Abstract
Rationale & Objective:
Infection prevention efforts in dialysis centers can avert patient morbidity and mortality but are challenging to implement. The objective of this study was to better understand how the design of the work system might contribute to infection prevention in outpatient dialysis centers.
Study Design:
Mixed methods, observational study.
Setting & Participants:
Six dialysis facilities across the United States visited by a multidisciplinary team over 8 months.
Analytical Approach:
At each facility, structured macroergonomic observations were undertaken by a multidisciplinary team using the SEIPS 1.0 model. Ethnographic observations were collected about staff encounters with dialysis patients including the content of staff conversations. Selective and axial coding were used for qualitative analysis and quantitative data were reported using descriptive statistics.
Results:
Organizational and sociotechnical barriers and facilitators to infection prevention in the outpatient dialysis setting were identified. Features related to human performance, (eg, alarms, interruptions, and task stacking), work system design (eg, physical space, scheduling, leadership, and culture), and extrinsic factors (eg, patient-related characteristics) were identified.
Limitations:
This was an exploratory evaluation with a small sample size.
Conclusions:
This study used a systematic macroergonomic approach in multiple outpatient dialysis facilities to identify infection prevention barriers and facilitators related to human performance. Several features common across facilities were identified that may influence infection prevention in outpatient care and warrant further exploration.
Infections remain the second leading cause of mortality in patients receiving dialysis.1,2 The Centers for Disease Control and Prevention (CDC) has provided evidence-based recommendations and best practices to prevent infections in dialysis patients.3 Staff adherence to recommended practices is often imperfect, and failure to adhere has been recognized as a contributing factor in the occurrence of dialysis-related infections.4–6
To better understand these departures from best practice and related barriers and facilitators to infection prevention, the CDC and the American Society of Nephrology (ASN) initiated a national taskforce, Nephrologists Transforming Dialysis Safety (NTDS), with the goal of “Targeting Zero Infections” within outpatient dialysis facilities.7 These groups further sought to understand the infection prevention-related behaviors of individuals within the dialysis work setting in order to develop more sustainable solutions.
Human factors engineering (HFE) focuses on understanding human capabilities and limitations, whether they be cognitive, interpersonal, or physical, and promotes use of that knowledge to inform the design of work, environment, or technology so that the work is designed to fit the human. There are 3 core elements of the field of HFE: (1) using a systems-oriented perspective (rather than individual or team-oriented), (2) focusing on the design of the system and its impact to human performance, and (3) seeking joint optimization of human performance and human well-being.8 The idea that larger organizational context and sociotechnical systems influence patient safety and quality of care has led to the integration of macroergonomics into health care quality and patient/employee safety initiatives.9,10 The field of macroergonomics and systems science has shown that there are significant, complex issues within the design of our systems of care that also influence human performance and outcomes.11–13 Macroergonomics, an area of study within the field of human factors, explores the organizational and sociotechnical context of work activities and processes to align with these core elements.14 A macroergonomic approach involves acknowledgment of specific problems while identifying system-level influences on lower-level phenomena.15
Different macroergonomic models, such as the Systems Engineering Initiative for Patient Safety11 (SEIPS) or SocioTechnical Systems (STS) model, have been widely used to explore the impact of systems factors on frondine health care work.11,16–19 To gain insight into the system influences on provider and patient performance, SEIPS evaluates 5 unique aspects of a system: organization, people, task, technology, and physical environment. Interactions of each of these aspects are evaluated as they relate to clinical care processes and outcome measures. Specifically, there has been work focused on applications of macroergonomic approaches within dialysis to show the feasibility of exploring infection prevention using this approach.20
A gap remains between the insights developed through systems-based approaches and actual practice change. In this exploratory evaluation, we sought to better understand how the design of the work system influences adherence to infection prevention standards in dialysis facilities. The overarching purpose of this work is to provide a qualitative foundation that could inform future interventions that might improve adherence to recommended infection prevention practices.
Methods
A mixed-method exploratory evaluation was conducted with a convenience sample of 6 outpatient dialysis centers across the United States from August 2018 to April 2019. A separate initial pilot-facility visit was conducted to test the data collection tools and help better understand the logistical issues of a dialysis center (eg, where in a dialysis facility to stand to conduct observations but not interrupt patient care). The initial pilot facility data were not included in the analysis. The centers were recruited through ASN representatives (K.A.L., A.S.K., R.E.G., and others) via an online sign-up portal. The online sign-up asked about patient population, location, and willingness to host the team. Our goal was to include large dialysis organizations (LDOs), small dialysis organizations, for-profit and not-for-profit facilities, academic and nonacademic, and adult and pediatric units. If a center expressed interest, ASN representatives worked directly with leadership from each site and then with legal representatives and others to ensure that all concerns were addressed.
At all facility visits, the team included 3 human factors engineers, and a minimum of 1 expert in dialysis infection prevention, 1 nephrologist, and 1 nephrology nurse. The facilities included both pediatric and adult outpatient dialysis centers, those owned by large for-profit and not-for-profit dialysis organizations, and an academic center. For most of the participating sites, NTDS leaders volunteered their own facility; for some of the facilities, the NTDS member was also a dialysis organization leader and connected us with a facility within their organization. A connection was made with the nurse manager and medical director of the facility in advance of the visit, and ASN staff collaborated on details of the visit with the nurse manager. The facilities were notified in advance, and dates were planned with the facilities.
Structured observations were obtained using the SEIPS 1.0 model. We chose SEIPS because of its health care origins, and chose 1.0 as the simplest representation of the interconnected macroergonomic factors. Encounters were defined as a staff member entering the patient’s dialysis station to perform a task with the dialysis patient or with the associated equipment in the patient station. The “patient dialysis station” was defined as the immediate vicinity of the dialysis chair, chairside table, dialysis machine, and/or adjacent computer station. Definitions of the terms used in this approach are described in Table 1.
Table 1.
Definition of Terms
| Term | Definition | Example |
|---|---|---|
| Encounter | A staff member entering the patient’s dialysis station area (within vicinity of dialysis chair, chairside table, dialysis machine, computer station) to perform a task with the dialysis patient or their equipment. | Staff member walks into a patient station to silence an alarm. |
| Process | An activity that may include several tasks that need to be completed to be successful. There were 4 processes of interest (disinfection of the patient station, hand hygiene, injection safety, and CVC/ vascular access care) covered in our observations. Tasks within a process may occur inside or outside of the dialysis station. | Routine disinfection of the dialysis station is a process with many tasks. They all need to be completed to be successful. |
| Task | An activity that a staff member must do to complete a process. One process can contain multiple tasks. | Disinfecting the dialysis chair is 1 task in the routine disinfection process. |
| Task stacking | Performing 2 or more tasks simultaneously. | Wiping down part of the dialysis chair without finishing, pausing to turn off the dialysis machine, clicking into the medical record, and then going back to finish wiping down the chair. |
| Distraction | Whenever something causes staff members to pause or stop the task they are performing (could be physical or cognitive). | A coworker asks for help while a staff member is in the middle of performing a different action (process or task). |
| Interruption | Interruptions take the staff member’s attention away from the primary task and can be valuable or nonvaluable. | A staff member pauses his or her primary task to assist a coworker in another station or to address an alarm. |
| Alarm | Any audible noise alarm in or outside of an individual patient station made by equipment during an encounter. An alarm may cause a distraction. | A dialysis machine beeps when something is wrong, and it needs to be checked. |
Abbreviation: CVC, central venous catheter.
Several types of data were collected. First, structured and unstructured ethnographic observations were conducted on the treatment floor. Ethnography is a method used in social and behavioral sciences in which observations of individuals are gathered in their natural environment rather than in a laboratory. The goal of an ethnographic approach is to gain insight into how individuals interact in their natural environment. Second, qualitative information was gathered from staff conversations as a group or individually.
Finally, direct environmental data (eg, quantitative measurements of noise and lighting using consumer apps) were captured. The data collection focused on 4 infection prevention processes: environmental disinfection of the dialysis station, hand hygiene, injection safety (ie, injectable medication preparation and administration), and central venous catheter (CVC) and arteriovenous vascular access (fistulae/graft) care. These processes have been identified as central to infection prevention.21
During observations of these processes, we assessed and identified system components such as human factors, work system factors, and extrinsic factors (Table 2). Human factors are those issues that are intrinsic to humans and impact their performance. Here we highlight distractions (ie, interruptions, alarms), task stacking, and perceived differences between what items are considered “clean” and what are “dirty” and when. Work system factors are those that impact human performance but are not intrinsic to individuals. These factors are part of the design of the work system, including contributions of the physical environment, workflow scheduling, and policies and procedures. Extrinsic factors are those that are outside the control of the individual or work system.
Table 2.
System Components Used for Categorizing Results
| System Component | Data Collected | Rationale for Data Collection |
|---|---|---|
| Human factors | Interruptions | If a person is interrupted, it could disrupt a task sequence and increase the risk of error. |
| Alarms | Alarms can be necessary, but they can also interrupt a task sequence and lead to alarm fatigue. | |
| Task stacking | Simultaneously performing more than 1 task can lead to interruptions in task sequence and cognitive overload. | |
| Clean and dirty delineation | Determining and understanding what is clean and dirty and at what moment are critical to infection prevention. | |
| Work system factors | Physical environment | The layout of equipment and supplies can influence efficiency, motion, noise, and distractions. |
| Workflow scheduling | Patient schedules are created and designed based on prescriptions but may be adjusted according to extrinsic factors. | |
| Policies and procedures | Policies, procedures, and checklists do not necessarily reflect the work tasks as performed. | |
| Culture/leadership engagement | Engaged management who are available for support and escalation of problems can improve resources and stress levels of staff. | |
| Extrinsic factors | Patient factors | Factors related to individual patient characteristics and psychosocial needs can affect infection risk. Patient-specific treatment and transportation-related variables can influence work processes and flow. |
Objective, quantitative observations, such as time on task, were recorded in the TimeCaT 3.9 application (HICAPPS SpA). Structured observations were also conducted specifically on the task of environmental disinfection using link analysis, which is a method to track the time and motion of staff. Unstructured ethnographic observations were manually recorded with paper and pencil.11,16‘18 Routine care was observed at patient stations (such as catheter care). If observed, tasks not directly related to the 4 process areas of focus were also recorded (eg, adjusting dialysis machine settings, gathering supplies, completing routine patient assessments, documenting in the electronic medical record, silencing an alarm, or visualizing a patient’s blood lines). Observers identified system design factors that might influence staff performance on infection prevention tasks, thereby mitigating or escalating the risk of an avoidable infection. The observations were not intended to assess for “errors” per se but rather to gather objective and subjective information regarding the work-system of the facility.
To assess staff perceptions of safety and infection prevention, facility staff were engaged in semistructured conversations. Open-ended questions were posed to elicit system or work culture challenges and facilitators perceived by staff. During observations on the treatment floor, brief inquiries to the staff may have been made. These inquiries were semistructured and focused on staff-reported challenges or facilitators related to infection prevention.
The team conducted exit discussions with facility leadership and issued each a follow-up summary of our observations and the opportunity to discuss the report with the research team. These conversations were led by individuals with experience in quality improvement and patient safety (S.H.P., L.D.W.), with significant attention paid to how the feedback was framed and might he received. Facility reports were not binding in any way to participation in this study, did not include individual staff or patient identifying information, and were not shared publicly.
This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy (45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241 (d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.). Virginia Tech’s institutional review board determined this work to be not human subjects research (18–911).
Analysis
TimeCaT 3.9 data included time stamps and task information that were analyzed using descriptive statistics. Hand hygiene, alarm, and interruption occurrences (per minute) were calculated where appropriate to facilitate comparison. Standard link analyses to objectively track and describe the interactions between the staff and the physical layout of their working environment were performed at each facility. Qualitative data from staff conversations were analyzed using selective and axial coding.22 We did not conduct statistical analyses to determine the significance of the components; rather, we report observations as high-level, qualitative results.
Results
Over the course of approximately 2.5 days per facility, a total of 157.5 hours of facility observations were conducted. Observations occurred across hours of facility operations, including early morning start and evening shift (Table 3).
Table 3.
Facility Visit Information and Observation Data
| Observation Data | Facilitya | ||||||
|---|---|---|---|---|---|---|---|
| B | C | D | E | F | G | Total | |
| Days at facility | 3 | 2 | 3 | 3 | 3 | 3 | 17 |
| Hours of observation | 23 | 23 | 28 | 30 | 35 | 19 | 158 |
| No. of encounters | 74 | 61 | 104 | 72 | 86 | 82 | 479 |
| No. of link analyses | 10 | 5 | 8 | 6 | 7 | 6 | 42 |
Facility A was a pilot facility and was intentionally left out of the analysis data set.
Human Factors
Interruptions
Of all encounters observed (n = 479), 92 encounters (19%) had 1 or more interruptions. Of the 92 encounters with an interruption, 42 encounters (45.7%) had 2 or more interruptions. Examples of interruptions included a coworker requesting assistance or a phone call that took the caregiver away from the primary task.
Alarms
The average time for a patient to be connected to start treatment was 14 minutes; the mean number of alarms that occurred during that interval was 1.95 ± 2.49 SD. Of all encounters observed (N = 479), 243 encounters (50.7%) had 1 or more alarms occur. Staff comments reinforced the notion that alarms were prevalent and disruptive. One staff member identified that “the machine at the next station [alarms, which] causes you to grab a glove and poke at the machine, but then you have to change the glove.” Another individual stated, “The machine alarms before we have time to prep catheter ports during disconnection,” suggesting a misalignment between machine programs and corresponding work processes. A technician observed, “It’s like babysitting a child, you’ve got to calm it down and then ask nicely” when referring to the alarm frequency and utility.
Table 4 describes interruption events (alarms and interruptions) during connection, disconnection, medication administration, and disinfection of the station.
Table 4.
Description of Encounters and Interruption Events During Infection Prevention Processes Within the Patient Station (N = 275)
| Average Occurrences per Encounter |
Occurrences per Minute |
|||||||
|---|---|---|---|---|---|---|---|---|
| Process | Encounters (n) | Time on Task | Hand Hygiene | Alarms | Interruptions | Hand Hygiene | Alarms | Interruptions |
|
| ||||||||
| Connectiona | 93 | 14:15 ± 07:08 | 4.66 ± 3.95 | 1.95 ± 2.49 | 0.86 ± 1.51 | 0.33 ± 0.28 | 0.14 ± 0.18 | 0.07 ± 0.11 |
| Disconnectiona | 92 | 11:42 ± 08:11 | 3.03 ± 3.11 | 2.29 ± 2.75 | 0.87 ± 1.62 | 0.26 ± 0.27 | 0.2 ± 0.24 | 0.08 ± 0.14 |
| Injection administration | 35 | 04:43 ± 11:22 | 1.20 ± 1.30 | 0.14 ± 0.43 | 0.20 ± 0.47 | 0.26 ± 0.28 | 0.04 ± 0.1 | 0.05 ± 0.11 |
| Disinfection of the patient station | 55 | 05:45 ± 04:15 | 1.35 ± 1.19 | 0.33 ± 0.58 | 0.33 ± 0.89 | 0.24 ± 0.21 | 0.06 ± 0.11 | 0.07 ± 0.16 |
Values for continuous variables given as mean ± SD. Of the total encounters (N = 479), 275 were related to these infection prevention processes.
Central venous catheter, fistula, or graft.
Task Stacking
When staff were performing 1 task, they were also simultaneously performing 1 or more additional tasks (task stacking) about 76% of the time (Fig 1). Individuals performed a single task just 24% of the time across all observed encounters.
Figure 1.
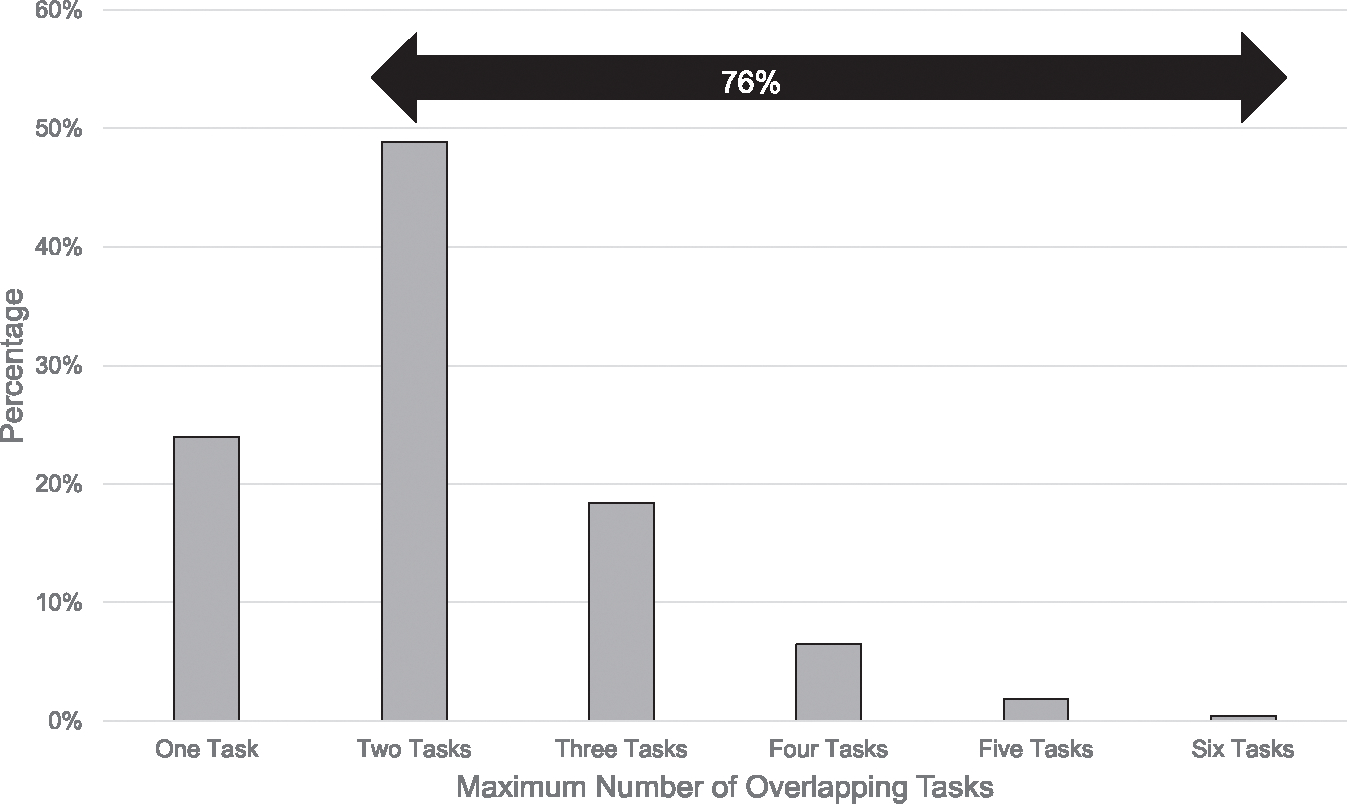
Percent of encounters by maximum number of overlapping tasks performed by the staff member (N = 479). During 76% of encounters observed, staff performed 2 or more tasks simultaneously (task stacking).
Understanding of “Clean” and “Dirty”
The terms “clean” and “dirty” are used by staff to describe a wide array of different items, surfaces, and areas within the facility (eg, the handwashing sink is labeled “dean sink” while sinks used to soak hemostat damps are labeled “dirty sink”). The delineation between dean versus dirty spaces and items was noted by many staff to be inconsistent, process dependent, and temporally driven, making infection prevention and hand hygiene policies and procedures difficult to understand and follow. For example, during one observation, a staff member asked, “How is it possible that the computer between patient stations is dean? It’s not—it could be cross contaminated. Is it considered dean? I don’t know.” Staff repeatedly expressed that it was not dear why something was considered dean or dirty. “[Going from] patient [contact] to machine [contact] is considered dirty to dirty; however, [going from] machine [contact] to patient [contact] is considered dean to dirty.” “[You] can’t set up the dialysis machine until patient in the station leaves, but there’s another patient sitting on the other side [equidistant away], so why is that different?” When some staff were asked, “What are your triggers to know when to do hand hygiene?” the responses were inconsistent and nonspecific: “Whenever I feel like I need to,” or “Whenever I enter or leave the station.”
Work System Factors
Physical Environment
Link analysis showed wide variation in work practices; for example, a staff member in one facility required 24 links (physical motions between equipment) while a staff member at another facility required 12 links to complete environmental disinfection of the dialysis station (Fig 2). Differences such as these could be the result of variation in the facility policies, layout, equipment, interruptions, preferences of the individual staff performing the procedures, and/or other factors. No judgment about the quality of cleanliness (thoroughness or completeness) can be inferred because no measure of cleanliness was assessed.
Figure 2.
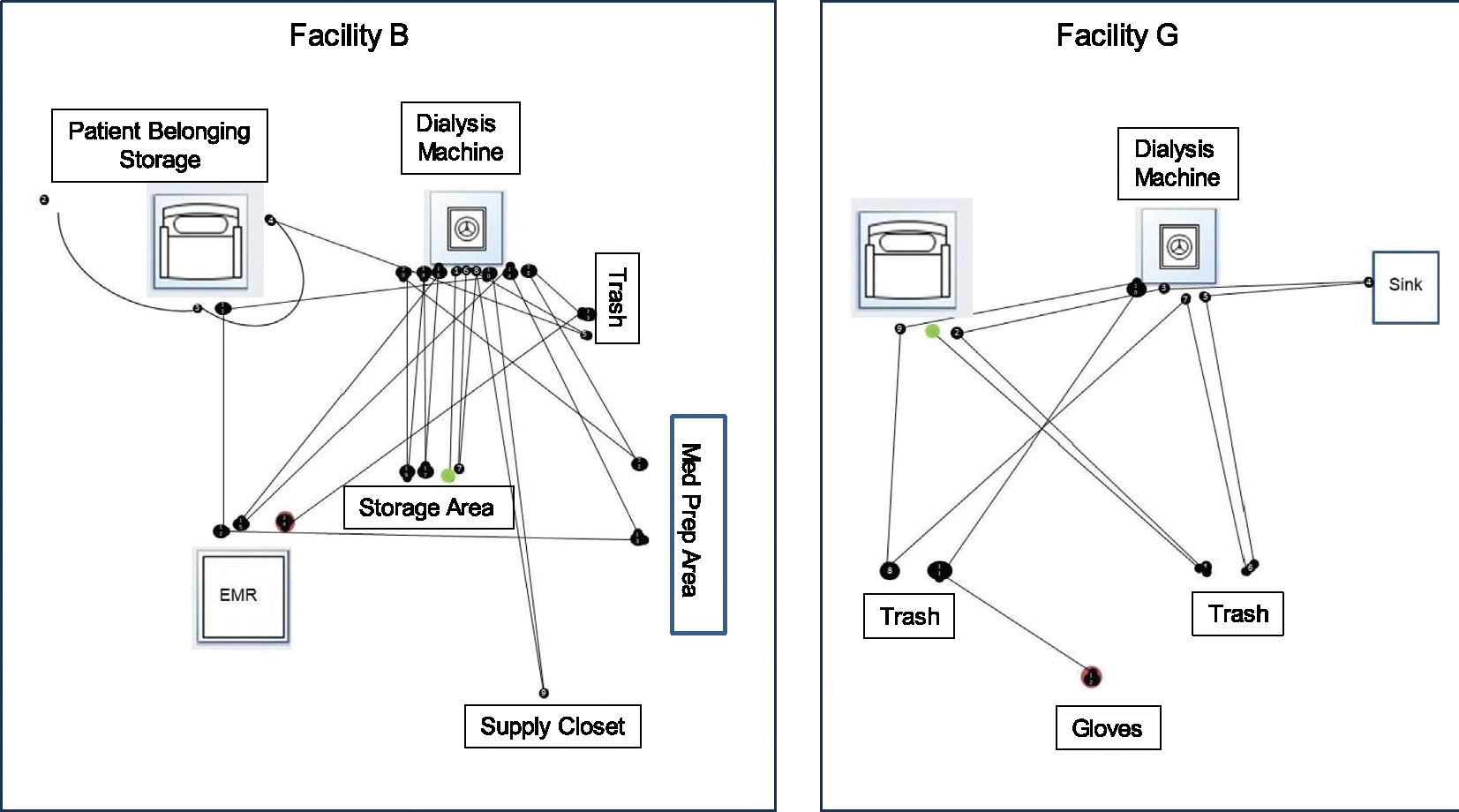
Link analysis visually capturing staff motion through the facility to complete environmental disinfection of the dialysis station in 2 facilities. Differences such as these could be the result of variation in the facility policies, layout, interruptions, and/or preferences of the individual staff performing the procedures.
Several elements of the physical design were identified as possible barriers or facilitators to infection prevention. At one facility, a staff member was observed to be unable to open the dialysis chair sections to perform environmental disinfection due to the arms of the chair being too close to an adjacent wall. As a result, the staff member could not physically reach interior-facing surfaces of the chair. Another example of the influence of the physical space design is the use of clocks during catheter hub disinfection. Easily visible clocks were available at some facilities, and the team observed staff using them to time disinfection of the catheter hub during CVC care.
Several staff members described machine alarms and facility noise as “disruptive” and as “a distraction” from the task at hand. Sometimes organizational factors combine to make it difficult to achieve hand hygiene goals. For example, a technician’s ability to perform hand hygiene is influenced by organization-level constraints such as how many patients that individual is assigned to care for and the location of the hand sanitizer in accordance with workflows.
Workflow Scheduling
Staff described a lack of alignment between the workflows anticipated in facility policies and the “real time” workflows of the facility. Patient scheduling was observed to be very rigidly timed, and limited flexibility in turnover time was identified at multiple centers. Although intervening events such as transportation delays, treatment interruptions for patients’ needs, difficulty with access cannulation and/or delayed hemostasis were routinely observed, extra time was not routinely allotted for such occurrences.
As shown in Figure 3, patient disconnection and connection activities often overlapped. Five patients were scheduled for disconnection at the same time by 3 staff members in 3 different pods. When scheduling overlaps, staff ability to assist coworkers is limited. Staff commented that the “acuity of the patient is not accounted for in the time allotment” and “cleaning has to begin before the patient leaves; it allows us more time between patients” and “[there are] several steps with a CVC, but we are not given enough time to complete [the steps].”
Figure 3.
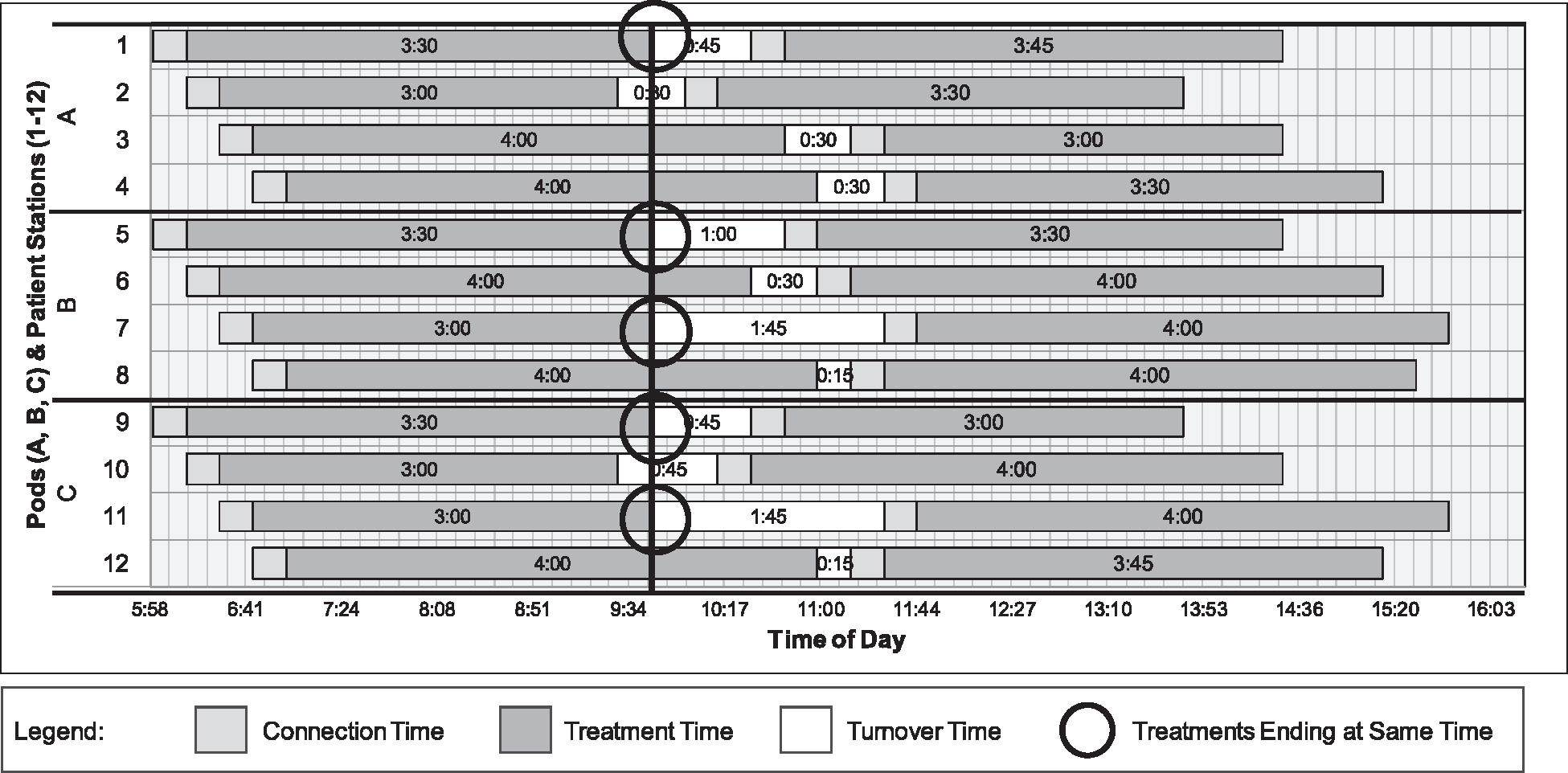
Patient arrival and treatment times for 24 patients treated in 12 dialysis stations on 1 day in a single facility. A pod is defined as a group of patient stations. The graph depicts 3 pods with 4 patients with staggered arrival times. Circles indicate 5 patients had treatments scheduled to end at the exact same time. One dialysis technician is assigned to each pod.
Policies and Procedures
We observed variability in policies and procedures among facilities and in strategies individual staff used to complete tasks even within the same facility. Sometimes work as performed included more steps in practice than were included in facility policy; for example, there may have been more opportunities for hand hygiene in practice than was described in the policy for catheter connection.
Culture/Leadership Engagement and Other Facilitators
Staff members at several facilities stated that their colleagues and team were facilitators of supportive work culture. At 2 facilities, we observed morning team meetings led by the center director, which included the plan for the day and any updates to available resources or possible challenges during the day. We observed the leaders running the meeting and engaging in the work of their staff (eg, presence on the floor during opening hours). We observed facilitators for adherence to infection prevention that were facility specific. For example, one facility had easy access to bleach solution for disinfection. This facility has a secondary tap that proportions and dispenses a continuous supply of bleach solution in 2 available concentrations (1:10 and 1:100 dilutions). Another facility had a skilled staff member in a support role rather than being assigned to specific patient care tasks. This staff member was available to assist with various tasks, including gathering supplies and cleaning.
Extrinsic Factors
Patient Factors
A number of staff members noted that extrinsic factors related to patient hygiene, transportation, access cannulation, and hemostasis can randomly and unpredictably disrupt the flow of care and compromise compliance with infection control procedures. Although these issues are not within the control of a dialysis facility, they certainly influence the work occurring within the facility.
Discussion
Infection prevention in outpatient hemodialysis is highly related to staff behavior, specifically adherence to recommended hand hygiene, environmental disinfection, injection safety, and catheter care practices.6 This study does not offer tested solutions but a better understanding of how the system design influences normal infection prevention-related work.
Our findings suggest that there are many macroergonomic factors influencing human performance. This type of assessment can help to identify barriers and facilitators of infection prevention practices within dialysis facilities. System level observations demonstrated that interruptions, alarms, and task stacking occur commonly and can be barriers to the timely and thorough execution of infection control processes. The impact of a disruption is determined by the duration of the interruption, the complexity of the task being interrupted, the complexity of the distracting task, and the moment of interruption.23–25 Distractions related to machine alarms and those related to task interruptions, which are pauses in the original task, have been previously described. These types of interruptions are known to increase errors.26 Nuisance alarms can increase staff stress, unnecessarily increase the need for machine interaction and hand hygiene tasks, lead to alarm fatigue, and can harm patients by delaying the time to alarm response.27 Task stacking may require substantial cognitive resources (visual, auditory, tactile, verbal, or spatial), which compounds the difficulty of the focused clinical task, especially if the task is being performed under pressure of time.28
Dialysis-related infection prevention procedures require rigorous attention to complex tasks, manual dexterity, and attention to patient-related factors. Patient and dialysis shift turnover time was observed to be particularly busy, and time pressure was a common theme among staff comments. In this instance, the sheer volume of tasks and the perception of feeling rushed could influence individual caregivers’ ability to adhere to infection prevention tasks. Our observations suggest that there may be a mismatch between the time available and expectations for performance. One expert told us, “[This is] an ICU-type procedure, that would ideally be conducted in an inpatient sterile setting, being done outpatient with providers who often have much less training and expertise.” Human/system factors may be inadvertently aligned to test human limitations and thereby challenge compliance with the processes of infection prevention.
The study also showed differences in the design of the physical layout and the steps taken during our link analysis data collection. The difference could be the result of facility policies, layout, individual staff performing the procedures or other features. We caution over-interpretation of this finding as “optimal” or “suboptimal.” Rather, the result is that there are simply observed differences in practices across facilities.
System level observations and staff conversations also highlighted that external patient-related factors such as transportation issues and late arrivals (“Patients are slow to leave because of clotting or other things, and others arrive early. Some have to get taken off [dialysis] early … for transportation”), and internal in-center factors, such as scheduling, workflow, and facility design can exert pressures on strict compliance with infection control procedures. For example, although the time allotments between patients may appear to be adequate, they may be insufficient when viewed in the context of facility workflow, which in turn can inadvertently lead to staff workarounds that bypass infection prevention procedures. Future studies should further consider the benefits of patient and clinician stories, which might provide further insight into how work is performed on a daily basis.
Several of the facilitators for infection prevention identified in this study were related to teamwork and leadership. Although not measured here, previous work has highlighted the importance of frontline leadership’s engagement in safety-related behaviors and the resulting increase in follower safety behavior.28 In addition, a culture of safety is highly related to daily engagement and communication, and leaders asking the frontline staff to discuss ongoing issues.6–16 We did not observe these behaviors occurring consistently across all facilities in our exploratory sample. All units were made aware of the dates of the site visits. Although this is imperative for planning purposes, it also may have resulted in changes to staffing or additional training before our visit.
The data here represent a very small subset of hemodialysis centers across the United States. Our design was descriptive, so statistical comparisons are not available or appropriate. The results presented here should be interpreted with caution. Further validation of use of the SEIPS model in a follow-up study is necessary. We chose to use the most basic SEIPS model, version 1.0, but there are other, more nuanced versions of the model available in the literature, which could and should be considered for future studies. Although our coding was overall consistent and we used a structured coding system, we did not measure interrater reliability, and unintentional bias was not assessed.
Our study is exploratory and our conclusions meant to be hypothesis-generating. Nonetheless, the consistency of our findings across several geographies and types of dialysis facilities does raise important considerations about the relationship of macroergonomic factors for infection prevention. One major limitation of our work is the Hawthorne effect, which is likely inevitable when an unfamiliar group comes to visit. In addition, despite significant effort to ensure the sites and frontline workers were aware that the visits were not “audits,” some of the comments from the staff made it very clear that they were concerned about our presence and doing “the correct procedure.” This is an inherent limitation of observation methods, but we attempted to mitigate it by showing our notes to the staff if they asked to see them and by conducting briefings and out-briefings with leadership. Scheduled visits (rather than unannounced) were necessary for this study. It is difficult to interpret, as a short-term visitor, whether a unit is doing work as usual, but our assumption is that it is unlikely. Even so, we observed challenges, particularly germane if the unit was overstaffed for our benefit. Future studies should attempt to alleviate the obtrusiveness and disruptiveness of these kinds of visits; however, this would take significant organizational engagement and trust at a high level.
The data from our evaluation suggest that the complex constellation of human skills required for the optimal completion of infection prevention tasks within dialysis may be significantly affected (both positively and negatively) by the design of our systems of care. Dialysis operators and facility medical directors may find that an assessment of human factors in their dialysis unit will shed light on facilitators and barriers to infection prevention and other safety procedures, and lead to better facility workflow design. Further studies should explore how to incorporate these concepts into our risk-reduction strategies to help mitigate infection risks to patients and staff.
Acknowledgements:
The authors would like to acknowledge the participating hemodialysis center patients, clinicians, staff, and leaders at each of the facilities we visited. Without their generosity, this study would not be possible. We would like to thank Dr Shannon Novosad for her thoughtful revisions of this article. We’d like to thank Dr Ibironke Apata and Dr Due Nguyen for their help on the site visits, and Ms Darlene Rodgers and Ms Susie Stark for their critical engagement in organizing the project. Finally, we would like to thank the NTDS Human Factors Workgroup for their strategic engagement and support.
Support:
This work was directly supported by the American Society of Nephrology, through a Centers for Disease Control contract 200–2016-88832 with the American Society of Nephrology. The funder had a role in the decision to submit for publication.
Footnotes
Financial Disclosure: Dr Patel owns stock in Johnson and Johnson and Pfizer. The other authors declare that they have no relevant financial interests.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the American Society of Nephrology.
Peer Review: Received September 11, 2023. Evaluated by 2 external peer reviewers, with direct editorial input from an Associate Editor and the Editor-in-Chief. Accepted in revised form December 23, 2023.
Contributor Information
Sarah Henrickson Parker, Carilion School of Medicine, Virginia Tech, Roanoke, Virginia.
Matthew N. Jesso, Carilion School of Medicine, Virginia Tech, and Carilion Clinic, Roanoke, Virginia.
Laurie D. Wolf, Carilion School of Medicine, Virginia Tech, and Carilion Clinic, Roanoke, Virginia.
Kerry Avondet Leigh, Virginia; American Society of Nephrology, Washington, DC.
Stephanie Booth, Centers for Disease Control and Prevention, Atlanta, Georgia.
Nicole Gualandi, Centers for Disease Control and Prevention, Atlanta, Georgia.
Renee E. Garrick, New York Medical and Westchester Medical Center, Valhalla, New York.
Alan S. Kliger, Department of Medicine, Section of Nephrology, School of Medicine, Yale University, New Haven, Connecticut.
Priti R. Patel, Centers for Disease Control and Prevention, Atlanta, Georgia.
References
- 1.Johansen KL, Chertow GM, Gilbertson DT, et al. US Renal Data System 2022 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2023;81 (3)(suppl 1):A8–A11. doi: 10.1053/j.ajkd.2022.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2018 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2019;73(3)(suppl 1):A7–A8. doi: 10.1053/j.ajkd.2019.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control. Dialysis Safety [website]. 2017. Accessed July 11,2019. https://www.cdc.gov/dialysis/index.html [Google Scholar]
- 4.Novosad SA, Lake J, Nguyen D, et al. Multicenter outbreak of Gram-negative bloodstream infections in hemodialysis patients. Am J Kidney Dis. 2019;74(5):610–619. doi: 10.1053/j.ajkd.2019.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen DB, Gutowski J, Ghiselli M, et al. A large outbreak of hepatitis C virus infections in a hemodialysis clinic. Infect Control Hosp Epidemiol. 2016;37(2):125–133. doi: 10.1017/ice.2015.247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waheed S, Philipneri M. Targeting zero infections in the outpatient dialysis unit: core curriculum 2020. Am J Kidney Dis. 2020;76(1):130–140. doi: 10.1053/j.ajkd.2020.02.441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Society of Nephrology. No date. Nephrologists transforming dialysis safety [website]. https://epc.asn-online.org/projects/ntds/ [Google Scholar]
- 8.Dul J, Bruder R, Buckle P, et al. A strategy for human factors/ergonomics: developing the discipline and profession. Ergonomics. 2012;55(4):377–395. doi: 10.1080/00140139.2012.661087 [DOI] [PubMed] [Google Scholar]
- 9.Shekelle PG, Pronovost PJ, Wachter RM, et al. Advancing the science of patient safety. Ann Intern Med. 2011; 154(10):693–695. doi: 10.7326/0003-4819-154-10-201105170-00011 [DOI] [PubMed] [Google Scholar]
- 10.Shekelle PG, Pronovost PJ, Wachter RM, et al. Technical Expert Panel. AHRQ Publication No. 11–0006-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 11.Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(suppl 1):50–58. doi: 10.1136/qshc.2005.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sarker SK, Vincent C. Errors in surgery. Int J Surg. 2005;3(1):75–81. doi: 10.1016/j.ijsu.2005.04.003 [DOI] [PubMed] [Google Scholar]
- 13.Gonzalo JD, Haidet P, Papp KK, et al. Educating for the 21st-century health care system: an interdependent framework of basic, clinical, and systems sciences. Acad Med. 2017;92(1):35–39. doi: 10.1097/ACM.0000000000000951 [DOI] [PubMed] [Google Scholar]
- 14.Carayon P, Karsh BT, Gurses AP, et al. Macroergonomics in health care quality and patient safety. Rev Hum Factors Ergon. 2013;8(1) :4–54. doi: 10.1177/1557234X13492976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karsh BT, Brown R. Macroergonomics and patient safety: the impact of levels on theory, measurement, analysis and intervention in patient safety research. Appl Ergon. 2010;41(5):674–681. doi: 10.1016/j.apergo.2009.12.007 [DOI] [PubMed] [Google Scholar]
- 16.Kaplan G, Bo-Linn G, Carayon P, et al. Bringing a systems approach to health. NAM Perspect. 2013;3(7):1–26. doi: 10.31478/201307a [DOI] [Google Scholar]
- 17.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–1686. doi: 10.1080/00140139.2013.838643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carayon P, Wooldridge A, Hoonakker P, Hundt AS, Kelly MM. SEIPS 3.0: human-centered design of the patient journey for patient safety. Appl Ergon. 2020;84:103033. doi: 10.1016/j.apergo.2019.103033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kleiner BM. Sociotechnical systems in health care. In: Carayon P, ed. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Lawrence Erlbaum; 2007:79–95. [Google Scholar]
- 20.Lewis VR, Clark L, Benda N, Hardwick MJ. Reducing healthcare-associated infections in an ambulatory dialysis unit: identification and alignment of work system factors. Am J Infect Control. 2014;42(10):S284–S290. doi: 10.1016/j.ajic.2014.05.016 [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Dialysis safety: audits and checklists. Published 2023. https://www.cdc.gov/dialysis/prevention-tools/audit-tools.html
- 22.Saldaña J The Coding Manual for Qualitative Researchers. 2nd ed. SAGE; 2013. [Google Scholar]
- 23.Lee BC, Duffy VG. The effects of task interruption on human performance: a study of the systematic classification of human behavior and interruption frequency. Hum Factors Ergon Manuf Serv Industries. 2015;25(2):137–152. doi: 10.1002/hfm.20603 [DOI] [Google Scholar]
- 24.Borst JP, Taatgen NA, Van Rijn H. What makes interruptions disruptive? A process-model account of the effects of the problem state bottleneck on task interruption and resumption. Proc 33rd Ann ACM Corrf Hum Factors Comput Syst (CHI ‘15). 2015:2971–2980. doi: 10.1145/2702123.2702156 [DOI] [Google Scholar]
- 25.Cades DM, Werner N, Trafton JG, Boehm-Davis DA, Monk CA. Dealing with interruptions can be complex, but does interruption complexity matter: a mental resources approach to quantifying disruptions. Proc Hum Factors Ergon Soc. 2008;1(2014):398–402. doi: 10.1177/154193120805200442 [DOI] [Google Scholar]
- 26.Horkan AM. Alarm fatigue and patient safety. Nephrol Nurs J. 2014;41(1):83–85. [PubMed] [Google Scholar]
- 27.Douglas HE, Raban MZ, Walter SR, Westbrook JI. Improving our understanding of multi-tasking in healthcare: drawing together the cognitive psychology and healthcare literature. Appl Ergon. 2017;59(A):45–55. doi: 10.1016/j.apergo.2016.08.021 [DOI] [PubMed] [Google Scholar]
- 28.Zohar D Modifying supervisory practices to improve subunit safety: a leadership-based intervention model. J Appl Psychol. 2002;87(1):156–163. doi: 10.1037/0021-9010.87.1.156 [DOI] [PubMed] [Google Scholar]


