Abstract
INTRODUCTION:
Higher levels of perceived stress are associated with adverse cardiovascular health. It is plausible that these associations are attenuated among individuals with positive psychological factors such as social support and health enhancing behaviors. Therefore, this study examined longitudinal associations of chronic stress with cardiovascular disease (CVD) events, and whether social support and physical activity (PA) modify these associations.
METHODS:
Data from 3,401 adults (mean age 40.2 years; 46.7% Black; 56.2% women) from the Coronary Artery Risk Development in Young Adults (CARDIA) study, with no prior CVD event in 2000–2001 were analyzed. Chronic stress lasting ≥6 months across five life domains (work, financial, relationships, health of self, and health of close other) was self-reported. Adjudicated CVD events (fatal/or nonfatal CVD event) were ascertained yearly through 2020. PA and social support were self-reported via questionnaires. Statistical analyses were conducted in 2023 using multivariable stepwise Accelerated Failure Time analysis to assess associations between key study variables.
RESULTS:
Mean chronic stress score was 1.30±1.33 stressors and, by 2020, 220 participants had experienced a CVD event. Chronic stress was associated with lowered survival (time ratio: 0.92; 95% CI: 0.854–0.989), when adjusted for sociodemographic and lifestyle variables but no longer significant when adjusting for clinical factors. Neither PA nor social support were significant modifiers (all ps>0.05).
CONCLUSIONS:
Chronic stress was associated with risk of having a CVD event among middle-aged adults, due at least in part to clinical mediators. Studies should continue exploring positive psychosocial and behavioral factors that may modify this association.
Keywords: Chronic stress, cardiovascular disease, physical activity, social support, adults
INTRODUCTION
Evidence from laboratory and clinical studies have demonstrated that high chronic psychological stress is associated with cardiovascular disease (CVD).1–8 For example, investigators examining multiple stress indicators such as chronic and traumatic stress have observed that chronic stress is associated with higher prevalence of coronary heart disease, hypertension, and stroke.2 More recently, in a population-based cohort of adults living in low-, middle-, and high-income countries, investigators reported that adults experiencing high levels of psychological stress had greater incidence of CVD and stroke even after adjusting for sociodemographic and behavioral factors, diabetes, hypertension and family history of CVD.8 Such evidence underscores the importance of identifying and promoting strategies to combat the detrimental influence of stress on cardiovascular disease risk among adults.
One such strategy is regular engagement in physical activity (PA). Habitual, higher intensity leisure-time PA (e.g., exercise) provides numerous health benefits, including the buffering of psychological stress and the physiological stress responses through what is known as the cross-stressor adaptation hypothesis.9 Studies exploring the cross-stressor adaptation hypothesis and the buffering effects of exercise have shown that both acute and longer-term exercise dampens stress reactivity, in turn protecting against the detrimental effects of stress on cardiovascular health among adults and children.10–13 Similarly, greater social support in its numerous forms has been hypothesized to negate or otherwise weaken the negative effects of stress on psychological wellbeing and health outcomes by providing individuals with access to psychosocial resources, in turn relieving mental and physical burdens arising from stress.14–16 For example, Bowen and colleagues found that informational support consistently buffered the association between momentary stress and ambulatory systolic and diastolic blood pressure.16 More recently, investigators have also observed that higher perceived social support quality buffers blood pressure reactivity in response to a laboratory stressor among older adults.17
Thus, the present study aimed to explore whether chronic stress across multiple domains at middle age is associated with incident CVD and whether positive psycho-behavioral factors (social support and PA) modify this association. Based on previous research, it was hypothesized that chronic stress would be associated with higher risk of CVD events during follow-up, and that greater social support and greater participation in higher intensity activity would buffer the association between chronic stress and cardiovascular events.
METHODS
Study Sample
The Coronary Artery Risk Development in Young Adults (CARDIA) study is an ongoing longitudinal cohort study of Black and White men and women, aged 18–30 years at baseline. The study enrolled 5,115 participants who took part in a clinical exam in 1985–86 (baseline of the CARDIA study) at one of four field centers: Birmingham, AL; Minneapolis, MN; Chicago, IL; or Oakland, CA. Since that time, additional examinations have been held approximately every 2–5 years. Details regarding the eligibility criteria, methods of participant selection, and follow-up have been previously reported.18
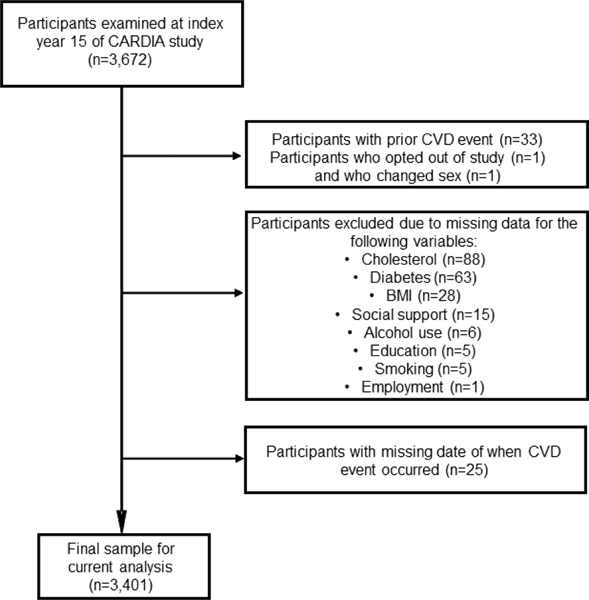
For the current study, data from index year 15 of the CARDIA study was used. A total of 3,672 participants were examined at index year 15, and among these individuals, 33 were excluded presently, due to having prior CVD or CVD events at index year 15. An additional 238 participants were excluded due to missing covariates (n=213) or not having a date for when their CVD event occurred (n=25) (see Fig. 1). In total, the final analytical sample comprised of 3,401 CARDIA participants with complete data at index year 15 through the calendar year 2020. The institutional review board at each center approved all study protocols, and written informed consent was obtained from each participant at each exam.
Fig. 1.
Sample inclusion diagram.
Measures
Adjudicated incident CVD was defined as CVD events that included fatal and nonfatal myocardial infarction, acute coronary syndrome not resulting in infarction, stroke, transient ischemic attacks, heart failure, carotid artery disease, peripheral arterial disease, congestive heart failure, and other fatal atherosclerotic events. New CVD cases/events were assessed during scheduled study visits and yearly phone interviews conducted by the CARDIA study staff and verified by two physician members of CARDIA.19 All disagreements were resolved by full committee review. This protocol of ascertaining CVD events has been used throughout the CARDIA study. The follow-up for cardiovascular events for this current analysis occurred from index year 15 until the end of the calendar year 2020, approximately a 20-year follow-up period.
Chronic stress was measured using a 5-item chronic stress burden scale that assessed the number of ongoing stressors experienced by respondents for at least 6 months at index year 15. The scale included chronic stressors stemming from five major life domains: i) health-related problem of self, ii) of close other, iii) occupational difficulty, iv) financial strain, and v) relationship difficulties. Example questions from the chronic burden scale were: ‘please indicate whether you have experienced ongoing difficulties in your job or ability to work’, and ‘please indicate whether you have experienced ongoing difficulties in a relationship with someone close to you’. For each question, participants indicated whether they experienced difficulties stemming from the domains longer than 6 months, and how stressful each experience had been, on a 4-point scale anchored by 1 (no), 2 (yes, but not very stressful), 3 (yes, moderately stressful), to 4 (yes, very stressful). For each of the 5 domains, responses were recoded as ‘0’ for responses= 1 and 2 (no/low stress) and recoded as ‘1’ for responses= 3 and 4 (moderate/high stress). A domain was considered stressful if respondents stated the experience caused moderate or high stress, and not stressful if they stated the experience caused no or low stress, in line with prior investigators.20,21 The number of stressful domains were summed together to give a total chronic stress score for each participant that ranged from 0–5. The questionnaire is publicly available and can be accessed on the CARDIA study website (https://www.cardia.dopm.uab.edu/).
The covariates that were included in the analyses were self-reported age, race, sex, education, employment status, field center, BMI, hypertension, diabetes, smoking, and alcohol use at index year 15. Note that race was presently conceptualized as a social construct/label used as a proxy measure for exposure to discrimination, socioeconomic disadvantage, and other racialized contextual-level exposures, and not an assessment of biological differences. Education was operationalized as an individual’s highest earned degree (high school diploma/GED or less, associate degree, bachelor’s degree, master’s degree, doctorate/professional degree, and other). Employment status was operationalized as currently employed full-time or not. Participants’ alcohol use was operationalized as alcohol intake per day (in ml), while cigarette smoking was categorized as non-, former-, and current. Height (to the nearest 0.5 cm) and body weight (to the nearest 0.2 kg) were measured and used to calculate participants’ BMI. Hypertension was defined as a systolic blood pressure ≥140 mm Hg, and/or diastolic blood pressure ≥90 mm Hg, and/or taking antihypertensive medications based on the former guidelines in place at the time of data collection. Diabetes was defined as a fasting serum glucose of ≥126 mg/dL, 2-hr glucose≥200 mg/dL, HbA1c ≥6.5%, or use of antihyperglycemic medications. Hyperlipidemia was defined as serum total cholesterol levels of ≥240 mg/dL, low-density lipoprotein cholesterol ≥160 mg/dL, triglycerides ≥200 mg/dL, or high-density lipoprotein cholesterol of ≤40 mg/dL, and/or taking a cholesterol-lowering medication.
In terms of moderators, social support was queried at index year 15 of the CARDIA study using the four positive social interaction questions in the social support and conflict questionnaire—an 8-item self-reported questionnaire that includes four positive and four negative social interactions adapted from Shuster and colleagues,22 and has been previously used by prior CARDIA investigators.23 Each item is rated on a Likert-type scale anchored by 0 (‘Not at all’) and 3 (‘A lot’). All four positive social interaction items were summed to obtain the total social support score, with higher scores corresponding to greater social support. PA over the past year was estimated from the interviewer administered CARDIA PA history questionnaire at index year 15. CARDIA participants reported the total number of months they participated in 13 different activity types/categories over the past year. Participants were then asked to report how many months they participated in each activity/category for at least one hour in at least one month, and the frequency of participating in each activity that was performed for at least an hour in the past month. Each reported activity was then scored in exercise units (EU)—a weighted sum derived from intensity of the activities (ranging from 3 to 8 metabolic equivalents), frequency, and duration of PA.24,25 In alignment with prior CARDIA publications, inadequate PA was defined as EUs less than 300,25 while meeting 2018 Physical Activity Guidelines for Americans as greater than or equal to 300 EUs.
Statistical Analysis
All data analyses were conducted in the year 2023 using Stata 17.0 (StataCorp LP, College Station, TX). Means and frequencies were determined for the participant characteristics across chronic stress levels. Accelerated Failure Time (AFT) models were used to evaluate whether chronic stress was associated with incident CVD, following the violation of the Cox Proportional Hazards assumption when using multivariable Cox proportional hazards regression models (see Appendix Table 1 for Cox proportional hazards results). The generalized gamma (GG) distribution was identified as the AFT model with the lowest AIC and BIC values and 4 multivariable GG models were fitted for the main analysis. Participants were considered at risk of developing CVD from index year 15 until either the follow up date at which CVD was identified or censored as the last follow up date. Model 1 of the GG model included the covariates age, race, and sex. Model 2 was adjusted for employment status, education, field center, and model 1 covariates. Model 3 was adjusted for alcohol use, smoking, and model 2 covariates. Model 4 was adjusted for BMI, hypertension, diabetes, hyperlipidemia, and model 3 covariates. The a priori hypothesis that PA or social support modify the association between chronic stress and incident CVD was tested by adding a multiplicative interaction term (e.g., chronic stress*social support score) for social support and PA (each separately) into the fully adjusted model (model 4). A continuous social support variable and a dichotomous PA variable corresponding to participation in < or ≥ 300 EUs25 was used in interaction models. To test if there was any difference by race in the association between chronic stress and CVD events, a multiplicative interaction term race*chronic stress was added into the fully adjusted model. Statistical significance was set at p < 0.05.
RESULTS
Participant characteristics (mean and SD or %) across chronic stress levels are reported in Table 1. By the end of the follow-up period, 220 participants had experienced a CVD event. The median follow-up time was 19.2 years, whereas the maximum follow-up time was 22.1 years. In total, study participants were: 56.2% women (43.8% men), 46.7% Black (53.3% White) and had a mean age of 40.2±3.6 years. Mean chronic stress score was 1.30±1.33 stressors within the sample and ranged from 0 (no/low stress across all 5 stressors) to 5 (moderate/high stress across all 5 stressors). A total of 31.31% of the sample reported relationship difficulties with someone close causing ongoing moderate or very stressful experiences. This domain was followed by chronic stress stemming from ongoing financial stress (30.55% of the sample), serious ongoing health problems of someone close (29.19%), ongoing occupational difficulty (26.33%), and serious ongoing health problem of self (11.95%) (see Appendix Table 2). In total, approximately 46.9% of the participants met or exceeded the PA guideline threshold of 300 EUs.
Table 1.
Participant characteristics.
| Variables | Total Sample (n=3,401) Mean (SD) | No chronic stress (n=1,247) | Low chronic stress (n=902) | Moderate chronic stress (n=579) | High chronic stress (n=673) |
|---|---|---|---|---|---|
| Age at index year 15 (years) | 40.2 (3.6) | 40.0 (3.6) | 40.2 (3.6) | 40.3 (3.6) | 40.4 (3.5) |
| Sex (% female) | 56.2 | 50.4 | 55.1 | 61.0 | 64.2 |
| Race (% Black) | 46.7 | 52.9 | 41.6 | 45.1 | 43.4 |
| Chronic stress score (range 0–5) | 1.30 (1.33) | 0 | 1 | 2 | 3.50 (0.69) |
| BMI (kg/m2) | 28.7 (6.8) | 28.5 (6.5) | 27.9 (6.1) | 29.1 (7.5) | 29.7 (7.5) |
| Blood pressure (% hypertensive) | 15.6 | 15.8 | 11.9 | 16.8 | 19.3 |
| Diabetes (% diabetic) | 3.65 | 2.97 | 4.32 | 3.11 | 4.5 |
| Hyperlipidemia (% with hyperlipidemia) | 32.2 | 31.3 | 29.7 | 32.1 | 37.4 |
| Education (%) | |||||
| High school diploma/GED or less than high school | 38.81 | 41.06 | 35.48 | 33.71 | 39.08 |
| Associates degree | 11.17 | 11.95 | 11.53 | 9.60 | 10.55 |
| Bachelors degree | 27.55 | 25.98 | 28.82 | 29.38 | 28.38 |
| Graduate or professional degree | 16.73 | 15.15 | 18.74 | 17.32 | 16.94 |
| Other | 5.73 | 5.85 | 5.43 | 6.97 | 5.05 |
| Work status (% full time) | 74.8 | 77.0 | 78.2 | 72.5 | 68.8 |
| Smoking (% non-smoker or former smoker) | 78.4 | 79.2 | 82.5 | 77.2 | 72.5 |
| Alcohol intake (ml/day) | 11.2 (25.4) | 11.0 (22.8) | 10.4 (19.7) | 11.4 (23.6) | 12.2 (35.9) |
| Physical activity (% ≥ 300 EUs) | 46.9 | 48.0 | 49.3 | 46.8 | 41.6 |
| Social support score (range 0–12) | 10.0 (2.3) | 10.4 (2.0) | 10.2 (2.2) | 9.8 (2.4) | 9.4 (2.7) |
Statistics are reported in either mean and standard deviation (SD) or percentage (%). No chronic stress = stress score of 0; low chronic stress = stress score of 1; moderate chronic stress = stress score of 2; high chronic stress = stress score of 3 or more.
The associations between chronic stress and CVD events are seen in Table 2 and overall survival probability stratified across chronic stress levels can be seen in Fig. 2 (Kaplan-Meier curve). Every one-unit increase in chronic stress was associated with a 9.3% reduction in mean survival time (time ratio: 0.907; 95% CI: 0.842–0.978) when adjusted for demographic variables (model 1). Similarly, a one-unit increase in chronic stress was also associated with a 9.2% reduction in mean survival time (time ratio: 0.908; 95% CI: 0.842–0.978) when adjusted for demographic and socioeconomic factors (model 2). A one-unit increase in chronic stress was associated with 8.1% reduction in mean survival time (time ratio: 0.919; 95% CI: 0.854–0.989), when adjusted for sociodemographic and behavioral lifestyle factors (model 3). When adjusting for potential clinical mediators (model 4) however, chronic stress was no longer associated with CVD events (time ratio: 0.968; 95% CI: 0.902–1.04).
Table 2.
Chronic stress and incidence of CVD events.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Survival | ||||
| Predictor | Time ratio (95%CI) | Time ratio (95%CI) | Time ratio (95%CI) | Time ratio (95%CI) |
| Chronic stress burden | 0.907 (0.842, 0.978) | 0.908 (0.842, 0.978) | 0.919 (0.854–0.989) | 0.968 (0.902–1.04) |
| Chronic stress*PA | -- | -- | -- | 0.979 (0.85, 1.13) |
| Chronic stress*Social Support | -- | -- | -- | 1.00 (0.98, 1.03) |
Model 1: Adjusted for covariates age, race and sex.
Model 2: Adjusted for employment status, highest obtained educational degree, field center, and all model 1 covariates.
Model 3: Adjusted for smoking status, alcohol consumption, and all model 2 covariates.
Model 4: Adjusted for BMI, hypertension-, diabetes-status, hyperlipidemia, and all model 3 covariates. Note: Boldface indicates statistical significance (p<0.05).
Fig. 2.
Kaplan-Meier curve of survival probability across chronic stress levels. Time 0 corresponds to index year 15 of the CARDIA study.
When testing for the modifying effects of PA and social support in separate models, neither PA nor social support were observed to be significant modifiers of the association between chronic stress and CVD events (all ps>0.05). There was also no significant race*chronic stress interaction (p>0.05).
DISCUSSION
In partial support of the study hypothesis, chronic stress was associated with a reduction in mean survival time/accelerated time of subsequent CVD events when adjusting for sociodemographic and behavioral factors; however, when adjusting for clinical factors such as hypertension, this association was no longer significant. Moreover, neither PA nor social support modified the association between chronic stress and CVD events. Given that prior studies have observed links between psychological stress and CVD events, the present findings again point to the adverse negative long-term influence of chronic stress on cardiovascular health, but also highlight the need for identifying potential stress buffers in middle-aged adults.
Presently, it was observed that chronic stress was associated with an accelerated time to CVD events in this sample of middle-aged Black and White adults when controlling for sociodemographic factors, employment, education, and field center location, and lifestyle factors consistent with prior studies (e.g. 8,26,27). However, further adjustments for clinically relevant factors led to this association being no longer significant and may potentially explain the pathways through which chronic stress impacts CVD risk. The physiological consequences of chronic stress on cardiovascular events are due, in part, to chronic or over-activation of the hypothalamic pituitary adrenal (HPA) axis and the sympathetic nervous system (SNS), leading to increased circulating glucocorticoids and a host of detrimental downstream effects on the cardiovascular system and metabolic processes.28 More specifically, these downstream effects include but are not limited to increased peripheral vascular resistance, upregulation of a pro-inflammatory state, visceral fat accumulation, insulin resistance, and behavioral changes such as increased intake of energy dense, highly palatable foods.28,29
Moreover, after adjusting for clinical (possible mediator variables), the association between chronic stress and CVD events was no longer significant. It is thus possible that the clinical factors are not only confounding variables, but are also in fact mediators within the causal pathway in the association between stress and CVD, given evidence from other investigations.30,31 Thus, it is reasonable to believe that part of the mechanistic link explaining the association between chronic stress and CVD may go beyond the traditional behavioral factors and social factors. Greater work is needed in this area of study.
One of the novel aspects of the current analyses is the consideration of habitual PA and social support as chronic stress buffers. Presently, neither PA nor social support were found to significantly modify in the association between chronic stress and CVD events. Empirical evidence has previously demonstrated the association between PA, fitness, and stress reduction (e.g.32,33). Furthermore, researchers have proposed that PA—particularly moderate-to-vigorous intensity PA—leads to biological adaptations resulting in more efficient cardiovascular stress responses and reduced arousal during periods or instances of stress.10 Likewise, increased levels of social support have been found to lower stress and dampen stress responses through a myriad of pathways that consists of instrumental, emotional, and informational assistance amongst others,34 in order to help individuals handle and cope with the stress they encounter. Although neither PA nor social support were significant moderators presently, future studies may seek to refine the PA variable using device-based measures as well as explore the effects of differing types of social support on this association.
Limitations
The present findings should be interpreted in light of limitations. One such limitation is solely measuring chronic stress in a self-reported manner without the inclusion of a biological/physiological chronic stress measure. Nevertheless, broadly captioning the source of stress was achieved (ongoing financial stress, ongoing health-related stress, ongoing relational stress, etc). Additionally, chronic stress from only one time point (index year 15 of CARDIA) was used and may not fully capture cumulative stress burden. Yet, it is widely accepted that ongoing stressors lasting greater than 6 months are considered chronic psychological stressors35. Future studies must consider cumulative lifetime stressors that include childhood stressors (e.g., adverse childhood events, childhood trauma), past-, and present socio-environmental stressors. Moreover, physical activity was self-reported, which is prone to reporting and prevarication biases. Future studies should continue to explore the potential moderating role using device-based methods, such as accelerometry.
CONCLUSIONS
Given the possible longer term physiological implications of chronic activation of the stress response system, this study once again highlights the pressing need for public health researchers, clinicians, and interventionists to find effective and novel approaches to reduce stress among adults. This in turn may help reduce the risk of developing cardiovascular disease in the long term.
Supplementary Material
Acknowledgments:
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I & HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). No financial disclosures have been reported by the authors of this paper.
Footnotes
Author statement
Tiwaloluwa Ajibewa: Conceptualization, Writing—original draft preparation, Writing—review and editing, Formal analysis, Visualization
Kiarri Kershaw: Writing—review and editing, Writing—original draft preparation
J. Jeffrey Carr: Writing—review and editing
James G. Terry: Writing—review and editing
Kelley Pettee Gabriel: Writing—review and editing
Mercedes Carnethon: Writing—review and editing, Writing—original draft preparation
Mandy Wong: Formal analysis, Data curation, Writing—review and editing
Norrina Allen: Writing—original draft preparation, Writing—review and editing, Formal analysis, Supervision
All authors have read and agreed to the submitted version of the manuscript
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9(6):360–370. doi: 10.1038/nrcardio.2012.45 [DOI] [PubMed] [Google Scholar]
- 2.Gallo LC, Roesch SC, Fortmann AL, et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the HCHS/SOL Sociocultural Ancillary Study. Psychosom Med. 2014;76(6):468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dimsdale JE. Psychological Stress and Cardiovascular Disease. J Am Coll Cardiol. 2008;51(13):1237–1246. doi: 10.1016/j.jacc.2007.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jennings JR, Kamarck TW, Everson-Rose SA, Kaplan GA, Manuck SB, Salonen J t. Exaggerated Blood Pressure Responses During Mental Stress Are Prospectively Related to Enhanced Carotid Atherosclerosis in Middle-Aged Finnish Men. Circulation. 2004;110(15):2198–2203. doi: 10.1161/01.CIR.0000143840.77061.E9 [DOI] [PubMed] [Google Scholar]
- 5.Seldenrijk A, Hamer M, Lahiri A, Penninx BWJH, Steptoe A. Psychological distress, cortisol stress response and subclinical coronary calcification. Psychoneuroendocrinology. 2012;37(1):48–55. doi: 10.1016/j.psyneuen.2011.05.001 [DOI] [PubMed] [Google Scholar]
- 6.Kivimäki M, Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. 2018;15(4):215–229. doi: 10.1038/nrcardio.2017.189 [DOI] [PubMed] [Google Scholar]
- 7.Rosengren A, Hawken S, Ôunpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): case-control study. The Lancet. 2004;364(9438):953–962. doi: 10.1016/S0140-6736(04)17019-0 [DOI] [PubMed] [Google Scholar]
- 8.Santosa A, Rosengren A, Ramasundarahettige C, et al. Psychosocial Risk Factors and Cardiovascular Disease and Death in a Population-Based Cohort From 21 Low-, Middle-, and High-Income Countries. JAMA Netw Open. 2021;4(12):e2138920. doi: 10.1001/jamanetworkopen.2021.38920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sothmann MS. The Cross-Stressor Adaptation Hypothesis and Exercise Training. In: Psychobiology of Physical Activity. Human Kinetics; 2006:149–160. [Google Scholar]
- 10.Gerber M, Pühse U. Review Article: Do exercise and fitness protect against stress-induced health complaints? A review of the literature. Scand J Public Health. 2009;37(8):801–819. doi: 10.1177/1403494809350522 [DOI] [PubMed] [Google Scholar]
- 11.Lambiase MJ, Barry HM, Roemmich JamesN. Effect of a Simulated Active Commute to School on Cardiovascular Stress Reactivity. Med Sci Sports Exerc. 2010;42(8):1609–1616. doi: 10.1249/MSS.0b013e3181d0c77b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roemmich JN, Lambiase M, Salvy SJ, Horvath PJ. Protective effect of interval exercise on psychophysiological stress reactivity in children. Psychophysiology. 2009;46(4):852–861. [DOI] [PubMed] [Google Scholar]
- 13.Throne LC, Bartholomew JB, Craig J, Farrar RP. Stress Reactivity in Fire Fighters: An Exercise Intervention. :12. [Google Scholar]
- 14.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. Jama. 2007;298(14):1685–1687. [DOI] [PubMed] [Google Scholar]
- 15.Strahler J, Wurst R, Fuchs R, Wunsch K. Joint associations of regular exercise and healthy diet with psychobiological stress reactivity in a healthy male sample. Stress. 2021;0(0):1–14. doi: 10.1080/10253890.2021.1878496 [DOI] [PubMed] [Google Scholar]
- 16.Bowen KS, Uchino BN, Birmingham W, Carlisle M, Smith TW, Light KC. The Stress-Buffering Effects of Functional Social Support on Ambulatory Blood Pressure. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2014;33(11):1440–1443. doi: 10.1037/hea0000005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howard S, Creaven AM, Hughes BM, O’Leary ÉD, James JE. Perceived social support predicts lower cardiovascular reactivity to stress in older adults. Biol Psychol. 2017;125:70–75. doi: 10.1016/j.biopsycho.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 18.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. [DOI] [PubMed] [Google Scholar]
- 19.Thomas SJ, Booth JN, Jaeger BC, et al. Association of Sleep Characteristics With Nocturnal Hypertension and Nondipping Blood Pressure in the CARDIA Study. J Am Heart Assoc. 2020;9(7). doi: 10.1161/JAHA.119.015062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen S, Schwartz JE, Epel E, Kirschbaum C, Sidney S, Seeman T. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med. 2006;68(1):41–50. [DOI] [PubMed] [Google Scholar]
- 21.de Baca TC, Prather AA, Lin J, et al. Chronic psychosocial and financial burden accelerates 5-year telomere shortening: Findings from the Coronary Artery Risk Development in Young Adults Study. Mol Psychiatry. 2020;25(5):1141–1153. doi: 10.1038/s41380-019-0482-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18(3):423–438. [DOI] [PubMed] [Google Scholar]
- 23.Loucks EB, Taylor SE, Polak JF, Wilhelm A, Kalra P, Matthews KA. Childhood family psychosocial environment and carotid intima media thickness: The CARDIA study. Soc Sci Med. 2014;104:15–22. doi: 10.1016/j.socscimed.2013.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobs DR, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and Reliability of Short Physical Activity History: Cardia and the Minnesota Heart Health Program. J Cardpulm Rehabil. 1989;9(11):448–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gabriel KP, Sidney S, Jacobs DR, et al. Convergent Validity of a Brief Self-reported Physical Activity Questionnaire. Med Sci Sports Exerc. 2014;46(8):1570–1577. doi: 10.1249/MSS.0000000000000278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Booth J, Connelly L, Lawrence M, et al. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC Neurol. 2015;15(1):233. doi: 10.1186/s12883-015-0456-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berntson J, Patel JS, Stewart JC. Number of recent stressful life events and incident cardiovascular disease: Moderation by lifetime depressive disorder. J Psychosom Res. 2017;99:149–154. doi: 10.1016/j.jpsychores.2017.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osborne MT, Shin LM, Mehta NN, Pitman RK, Fayad ZA, Tawakol A. Disentangling the links between psychosocial stress and cardiovascular disease. Circ Cardiovasc Imaging. 2020;13(8):e010931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. doi: 10.1016/j.physbeh.2007.04.011 [DOI] [PubMed] [Google Scholar]
- 30.Kershaw KN, Brenes GA, Charles LE, et al. Associations of Stressful Life Events and Social Strain With Incident Cardiovascular Disease in the Women’s Health Initiative. J Am Heart Assoc. 3(3):e000687. doi: 10.1161/JAHA.113.000687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kershaw KN, Droomers M, Robinson WR, Carnethon MR, Daviglus ML, Monique Verschuren WM. Quantifying the contributions of behavioral and biological risk factors to socioeconomic disparities in coronary heart disease incidence: the MORGEN study. Eur J Epidemiol. 2013;28(10):807–814. doi: 10.1007/s10654-013-9847-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schnohr P, Kristensen T s., Prescott E, Scharling H. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time—The Copenhagen City Heart Study. Scand J Med Sci Sports. 2005;15(2):107–112. doi: 10.1111/j.1600-0838.2004.00394.x [DOI] [PubMed] [Google Scholar]
- 33.Stults-Kolehmainen MA, Sinha R. The Effects of Stress on Physical Activity and Exercise. Sports Med. 2014;44(1):81–121. doi: 10.1007/s40279-013-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pilcher JJ, Bryant SA. Implications of Social Support as a Self-Control Resource. Front Behav Neurosci. 2016;10:228. doi: 10.3389/fnbeh.2016.00228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epel ES, Crosswell AD, Mayer SE, et al. More than a feeling: A unified view of stress measurement for population science. Front Neuroendocrinol. 2018;49:146–169. doi: 10.1016/j.yfrne.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.