Abstract
Background:
Mental health disparities were prevalent among racially and ethnically minoritized youth prior to the COVID-19 pandemic. As complete datasets from 2022 become available, we can estimate the extent to which the pandemic further magnified existing inequities.
Objective(s):
To quantify disparities in trajectories of depression, anxiety, and suicide risk-related diagnoses in youth before and after the start of the COVID-19 pandemic, using an intersectional lens of race, ethnicity and gender.
Methods:
Using Electronic Medical Record data from one mid-Atlantic health care system (2015–2022), we evaluated changes in annual rates of depression, anxiety and suicide risk-related diagnoses in 29,117 youths, aged 8–20 years, using graphical analysis, comparison of adjusted mean differences (AMD) and adjusted mixed multilevel logistic regression.
Results:
Almost all racial and gender subgroups had significantly higher rates of depression and anxiety after the start of COVID-19 compared to the years prior, with the greatest changes observed in Hispanic and Asian females. Suicide risk-related diagnoses significantly increased among all female subgroups, with the largest increase among Asian females (AMD 4.8, 95% CI 0.2–9.3) and Black females (AMD 4.6, 95% CI 2.2–6.9).
Conclusions:
Rates of depression, anxiety, and suicidal thoughts and/or behaviors in young people continued to increase in the post-pandemic period. Many pre-existing disparities between subgroups, especially females, significantly widened, highlighting the importance of using an intersectional lens. Urgent action is warranted, including universal screening of pediatric patients for suicide risk, broadening effective treatment and support options in minoritized patients, and increasing support services to patients and families.
Keywords: suicide, adolescent, disparities, COVID-19
Background
Suicide was the second leading cause of death among youths aged 8 to 17 years in the United States (U.S.) in 2023 and the third leading cause of death among youth aged 8 to 20 years.1 Rates of suicidal ideation, attempts, and deaths among racially and ethnically minoritized youth have shown increasing trends in recent decades, and these increases have been the most pronounced among young females.1–3 These troubling trends have led to calls to use an intersectional lens in suicide-related research, in order to acknowledge the unique structural and individual discrimination experienced by individuals belonging to multiple marginalized groups.4,5 There are subgroup-specific stressors and sociocultural constructs unique to Asian, Black, Hispanic and White young males and females (respectively) in the U.S., which are contributing in unique ways to the mental health crisis within each subgroup.6 In addition to the stress caused by isolation from peers, economic concerns and health worries directly related to the pandemic, these groups have also experienced racism-specific stress. In the case of Black Americans, worsening mental health has been attributed to fear of police-involved racialized violence and internalized racism-related vigilance and anxiety.7–9 Anti-Asian racism and violence as a result of the politicization of the COVID-19 pandemic have negatively impacted Asian Americans’ mental health.10 Increased externalizing and internalizing symptoms during the pandemic have been found among Hispanic youth, and have been attributed to increased childcare responsibilities and perceived family financial instability.11 Given these and other external stressors, it is important to note that there are also subgroup-specific stigma, preferences and beliefs that have led racial and ethnic minoritized subgroups to traditionally be less likely to engage in mental health treatment6,12–15.
Recent historical, political and public health events, most notably the COVID-19 pandemic, have collectively contributed to increased stress and mental health challenges that disproportionately affected minoritized racial and ethnic groups.7,16–19 Among adolescents, increases in racial and/or gender disparities in mental health diagnoses, such as suicidal ideation and depression, were documented during the first year of the COVID-19 pandemic, and were attributed largely to social isolation and family stress.7,10,20 The direction of trends in these mental health diagnoses after the peak of the pandemic and related quarantines and school closures are not yet known. It is critically important to understand the extent to which trajectories in mental health disparities seen prior to and during COVID-19 continued in the years that followed.
In this study, we sought to leverage Electronic Medical Record (EMR) data because it is an accessible way for health systems, governments, and other stakeholders to track and understand patient-level service interaction and care utilization. EMR data is increasingly available, and best practices are being developed for employing this type of data for precision patient care and larger scale public health program planning.21 EMR data can provide valuable information about longitudinal interactions with service providers as they relate to patients’ histories, diagnoses, referrals for outside care and medications without the extensive financial and time cost of implementing a large-scale survey effort.
Our study aims to quantify annual changes in mental health for racial, ethnic and gender subgroups of pediatric patients using proxy measures available in the pediatric primary care EMR. We focused specifically on annual trends and mean rates of first diagnoses of anxiety, depression and suicidal thoughts and behaviors before and during the pandemic. Examining the presence of mental health diagnoses stratified by specific subgroups may help to tease apart the complicated web of gender, race and ethnicity when it comes to suicide prevention and mental health needs, especially in light of the political and historical events surrounding the COVID-19 time period.
Methods
Patient population
We conducted a retrospective, cross-sectional cohort study22 using outpatient EMR encounter data from the Johns Hopkins Community Physicians (JHCP), a health care system that includes 40 locations providing ambulatory, general, and specialty care throughout Maryland. Fully de-identified patient data was extracted from Epic, the EMR system used by JHCP beginning in 2013. The institutional review boards of Johns Hopkins approved this study as exempt, due to the full de-identification of the data. The study cohort included patients from JHCP pediatric and family practices, ages 8–20 years old, who had a primary care encounter between 1/1/2015 and 12/31/2022.
In order to create a cohort of patients who would be likely to seek services from JHCP the majority of the time, patients were excluded if they had less than two years between first and last encounter during the study period, or if they were older than 20 at the time of the first encounter, or if the first encounter was after December 31, 2022. A patient was counted as part of the denominator for the annual cross-sectional rates of the outcomes of interest if they had any type of primary care encounter in a given year. A patient was counted as part of the numerator for the annual rate if they had an encounter and a first recorded diagnosis of anxiety depression and /or suicide in a given year. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines were followed in this work.23
Measures
Race was defined using the first chosen race category for the child by parent or caregiver upon registration with the health system. We generated an eight-level composite gender and race variable, coded as 1) White male, 2) White female, 3) Black male, 4) Black female, 5) Hispanic male, 6) Hispanic female, 7) Asian male and 8) Asian female. For these analyses, patients were classified as Hispanic if ethnicity was identified as “Hispanic or Latino” in the EMR. Patients were classified as Asian if their race was any of 13 separate East and South Asian and Pacific Islander identities in the EMR race field. We use the term “Asian”, while noting that this group does include <.05% of patients who identified as Native Hawaiian or Pacific Islander. Patients with a race or ethnicity that did not fall into any of these categories were not included in this analysis. Gender was defined using the “sex” variable in the Epic demographic module, which represented legal gender of the patient as reported by the parent or caregiver upon registration with the health system. More specific information about gender identity was not collected within the JHCP Epic system until 2019, and as a result there is extremely sparse recording of gender subgroups other than “Male” or “Female” (<0.05%). For the purposes of this analysis, patients identifying as “Nonbinary”, “Other”, or “Unknown” were excluded.
Patients were classified according to whether there was a diagnosis of depression, anxiety, and/or suicide, and by the year that each was first recorded in a patient’s EMR. We used a broad classification that encompassed all suicide diagnoses including suicidal ideation, suicide attempt and/or intentional self-harm with suicidal intent in order to ensure that no suicide risk-related diagnoses would be missed due to misspecification.3 Anxiety and depression were also broadly classified using any anxiety- and/or depression- related diagnosis code. Each of the three outcomes (anxiety, depression, suicide-risk related diagnosis) was defined as positive for a patient if a related ICD-10 code was listed in an encounter diagnosis list, in the problem list, or in the history and was classified using the coding conventions presented in Supplemental Table 1.3
Insurance was classified based on insurance at first recorded encounter and was categorized as public, private, or other (self-pay, none). National Area Deprivation Index (ADI) was calculated within the EMR using patient’s address and corresponding Census block group, with those with greatest deprivation having higher values.24 The Elixhauser score was calculated using all encounter diagnosis codes, and was used as a measure of underlying comorbidities.25 Number and type of complex chronic conditions were calculated using ICD-10 codes.26 Number of primary care encounters during the period of interest was calculated for each patient. Missing data was a problem only for the national ADI measure (<10%), and missing values were imputed using the mean value.
Graphical retrospective cross-sectional cohort study design
Clinical and demographic characteristics were explored for patients in the entire cohort, and the outcomes of interest were calculated in terms of “ever” presence of a given diagnosis, as well as the year of a “first” presence of a given diagnosis. As a first step in the retrospective cohort analysis, we graphically represented unadjusted annual rates of first diagnosis during the study period of depression, anxiety and suicidality by race and gender subgroup, comparing each minoritized subgroup with White males and females in separate graphs.
Adjusted mean differences (AMD) analysis design
We calculated the adjusted mean rates and differences of first recorded anxiety, depression or suicide risk-related diagnosis by composite race/gender group separately before (2015–2019) and after (2020–2022) the start of the pandemic. These analyses were performed using a series of mixed multilevel logistic regression models controlling for age, insurance type, National ADI, number of complex chronic conditions, Elixhauser score, year, number of encounters in the data, number of years in the data and Department of encounter. Due to the longitudinal nature of the data, the patient was treated as a nested layer within the model and given the potential clustering of patient outcomes and demographic characteristics within practices, individual JHCP Departments were also analyzed as a nested level within the model.
Relative disparities analysis study design
To understand potential changes in relative disparities before versus during the pandemic, we employed a series of mixed multilevel logistic regression models calculating the odds of the first recorded anxiety, depression or suicide risk-related diagnosis by composite race/gender group. The models included age at first encounter, insurance type, National ADI, number of complex chronic conditions, Elixhauser score, year, number of encounters in the data, number of years in the data and Department and were calculated separately for the two time periods (before vs during the pandemic). As in the previous models, JHCP practices and patients were treated as nested levels within the model to account for clustering and the longitudinal structure of the data. Odds ratios were deemed to differ significantly between the two time periods if the 95% confidence intervals for a given subgroup did not overlap. All analyses were conducted using Stata software, version 18.0.27
Results
While the overall number of patients seen during the study period was 76,000, after applying the exclusion criteria, our final analytic cohort consisted of 29,117 patients, with 4.85 mean years between first and last encounter (SD 2.04) and 9 median encounters during the study period (IQR 6,14), (Figure 1, Table 1). This analytic cohort was used for all analyses. As seen in Table 1, the mean age at first encounter was 11.37 (SD 3.00) years, and 16,440 (51.7%) were female. For the measure of primary race, 15,555 (48.9%) of patients were classified as Non-Hispanic White, 10,278 (32.3%) of patients were non-Hispanic Black, 2,159 (6.8 %) were Hispanic, and 1,805 (5.7%) were non-Hispanic Asian. At first recorded encounter, 16,207 (51.3 %) of patients had a private primary health insurance and 6,632 (21.0%) of patients had public health insurance. At least one complex chronic condition was present in 2,867 (9.0%) of patients, and the mean Elixhauser score was 0.58 (SD 0.76). The national ADI rank median was 22 (IQR 14, 37).
Figure 1. Numbers Flow Chart.
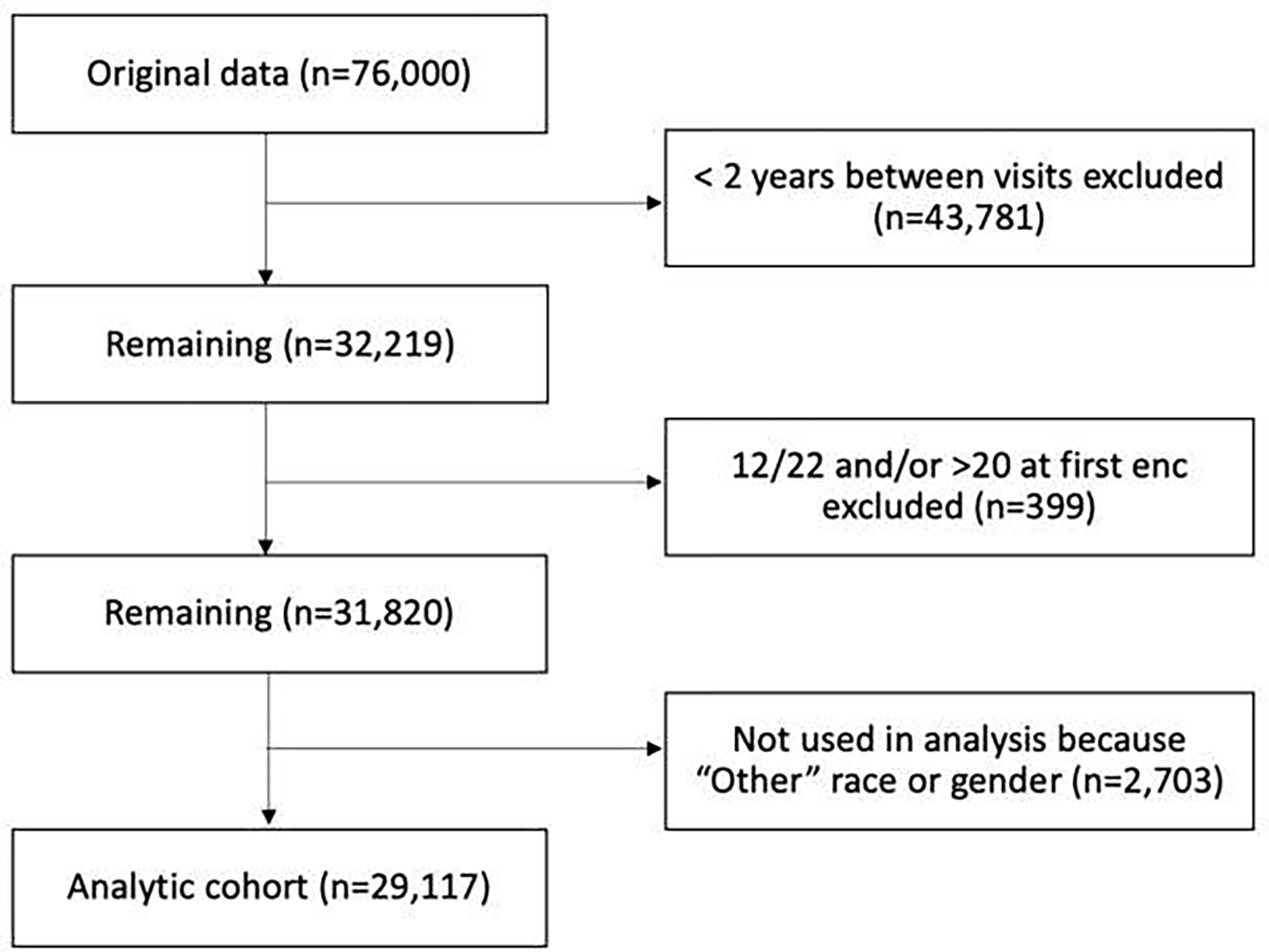
Table 1. Demographic and Clinical Characteristics of Patients in Analytical JHCP Cohort*.
| Characteristic | N (%), mean (SD) or median (IQR) |
|---|---|
| N | 31,820 |
| Age at first encounter, mean (SD) | 11.37 (3.00) |
| Number of encounters, median (IQR) | 9 (6, 14) |
| Years stayed in cohort, mean (SD) | 4.85 (2.04) |
| Gender | |
| Female | 16440 (51.7%) |
| Male | 15364 (48.3%) |
| Nonbinary | 13 (<1%) |
| Other or Unknown | 3 (<1%) |
| Race/Ethnicity | |
| Non-Hispanic White | 15555 (48.9%) |
| Non-Hispanic Black | 10278 (32.3%) |
| Hispanic | 2159 (6.8%) |
| Non-Hispanic Asian | 1805 (5.7%) |
| Other | 2023 (6.4%) |
| Insurance | |
| Public | 6632 (21.0%) |
| Private | 16207 (51.3%) |
| Other/None** | 8755 (27.7%) |
| Elixhauser comorbidity score, mean (SD) | 0.58 (0.76) |
| National ADI percentile, median (IQR) | 22 (14, 37) |
| Any presence of Complex Chronic Condition (CCC) | |
| No | 28953 (91.0%) |
| Yes | 2867 (9.0%) |
| Number of CCC, mean (SD) | |
| 0 | 28953 (91.0%) |
| 1 | 2519 (7.9%) |
| 2 | 266 (0.8%) |
| >=3 | 82 (0.3%) |
| Combined gender and race | 29,117 |
| White Female | 7799 (24.5%) |
| White Male | 7348 (23.1%) |
| Black Female | 5275 (16.6%) |
| Black Male | 4782 (15.0%) |
| Hispanic Female | 1087 (3.4%) |
| Hispanic Male | 1072 (3.4%) |
| Asian Female | 924 (2.9%) |
| Asian Male | 830 (2.6%) |
| Other | 2703 (8.5%) |
| MBHD Prevalence | |
| Anxiety | 8109 (25.5%) |
| Depression | 5963 (18.7%) |
| Behavioral disorders | 8856 (27.8%) |
| Substance use | 777 (2.4%) |
| Suicide-related behavior | 1059 (3.3%) |
| Schizophrenia | 78 (0.2%) |
| Other disorders | 1208 (3.8%) |
Patients with at least 2 years of encounter data, 2015–2022, aged 8–20 at first encounter
Includes Government/Military insurance
Graphical retrospective analysis
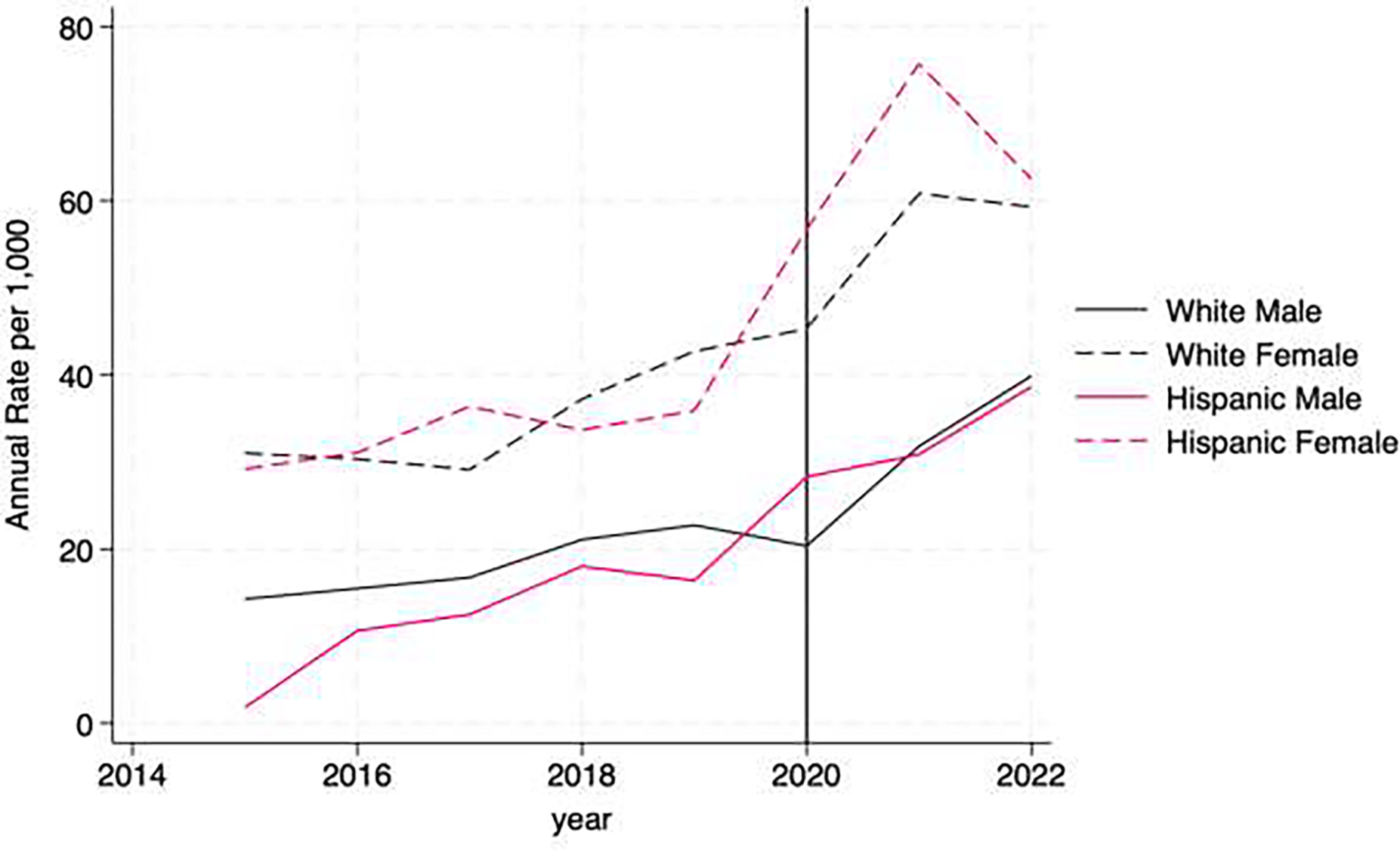
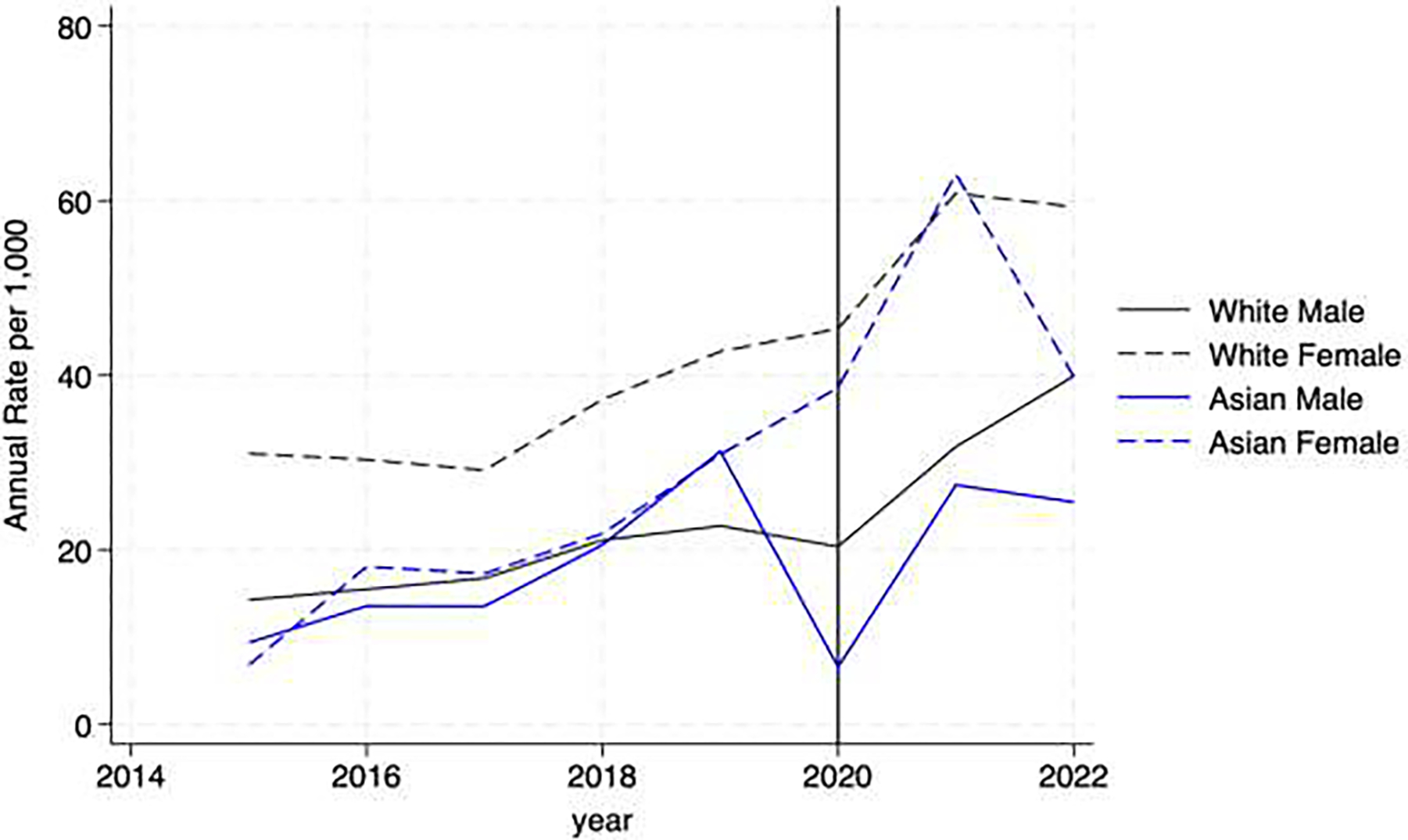
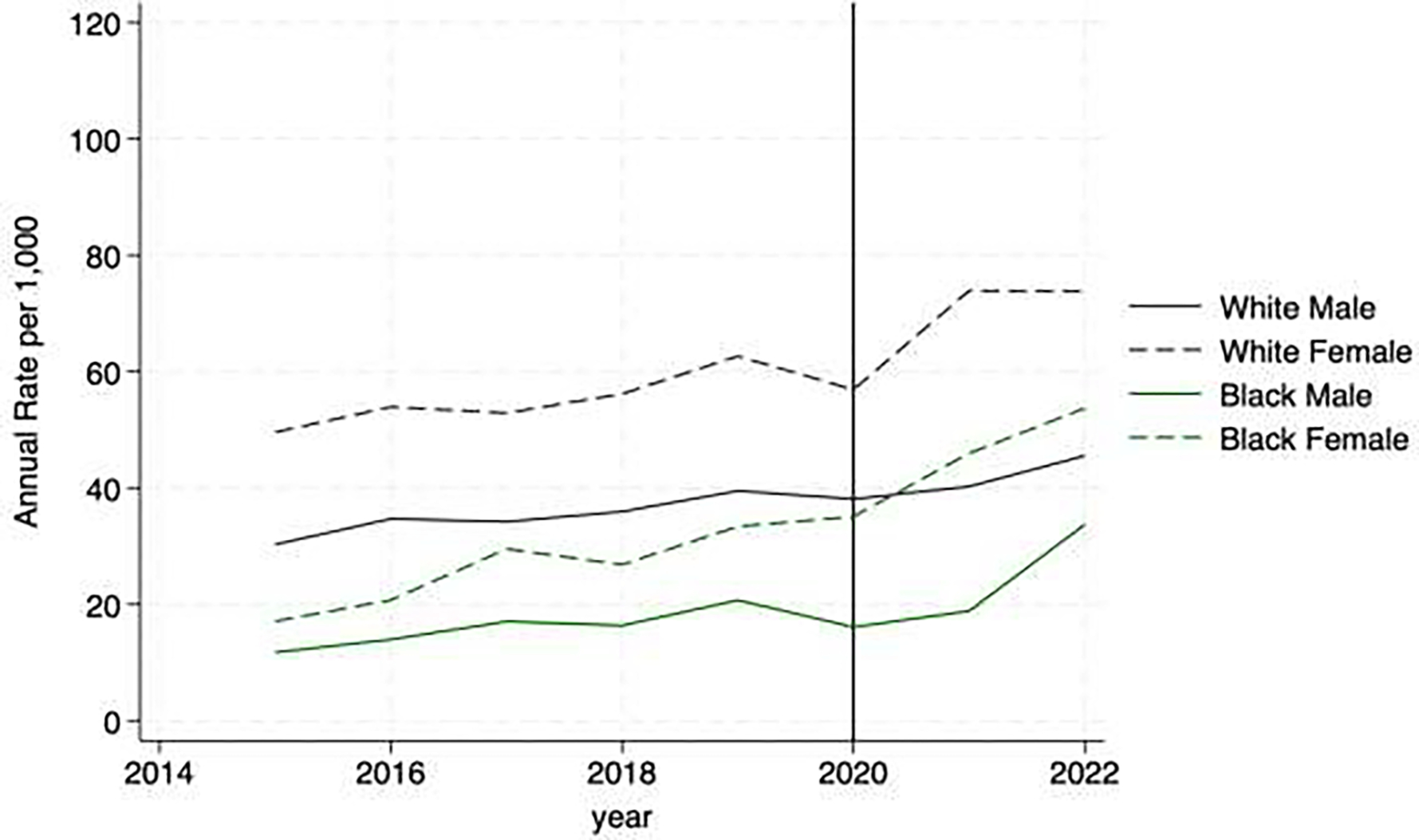
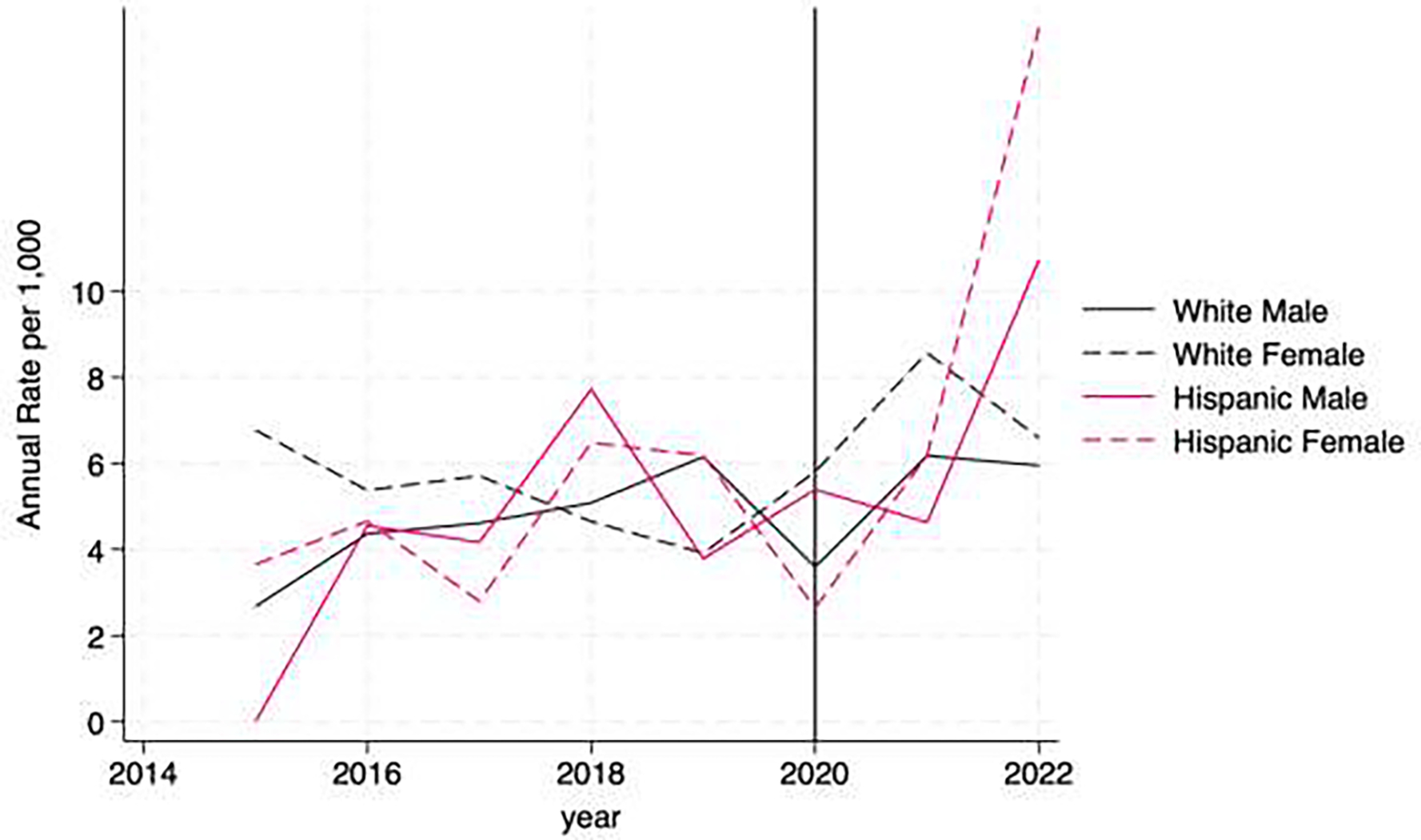
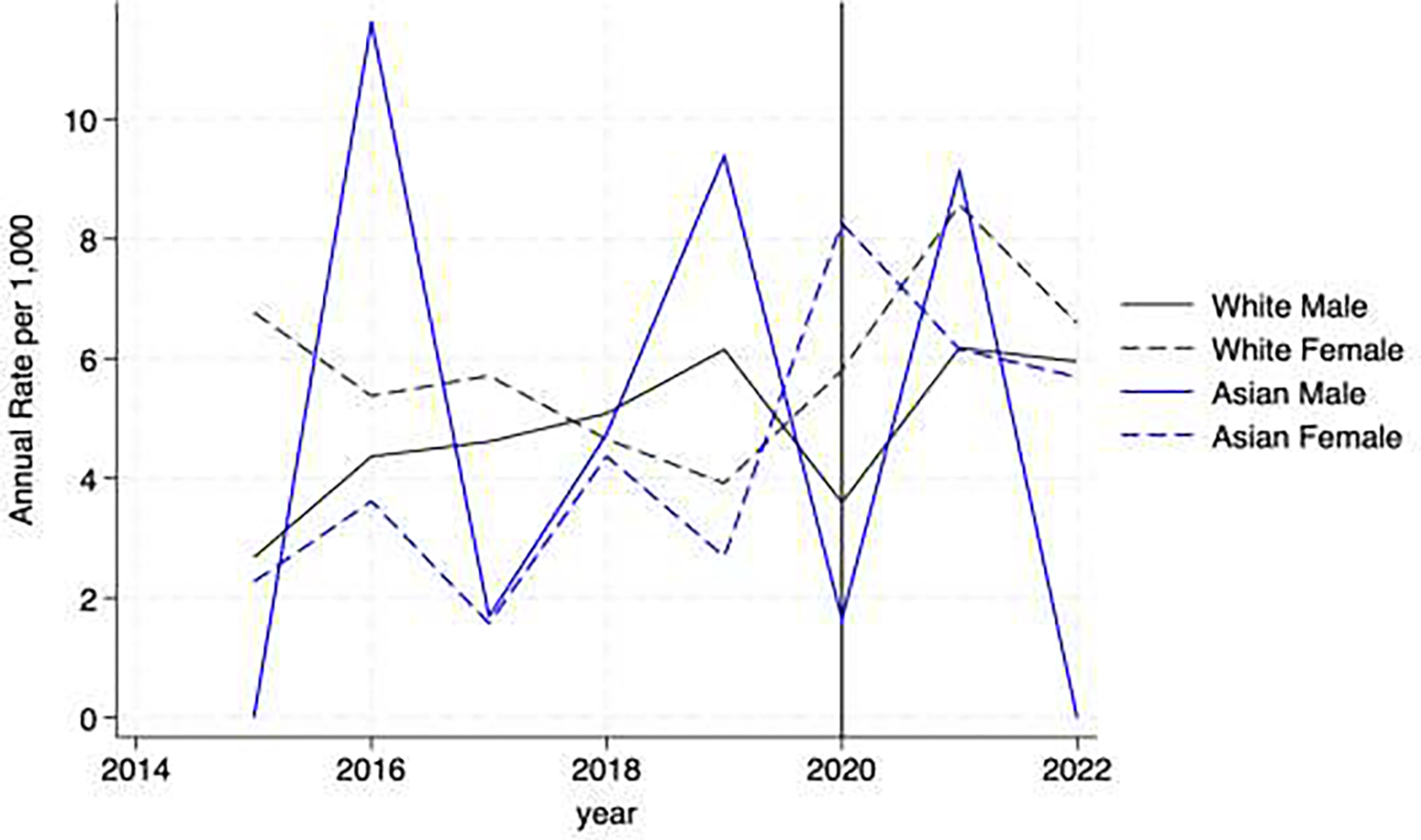
In the unadjusted graphical retrospective analysis of depression, we found that all groups displayed increasing trends, and this slope frequently appeared steeper after 2019. Black, Asian and Hispanic females tracked higher than male counterparts (at rates similar to White females, especially after 2020) and Black, Asian and Hispanic males also tracked at similar rates (Figure 2). In the graphs depicting anxiety diagnoses, we found a similar pattern, though all slopes were generally less steep than for depression and Black females tracked at lower rates than White females, but Hispanic and Asian females had rates that increased over time to be similar to the higher rates of White females (Figure 3). In terms of suicide, small numbers made graphical depictions somewhat difficult to interpret, but it is notable that Hispanic and Black females are demonstrating sharp increases in suicide risk-related diagnosis rates after 2020 (Figure 4).
Figure 2. Depression Diagnoses.
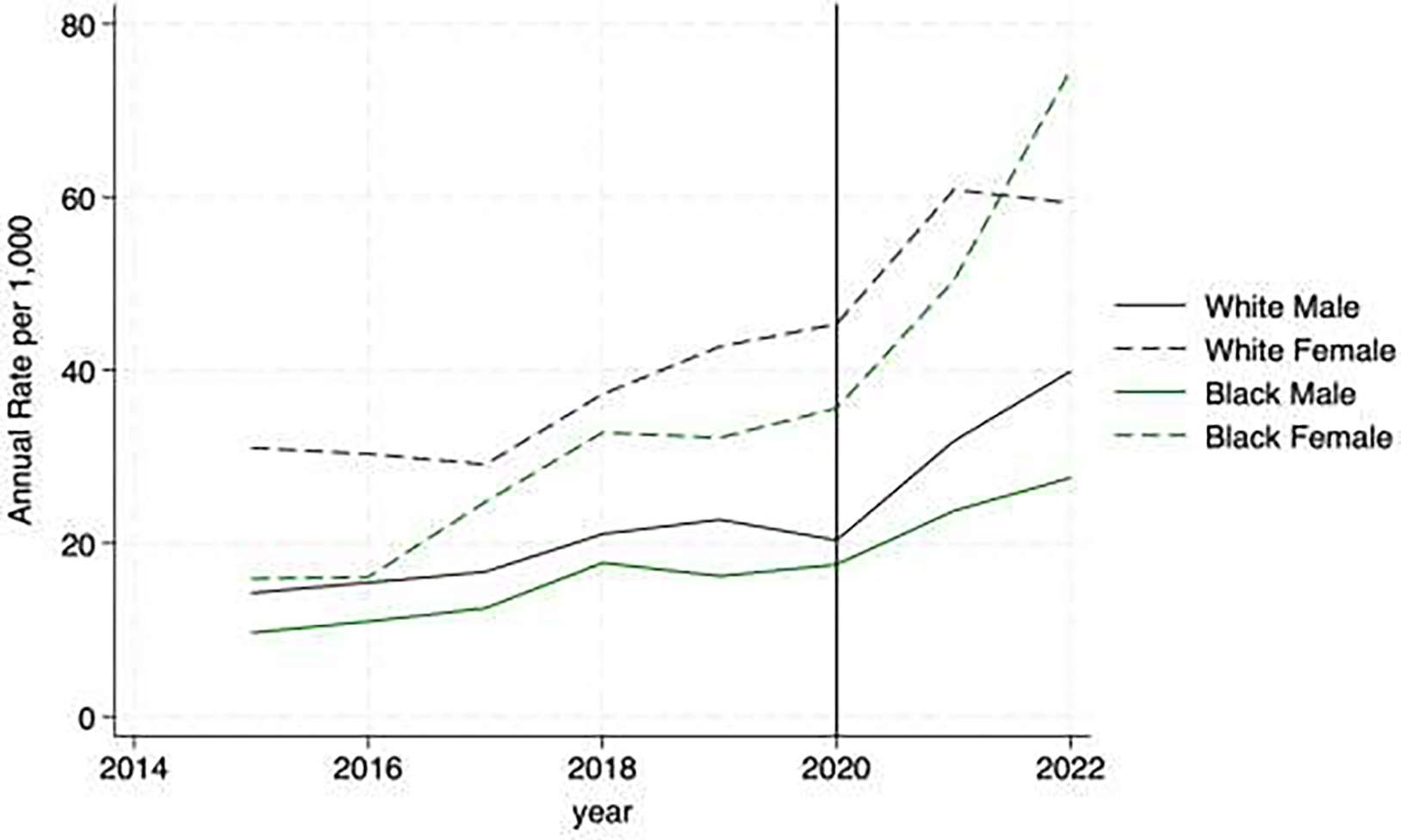
2a. Black Males and Females vs White Males and Females
2b. Hispanic Males and Females vs White Males and Females
2c. Asian Males and Females vs White Males and Females
Figure 3. Anxiety Diagnoses.
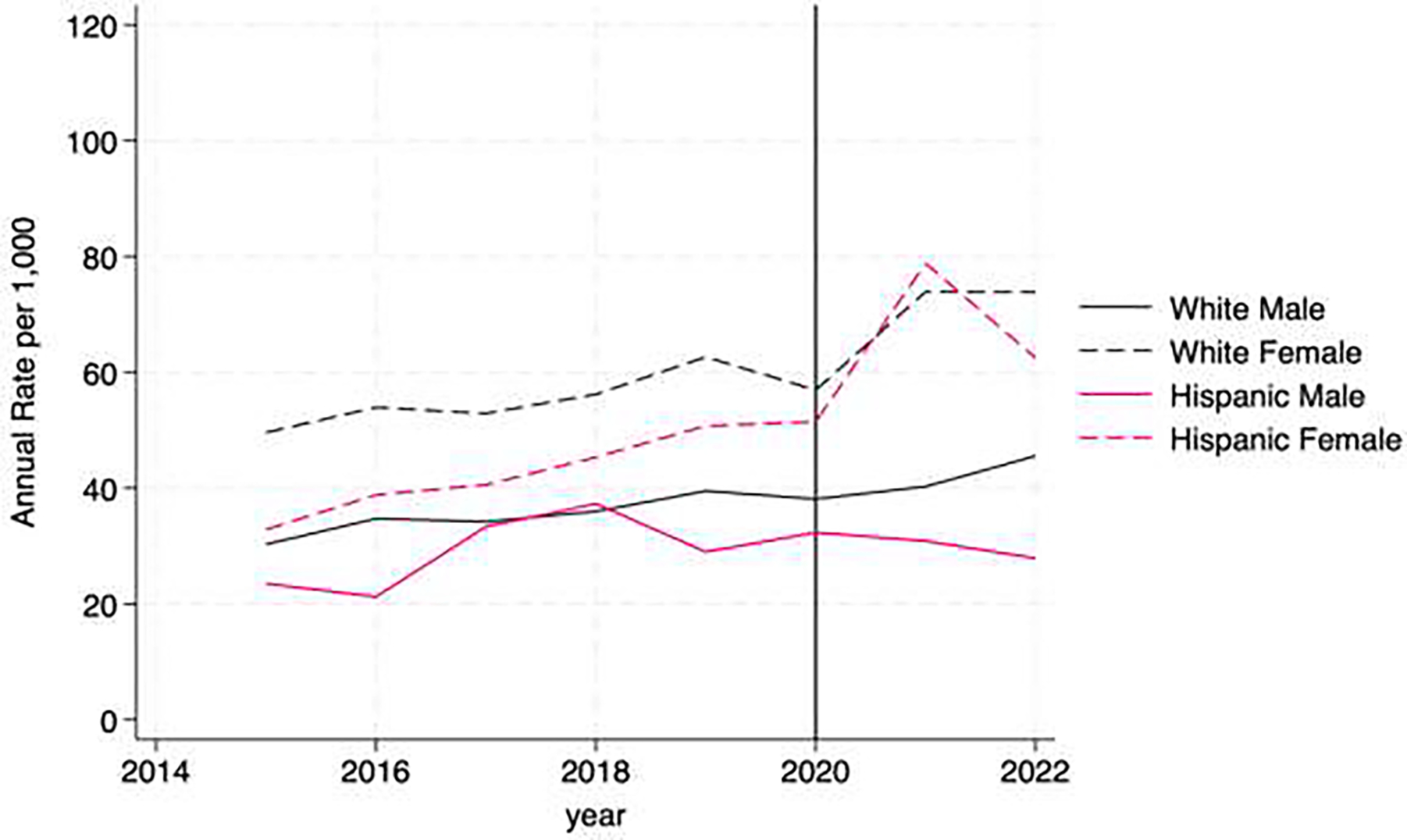
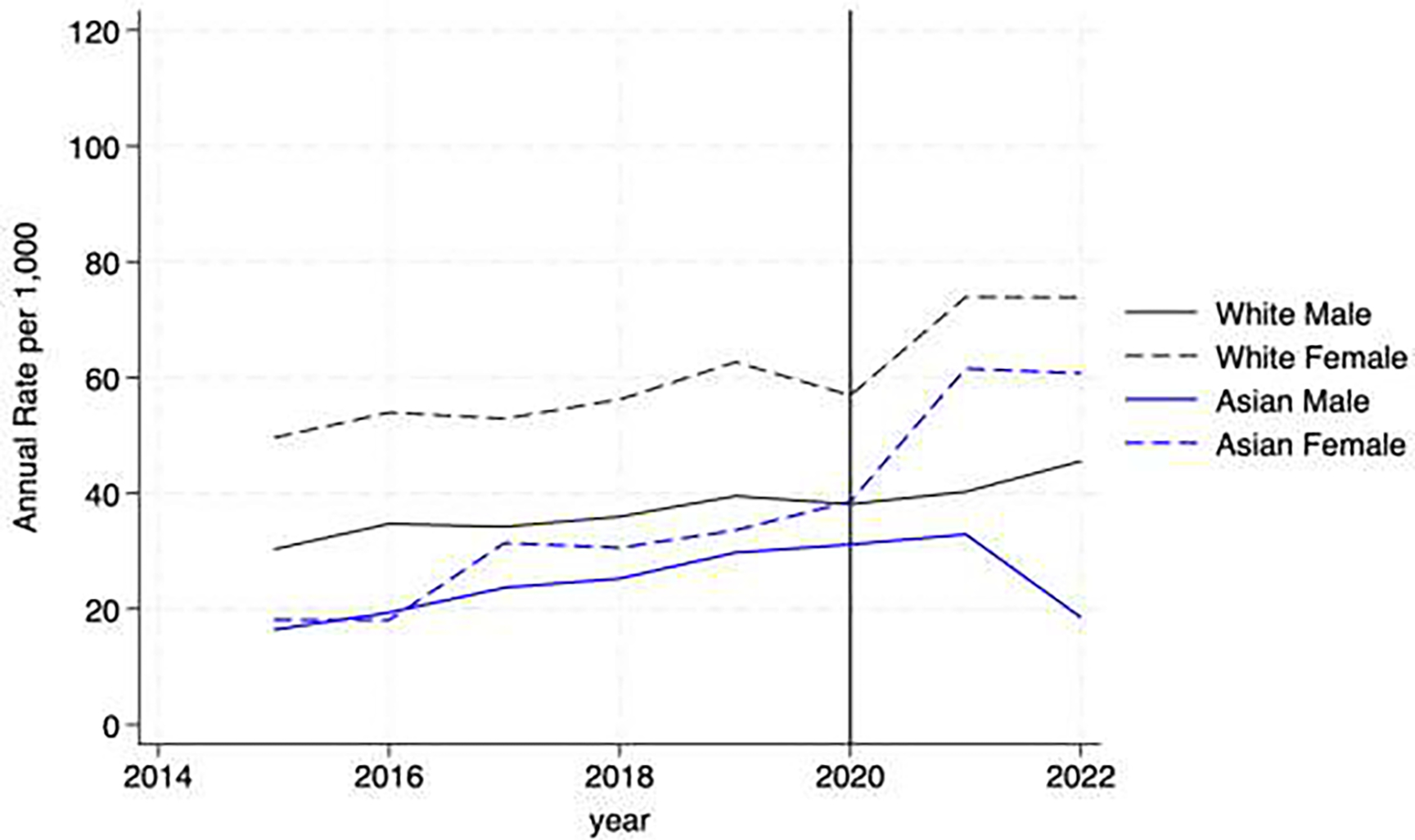
3a. Black Males and Females vs White Males and Females
3b. Hispanic Males and Females vs White Males and Females
3c. Asian Males and Females vs White Males and Females
Figure 4. Suicide-Related Diagnoses.
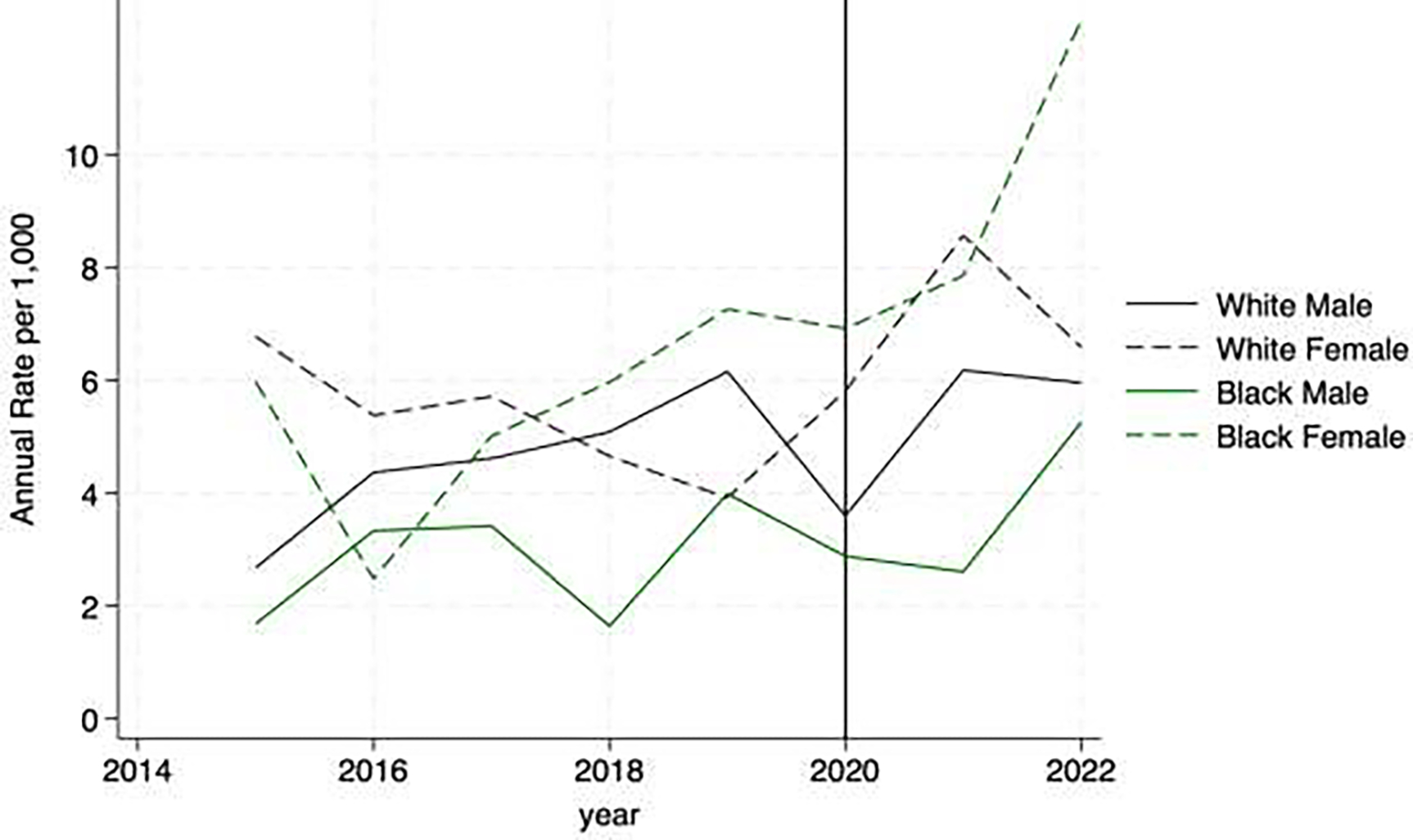
4a. Black Males and Females vs White Males and Females
4b. Hispanic Males and Females vs White Males and Females
4c. Asian Males and Females vs White Males and Females
Adjusted mean differences analysis
We found that there were significant differences in adjusted mean rates of depression across most subgroups during the pandemic (as compared to before the pandemic). The largest differences were seen in Hispanic females, AMD 41.9 per 1,000 (95% CI 28.1–55.6), but differences were also seen among Asian (AMD 34.2, 95% CI 22.6–45.8), Black (AMD 33.2, 95% CI 27.8–38.5) and White females (AMD 34.6, 95% CI 29.6–39.5). Rates of first depression diagnosis were not significantly different only for Asian males. For the outcome for first anxiety diagnosis, females also had higher AMD rates across racial groups, with the largest difference seen in Asian females (AMD 34.5, 95% CI 21.7–47.3). Rates of first anxiety diagnosis were not significantly different between the two time periods for Hispanic or Asian males. As for the outcome of first suicide risk-related diagnosis, the gender/race subgroups with significant increases in rates during the pandemic were Asian females (AMD 4.8, 95% CI 0.2–9.3), Black females (AMD 4.6, 95% CI 2.2–6.9) and White females (AMD 2.7, 95% CI 0.9–4.5; Table 2).
Table 2: Adjusted Mean Rates and Differences per 1,000 of First Diagnosis for Depression, Anxiety, or Suicidal Thoughts/Behaviors by Race and Gender Subgroup, Before versus During the COVID-19 Pandemic.
n= 29,117 years 2015–2022
| Pre-COVID (2015–2019) mean (SD) | During COVID (2020–2022) mean (SD) | Adjusted Mean Difference* (95% CI) | |
|---|---|---|---|
| First Depression Diagnosis (per 1,000) | |||
| White male | 16.6 (14.8) | 36.0 (35.7) | 19.4 (15.5–23.4) |
| White female | 31.2 (20.2) | 65.7 (45.8) | 34.6 (29.6–39.5) |
| Black male | 13.3 (13.8) | 24.5 (27.3) | 11.2 (7.4–15.1) |
| Black female | 23.9 (18.4) | 57.1 (40.5) | 33.2 (27.9–38.5) |
| Hispanic male | 12.1 (13.1) | 35.1 (32.6) | 23.0 (13.5–32.5) |
| Hispanic female | 31.5 (20.7) | 73.3 (46.4) | 41.9 (28.1–55.6) |
| Asian male | 17.3 (15.4) | 22.0 (25.6) | 4.7 (−4.3–13.6) |
| Asian female | 18.8 (16.5) | 53.0 (37.7) | 34.2 (22.6–5.8) |
| First Anxiety Diagnosis (per 1,000) | |||
| White male | 34.7 (22.5) | 42.2 (36.5) | 7.6 (3.2–12.0) |
| White female | 52.7 (27.1) | 73.7 (47.6) | 21.0 (15.6–26.5) |
| Black male | 16.5 (15.9) | 21.8 (25.3) | 5.3 (1.6–9.1) |
| Black female | 25.1 (19.1) | 48.7 (38.3) | 23.7 (18.5–28.8) |
| Hispanic male | 28.7 (20.4) | 32.9 (31.7) | 4.2 (−6.0–14.5) |
| Hispanic female | 40.9 (24.4) | 67.4 (44.3) | 26.4 (12.7–40.2) |
| Asian male | 23.0 (18.6) | 29.9 (29.3) | 6.9 (−3.5–17.3) |
| Asian female | 25.4 (19.3) | 59.9 (41.1) | 34.5 (21.7–47.3) |
| First Suicide-related Diagnosis (per 1,000) | |||
| White male | 4.5 (8.2) | 5.5 (13.6) | 1.0 (−0.6–2.6) |
| White female | 5.0 (8.5) | 7.7 (16.1) | 2.7 (0.9–4.5) |
| Black male | 3.0 (6.9) | 3.3 (9.8) | 0.4 (−1.2–1.9) |
| Black female | 5.1 (8.7) | 9.7 (17.5) | 4.6 (2.2–6.9) |
| Hispanic male | 4.2 (7.9) | 6.9 (14.7) | 2.8 (−1.8–7.3) |
| Hispanic female | 4.8 (8.5) | 7.8 (15.5) | 3.0 (−1.8–7.8) |
| Asian male | 5.8 (9.5) | 3.8 (15.5) | −2.0 (−6.2–2.2) |
| Asian female | 2.8 (6.6) | 7.5 (14.9) | 4.8 (0.2–9.3) |
Mixed multilevel adjusted logistic regression analysis, nested level is individual patient and Department
Adjusted for age, insurance type, number of encounters, years in the data, number of complex chronic conditions, Elixhauser score, National Area Deprivation Index and Department of encounter
Relative disparities analysis
The results of the mixed multilevel adjusted logistic regression analysis of disparities during the pre-COVID-19 time period were compared to those reported during the pandemic, we found multiple changes over time among gender and racial subgroups, as compared to White males (the group presumed to be least impacted by racism and sexism). In terms of first depression diagnosis (Figure 5a), most notably, Black females had similar odds as White males to have a first depression diagnosis before the pandemic (OR 0.96, 95% CI 0.83, 1.11), but during the pandemic were more likely to have a depression diagnosis (OR 1.47, 95% CI 1.27–1.71), and the confidence intervals for the two time periods did not overlap, indicating a significant difference in relative odds between the two time periods for Black females as compared with White males.
Figure 5a. Forest Plot of the Odds Ratios and 95% Confidence Intervals for First Depression Diagnosis Before and During the COVID-19 Pandemic as Compared to White Males.
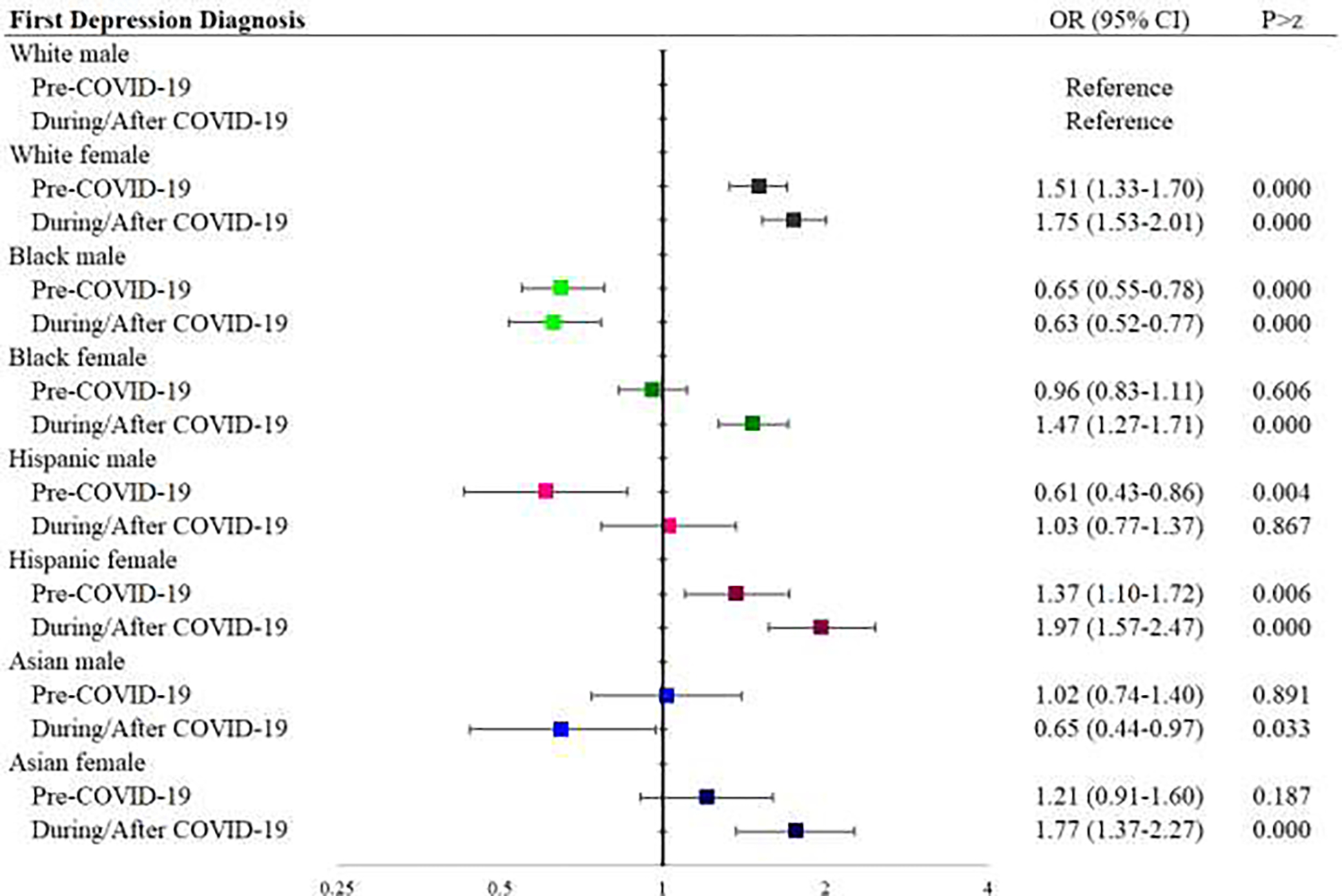
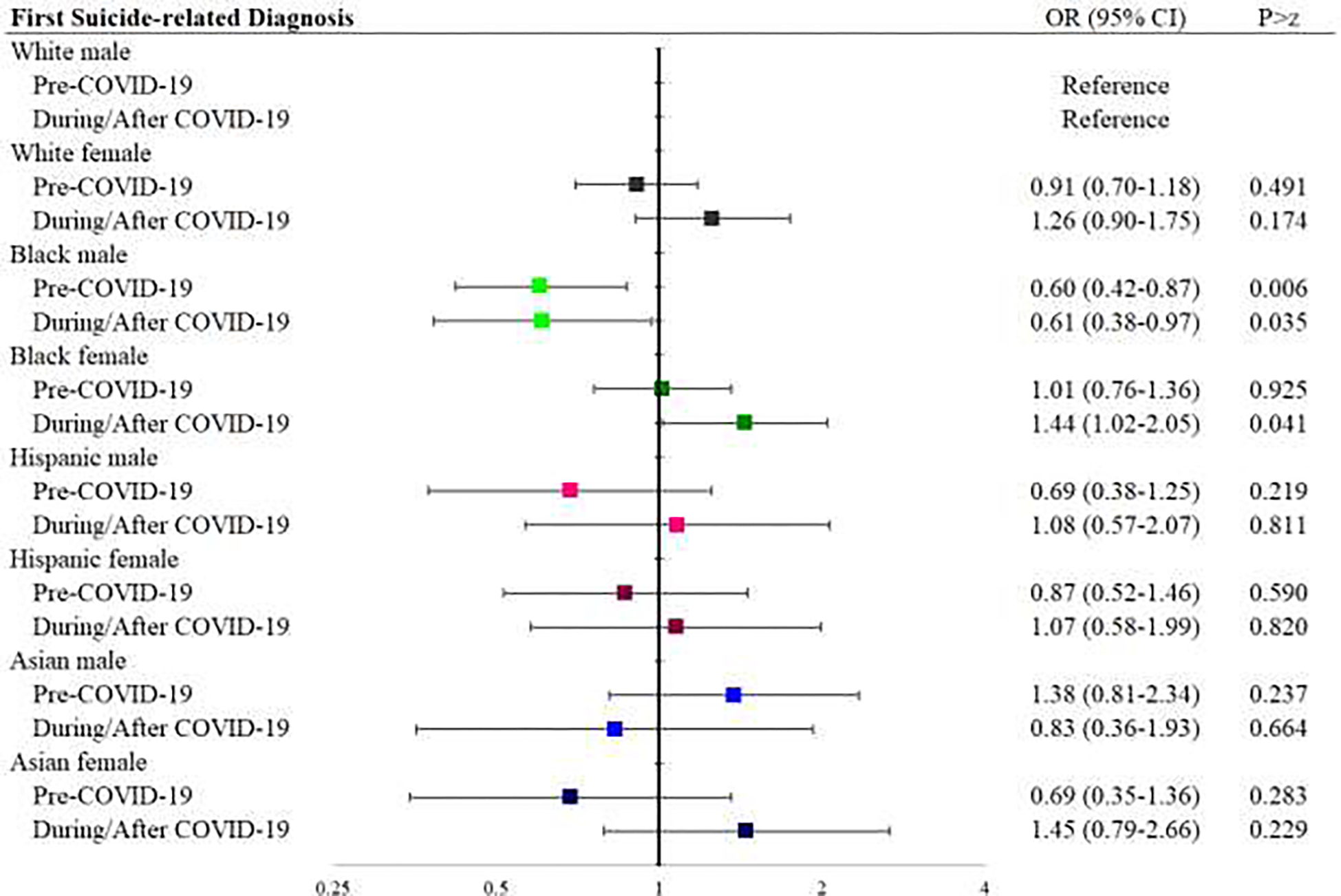
For the outcome of first anxiety diagnosis, Black females had lower odds than White males to have a first anxiety diagnosis before the pandemic (OR 0.67, 95% CI 0.59, 0.76), but similar odds of first anxiety diagnosis during the pandemic (OR 1.06, 95% CI 0.92–1.22). Asian females had lower odds of a first anxiety diagnosis before the pandemic (OR 0.79, 95% CI 0.62, 0.99), but during the pandemic were more likely than White males to have a first anxiety diagnosis (OR 1.33, 95% CI 1.06–1.67), in both cases the confidence intervals for the two time periods did not overlap, indicating a significant difference (Figure 5b). As for the outcome of first suicide risk-related diagnosis, Black males had lower odds of first suicide risk-related diagnosis, both before and during the pandemic, as compared to White males (pre- OR 0.60, 95% CI 0.42–0.87, post- OR 0.61, 95% CI 0.38–0.97). Other differences were not significant (Figure 5c).
Figure 5b. Forest Plot of the Odds Ratios and 95% Confidence Intervals for First Anxiety Diagnosis Before and During the COVID-19 Pandemic as Compared to White Males.

Figure 5c. Forest Plot of the Odds Ratios and 95% Confidence Intervals for First Suicide-related Diagnosis Before and During the COVID-19 Pandemic as Compared to White Males.
Discussion
We employed EMR data to quantify changes in mental health disparities among gender and racial subgroups of youths before and after the start of the COVID-19 pandemic. We were able to illuminate some specific patterns in mental health needs in this work, supporting previous work that has found sharply increasing depression, anxiety and/or suicidality in recent years among Black, Hispanic, and Asian females.1,5,10,28–30 Even when adjusting for a wide range of socioeconomic and health measures, the intersectional differences in mental health indicators persisted, and among most groups these indicators increased after the start of the pandemic. It is of note that we had access to data through the end of 2022, allowing us to analyze some of the most recent peri-pandemic data available. Although three years of data (2020–2022) were not sufficient to have a clear understanding of trajectories for our outcomes for every subgroup, it is troubling that females in minoritized groups are trending toward ever higher rates of depression, anxiety, and suicidal thoughts and/or behaviors in the post-pandemic period. While this data is not nationally representative, and thus not necessarily generalizable to the entire U.S., the study cohort represents a diverse, mid-Atlantic urban and suburban population of pediatric patients, and thus provides important call for future, larger scale research efforts to explore these trends among ethnically and racially diverse subgroups of pediatric patients.
There are limitations inherent in using EMR demographic data. Importantly, we have very little information about gender identity of sexual orientation, and we hope that future research will focus on the mental health effects of the unique intersectional stressors faced by subgroups within the LGBTQIA+ community. Additionally, we recognize that the broad racial and ethnic groupings used in this analysis mask the myriad of heterogeneous subgroups within each, and that because we used these broad groupings, we did not include 6.4% of patients in the analysis. It is an important direction for future research to develop best practices to address race and ethnicity in a more inclusive manner.
It is a limitation that for anxiety or depression to be recorded in the medical record, it must first be recognized and/or treated clinically. Given that racial and ethnic minoritized groups have historically been less likely to have recognized need from health providers for mental health treatment, more likely to have underlying depression or anxiety misdiagnosed as a behavioral disorder,31 and less likely to access services successfully if a need is identified, this hinders our ability to draw conclusions based on this data.32 We cannot determine, based on EMR data, whether the intersectional trends we are seeing represent actual increases in prevalence of these mental health indicators, better primary care identification of these mental health indicators, or increased willingness to ask providers for treatment of mental health concerns which may represent decreased cultural stigma or other cultural trends. It is most likely these findings are the result of all three factors, to some extent. Finally, we want to note that previous studies have found increasing trends in anxiety, depression and suicidal thoughts and behaviors in the years prior to the pandemic, and this makes it difficult to distinguish between the impact of the pandemic versus a continuation of existing trends.7,19,29,30
The historical under-recognition of anxiety and depression among minoritized subgroups makes our findings that Hispanic, Asian and Black youth in post-COVID years have rates of these disorders as high as White counterparts especially troubling, as the rates that we see using primary care data are very likely undercounting minoritized patients with mental health needs.33 We also caution that null results, such as the finding that Asian male youth are less likely than White males to have an anxiety or depression diagnosis post-pandemic, do not necessarily indicate an absence of mental health needs, but possibly indicate persistent under-recognized need for mental health treatment in this subgroup.
EMR-recorded suicidal thoughts and/or behaviors are less likely to be impacted by ascertainment bias, as these can be entered into the medical record through a positive in-office screening or through health exchange technology, meaning that suicide risk-related emergency visit would likely be recorded in a patient’s primary care record. That our findings related to suicidal thoughts and/or actions track closely with our anxiety and depression results would also argue against ascertainment bias as the cause for our findings. That said, in this work we group intentional self-harm (with suicidal intent) with suicidal ideation and attempt, which represent different constructs. Studying each of these as independent outcomes is an important direction for future research. We want to note that much previous work has focused on rates of death by suicide, which has created a narrative in the literature that suicide is a problem isolated largely to male youth.34,35 By using EMR data to explore rates of suicidal thoughts and/or behaviors as well as depression and anxiety, we are able to see a broader picture that includes female youth, a subgroup who do not die by suicide as often as male peers, but who are still clearly in need of screening and mental health care, including suicide prevention resources.
White males and females were used as the comparison group in the graphs, because these groups have historically not been impacted by structural racism and in relation to health care access, nor have they experienced the stressors of belonging to a racial or ethnic minoritized group. White males were used as the reference group in the regression models focused on disparities for a similar reason, as they have generally been less impacted by racism and sexism in relation to mental health care. In the disparities analysis, we are most interested in whether the comparative odds (as compared to White males) have changed over time for various race, ethnic and gender subgroups. This is not to indicate that rates of depression, anxiety and suicide have not also been rising among White males, we can see clearly from the AMD analysis that White males have trended higher in depression and anxiety diagnoses since the pandemic as have Black and Hispanic males. Using an intersectional lens in this analysis allowed us to tease out gender and race/ethnicity-specific patterns in mental health indicators that may be missed if investigators focus solely on gender, race or ethnicity as groupings of interest, which supports recent trends supporting intersectional approaches to mental health research.4,5
Our results support previous studies indicating that suicide-related diagnosis trends continue to rise at an alarming rate among young females, especially Black, Asian and Hispanic females. In contrast, rates have plateaued or decreased among young males and White females since 2021, suggesting some young people may be recovering from the toll the pandemic has taken on their mental health, while others continue to struggle immensely. Disparities in receiving mental health specialty care, for example, treatment from a therapist, have been demonstrated in previous studies and may be contributing to these trends.32,33 Whether related to the differences in primary care or mental health access available to minoritized groups, the under recognition of the mental health disorders in these groups, or the inequity in community and school resources available, an urgent and comprehensive call to action is necessary.33,36 Important next steps include universal screening of youths in multiple settings including schools and in primary care, broadening our understanding of effective treatment and support options in minoritized patients, and increasing support services to these patients and families at school, work, and home.7,33,37
Supplementary Material
Table 3: Odds of First Diagnosis for Depression, Anxiety, or Suicide by Race and Gender Subgroup, Before versus During the COVID-19* Pandemic.
n= 29,117 years=2015–2022
| Pre-COVID (2015–2019) | During/Post-COVID (2020–2022) | |||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio | 95% conf. interval | P>z | Odds ratio | 95% conf. interval | P>z | |||
| First Depression Diagnosis | ||||||||
| White male | Reference | Reference | ||||||
| White female | 1.51 | 1.33 | 1.70 | 0.000 | 1.75 | 1.53 | 2.01 | 0.000 |
| Black male | 0.65 | 0.55 | 0.78 | 0.000 | 0.63 | 0.52 | 0.77 | 0.000 |
| Black female | 0.96 | 0.83 | 1.11 | 0.606 | 1.47 | 1.27 | 1.71 | 0.000 |
| Hispanic male | 0.61 | 0.43 | 0.86 | 0.004 | 1.03 | 0.77 | 1.37 | 0.867 |
| Hispanic female | 1.37 | 1.10 | 1.72 | 0.006 | 1.97 | 1.57 | 2.47 | 0.000 |
| Asian male | 1.02 | 0.74 | 1.40 | 0.891 | 0.65 | 0.44 | 0.97 | 0.033 |
| Asian female | 1.21 | 0.91 | 1.60 | 0.187 | 1.77 | 1.37 | 2.27 | 0.000 |
| First Anxiety Diagnosis | ||||||||
| White male | Reference | Reference | ||||||
| White female | 1.40 | 1.28 | 1.54 | 0.000 | 1.63 | 1.45 | 1.83 | 0.000 |
| Black male | 0.47 | 0.40 | 0.54 | 0.000 | 0.55 | 0.46 | 0.66 | 0.000 |
| Black female | 0.67 | 0.59 | 0.76 | 0.000 | 1.06 | 0.92 | 1.22 | 0.406 |
| Hispanic male | 0.79 | 0.63 | 0.98 | 0.032 | 0.74 | 0.56 | 0.99 | 0.044 |
| Hispanic female | 0.98 | 0.81 | 1.19 | 0.823 | 1.48 | 1.19 | 1.83 | 0.000 |
| Asian male | 0.67 | 0.52 | 0.88 | 0.003 | 0.70 | 0.51 | 0.97 | 0.030 |
| Asian female | 0.79 | 0.62 | 0.99 | 0.044 | 1.33 | 1.06 | 1.67 | 0.013 |
| First Suicide-related Diagnosis | ||||||||
| White male | Reference | Reference | ||||||
| White female | 0.91 | 0.70 | 1.18 | 0.491 | 1.26 | 0.90 | 1.75 | 0.174 |
| Black male | 0.60 | 0.42 | 0.87 | 0.006 | 0.61 | 0.38 | 0.97 | 0.035 |
| Black female | 1.01 | 0.76 | 1.36 | 0.925 | 1.44 | 1.02 | 2.05 | 0.041 |
| Hispanic male | 0.69 | 0.38 | 1.25 | 0.219 | 1.08 | 0.57 | 2.07 | 0.811 |
| Hispanic female | 0.87 | 0.52 | 1.46 | 0.590 | 1.07 | 0.58 | 1.99 | 0.820 |
| Asian male | 1.38 | 0.81 | 2.34 | 0.237 | 0.83 | 0.36 | 1.93 | 0.664 |
| Asian female | 0.69 | 0.35 | 1.36 | 0.283 | 1.45 | 0.79 | 2.66 | 0.229 |
Mixed multilevel logistic regression analysis, nested levels are individual patient and Department
Adjusted for age, insurance type, number of encounters, years in the data, number of complex chronic conditions, year, Elixhauser score, National Area Deprivation Index and Department of encounter
Bold= Confidence Intervals for the two time periods do not overlap
What’s New:
We used an intersectional approach to elucidate changes in disparities during the COVID-19 pandemic. We found that rates of depression, anxiety, and suicidality in youth increased in the post-pandemic period and many pre-existing disparities between subgroups, especially females, widened significantly.
Funding:
This work was supported by the National Institute of Health /BIRCWH Grant mechanism (Dr. Prichett, K12AR084229), the Stanley Medical Research Institute (grant #7R-1690), the National Institute of Drug Abuse (Dr. Young, K23 DA044288). This work was also supported by Johns Hopkins Biostatistics, Epidemiology and Data Management (BEAD) Core (internal funding); Dr. Young has received research support from NIH, the Brain and Behavior Research Foundation, Supernus Pharmaceuticals and Psychnostics, LLC. She has served as a consultant to NIH, PCORI and the Montana State University’s American Indian/Alaska Native Clinical & Translational Research Program, on the Board of Directors for Helping Give Away Psychological Science and on the editorial boards for the Journal of Clinical Child and Adolescent Psychology and Evidence-Based Practice in Child and Adolescent Mental Health. All other authors certify that they have no affiliations with or involvement in any organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript. The findings and conclusions in this article are those of the authors and do not necessarily reflect the opinions of the National Institute of Health.
Abbreviations:
- ED
Emergency Department
- EMR
Electronic Medical Record
- PCP
Primary care physician
- JHCP
Johns Hopkins Community Physicians
Footnotes
Declaration of interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
The authors have received support from the following for the production of this manuscript:
Grants and Contracts: NIH BIRCWH (K12 award) (Dr. Prichett), NIDA (K23 award) (Dr. Young), Intramural JHU award (Dr. Young) Stanley Medical Research Institute (Dr. Yolken, Dr. Severance)
Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events: Only to non-profit academic institutions
Leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid:
Helping Give Away Psychological Science (503b) (Dr. Young) (Board member)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Center for Health Statistics. About multiple causes of death, 1999–2023. Hyattsville, MD: US Department of Health and Human Services. CDC. National Center for Health Statstics. Published June 2023. Accessed June 12, 2023. https://wonder.cdc.gov/mcd.html [Google Scholar]
- 2.Lo CB, Bridge JA, Shi J, Ludwig L, Stanley RM. Children’s Mental Health Emergency Department Visits: 2007–2016. Pediatrics. 2020;145(6):e20191536. doi: 10.1542/peds.2019-1536 [DOI] [PubMed] [Google Scholar]
- 3.Bommersbach TJ, McKean AJ, Olfson M, Rhee TG. National Trends in Mental Health–Related Emergency Department Visits Among Youth, 2011–2020. JAMA. 2023;329(17):1469. doi: 10.1001/jama.2023.4809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Standley CJ. Expanding our paradigms: Intersectional and socioecological approaches to suicide prevention. Death Stud. 2022;46(1):224–232. doi: 10.1080/07481187.2020.1725934 [DOI] [PubMed] [Google Scholar]
- 5.Forrest LN, Beccia AL, Exten C, Gehman S, Ansell EB. Intersectional Prevalence of Suicide Ideation, Plan, and Attempt Based on Gender, Sexual Orientation, Race and Ethnicity, and Rurality. JAMA Psychiatry. Published online July 19, 2023. doi: 10.1001/jamapsychiatry.2023.2295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.English D, Lambert SF, Tynes BM, Bowleg L, Zea MC, Howard LC. Daily multidimensional racial discrimination among Black U.S. American adolescents. J Appl Dev Psychol. 2020;66:101068. doi: 10.1016/j.appdev.2019.101068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bridge JA, Ruch DA, Sheftall AH, et al. Youth Suicide During the First Year of the COVID-19 Pandemic. Pediatrics. 2023;151(3):e2022058375. doi: 10.1542/peds.2022-058375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bor J, Venkataramani AS, Williams DR, Tsai AC. Police killings and their spillover effects on the mental health of black Americans: a population-based, quasi-experimental study. The Lancet. 2018;392(10144):302–310. doi: 10.1016/S0140-6736(18)31130-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheftall AH, Vakil F, Ruch DA, Boyd RC, Lindsey MA, Bridge JA. Black Youth Suicide: Investigation of Current Trends and Precipitating Circumstances. J Am Acad Child Adolesc Psychiatry. 2022;61(5):662–675. doi: 10.1016/j.jaac.2021.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu SR, Davis EP, Palma AM, Stern HS, Sandman CA, Glynn LM. Experiences of COVID-19-Related Racism and Impact on Depression Trajectories Among Racially/Ethnically Minoritized Adolescents. J Adolesc Health. 2023;72(6):885–891. doi: 10.1016/j.jadohealth.2022.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roche KM, Huebner DM, Lambert SF, Little TD. COVID-19 Stressors and Latinx Adolescents’ Mental Health Symptomology and School Performance: A Prospective Study. J Youth Adolesc. 2022;51(6):1031–1047. doi: 10.1007/s10964-022-01603-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shobeiri P, Kalantari A, Teixeira AL, Rezaei N. Shedding light on biological sex differences and microbiota–gut–brain axis: a comprehensive review of its roles in neuropsychiatric disorders. Biol Sex Differ. 2022;13(1):12. doi: 10.1186/s13293-022-00422-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaycox LH, Asarnow JR, Sherbourne CD, Rea MM, LaBorde AP, Wells KB. Adolescent Primary Care Patients’ Preferences for Depression Treatment. Adm Policy Ment Health Ment Health Serv Res. 2006;33(2):198–207. doi: 10.1007/s10488-006-0033-7 [DOI] [PubMed] [Google Scholar]
- 14.Stafford AM, Garbuz T, Etter DJ, et al. The Natural Course of Adolescent Depression Treatment in the Primary Care Setting. J Pediatr Health Care. 2020;34(1):38–46. doi: 10.1016/j.pedhc.2019.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merikangas KR, He J ping, Burstein M, et al. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Runkle JD, Yadav S, Michael K, Green S, Weiser J, Sugg MM. Crisis Response and Suicidal Patterns in U.S. Youth Before and During COVID-19: A Latent Class Analysis. J Adolesc Health. 2022;70(1):48–56. doi: 10.1016/j.jadohealth.2021.10.003 [DOI] [PubMed] [Google Scholar]
- 17.Barzilay S, Apter A. Recent research advances in identification and prevention of youth suicide risk. Curr Opin Psychiatry. 2022;35(6):395–400. doi: 10.1097/YCO.0000000000000816 [DOI] [PubMed] [Google Scholar]
- 18.Kauhanen L, Wan Mohd Yunus WMA, Lempinen L, et al. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. Published online August 12, 2022. doi: 10.1007/s00787-022-02060-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hannan C, Mayne SL, Kelly MK, et al. Trends in Positive Depression and Suicide Risk Screens in Pediatric Primary Care During COVID-19. Acad Pediatr. 2023;23(6):1159–1165. doi: 10.1016/j.acap.2022.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montero-Marin J, Hinze V, Mansfield K, et al. Young People’s Mental Health Changes, Risk, and Resilience During the COVID-19 Pandemic. JAMA Netw Open. 2023;6(9):e2335016. doi: 10.1001/jamanetworkopen.2023.35016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elia J, Pajer K, Prasad R, et al. Electronic health records identify timely trends in childhood mental health conditions. Child Adolesc Psychiatry Ment Health. 2023;17(1):107. doi: 10.1186/s13034-023-00650-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hudson JI, Pope HG, Glynn RJ. The Cross-Sectional Cohort Study: An Underutilized Design. Epidemiology. 2005;16(3):355–359. doi: 10.1097/01.ede.0000158224.50593.e3 [DOI] [PubMed] [Google Scholar]
- 23.Ghaferi AA, Schwartz TA, Pawlik TM. STROBE Reporting Guidelines for Observational Studies. JAMA Surg. 2021;156(6):577. doi: 10.1001/jamasurg.2021.0528 [DOI] [PubMed] [Google Scholar]
- 24.Center for Health Disparities Research. Neighborhood Atlas, Area Deprivation Index. Published January 2019. Accessed August 23, 2023. https://www.neighborhoodatlas.medicine.wisc.edu
- 25.Menendez ME, Neuhaus V, van Dijk NC, Ring D. The Elixhauser Comorbidity Method Outperforms the Charlson Index in Predicting Inpatient Death After Orthopaedic Surgery. Clin Orthop. 2014;472(9):2878–2886. doi: 10.1007/s11999-014-3686-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14(1):199. doi: 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.StataCorp. Stata Statistical Software: Release 17. Published online 2021. [Google Scholar]
- 28.Strashny A, Cairns C, Ashman J. Emergency Department Visits With Suicidal Ideation: United States, 2016–2020. National Center for Health Statistics (U.S.); 2023. doi: 10.15620/cdc:125704 [DOI] [PubMed] [Google Scholar]
- 29.CDC. Centers for Disease Control and Prevention. 2019. Youth Risk Behavior Survey Questionnaire. Available at: www.cdc.gov/yrbs. Accessed on 5/4/23. [Google Scholar]
- 30.Shankar LG, Habich M, Rosenman M, Arzu J, Lales G, Hoffmann JA. Mental Health Emergency Department Visits by Children Before and During the COVID-19 Pandemic. Acad Pediatr. 2022;22(7):1127–1132. doi: 10.1016/j.acap.2022.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Valdez CR, Rodgers CRR, Gudiño OG, et al. Translating research to support practitioners in addressing disparities in child and adolescent mental health and services in the United States. Cultur Divers Ethnic Minor Psychol. 2019;25(1):126–135. doi: 10.1037/cdp0000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prichett LM, Yolken RH, Severance EG, et al. Racial and Gender Disparities in Suicide and Mental Health Care Utilization in a Pediatric Primary Care Setting. J Adolesc Health. Published online October 2023:S1054139X23004469. doi: 10.1016/j.jadohealth.2023.08.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goodwill JR, Yasui M. Mental Health Service Utilization, School Experiences, and Religious Involvement Among a National Sample of Black Adolescents Who Attempted Suicide: Examining Within and Cross-Race Group Differences. Child Adolesc Soc Work J. Published online October 14, 2022. doi: 10.1007/s10560-022-00888-8 [DOI] [Google Scholar]
- 34.Entrup P, Brodsky L, Trimble C, et al. Years of life lost due to deaths of despair and COVID-19 in the United States in 2020: patterns of excess mortality by gender, race and ethnicity. Int J Equity Health. 2023;22(1):161. doi: 10.1186/s12939-023-01949-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trigylidas TE, Reynolds EM, Teshome G, Dykstra HK, Lichenstein R. Paediatric suicide in the USA: Analysis of the national child death case reporting system. Inj Prev. 2016;22(4):268–273. doi: 10.1136/injuryprev-2015-041796 [DOI] [PubMed] [Google Scholar]
- 36.American Academy of Pediatrics. Suicide: Blueprint for Youth Suicide Prevention. Published 2023. Accessed September 15, 2023. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/
- 37.Robinson J, Cox G, Malone A, et al. A Systematic Review of School-Based Interventions Aimed at Preventing, Treating, and Responding to Suicide- Related Behavior in Young People. Crisis. 2013;34(3):164–182. doi: 10.1027/0227-5910/a000168 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


