Abstract
Introduction and importance
Os odontoideum is a rare condition commonly associated with atlantoaxial instability (AAI) and leading to atlantoaxial dislocation. The incidence of Os odontoideum is higher in patients with Down syndrome. Similar to odontoid fractures, atlantoaxial dislocation in patients with Os odontoideum can result in neurological deficits, disability, and even mortality.
Case presentation
We present two cases of Os odontoideum accompanied by Down syndrome. Both patients were hospitalized due to progressive tetraparesis after falls several months prior. Upon examination, the patients exhibited myelopathy and were unable to walk or stand. MRI revealed spinal stenosis at the C1-C2 level due to atlantoaxial dislocation. C1-C2 fixation using Harms' technique was performed in both cases. One case experienced a complication involving instrument failure, necessitating revision surgery.
Clinical discussion
Due to the characteristics of transverse ligament laxity, low muscle tone, excessive joint flexibility, and cognitive impairment, children with both Down syndrome and Os odontoideum are at a high risk of disability and even mortality from spinal cord injury. Most authors recommend surgical management when patients exhibit atlantoaxial instability. Additional factors such as low bone density, cognitive impairment, and a high head-to-body ratio may increase the risk of surgical instrument failure and nonunion postoperatively in patients with Down syndrome.
Conclusion
Os odontoideum is a cause of AAI in patients with DS. Indication of surgery in the presence of AAI helps to resolve neurological injury and prevent further deterioration. The use of a cervical collar is considered to prevent instrument failure postoperatively.
Keywords: Os odontoideum, Down syndrome, Atlantoaxial instability, Atlantoaxial dislocation, Case report
Highlights
-
•
Os odontoideum is a rare condition associated with atlantoaxial instability and leading to atlantoaxial dislocation.
-
•
The incidence of Os odontoideum is higher in patients with Down syndrome.
-
•
Children having Os odontoideum accompanied by Down syndrome are at a high risk of disability and even mortality from spinal cord injury.
-
•
Indication of surgery in the presence of atlantoaxial instability helps to resolve neurological injury and prevent further deterioration.
-
•
Children with Down syndrome are at risk of surgical instrument failure and nonunion postoperatively.
1. Introduction
Os odontoideum (OsO) is a rare pathology, first described by Giacomini in 1886. Most cases are associated with atlantoxial instability (AAI) and can lead to atlantoaxial dislocation (AAD) [1]. OsO is characterized by a small bone at the apex of the odontoid process, with a smooth circumferential cortical margin, and no osseous continuity with the axis's body. The instability mechanism is similar to a Type II odontoid fracture. The etiology of OsO is debated; some authors suggest a congenital origin due to failed fusion of two ossification centers, others propose a traumatic genesis leading to a chronic non-union fracture of the odontoid process. OsO is anatomically classified into orthotopic and dystopic types. An orthotopic OsO moves with the anterior arch of C1, while a dystopic one is functionally fused to the basion [2]. The incidence is increased in groups of patients with Klippel-Feil syndrome, Down syndrome, multiple epiphyseal dysplasia, other skeletal dysplasias [3].
Trisomy 21, the most common chromosomal abnormality in humans, occurs in approximately 1 per 700 live births [4]. The clinical features of this pathology were originally described by Langdon Down in 1866, and his name was later used to name the syndrome. This syndrome is characterized by mild to moderate mental retardation, craniofacial-skull base anomalies, cardiovascular disorders, and gastrointestinal problems. Other notable problems in Down syndrome (DS) are ligament laxity, excessive joint flexibility, which are particularly relevant with AAI. In 1994, Harley described a secondary neurological complication occurring in children with Down syndrome during otolaryngologic procedures [5]. Regarding to this, children with Down syndrome quite often have to experience otolaryngologic procedures such myringotomy, adenotonsillar surgery under general anesthesia and ventilation tubes. He noted that atlantoaxial instability occurs in 10–20 % of patients with Down syndrome who are at risk for atlantoaxial subluxation and subsequent complications during anesthetic induction, positioning and manipulation associated with surgery, thereby causing neurological complications. Pueschel et al. reported that 14,6 % of 404 patients with Down syndrome had AAI on plain radiographs, but only 1,5 % had symptomatic AAI [6].
Os odontoideum is one of the causes of atlantoaxial instability in patients with Down syndrome. French et al. screened 185 patients with DS and found that OsO occurred in 6 cases (3 %), with 3 of these patients having a normal odontoid 13 years prior (via X-ray) [7]. In a literature review, Sergeenko found 80 cases of DS with OsO, 63 of which had AAI (79 %) [8]. On the occasions of two cases of Down syndrome accompanied by Os odontoideum, we review the literature and share our experience of surgical treatment in these patients. Both of cases were managed at Viet Duc University Hospital. This work has been reported in line with the SCARE criteria [9].
2. Presentation of cases
2.1. Case 1
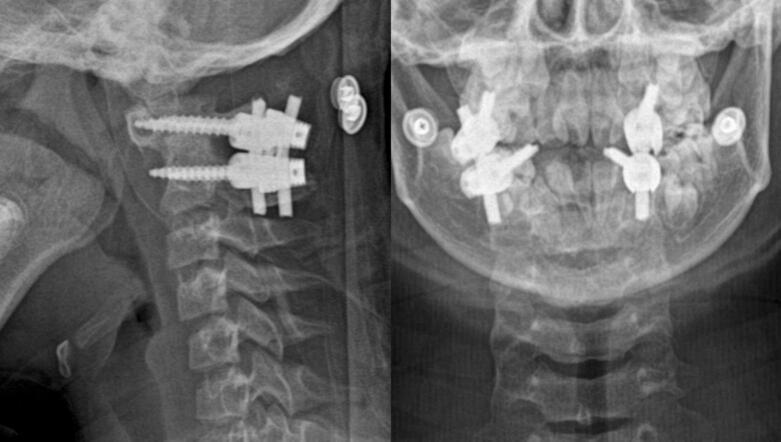
An 8-year-old girl with DS was admitted to our hospital, with progressive tetraparesis after falling on the ground 2 months piror. At presentation, she was wheelchair- bound, unable to walk or stand, and exhibited progressive tetraparesis with muscular strength graded at 2/5, hyperreflexia in all limbs. X-rays revealed anterior AAD and dystopic OsO. MRI showed spinal cord compression due to AAD (Fig. 1).
Fig. 1.
Preoperative X-ray and MRI of the 8-year-old girl with DS and OsO (Case 1) showing AAD and dystopic OsO (white arrow).
The surgical plan included intraoperative reduction and posterior fusion. The patient underwent C1–C2 instrumentation using Harm's technique, with lateral mass screws at C1, pedicle srews at C2, and two 3-mm rods placed into the polyaxial screw heads. The laminae of C1 and C2 were decorticated by the high-speed drill, and homologous bone graft was placed for posterior fusion. A semi-rigid collar was used postoperatively to support immobilization of the instrument, which was made according to the size of the child's neck.
Postoperative X-rays showed completed reduction of AAD (Fig. 2). The patient's neurological function began to improve; muscular strength was grade at 3/5 one week after surgery. Six months postoperatively, she could walk independently.
Fig. 2.
Post-operative X-rays of the 8-year-old girl with DS and OsO (Case 1) showing complete reduction of C1–C2 joint.
2.2. Case 2
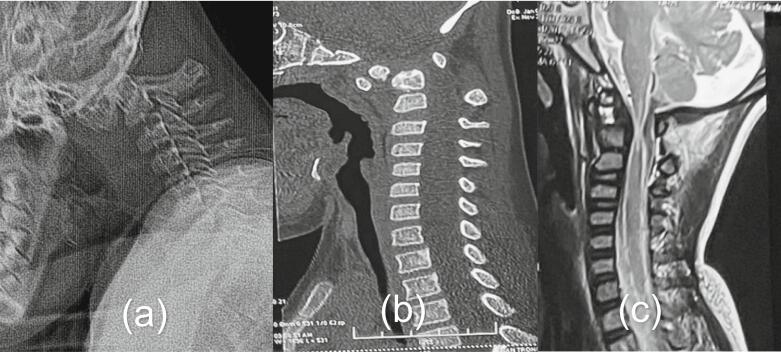
A 5-year-old boy with DS, was hospitalized because of progressive tetraparesis after falling on the ground 4 months before. Upon admission, he was unable to stand or walk, had muscular strength grade at 2/5, and exhibited hyperreflexia in all limbs. X-rays and CT scans showed anterior AAD and orthotopic OsO. MRI indicated spinal stenosis and spinal cord edema at the C1-C2 level (Fig. 3).
Fig. 3.
Preoperative radiological studies of the 5-year-old boy with DS and OsO (Case 2). (a) X-rays showed anterior AAD (b) CT showed orthotopic OsO (c) MRI showed spinal cord compressed by odontoid process anteriorly and posterior arch of C1 posteriorly.
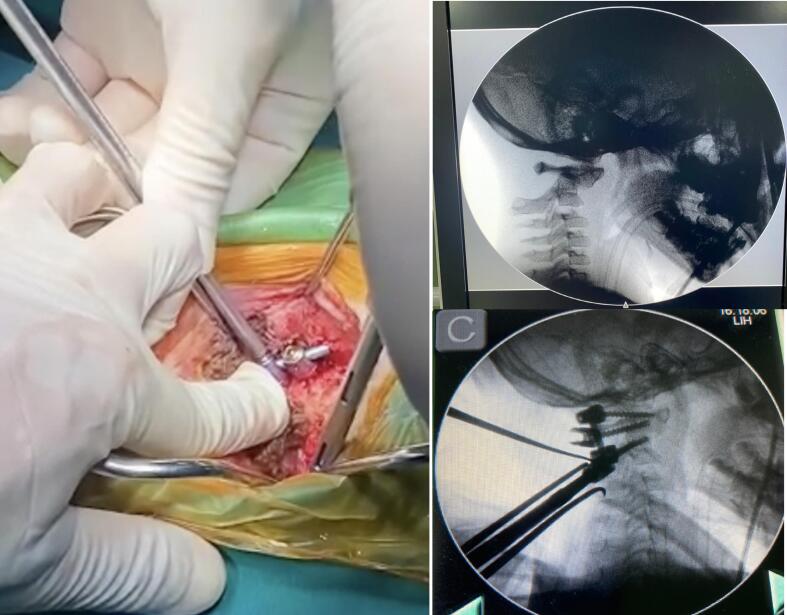
The patient underwent intraoperative reduction and C1-C2 stabilization with Harms's arthrodesis (Fig. 4). Postoperative X-rays revealed a complete reduction of AAD. A semi-rigid collar was used for postoperative immobilization. Postoperatively patient's neurological function improved, with muscular strength graded at 3/5.
Fig. 4.
Intraoperative reduction with rod placement on one side: A screwdriver was used to elevate the C1 screw while manual downward pressure was applied to the C2 spinous process. Subsequently, a rod was positioned on the contralateral side to maintain the reduction.
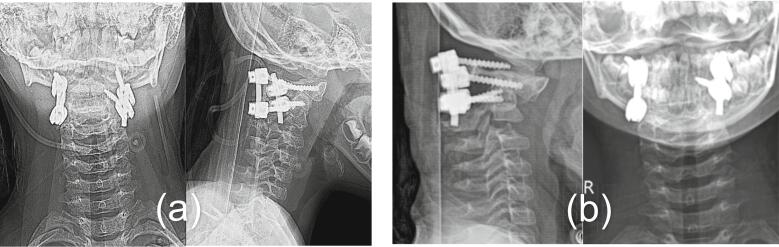
One month postoperatively, the patient's neurological function had deteriorated, with the muscular strength decreasing to 2/5. X-rays revealed instrument failure with a recurrent AAD (Fig. 5). The patient's parents admitted to not following our advice regarding collar use. We decided to perform revision surgery with a plan for occiptocervical fusion. The instrumentation included a plate fixed with three bicortical screws to the occiput, pedicle screws at C2, lateral mass crews at C3. Postoperative X-rays showed a complete reduction of AAD (Fig. 6). Six months after surgery, patient exhibited improved neurological function with an AIS Grade of D. At the last follow-up, one year after surgery, the patient was able to walk independently, and there was no evidence of instrument failure on the X-rays.
Fig. 5.
Postoperative X-rays of 5-year-old boy with DS and OsO (Case 2). (a) A day after surgery, X-rays showed complete reduction of C1-C2 joint (b) One month after surgery, X-rays showed instruments failure and recurrent AAD.
Fig. 6.
X-rays after revision surgery showed occipitocervical fixation and complete reduction of C1-C2 joint.
3. Discussion
Patients with DS and OsO may present acute clinical manifestation after a minor trauma without any precursors, or progressive neurological deficits that worsen over time. Patients who exhibit only transient weakness of the extremities and paresthesia after minor trauma usually recover fully. However, those with a gradual onset and progressive neurologic impairment have a greater potential for permanent deficits [2].
AAI in DS patients with OsO is more commonly seen in childhood and adolescence, rarely in adult when ligament relaxation is reduced. AAI is typically indicated by an increase of atlantodental interval (ADI). However, since the OsO often moves with the anterior arch of C1, measurements of its distance to C1 are of little value. AAI may decrease the space available for the cord (SAC) but not affect ADI. A reduced SAC with neck extension significantly correlates with a higher risk for myelopathy [10].
Pre- and postoperative neurological evaluation is crucial for assessing surgical outcomes. However, neurological assessment in children can be challenging, because they are not cooperative, especially those with cognitive impairment like DS.
Most of the authors agree on the opinion of fusion surgery when AAI occurs. However, the optimal management of asymptomatic OsO remains elusive due to its rarity and the limited case reports or small series in the literature, which makes it difficult to offer a standard guideline for the treatment of this condition. This difficulty stems from the inability to accurately predict the risk of spinal cord injury in untreated patients. Without consensus or evidence-based guideline for treatment, experts relying on case reports for recommendations. Some suggest observation for asymptomatic patients due to the low risk of sudden neurological injury. Others advocate prophylactic surgery, as it's difficult to predict which patients will develop neurological issues. According to Klimo, the presence of Os odontoideum puts patients in considerable risk. Through a retrospective study of 78 cases, the author noted that 4 % of patients presented late neurological injury after being diagnosed with Os odontoideum, and 44 % presented with myelopathy at the time of examination. The likelihood of unforeseen trauma that leads to spinal cord injury (SCI) may be low; however, the impact on daily activities and the patient's life can be significant. Furthermore, the risk of SCI is heightened in patients with cognitive impairments. Therefore, we recommend providing the patient's family with counseling regarding the risk of SCI, as well as discussing a strategy for prophylactic surgery.
Various techniques for treating of AAI included posterior arch wiring, posterior screw fixation, and anterior plating. The rate of non-union occurs relatively high in posterior arch wiring technique. Fusion rates have generally been worse with ligamentous injury and congenital anomalies [11,12]. Nowadays posterior screw fixation, with advances in surgical instruments, has a high fusion rate and good outcome but comes with a risk of vertebral artery injury, estimated at approximately 2 % [13]. Posterior screw fixation can be achieved by C1-C2 transarticular screws or C1 lateral mass screws, C2 pedicle screws/C2 pars interarticularis screws/C2 translaminar screws, subaxial lateral mass screws combined with a rod. In such cases of AAD (atlantoaxial dislocation), the posterior approach is considered safe and sufficient for fixation and reduction. Due to obstruction of the mandible, the anterior approach is restricted. However, when posterior reduction fails, a transoral odontoidectomy is indicated to decompress the spinal cord.
In most cases of AAI, atlantoaxial fixation is sufficient, but occipitocervical fixation is preferred in cases of atlantooccipital dislocation, atlas abnormalities precluding screw implantation, repeated atlantoaxial fusion failure, or post-anterior odontoidectomy. In case 1, we performed occipital to C3 fixation due to instrument failure after previous HARMS surgery.
Besides fixation and fusion, decompression of spinal cord due to AAD is an important aspect to consider. Most authors advocated that reduction of dislocation is sufficient to decompress spinal cord and does not require additional decompression. Reduction can be performed using a closed method (with Halo traction) or open method (through surgery). If intraoperative repositioning of AAD fails, posterior C1-C2 laminectomy or anterior odontoidectomy is necessary.
Regarding the use of rigid or semi-rigid collar to support immobilization after surgery, we believe it is very necessary. There are some factors that increase the risk of instrument failure and non-union after surgery:
-
(1).
Many studies have shown that the bone density of people with DS is lower than that general population [14].
-
(2).
In patients with cognitive impairment, the ability to control movements of the cervical spine is poor. It probably results in undue movement of the patient's neck after surgery.
-
(3).
The child's head is proportionately larger than in the adult. This heavier head mass results in greater forces applied on instruments when patient's head moves passively.
Instrument failure can cause non-union, loss of reduction, and neurological injury. Revision surgery is often required, and sometimes an extended fixation is necessary. In Case 1, when we performed revision surgery, three out of four screws had loosened. The residual bone was too small to create another hole, so we had to extend the fixation with occipital and subaxial screws. This complication can be disastrous and needs to be prevented. Therefore, we place great importance on explaining to and guiding the patient's parents about the use of a rigid or semi-rigid collar after surgery until signs of bone fusion are detected.
4. Literature review
See Table 1.
Table 1.
Important finding of the Os odontoideum-related article.
| First author, year | Title | Important finding |
|---|---|---|
| J.W. Fielding, 1980 | Os Odontoideum | 9/35 cases of Os odontoideum had normal odontoid process prior to the development of the os odontoideum Only one-third of the patients had symptoms of neural deficits |
| H.G. French, 1987 | Upper Cervical Ossicles in Down Syndrome | 6/184 patients with Down syndrome had abnormal ossicles of the dens. Only one patient had AAI |
| A.H. Menezes, 1992 | Craniovertebral Abnormalities in Down's Syndrome | Os odontoideum was seen in 3/18 patients with craniovertebral abnormalities. |
| E.H. Harley, 1994 | Neurologic Sequelae Secondary to Atlantoaxial Instability in Down Syndrome: Implications in Otolaryngologic Surgery | 10 % to 20 % of children with DS have AAI. Up to 1.5 % of these patients will exhibit neurologic symptoms. |
| M. Watanabe, 1996 | Atlantoaxial Instability in Os Odontoideum With Myelopathy | If the patient has either a sagittal plane rotation angle of more than 20° or an Instability Index of more than 40 %, he or she is likely to have the cord signs |
| O.M. Sergeenko, 2020 | Atlantoaxial dislocation due to os odontoideum in patients with Down's syndrome: literature review and case reports | Most patients with DS and OsO had AAI (80 %). The appropriate treatment in such cases is posterior screw fixation |
5. Conclusion
In patients with DS, Os odontoideum is a cause of AAI. Neurological injury can manifest acutely through minor trauma or gradually over a progressive period. Surgical intervention in the presence of AAI is indicated to resolve neurological injury and prevent further deterioration. Down syndrome's characteristic features, including low bone density, cognitive impairment, and a high head-to-body ratio may increase the risk of surgical instrument failure and nonunion postoperatively. The use of a cervical collar is considered effective in preventing instrument failure postoperatively.
Ethical approval
A written consent was received from the parents' patient. In such case, the anonymised presentation of case report does not required a separate approvement by the ethics committee.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Long Hoang Nguyen, Hoang Minh Bui, Khanh Manh Nguyen, Tien Le Bao Nguyen: study concept, data collection, data analysis, writing the paper. Dang Hai Do, Hung Manh Do, Hoang Vu Nguyen: reviewing and correction of the paper.
Guarantor
Hoang Minh Bui.
Research registration number
None.
Declaration of competing interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Giacomini C. Sull’esistenzadell’ “osodontoideum” nell’uomo. Gior. Accad. Med. Torino. 1886:24–28. [Google Scholar]
- 2.Fielding J.W., Hensinger R.N., Hawkins R.J. Os Odontoideum. J. Bone Joint Surg. Am. 1980;62:376–383. [PubMed] [Google Scholar]
- 3.Menezes A.H., Ryken T.C. Craniovertebral abnormalities in Down’s syndrome. Pediatr. Neurosurg. 1992;18:24–33. doi: 10.1159/000120638. [DOI] [PubMed] [Google Scholar]
- 4.Mai C.T., Isenburg J.L., Canfield M.A., Meyer R.E., Correa A., Alverson C.J., Lupo P.J., Riehle-Colarusso T., Cho S.J., Aggarwal D., Kirby R.S., National Birth Defects Prevention Network National population-based estimates for major birth defects, 2010–2014. Birth Defects Res. 2019;111:1420–1435. doi: 10.1002/bdr2.1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harley E.H., Collins M.D. Neurologic sequelae secondary to atlantoaxial instability in down syndrome: implications in otolaryngologic surgery. Arch. Otolaryngol. Head Neck Surg. 1994;120:159–165. doi: 10.1001/archotol.1994.01880260031007. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson R.L., Putney M.E., Allen B.L. Comparison of neurologic deficits with atlanto-dens intervals in patients with Down syndrome. J. Spinal Disord. 1997;10:246–252. [PubMed] [Google Scholar]
- 7.French H.G., Burke S.W., Roberts J.M., Johnston C.E., Whitecloud T., Edmunds J.O. Upper cervical ossicles in Down syndrome. J. Pediatr. Orthop. 1987;7:69–71. doi: 10.1097/01241398-198701000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Sergeenko O.M., Dyachkov K.A., Ryabykh S.O., Burtsev A.V., Gubin A.V. Atlantoaxial dislocation due to os odontoideum in patients with Down’s syndrome: literature review and case reports. Childs Nerv. Syst. 2020;36:19–26. doi: 10.1007/s00381-019-04401-y. [DOI] [PubMed] [Google Scholar]
- 9.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A., Collaborators The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109:1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watanabe M., Toyama Y., Fujimura Y. Atlantoaxial instability in os odontoideum with myelopathy. Spine. 1996;21:1435–1439. doi: 10.1097/00007632-199606150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Smith M.D., Phillips W.A., Hensinger R.N. Complications of fusion to the upper cervical spine. Spine. 1991;16:702–705. doi: 10.1097/00007632-199107000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Dickman C.A., Sonntag V.K.H., Papadopoulos S.M., Hadley M.N. The interspinous method of posterior atlantoaxial arthrodesis. J. Neurosurg. 1991;74:190–198. doi: 10.3171/jns.1991.74.2.0190. [DOI] [PubMed] [Google Scholar]
- 13.Ghaith A.K., Yolcu Y.U., Alvi M.A., Bhandarkar A.R., Sebastian A.S., Freedman B.A., Bydon M. Rate and characteristics of vertebral artery injury following C1-C2 posterior cervical fusion: a systematic review and Meta-analysis. World Neurosurg. 2021;148:118–126. doi: 10.1016/j.wneu.2020.12.165. [DOI] [PubMed] [Google Scholar]
- 14.Carfì A., Liperoti R., Fusco D., Giovannini S., Brandi V., Vetrano D.L., Meloni E., Mascia D., Villani E.R., Manes Gravina E., Bernabei R., Onder G. Bone mineral density in adults with Down syndrome. Osteoporos. Int. 2017;28:2929–2934. doi: 10.1007/s00198-017-4133-x. [DOI] [PubMed] [Google Scholar]