/j.smrv.2023.101808. [DOI] [PubMed] [Google Scholar]
- 50.Parvataneni T, Srinivas S, Shah K, Patel RS. Perspective on melatonin use for sleep problems in autism and attention-deficit hyperactivity disorder: a systematic review of randomized clinical trials. Cureus. 2020;12:e8335. doi: 10.7759/cureus.8335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rzepka-Migut B, Paprocka J. Efficacy and safety of melatonin treatment in children with autism spectrum disorder and attention-deficit/hyperactivity disorder—a review of the literature. Brain Sci. 2020;10:219. doi: 10.3390/brainsci10040219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Edemann-Callesen H, Andersen HK, Ussing A, Virring A, Jennum P, Debes NM, Laursen T, Baandrup L, Gade C, Dettmann J, Holm J, Krogh C, Birkefoss K, Tarp S, Händel MN. Use of melatonin in children and adolescents with idiopathic chronic insomnia: a systematic review, meta-analysis, and clinical recommendation. eClinicalMedicine. 2023;61:102048. doi: 10.1016/j.eclinm.2023.102048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Händel MN, Andersen HK, Ussing A, Virring A, Jennum P, Debes NM, Laursen T, Baandrup L, Gade C, Dettmann J, Holm J, Krogh C, Birkefoss K, Tarp S, Bliddal M, Edemann-Callesen H. The short-term and long-term adverse effects of melatonin treatment in children and adolescents: a systematic review and GRADE assessment. eClinicalMedicine. 2023;61:102083. doi: 10.1016/j.eclinm.2023.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Choi K, Lee YJ, Park S, Je NK, Suh HS. Efficacy of melatonin for chronic insomnia: systematic reviews and meta-analyses. Sleep Med Rev. 2022;66:101692. doi: 10.1016/j.smrv.2022.101692. [DOI] [PubMed] [Google Scholar]
- 55.Goldman RD, Bongiorno PB, Olcese JM, Witt-Enderby PA, Shatkin JP. Myths and evidence regarding melatonin supplementation for occasional sleeplessness in the pediatric population. Pediatr Ann. 2021;50:e391–e395. doi: 10.3928/19382359-20210823-01. [DOI] [PubMed] [Google Scholar]
- 56.Pin Arboledas G, Merino Andreu M, de la Calle CT, Hidalgo Vicario MI, Rodríguez Hernández PJ, Soto Insuga V. Madrid Pérez JA (2014) [Consensus document on the clinical use of melatonin in children and adolescents with sleep-onset insomnia] An Pediatr Barc Spain. 2003;81(328):e1–9. doi: 10.1016/j.anpedi.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 57.Bruni O, Alonso-Alconada D, Besag F, Biran V, Braam W, Cortese S, Moavero R, Parisi P, Smits M, Van der Heijden K, Curatolo P. Current role of melatonin in pediatric neurology: clinical recommendations. Eur J Paediatr Neurol EJPN Off J Eur Paediatr Neurol Soc. 2015;19:122–133. doi: 10.1016/j.ejpn.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 58.Hagan JS, Duncan P, Shaw JD. Bright futures: guidelines for health supervision of infants, children, and adolescents. Third Edition. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 59.Wilson K, St-Onge M-P, Tasali E. Diet composition and objectively assessed sleep quality: a narrative review. J Acad Nutr Diet. 2022;122:1182–1195. doi: 10.1016/j.jand.2022.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ríos-Hernández A, Gilchrist C, Chelimo C, Castro TG, Izquierdo-Pulido M, Wall C, Thabrew H, Berry S, Morton S, Grant C. The relationship between diet and sleep in 2-y-old children: results from growing up in New Zealand. Nutrition. 2022;95:111560. doi: 10.1016/j.nut.2021.111560. [DOI] [PubMed] [Google Scholar]
- 61.Faris ME, Vitiello MV, Abdelrahim DN, Cheikh Ismail L, Jahrami HA, Khaleel S, Khan MS, Shakir AZ, Yusuf AM, Masaad AA, Bahammam AS. Eating habits are associated with subjective sleep quality outcomes among university students: findings of a cross-sectional study. Sleep Breath. 2022;26:1365–1376. doi: 10.1007/s11325-021-02506-w. [DOI] [PubMed] [Google Scholar]
- 62.Zhao Y, Qu D, Liang K, Bao R, Chen S. Eating habits matter for sleep difficulties in children and adolescents: a cross-sectional study. Front Pediatr. 2023;11:1108031. doi: 10.3389/fped.2023.1108031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: sleep, development, and beyond. Sleep Med Rev. 2018;40:93–108. doi: 10.1016/j.smrv.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr JDBP. 2009;30:394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kitsaras G, Goodwin M, Allan J, Kelly M, Pretty I. Bedtime routine characteristics and activities in families with young children in the north of England. Int J Environ Res Pub Health 18. 2021 doi: 10.3390/ijerph18178983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mindell JA, Leichman ES, Lee C, Williamson AA, Walters RM. Implementation of a nightly bedtime routine: how quickly do things improve? Infant Behav Dev. 2017;49:220–227. doi: 10.1016/j.infbeh.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10:771–779. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 68.Philbrook LE, Teti DM. Bidirectional associations between bedtime parenting and infant sleep: parenting quality, parenting practices, and their interaction. J Fam Psychol JFP J Div Fam Psychol Am Psychol Assoc Div. 2016;43(30):431–441. doi: 10.1037/fam0000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sadeh A, Mindell J, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18:60–73. doi: 10.1111/j.1365-2869.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 70.Bruni O, Angriman M. Pediatric insomnia: new insights in clinical assessment and treatment options. Arch Ital Biol. 2015;153:144–156. doi: 10.12871/000398292015239. [DOI] [PubMed] [Google Scholar]
- 71.Etherton H, Blunden S, Hauck Y. Discussion of extinction-based behavioral sleep interventions for young children and reasons why parents may find them difficult. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2016;12:1535–1543. doi: 10.5664/jcsm.6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kahn M, Barnett N, Gradisar M. Implementation of behavioral interventions for infant sleep problems in real-world settings. J Pediatr. 2023;255:137–146.e2. doi: 10.1016/j.jpeds.2022.10.038. [DOI] [PubMed] [Google Scholar]
- 73.Erland LAE, Saxena PK. Melatonin natural health products and supplements: presence of serotonin and significant variability of melatonin content. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2017;13:275–281. doi: 10.5664/jcsm.6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Consumer Product Safety Commission Child-resistant packaging for certain over-the-counter drug products. Final rule Fed Regist. 2001;66:40111–40116. [PubMed] [Google Scholar]
- 75.Malow BA, Findling RL, Schroder CM, Maras A, Breddy J, Nir T, Zisapel N, Gringras P. Sleep, growth, and puberty after 2 years of prolonged-release melatonin in children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2021;60:252–261.e3. doi: 10.1016/j.jaac.2019.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Salanitro M, Wrigley T, Ghabra H, de Haan E, Hill CM, Solmi M, Cortese S. Efficacy on sleep parameters and tolerability of melatonin in individuals with sleep or mental disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;139:104723. doi: 10.1016/j.neubiorev.2022.104723. [DOI] [PubMed] [Google Scholar]
- 77.Wei S, Smits MG, Tang X, Kuang L, Meng H, Ni S, Xiao M, Zhou X. Efficacy and safety of melatonin for sleep onset insomnia in children and adolescents: a meta-analysis of randomized controlled trials. Sleep Med. 2020;68:1–8. doi: 10.1016/j.sleep.2019.02.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.