Abstract
The Cancer Intervention and Surveillance Modeling Network-Lung Working Group (CISNET-LWG) age-period-cohort (APC) methodology to study smoking patterns can be applied to tackle important issues in tobacco control and public health. This paper summarizes analyses of smoking patterns in the US by race/ethnicity, educational attainment, family income and for each of the 50 US states using the CISNET-LWG APC approach, describing how decision-makers, policy advocates, and researchers can use the sociodemographic analyses in this supplement to project state smoking trends and develop effective state-level tobacco control strategies. The all-cause mortality relative risk estimates associated with smoking for US race/ethnicity and education groups are also discussed in the context of research that measures and evaluates health disparities. Finally, the application of the CISNET-LWG APC methodology to Brazil is reviewed with a view towards how the same types of analyses can be applied to other low- and middle-income countries.
Introduction
The present supplement of the AJPM, published in January 2023,1 provides detailed smoking histories for disparate populations using the Cancer Intervention and Surveillance Modeling Network - Lung Working Group (CISNET-LWG) age, period, and cohort (APC) methodology. Until now, such detailed cohort-specific smoking data for US populations by race/ethnicity, educational attainment, family income, and state have not been available. These data facilitate in-depth examination of smoking disparities, and direct attention to patterns among recent birth cohorts that appear likely to affect future trends. They also invite further exploration of how smoking disparities across states may be related to racial/ethnic and socioeconomic status (SES) disparities and state tobacco control policies. New information about smoking-related mortality relative risk by race/ethnicity and education provides building blocks for future work evaluating the relationship between smoking disparities and mortality outcomes. The APC framework applied to Brazil shows how other countries may similarly benefit from developing comprehensive smoking estimates. This paper summarizes findings from across the supplement, and discusses their limitations and implications for both US and global smoking disparities research.
US smoking disparities and their relationship to mortality impacts
Race/ethnicity.
Despite reductions in initiation and increases in cessation among recent cohorts for all racial/ethnic groups, Meza et al.2 show how disparities in all smoking indicators across racial/ethnic groups persist in more recent birth-cohorts. While American Indian and Alaskan Native adults still have the highest rates of smoking, Hispanic adults have historically low smoking initiation and prevalence. Since the Hispanic population is driving much of US population growth,3 understanding these trends can help distinguish the impact of reduced smoking due to public health interventions from that of demographic turnover and change.4 Across cohorts, smoking prevalence among Non-Hispanic Black populations, particularly males, is lower than among Non-Hispanic White populations at younger ages, but higher at older ages. Despite Non-Hispanic Black cohorts’ relatively lower initiation rates, their low cessation rates compared to other groups suggest their need for improved cessation interventions. Estimates of cohort-specific smoking parameters for each of the racial/ethnic groups analyzed and interactive figures are available at apps.cisnetsmokingparameters.org/race/.
Education.
Although previous literature finds greater levels of education are linearly associated with lower smoking rates,5–8 Cao et al.9 find that the relationship between education and smoking in the US has the least educated (less than or equal to an 8th grade education) and most educated groups (a college degree or above) smoking at far lower rates compared to those in the middle (e.g., 9th to 11th grade, high school graduate or General Educational Development, or those with some college education). This pattern is partly driven by the increasing proportion of the non-U.S. born Hispanic population with less than or equal to an 8th grade education, indicating the need to especially consider this population in distinguishing tobacco use by education. Smoking disparities by education have also increased by birth cohort, with initiation rates highest among individuals with 9-11th grade education and lowest among individuals with at least a college degree in recent cohorts. These disparities reflect shifting societal norms as well as demographic composition. Larger shares of the young adult population are obtaining college degrees, which may reduce overall smoking but further concentrate smoking among the less educated. Estimates of cohort-specific smoking parameters by education and interactive figures are available at apps.cisnetsmokingparameters.org/education/.
Income.
Studies of historical smoking patterns by family income are difficult to interpret because of rising incomes and changing criteria for federal poverty thresholds. Jeon et. al.10 address this obstacle by calculating the ratio of individual family income to the federal poverty level adjusting for family size and structure and imputing missing income.11 Researchers analyzing historical trends in other health outcomes by family income can now adapt this methodology.4 Jeon et. al find that smoking prevalence and initiation probabilities across all income groups decreased while cessation probabilities increased. However, relative differences between low- and high-income groups are increasing, leading to greater declines in smoking prevalence among high-income groups in recent cohorts and increasing disparities.
Future modeling and trend analyses of smoking by income level should consider: 1) inflation-adjusted family incomes are rising over time reflecting increased labor market participation and income inequality; 2) estimates of income for youth or young adults often rely on parental income, which may be a poor proxy for their future incomes; and 3) survey results are sensitive to income questions and consequently subject to relatively high rates of missing data (ranging from 12-20%).12 While reliance on educational attainment as a measure for SES avoids some of these issues, education measures share the first two shortcomings. The studies on education and income both show the importance of information from more recent birth cohorts whose demographics, behaviors, and environments are more likely to represent that of future generations.4 Estimates of cohort-specific smoking parameters by income group and interactive figures are available at apps.cisnetsmokingparameters.org/income/.
U.S. States.
Holford et al.13 find vast differences in cohort-specific smoking behaviors by state. Exemplar findings from Kentucky and California show that age-specific initiation probabilities in Kentucky were consistently higher than in California across cohorts, with cessation rates higher in California for cohorts born after 1950. In subsequent cohorts, prevalence differences become more pronounced, resulting from Kentucky’s consistently lower cessation probabilities. Reasons for these disparities can be complex, reflecting differences in social norms, public policy, and sociodemographic composition. For example, Kentucky has lower SES on average than California, whereas California has been much more aggressive in its tobacco control policies (e.g. higher cigarette taxes, comprehensive smoke-free air laws). In addition, the size of the Hispanic population in California may contribute to their lower average smoking rates. However, estimates of the effect of different sociodemographic factors on smoking within each state are not yet available.
Many important tobacco control policies are decided at the state level.14 15 While none of the papers in this supplement have yet analyzed disparities at a state level, decision-makers, policy advocates, and researchers can use the data from their states as well as information from other papers on racial/ethnic and family income disparities to consider how policies may be directed at particular vulnerable groups in their state. The CISNET-LWG previously estimated the state-level impact of different tobacco control policies relying only on state-specific smoking prevalence data in its simulation models.15 Now those efforts can be improved with detailed state-specific information on smoking initiation, cessation, duration, intensity and pack-years. In addition, recent literature indicates that implementing cigarette taxes,16–23 increasing the minimum legal age of sale,24 25 and funding anti-smoking media campaigns26 may be efficacious in reducing smoking prevalence and initiation and promoting cessation in persons with (or whose parents had) low educational attainment as well as Non-Hispanic Black and Hispanic populations. However, other studies tend to find inconsistent or no evidence of differences by educational attainment or racial/ethnic identity,27–34 suggesting the need for further research. Analyses can then be conducted to compare smoking behaviors across multiple states, and to examine how policies impact geographic variations in smoking disparities.
State planners and researchers can view each state’s cohort-specific smoking behaviors at apps.cisnetsmokingparameters.org/states/.
Mortality
Differences in smoking behaviors by race/ethnicity and SES are not the only major contributors to smoking-related disparities; underlying differences in smoking-related mortality risk are also important drivers. Jeon et al. estimated all-cause mortality relative risk for current smokers, recent quitters, and long-term quitters compared to never smokers, specifically considering differences by race/ethnicity and education.35 Compared to never smokers, mortality relative risk among current smokers or recent quitters were generally highest for Non-Hispanic White individuals, followed by Non-Hispanic Black individuals, and lowest for Hispanic individuals. Notably, relative risks were substantially higher for smoking among high education compared to lower education groups, due in part to the lower overall mortality risks of never smokers among advantaged groups; i.e., for subpopulations with lower underlying mortality risk (e.g. high education, Non-Hispanic White populations), than for subpopulations that already have higher underlying mortality risk. Thus, relative risks do not correspond directly to disparities in smoking behaviors; lower relative risks were observed among lower education and Non-Hispanic Black populations with higher smoking rates. Beyond differences in smoking rates, underlying differences in mortality risk are important drivers of smoking-related disparities by race/ethnicity and education.
While the analysis suggests that smoking relative risk estimates are often lower for those with the highest smoking rates, the analysis, like earlier work,36 37 shows how both mortality risk and smoking behaviors determine health outcomes for specific racial/ethnic or education groups. In addition, reductions in smoking-attributable deaths among specific groups (e.g., due to a policy change) can be used to calculate the impact in reducing health disparities. For example, Issabaksch et al.38 estimated the impact of a menthol cigarette ban on Non-Hispanic Black smoking and smoking-related mortality.
Thus, policy planners can now obtain better mortality estimates to distinguish the roles of race/ethnicity and education in health outcomes and health disparities in policy evaluations. Simulation models and other analyses of public policy goals should carefully consider relative risk variations in evaluating the public health impact of smoking.35
Application of APC Analysis to other countries
Tam et al. apply the APC analytic approach to data from Brazil, marking the first time the CISNET methodology has been applied to a low or middle-income country.39 They found that male and female smoking prevalence declined considerably since the 1950 birth cohorts for males (1955 for females), reflecting decreased smoking initiation and increased smoking cessation rates. Among female cohorts born on or after 2000, smoking initiation may be increasing despite major increases in smoking cessation. Stagnating declines in smoking initiation among young women are consistent with adolescent surveys,40–43 indicating that smoking may be increasing among girls and young women. Slower progress in reducing smoking among recent birth cohorts also suggests that, despite Brazil being a leader in tobacco control,44 ongoing vigilance is needed so that reductions in smoking prevalence are not eroded by inaction. While Brazil has low smoking rates relative to other countries, the projections indicate that smoking rates may stop declining in the absence of additional policies. Estimates of cohort-specific smoking parameters for Brazil and interactive figures are available at apps.cisnetsmokingparameters.org/Brazil/.
As shown in this supplement and other CISNET-LWG work,45–48 each generation has its own unique experience of the tobacco epidemic, making data on birth cohort variations essential for developing reliable projections of future smoking trends. The Brazil analysis and earlier work by Manuel et al.49 applying this methodology to Canada demonstrate how the APC framework can be utilized across different country settings. The CISNET-LWG is currently conducting similar analyses for Mexico and Argentina in collaboration with local investigators. Unfortunately, many low- and middle-income countries share the same challenge, the lack of consistent nationally representative smoking surveillance data over time. For those countries with fewer available data points, alternative methods could be pursued. For example, individual countries may apply information from APC analyses of countries at similar stages in the tobacco epidemic50 and which have a similar tobacco product environment. For example, Levy et al.51 recently tailored CISNET-LWG US APC cohort projections to smoking trends in Australia to develop a simulation model of smoking trends for Australia. Similarly, relying on CISNET-LWG US cohort data, the US Smoking and Vaping Simulation model52 is now also being adapted and applied to other countries, such as Germany, and Japan.
Future Directions and Limitations
The rich smoking history data made available through this supplement offer a promising beginning for future surveillance and policy research in both domestic and global tobacco control efforts. Figure 1 provides a schema for applying the data to evaluate smoking trends across diverse settings. Researchers select the state or country setting of interest and begin the process by compiling the necessary population, smoking, mortality, morbidity, and policy data for modeling and trend analyses. The detailed smoking parameters (e.g. initiation, cessation, intensity, duration) published in this supplement can be used as direct inputs to tobacco simulation models for specific populations. Data permitting, simulation models can then be developed for subpopulations based on race/ethnicity, education, or family income. The simulation models would then project smoking rates and associated health outcomes across different sociodemographic groups. These models can compare health outcomes under different intervention scenarios, thereby quantifying the potential impact of past public health policies, or future ones.
Figure 1.
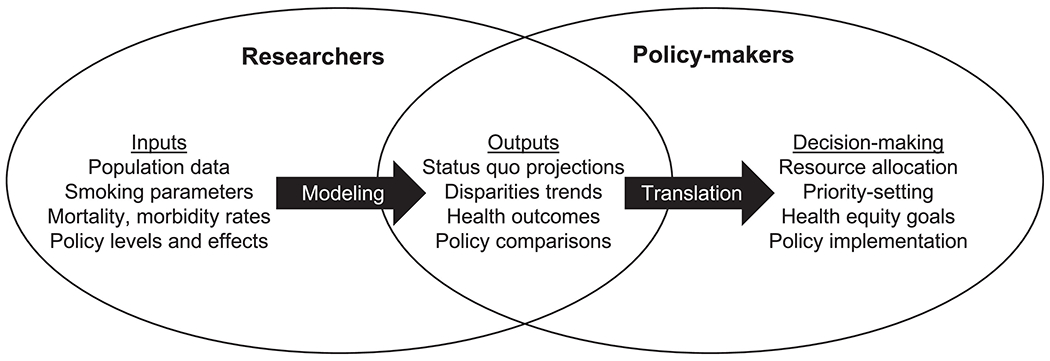
A Research and Policy Planning Strategy
The results may subsequently be used by policymakers to: 1) evaluate trends in smoking or in disparities between groups, 2) set public health goals, and 3) develop and prioritize policy strategies that reduce tobacco-related disease and death and improve health equity. The data produced and presented in this supplemental issue provides the inputs needed to conduct these analyses for the US, each of the 50 states and Washington DC, and Brazil. By developing APC analyses for different countries, modeling analyses can support World Health Organization tobacco control policy recommendations,53 54 assist with decision-making regarding resource allocation, and help to prioritize targeted interventions based on current model projections and patterns of tobacco use.
Although this paper and, more generally, this supplement has highlighted the potential for APC analyses to improve public health surveillance and tobacco control efforts, some key limitations to the APC approach should be acknowledged. APC analyses are only as reliable as the survey data on which they are built. The US analyses use data from the National Health Interview Survey and Tobacco Use Supplement to the Current Population Survey, both of which rely on self-reported smoking behavior, which may be subject to recall bias and underreporting. While the US has relatively large, continuous nationally representative surveys, low- or middle-income countries typically have far less data. In particular, other countries may not have sufficiently large samples to distinguish between sociodemographic groups, as necessary for subpopulation and disparities research.
Policy or market changes that occur during survey data collection periods can amplify small changes, particularly when the data are sparse. For example, initiation and cessation estimates for recent US birth cohorts (using data through 2018) indicate major changes, but because these estimates are based on limited information (i.e., the 2000 birth cohort only provides 18 years of data for the APC analysis), the analysis may be less reliable . Those in recent birth cohorts are also often the most directly impacted by changes in the tobacco market and policy environment because of their rising e-cigarette use.55–58 Although data for historical time-series analyses of e-cigarettes use are limited by their relatively recent entry, the smoking estimates for recent birth cohorts from the different studies in this supplement suggest that e-cigarette use and smoking declines are simultaneously occurring. Analyses by Levy et al.59 and Meza et al.60 suggest that one potential factor driving the remarkably large recent declines in US youth smoking may be e-cigarette use. In addition, cessation rates have likely changed because the dynamics of smoking histories61 62 have changed due in part also to the emergence of e-cigarettes in the tobacco product landscape.63 64 55–58
Thus, although data for historical time-series analyses of e-cigarettes use are limited by their relatively recent entry, the smoking estimates for recent birth cohorts from the different studies in this supplement hint at the future impact of e-cigarette use on declining smoking initiation and cessation patterns. However, while APC analyses reflect observed patterns in survey data, they cannot make causal inferences about what caused specific changes in smoking patterns. Beyond e-cigarettes, recent studies indicate that other nicotine delivery products may play an important role in future patterns of smoking, such as modern oral nicotine pouches65–67 and heated tobacco products.68 The CISNET-LWG is currently expanding its smoking models to consider e-cigarette use in the US.
The COVID-19 pandemic has also altered the behavioral landscape and likely impacted newer estimates.55 69 It is unclear whether COVID-19-related age, cohort, or period disruptions in tobacco use behaviors are temporary or have long-lasting implications for smoking trends. Given the potential to influence future projections, the short- and long-term role of the COVID-19 pandemic should be a priority area for future research inquiry.
Conclusions
This supplement has focused on identifying cohort patterns of smoking and related disparities in the US, while offering a preview for extension to low- and middle-income nations, starting with Brazil. States and countries with smaller populations and lower SES populations can now more easily benefit from simulation models adapted to their geographic contexts. To take full advantage of the smoking histories provided by this supplement, tobacco simulation models will also need additional estimates of policy effects on specific subpopulations, as well as appropriate mortality relative risk estimates.27–34 Moreover, modeling capacity is not necessarily available in local or resource-limited settings, so efforts are needed to build such capacity in affected communities. The publication of the detailed smoking histories in this supplemental issue is now publicly accessible for any interested individuals or groups to explore and download data. This supplement is only the first step in a series of efforts needed to translate findings from these data into policy decision tools that improve health and address disparities. The authors of this supplement invite the research and policy community to work together to make use of the vast data now available, and to meet the challenges ahead.
Conflict of interest statement:
This project was funded through National Cancer Institute (NCI) grants U01CA199284, U01CA253858 & U54CA229974. The study sponsor had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Footnotes
Financial disclosure: No financial disclosures were reported by the authors of this paper.
References
- 1.Tam J, Levy DT, Jeon J, et al. Using the past to understand the future of US and global smoking disparities: a birth cohort perspective. Am J Prev Med 2023. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meza R, Cao P, Jeon J, et al. Patterns of Birth Cohort-Specific Smoking Histories by Race and Ethnicity in the US. Am J Prev Med 2023;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Passel JS, Lopex MH, Cohn D. U.S. Hispanic population continued its geographic spread in the 2010s Washington, DC: Pew Foundation; 2022. [Available from: https://www.pewresearch.org/fact-tank/2022/02/03/u-s-hispanic-population-continued-its-geographic-spread-in-the-2010s/ accessed 2022 October 10. [Google Scholar]
- 4.Tam J, Warner KE, Gillespie BW, et al. Impact of changing U.S. demographics on the decline in smoking prevalence, 1980-2010. Nicotine Tob Res 2014;16(6):864–6. doi: 10.1093/ntr/ntt223. [DOI] [PubMed] [Google Scholar]
- 5.Zhu BP, Giovino GA, Mowery PD, et al. The relationship between cigarette smoking and education revisited: implications for categorizing persons’ educational status. Am J Public Health 1996;86(11):1582–9. doi: 10.2105/ajph.86.11.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huisman M, Kunst AE, Mackenbach JP. Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med 2005;40(6):756–64. doi: 10.1016/j.ypmed.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Pampel FC, Denney JT. Cross-national sources of health inequality: education and tobacco use in the World Health Survey. Demography 2011;48(2):653–74. doi: 10.1007/s13524-011-0027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi K, Jones JT, Ruybal AL, et al. Trends in education-related smoking disparities among U.S. Black/African American and White adults: Intersections of race, sex, and region. Nicotine Tob Res 2022. doi: 10.1093/ntr/ntac238 [published Online First: 2022/October/15]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao P, Jeon J, Tam J, et al. Smoking Disparities by Level of Educational Attainment and Birth Cohort in the US. Am J Prev Med 2023;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeon J, Cao P, Fleischer NL, et al. Birth Cohort-Specific Smoking Patterns by Family Income in the US. Am J Prev Med 2023;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.University of Michigan SRC. IVEware: Imputation and Variance Estimation Software 2021. [Available from: https://www.src.isr.umich.edu/software/iveware/ accessed December 23 2021.
- 12.Jeon J, Cao P, Fleischer N, et al. Birth Cohort-Specific Smoking Patterns by Family Income in the US. Am J Prev Med in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holford TR, McKay L, Jeon J, et al. Smoking Histories by State in the US. Am J Prev Med 2023;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy DT, Tam J, Kuo C, et al. The Impact of Implementing Tobacco Control Policies: The 2017 Tobacco Control Policy Scorecard. J Public Health Manag Pract 2018;24(5):448–57. doi: 10.1097/PHH.0000000000000780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tam J, Levy DT, Jeon J, et al. Projecting the effects of tobacco control policies in the USA through microsimulation: a study protocol. BMJ open 2018;8(3):e019169. doi: 10.1136/bmjopen-2017-019169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fleischer NL, Donahoe JT, McLeod MC, et al. Taxation reduces smoking but may not reduce smoking disparities in youth. Tob Control 2021;30(3):264–72. doi: 10.1136/tobaccocontrol-2019-055478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalousova L, Levy D, Titus AR, et al. Cigarette taxes, prices, and disparities in current smoking in the United States. SSM Popul Health 2020;12:100686. doi: 10.1016/j.ssmph.2020.100686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parks MJ, Patrick ME, Levy DT, et al. Tobacco Taxation and Its Prospective Impact on Disparities in Smoking Initiation and Progression Among Young Adults. J Adolesc Health 2021;68(4):765–72. doi: 10.1016/j.jadohealth.2020.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parks MJ, Patrick ME, Levy DT, et al. Cigarette Pack Price and Its Within-Person Association With Smoking Initiation, Smoking Progression, and Disparities among Young Adults. Nicotine Tob Res 2022;24(4):519–28. doi: 10.1093/ntr/ntab210 [published Online First: 2021/October/12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeCicca P, McLeod L. Cigarette taxes and older adult smoking: evidence from recent large tax increases. J Health Econ 2008;27(4):918–29. doi: 10.1016/j.jhealeco.2007.11.005 [published Online First: 2008/January/08] [DOI] [PubMed] [Google Scholar]
- 21.Le TTT, Jaffri MA. The association between smoking behaviors and prices and taxes per cigarette pack in the United States from 2000 through 2019. BMC Public Health 2022;22(1):856. doi: 10.1186/s12889-022-13242-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keeler C, Wang Y, Max W, et al. The Association of California’s Proposition 56 Tobacco Tax Increase With Smoking Behavior Across Racial and Ethnic Groups and by Income. Nicotine Tob Res 2021;23(12):2091–101. doi: 10.1093/ntr/ntab130. [DOI] [PubMed] [Google Scholar]
- 23.Sharbaugh MS, Althouse AD, Thoma FW, et al. Impact of cigarette taxes on smoking prevalence from 2001-2015: A report using the Behavioral and Risk Factor Surveillance Survey (BRFSS). PLoS One 2018;13(9):e0204416. doi: 10.1371/journal.pone.0204416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colston DC, Xie Y, Patrick ME, et al. Tobacco 21 laws may reduce smoking and tobacco-related health disparities among youth in the U.S. Prev Med Rep 2022;27:101762. doi: 10.1016/j.pmedr.2022.101762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grube JW, Lipperman-Kreda S, Garcia-Ramirez G, et al. California’s tobacco 21 minimum sales age law and adolescents’ tobacco and nicotine use: differential associations among racial and ethnic groups. Tob Control 2021. doi: 10.1136/tobaccocontrol-2020-056219 [published Online First: 2021/July/02]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burns EK, Levinson AH. Reaching Spanish-speaking smokers: state-level evidence of untapped potential for QuitLine utilization. Am J Public Health 2010;100 Suppl 1:S165–710. doi: 10.2105/AJPH.2009.166322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colston DC, Cho B, Thrasher JF, et al. Anti-Smoking Media Campaigns and Disparities in Smoking Cessation in the United States, 2001-2015. Am J Health Promot 2021;35(5):658–68. doi: 10.1177/0890117120985818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colston DC, Xie Y, Thrasher JF, et al. Exploring How Exposure to Truth and State-Sponsored Anti-Tobacco Media Campaigns Affect Smoking Disparities among Young Adults Using a National Longitudinal Dataset, 2002-2017. Int J Environ Res Public Health 2021;18(15) doi: 10.3390/ijerph1815780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slocum E, Xie Y, Colston DC, et al. Impact of the Tips from Former Smokers Anti-Smoking Media Campaign on Youth Smoking Behaviors and Anti-Tobacco Attitudes. Nicotine Tob Res 2022. doi: 10.1093/ntr/ntac152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agaku IT, Nkosi L, Agaku QD, et al. A Rapid Evaluation of the US Federal Tobacco 21 (T21) Law and Lessons From Statewide T21 Policies: Findings From Population-Level Surveys. Prev Chronic Dis 2022;19:E29. doi: 10.5888/pcd19.210430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flynn BS, Worden JK, Bunn JY, et al. Mass media interventions to reduce youth smoking prevalence. Am J Prev Med 2010;39(1):53–62. doi: 10.1016/j.amepre.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vallone DM, Perks SN, Pitzer L, et al. Evidence of the impact of a national anti-tobacco prevention campaign across demographic subgroups. Health Educ Res 2022;36(4):412–21. doi: 10.1093/her/cyab025. [DOI] [PubMed] [Google Scholar]
- 33.MacLean JC, Kessler AS, Kenkel DS. Cigarette Taxes and Older Adult Smoking: Evidence from the Health and Retirement Study. Health Econ 2016;25(4):424–38. doi: 10.1002/hec.3161. [DOI] [PubMed] [Google Scholar]
- 34.Yao T, Ong MK, Max W, et al. Responsiveness to cigarette prices by different racial/ethnic groups of US adults. Tob Control 2018;27(3):301–09. doi: 10.1136/tobaccocontrol-2016053434. [DOI] [PubMed] [Google Scholar]
- 35.Jeon J, Inoue-Choi M, Mok Y, et al. Relative Risk of All-Cause Mortality by Smoking Status, Race/Ethnicity, and Education in the United States Am J Prev Med 2023;In Press. [Google Scholar]
- 36.Carter-Pokras O, Baquet C. What is a" health disparity"? Public health reports 2002;117(5):426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Braveman P. What are health disparities and health equity? We need to be clear. Public health reports 2014;129(1_suppl2):5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Issabakhsh M, Meza R, Li Y, et al. Public health impact of a US menthol cigarette ban on the non-Hispanic black population: a simulation study. Tobacco control 2022. doi: 10.1136/tobaccocontrol-2022-057298 [published Online First: 2022/June/15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tam J, Jaffri M, Mok Y, et al. Patterns of Birth Cohort-Specific Smoking Histories in Brazil. Am J Prev Med 2023; In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúde do Escolar: 2012: Rio de Janeiro: IBGE; 2013. [Google Scholar]
- 41.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúde do Escolar: 2015: Rio de Janeiro: IBGE; 2016. [Google Scholar]
- 42.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúde do Escolar: 2019: Rio de Janeiro: IBGE; 2021. [Google Scholar]
- 43.PeNSE: Pesquisa Nacional de Saude do Escolar 2021 [Available from: https://www.ibge.gov.br/en/statistics/social/health/16837-national-survey-of-school-health-editions.html?=&t=resultados accessed 07/20 2022.
- 44.Levy D, de Almeida LM, Szklo A. The Brazil SimSmoke policy simulation model: the effect of strong tobacco control policies on smoking prevalence and smoking-attributable deaths in a middle income nation. PLoS Med 2012;9(11):e1001336. doi: 10.1371/journal.pmed.1001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holford TR, Levy DT, McKay LA, et al. Patterns of birth cohort-specific smoking histories, 1965-2009. Am J Prev Med 2014;46(2):e31–7. doi: 10.1016/j.amepre.2013.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964-2012. JAMA 2014;311(2):164–71. doi: 10.1001/jama.2013.285112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jeon J, Holford TR, Levy DT, et al. Smoking and Lung Cancer Mortality in the United States From 2015 to 2065: A Comparative Modeling Approach. Ann Intern Med 2018;169(10):684–93. doi: 10.7326/M18-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moolgavkar SH, Holford TR, Levy DT, et al. Impact of reduced tobacco smoking on lung cancer mortality in the United States during 1975-2000. J Natl Cancer Inst 2012;104(7):541–8. doi: 10.1093/jnci/djs136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manuel DG, Wilton AS, Bennett C, et al. Smoking patterns based on birth-cohort-specific histories from 1965 to 2013, with projections to 2041. Health Rep 2020;31(11):16–31. doi: 10.25318/82-003-x202001100002-eng. [DOI] [PubMed] [Google Scholar]
- 50.Thun M, Peto R, Boreham J, et al. Stages of the cigarette epidemic on entering its second century. Tob Control 2012;21(2):96–101. doi: 10.1136/tobaccocontrol-2011-050294. [DOI] [PubMed] [Google Scholar]
- 51.Levy DT, Gartner C, Liber AC, et al. The Australia Smoking and Vaping Model: The Potential Impact of Increasing Access to Nicotine Vaping Products. Nicotine Tob Res 2022. doi: 10.1093/ntr/ntac210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Levy DT, Tam J, Sanchez-Romero LM, et al. Public health implications of vaping in the USA: the smoking and vaping simulation model. Popul Health Metr 2021;19(1):19. doi: 10.1186/s12963-021-00250-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Levy DT, Li Y, Yuan Z. Impact of nations meeting the MPOWER targets between 2014 and 2016: an update. Tobacco control 2020;29(2):231–33. doi: 10.1136/tobaccocontrol-2018-054837. [DOI] [PubMed] [Google Scholar]
- 54.Levy DT, Yuan Z, Luo Y, et al. Seven years of progress in tobacco control: an evaluation of the effect of nations meeting the highest level MPOWER measures between 2007 and 2014. Tobacco control 2018;27(1):50–57. doi: 10.1136/tobaccocontrol-2016-053381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gentzke AS, Wang TW, Cornelius M, et al. Tobacco Product Use and Associated Factors Among Middle and High School Students - National Youth Tobacco Survey, United States, 2021. MMWR Surveill Summ 2022;71(5):1–29. doi: 10.15585/mmwr.ss7105a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gentzke AS, Wang TW, Jamal A, et al. Tobacco Product Use Among Middle and High School Students - United States, 2020. MMWR Morb Mortal Wkly Rep 2020;69(50):1881–88. doi: 10.15585/mmwr.mm6950a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang TW, Gentzke AS, Creamer MR, et al. Tobacco Product Use and Associated Factors Among Middle and High School Students - United States, 2019. MMWR Surveill Summ 2019;68(12):1–22. doi: 10.15585/mmwr.ss6812a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Park-Lee E, Ren C, Cooper M, et al. Tobacco Product Use Among Middle and High School Students - United States, 2022. MMWR Morbidity and mortality weekly report 2022;71(45):1429–35. doi: 10.15585/mmwr.mm7145a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Levy DT, Warner KE, Cummings KM, et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tobacco control 2019;28(6):629–35. doi: 10.1136/tobaccocontrol-2018-054446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meza R, Jimenez-Mendoza E, Levy DT. Trends in Tobacco Use Among Adolescents by Grade, Sex, and Race, 1991-2019. JAMA Netw Open 2020;3(12):e2027465. doi: 10.1001/jamanetworkopen.2020.27465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mendez D, Tam J, Giovino GA, et al. Has smoking cessation increased? An examination of the US Adult Smoking Cessation Rate 1990-2014. Nicotine & Tobacco Research 2017;19(12):1418–24. doi: 10.1093/ntr/ntw239 [DOI] [PubMed] [Google Scholar]
- 62.Jeon J, Holford TR, Levy DT, et al. Smoking and Lung Cancer Mortality in the United States from 2015 to 2065. Ann Intern Med 2018;169(10):684–93. doi: 10.7326/M18-1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brouwer AF, Jeon J, Cook SF, et al. The impact of menthol cigarette flavor in the U.S.: Cigarette and ENDS transitions by sociodemographic group. Am J Prev Med 2022;62(2):243–51. doi: 10.1016/j.amepre.2021.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gentzke A, Creamer M, Cullen K, et al. Vital Signs: Tobacco Product Use Among Middle and High School Students — United States. MMWR Morb Mortal Wkly Rep 2019;68:157–64. doi: 10.15585/mmwr.mm6806e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marynak K, Emery S, King BA. Nicotine Pouch Unit Sales in the US From 2016 to 2020-Reply. JAMA 2021;326(22):2331. doi: 10.1001/jama.2021.19056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Delnevo CD, Hrywna M, Miller Lo EJ, et al. Examining Market Trends in Smokeless Tobacco Sales in the United States: 2011-2019. Nic Tobacco Res 23(8):1420–24. doi: 10.1093/ntr/ntaa239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O’Connor R, Schneller LM, Felicione NJ, et al. Evolution of tobacco products: recent history and future directions. Tobacco control 2022;31(2):175–82. doi: 10.1136/tobaccocontrol-2021-056544 [DOI] [PubMed] [Google Scholar]
- 68.Levy DT, Cadham CJ, Li Y, et al. A Decision-Theoretic Public Health Framework for Heated Tobacco and Nicotine Vaping Products. International journal of environmental research and public health 2022;19(20). doi: 10.3390/ijerph192013431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bandi P, Asare S, Majmundar A, et al. Changes in Smoking Cessation-Related Behaviors Among US Adults During the COVID-19 Pandemic. JAMA Netw Open 2022;5(8):e2225149. doi: 10.1001/jamanetworkopen.2022.25149. [DOI] [PMC free article] [PubMed] [Google Scholar]


