Abstract
Background and Aims
The advent of 3D printing has revolutionized plastic surgery and prosthetic devices, providing personalized solutions for patients with traumatic injuries, deformities, and appearance‐related conditions. This review offers a comprehensive overview of 3D printing's applications, advantages, limitations, and future prospects in these fields.
Methods
A literature search was conducted in PubMed, Google Scholar, and Scopus for studies on 3D printing in plastic surgery.
Results
3D printing has significantly contributed to personalized medical interventions, with benefits like enhanced design flexibility, reduced production time, and improved patient outcomes. Using computer‐aided design (CAD) software, precise models tailored to a patient's anatomy can be created, ensuring better fit, functionality, and comfort. 3D printing allows for intricate geometries, leading to improved aesthetic outcomes and patient‐specific prosthetic limbs and orthoses. The historical development of 3D printing, key milestones, and breakthroughs are highlighted. Recent progress in bioprinting and tissue engineering shows promising applications in regenerative medicine and transplantation. The integration of AI and automation with 3D printing enhances surgical planning and outcomes. Emerging trends in patient‐specific treatment planning and precision medicine are potential game‐changers. However, challenges like technical considerations, economic implications, and ethical issues exist. Addressing these challenges and advancing research in materials, design processes, and long‐term outcomes are crucial for widespread adoption.
Conclusion
The review underscores the increasing adoption of 3D printing in healthcare and its impact on plastic surgery and prosthetic devices. It emphasizes the importance of evaluating the current state and addressing knowledge gaps through future research to foster further advancements
Keywords: 3D printing, customization, plastic surgery, prosthetic devices
1. INTRODUCTION
Plastic surgery and prosthetic devices enhance life quality for individuals with traumatic injuries, congenital deformities, or conditions affecting appearance or abilities. These interventions boost patients' well‐being, self‐esteem, and social participation. 1 A groundbreaking technology, 3D printing (additive manufacturing), has emerged in plastic surgery and prosthetic devices, offering customization, precision, and improved patient outcomes by overcoming conventional manufacturing limitations. Unlike traditional methods, 3D printing provides greater design flexibility and reduces complexity and production time for prosthetic devices. 2 , 3
Using computer‐aided design (CAD) software, surgeons and prosthetists can create precise models tailored to each patient's anatomy and needs. This customization ensures a better fit, improved functionality, and enhanced patient comfort. Moreover, 3D printing enables rapid prototype production and iterations, facilitating design refinement and optimized treatment plans efficiently.
In addition to customization, 3D printing offers increased precision with its layer‐by‐layer additive process. This allows for intricate geometries and fine details difficult to achieve with traditional methods. Consequently, 3D printing can significantly improve the aesthetic outcomes of plastic surgery, resulting in more natural‐looking results and greater patient satisfaction. For prosthetic devices, precisely replicating missing or impaired body parts enhances the patient's mobility and functionality. 1 , 4
The adoption of 3D printing in healthcare has increased due to its ability to produce patient‐specific and customizable medical devices. In plastic surgery and prosthetic devices, this technology offers precise and tailored solutions for individual patients. Using 3D scanning techniques and CAD software, accurate models can be generated and translated into physical objects using 3D printers. 3 This has led to anatomically precise implants, surgical guides, and patient‐specific prosthetics, improving surgical outcomes and patient satisfaction. 5 , 6
Numerous successful applications of 3D printing in plastic surgery (e.g., craniomaxillofacial surgery, hand and upper limb surgery, cosmetic surgery, transplant surgery) and prosthetic devices have been reported. For instance, 3D printing has been instrumental in fabricating customized craniofacial implants, enabling the reconstruction of complex defects with improved aesthetic and functional outcomes. 6 Additionally, patient‐specific prosthetic limbs and orthoses developed using 3D printing provide enhanced comfort, fit, and functionality. 5
Given the growing use of 3D printing in plastic surgery and prosthetic devices, it is essential to evaluate its current state. Understanding the scope, limitations, and challenges of 3D printing in these fields is crucial for further advancements and successful implementation. Although 3D printing has shown promising results in plastic surgery and prosthetic devices, knowledge gaps remain. This review aims to identify these gaps, highlighting areas for future research, including refining materials and techniques, optimizing design processes, and assessing long‐term outcomes and cost‐effectiveness.
2. METHODOLOGY
This comprehensive narrative review provides an in‐depth analysis of the current uses of 3D printing technology and its potential future applications in cosmetic surgery and prosthetics. The study employed a rigorous methodology to ensure a thorough search of published literature, which included observational, case‐control, cohort, case reports, and randomized controlled trials. The review encompassed all applications of 3D printing in plastic surgery and addressed both adult and pediatric populations. Only articles written in English were considered, and there was no deadline restriction.
Numerous databases, including PubMed, EMBASE, Google Scholar, and the Cochrane Library, were used in the literature search. Search terms such as “3D printing in plastic surgery,” “3D printing and prosthetics,” and “bioprinting” were used to get relevant results. To find more pertinent papers, references from recently released procedure‐specific evaluations were manually examined. Unpublished and abstracted works were not included in the review (Table 1).
Table 1.
Summary of methodology.
| Methodology Steps | Description |
|---|---|
| Literature search | PubMed, EMBASE, Google Scholar, and Cochrane Library searched for relevant 3D printing studies in plastic surgery and prosthetics. |
| Inclusion criteria | Full‐text articles written in English were considered. |
| The study design included observational studies, case‐control studies, cohort studies, case reports, and randomized controlled trials. | |
| The review encompassed all applications of 3D printing in plastic surgery and covered both adult and pediatric populations. | |
| Studies investigating outcomes such as surgical accuracy, patient satisfaction, postoperative complications, or other relevant clinical outcomes | |
| Studies summarizing the technical, economical, ethical, and legislative consideration | |
| Studies conducted on human subjects or animal models relevant to plastic surgery | |
| Exclusion criteria | Review papers, unpublished and abstracted works were excluded. |
| Studies focusing solely on other medical specialties or nonmedical applications of 3D printing. | |
| Studies lacking clear methodology or reporting insufficient data. | |
| Studies not conducted on living subjects (e.g., in vitro studies). | |
| Non‐English language studies (unless translated and published in English). | |
| Search terms | Keywords such as “3D printing in Plastic Surgery,” “3D printing and Prosthetics,” and “Bioprinting” were used for the search. |
| Additional search criteria | Supplementary sources were identified by manually examining references cited in recent reviews. |
| Sample size requirement | No specific sample size requirement. |
| Date range | 1950–2023 |
This review sought to offer a high‐quality academic evaluation of the existing uses and potential future applications of 3D printing technology in plastic surgery and prosthetics using a comprehensive and methodical methodology. This study provides insightful information that may be useful for a wide range of surgical procedures by thoroughly summarizing pertinent findings. Figure 1 gives a brief summary of the methodology of this narrative review.
Figure 1.
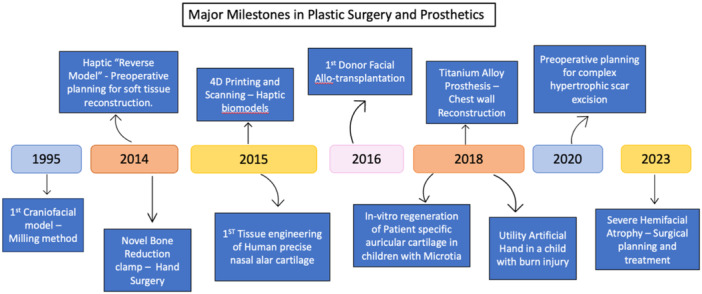
Depicting major milestones in 3D printing in Plastic Surgery and Prosthetics.
3. HISTORICAL DEVELOPMENT OF 3D PRINTING IN PLASTIC SURGERY AND PROSTHETIC DEVICES
3.1. Evolution of 3D printing technology and its adaptation in healthcare
3D printing, invented by Charles Hull in the early 1980s, was initially known as stereolithography. 2 In 1986, Hull patented stereolithography and founded 3D Systems Corporation, which developed the first 3D printer, the "stereolithography apparatus". 7 , 8 Various companies later created 3D printers for commercial and industrial uses. Initially, 3D printing served the automotive and aerospace industries for prototyping car and airplane parts, and for military gun prototyping. 7
In healthcare, 3D printing began in the late 1990s with bladders, dental implants, and custom prosthetics. 9 Its medical applications have significantly advanced since then, producing bones, ears, trachea, stem cells, blood vessels, vascular structures, and drug delivery devices. 8 Bioprinting now creates tissues, organs, customized prosthetics, implants, anatomical models, and 3D printed drugs, 10 especially for personalized dosing for patients with polymorphisms and drugs with narrow therapeutic indexes. 8
3.2. Milestones and breakthroughs in the application of 3D printing in plastic surgery and prosthetic devices
The first craniofacial model was produced in foam by milling. 11 In 2014, University of Chicago researchers designed the first 3D‐printed bone reduction clamp for hand surgery, offering multiple bone stabilization points, disassembly into smaller parts, and angled K‐wire insertion. 12 3D printing created “reverse models” for preoperative planning in soft tissue reconstruction. For a right ankle replacement patient needing soft tissue debridement, the left ankle served as a reverse model using Cubify and Magics software, guiding flap harvest with no postoperative complications. 13 In 2015, nasal alar cartilage was 3D printed using tissue‐engineering in mice, showing superior biomechanical properties compared to native cartilage. 14 4D CT scans have been used for targeted lung cancer radiotherapy, and 4D printing, adding time as the 4th dimension, provides spatiotemporal information for surgical planning, improving outcomes. 13
Facial allotransplantation, performed since 2005, saw a breakthrough in 2016 with 3D printing. Finnish researchers digitally photographed, scanned, processed, and 3D printed the donor's face, achieving superior resemblance to previous handmade grafts. 15 3D printing created sternum and rib prostheses for chest wall reconstruction post‐tumor invasion, showing superior mechanical properties. 16 CT scanning and 3D printing cultured autologous chondrocytes for microtia reconstruction in children, showing improved elasticity after 2 years. 17
A 3D‐printed artificial hand was created for a child with a left‐hand burn, improving cosmesis and some hand functions, aiding daily activities. 18 3D models assisted surgical planning for hypertrophic scar excision, reducing operative times and bleeding. 19 For severe hemifacial atrophy, 3D planning and printing guided surgery using rib cartilage grafts and adipo‐fascial flaps, with 42% needing secondary revision and significant postoperative volume improvement. 20 Figure 1 presents an overview of 3D printing milestones in plastic surgery and prosthetics.
4. ADVANTAGES OF 3D PRINTING IN PLASTIC SURGERY AND PROSTHETIC DEVICES
In recent years, 3D printing technology has significantly advanced the field of plastic and reconstructive surgery, addressing challenges faced by traditional methods. Key areas that have seen remarkable progress include preoperative planning, prosthetics and orthotics, and surgical guides and instruments. A summary of the advantages of 3D printing in plastic surgery is summarized in Figure 2.
Figure 2.
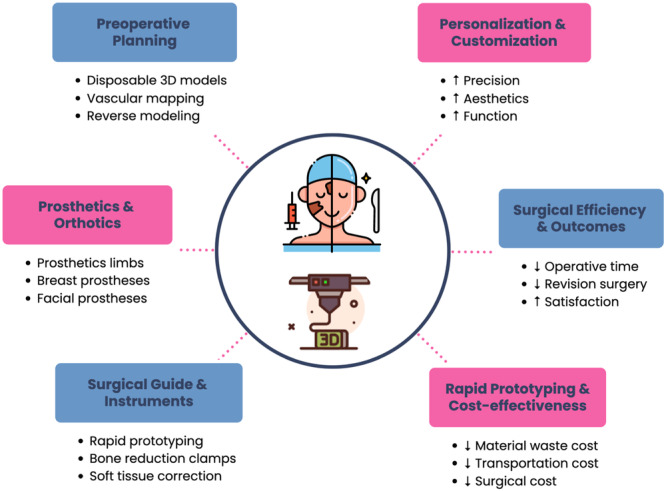
Applications and benefits of 3D printing in Plastic Surgery and Prosthetic Devices.
4.1. Cranio‐maxillofacial surgery
D'Urso et al. used stereolithography to create customized acrylic implants for 30 patients with large craniotomy defects. All implants fit well, except one needing 1 cm of burring and five needing minor trimming. Surgeons reported a 41% reduction in operating time compared to open cold cure molding. Patients were highly satisfied with the results. 21 Tepper et al. used 3D models for two cases: a comminuted mandibular fracture and a panfacial injury. They used virtual 3D models and 3D‐printed guides for preoperative planning and intraoperative guidance, finding them effective despite some disadvantages. 22
4.2. Hand and upper limb surgery
Simulations have become an alternative to traditional learning due to trainee work hour regulations24. Lazarus et al. compared a 3D‐printed procedural simulator to cadaveric surgery, finding cadaveric surgery better but the 3D model superior in fracture reproduction. 23 Michielsen et al. used 3D printing for preoperative planning and customized cutting guides in cases of fracture non‐union and mal‐union, beneficial for managing scaphoid and pediatric fractures. 24 Yang et al. did a randomized study on 40 patients with elbow fractures. 25 Operative time (p = 0.023), intraoperative blood loss (p = 0.018), and the Mayo elbow performance score (p = 0.001) were significantly lower when 3D models were used. They found that 83.1% of patients treated using 3D technology had good or excellent elbow function, compared to 71.4% in patients treated conventionally. The surgeons also reported a better preoperative assessment of the fracture. Patients and their families reported better preoperative communication when 3D models were used to explain the medical condition. 3D models helped in preoperative evaluation, planning, and intraoperative navigation. Polylactic acid (PLA) was a better material than acrylonitrile butadiene styrene (ABS), as curly edges were found only in 1 model compared to 4 in ABS. PLA models were not deformed after high‐pressure steam sterilization, whereas ABS models were deformed. 25
4.3. Cosmetic surgery
Suszynski et al. used 3D‐printed models for rhinoplasty, finding them helpful for tip projection, rotation, and dorsal reduction. 26 They used colored gypsum powder for printing, which made the models quite realistic and gave 3D anatomical, visual, and tactile information. The models took less than a week to be printed. The cost of the models was $300 and was either deducted from the surgeon's fee or paid by the patient. In the author's case, most patients were willing to pay for the models. They found it to be helpful in the following steps: tip projection, tip rotation, and assessing dorsal reduction. 26 These models were also used for counseling patients. Guevara et al. used a 3D‐printed guide for rhinoplasty, aiding in dorsum reduction, tip alteration, and asymmetry correction. Each guide cost around $5. 27
4.4. Burn and reconstruction
Burn victims often need advanced skin scaffolds and dressing materials to expedite wound healing and promote tissue regeneration. 28 3D printing advances burn treatment with skin scaffolds and dressing materials made from natural biomaterials, like nanocellulose and gelatin‐alginate combinations. 29 , 30 This process, known as bioprinting, results in a final 3D skin structure.
One remarkable advantage of bioprinted skin grafts is that they retain moisture for up to 7 days, accelerating healing and reducing pain. 29 Kang et al. enhanced bioprinting with fibroblast and myoblast cell lines, improving structural integrity. 31 Bioprinted skin grafts facilitate cell migration, tissue ingrowth, and blood vessel restoration. 32 Diatomite‐based dressings have antimicrobial properties against pseudomonas infections, validated both in vitro and in vivo. 33 , 34 , 35 , 36
4.5. Prosthetics
3D printing has revolutionized prosthetics. Park et al. used 3D‐printed scapular prostheses for chondrosarcoma recovery, showing tailor‐made advantages. 37 Integrating 3D models with CAD enabled comprehensive shoulder reconstruction. 38 Stereophotogrammetry personalized nasal prostheses, using 3D coordinates from 2D pixels. 38 CT scan data and silicone were used for crafting prosthetic fingers40. Electron beam additive manufacturing produced custom titanium implants for orbital reconstruction, maintaining precise shape. 39 Azuma et al. improved mandibular reconstruction with pre‐planned 3D‐printed plates, enhancing facial symmetry. 40
4.6. Importance of 3D simulation technology in customized surgery
-
1.
Enhanced Surgical Planning: 3D simulation allows detailed visualization of anatomical structures, aiding in personalized surgical strategies and anticipating challenges. 41
-
2.
Improved Patient Outcomes: Simulating interventions on 3D models refines techniques, reduces complications, and enhances postoperative outcomes. 42
-
3.
Education and Training: 3D simulation serves as an educational tool, allowing trainees to practice complex procedures in a risk‐free environment. 43
-
4.
Customized Implants and Prosthetics: 3D simulation helps design implants and prosthetics tailored to each patient's anatomy, ensuring better fit and functionality. 44
-
5.
Cost‐Effectiveness: Although initially costly, 3D simulation can lead to savings by minimizing revisions, reducing complications, and optimizing resource use. 45
5. LIMITATIONS AND CHALLENGES OF 3D PRINTING IN PLASTIC SURGERY AND PROSTHETIC DEVICES
Although 3D printing has revolutionized the field of plastic surgery and prosthetics manufacturing, limitation and challenges should be acknowledged as well (Figure 3).
Figure 3.
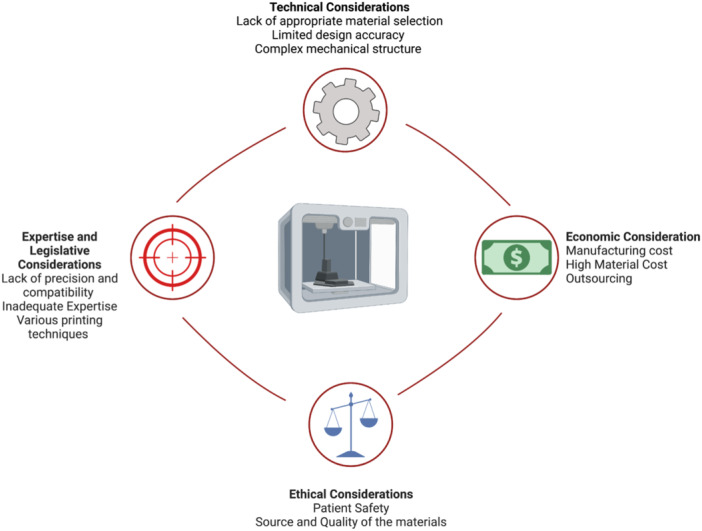
Limitations and Challenges of 3D Printing in Plastic Surgery and Prosthetic Devices.
5.1. Technical considerations
The lack of randomized studies proving 3D printing's superiority over conventional techniques is concerning. 24 Selecting appropriate materials for membranes and module components is a major challenge. 46 Despite efforts to match 3D implants with human organs, it's impossible to perfectly emulate texture, color, and structure. 47 Bio‐printed skin lacks critical appendages like hair follicles, sweat glands, and sebaceous glands, though research is ongoing to address this. 48 Natural biomaterials, while available, often lack the bioelasticity of native skin. Large quantities of cells with specific biochemical properties are also needed. 48 Ongoing research promises to address these limitations, making it a transformative technology for burn victims.
In 3D printing, binders are essential. Photopolymers are suitable for bone tissue using SLA, but organic binders, though more biocompatible, can affect the printing machines. 49 The mechanical quality of printing material impacts the final product. Achieving optimal scaffold tissue to match the tensile strength and flexibility of biological tissues is challenging. 50
Only one randomized study by Yang et al. was found on patients with elbow fractures. 25 The time for applying this technique varies. D'Urso et al. reported 1 month 21 while Guevara et al. reported 1 h. 27 Tepper et al. found no delay in patient care during trauma assessment and virtual 3D surgery planning. 22 his depends on the surgery type and model being printed. D'Urso et al. printed a whole skull model, while Guevara et al. printed a guide from the brows to the upper lip. 21 , 27 CAD‐based implants offered better volume and globe positioning but required longer production times (7–10 days vs. 2–5 days) and higher costs ($3500 vs. $300). 51 This highlights the challenge of balancing 3D printing's benefits with time and financial considerations.
Accurate sizing is crucial for prosthetics and engineered organs. However, design accuracy is limited by material availability matching the nozzle size, flow rate, and 3D printing speed. Material shrinkage during curing and cooling can alter the structure, further limiting usage.
5.2. Printing technologies in 3D printing for plastic surgery and prosthetic devices
Selecting the right printing technology is crucial for 3D printing in plastic surgery and prosthetics. Technologies like SLA, SLS, and FDM each have advantages and limitations that affect printed product quality. 52
SLA uses a photopolymer resin cured by a laser, offering high precision and surface quality for intricate models and surgical guides. 6 SLS uses a laser to sinter powdered materials, providing strength and durability, ideal for functional prototypes and prosthetic components. 53 FDM extrudes thermoplastic filaments layer by layer, offering cost‐effectiveness and ease of use but with lower surface quality. 52
Selecting the appropriate technology depends on specific needs, such as resolution, material properties, and budget, to ensure optimal outcomes in plastic surgery and prosthetics.
5.3. Economic considerations
3D printing's financial implications are significant due to limited material choices. Costs vary: D'Urso et al. reported $1300, Yang et al. $2, 3, and Guevara et al. $5. 2 , 25 , 27 Costs depend on time, whether printing is done in‐house or outsourced. Lazarus et al. found 3D‐printed simulators can be more cost‐efficient than cadaveric labs. 23 CT data manipulation and accuracy assessment were problems seen by D'Urso et al. 21 Advancements in software and equipment might improve this
Many materials are available, but not all are suitable for printing organs and tissues, leading to demand‐supply imbalance and increased material costs. Manufacturing costs depend on the production facility. 54 Cheap desktop 3D printers allow cheap models and guides but lack quality approvals compared to commercial manufacturers required to meet high standards. Design preparation costs vary based on software, technology, and design time. 55
Creating implant devices is more complex than anatomical models used as surgical guides. This complexity is particularly pronounced for hospitals attempting to manufacture customized implants internally, requiring the necessary equipment and technological know‐how. Hospitals often outsource 3D printing to external companies using expensive, sophisticated procedures that are challenging to fund with limited resources. 1 Outsourcing also poses economic challenges, as hospitals must meet regulatory standards on design and quality, making 3D printing less economical. 56
5.4. Expertise and legislative considerations
Embracing 3D printing in surgery is exciting but complex, requiring thorough understanding of mechanics, uses, and printing technologies. Surgeons need comprehensive instruction, including software competency, printing procedures, material selection, sterilization, cost considerations, and time consumption. 57 Surgical training is crucial, as lack of understanding can result in inferior precision. 58 Institutions now offer courses to educate surgeons and operating room workers in 3D printing. 59 , 60 , 61 However, training challenges remain due to resource scarcity, costs, and a lack of standardized curriculum. The field's rapid evolution makes it difficult for practitioners to stay updated. 62
Collaboration between surgeons, engineers, and 3D printing professionals fosters creativity and customized solutions, improving patient outcomes. 63 This collaboration is critical for progress in the field but requires careful management to address communication, time, and regulatory compliance.
3D printing in surgery presents risks of misuse and malpractice. A strong monitoring and regulatory framework is needed for using 3D‐printed objects and technologies in surgeries. The FDA currently oversees this sector. While the FDA distinguishes between over‐the‐counter and point‐of‐care devices, the latter poses compliance issues. 64 , 65 3D printing can reduce dependency on major surgical supply chains but raises legal issues for hospitals and doctors. Hospitals distributing preprinted products may be considered manufacturers under the law.
Patients must receive thorough preoperative education to understand novel implants. 66 There is an urgent need for coordinated efforts to reform the legal framework governing medical 3D printing, strengthening legal safeguards for surgeons and patient safety. Intellectual property protection is critical, including preserving unique designs essential to 3D printing. 67
Regulatory issues are crucial and need urgent attention. Bodies like the FDA and EMA ensure safety and efficacy of medical devices, including 3D‐printed implants. 68 Rapidly evolving technologies challenge regulatory frameworks, leading to inconsistency in requirements. Customization of 3D‐printed implants introduces regulatory complexities due to lack of standardization.
5.5. Ethical considerations
Obtaining informed consent for 3D‐printed interventions protects patient liberty and promotes trust. Patients must be educated on technology objectives, hazards, and benefits. 69 , 70 Patient autonomy allows active healthcare decision participation, including personalized 3D‐printed solutions. Overcoming geographical, financial, and institutional barriers is crucial for access to 3D printing. Regional centers, specialized training, and innovative finance structures democratize access, fostering innovation and patient care.
While 3D printing can reduce costs long‐term, 71 initial expenditure poses difficulties, especially in developing nations. Costs vary due to onsite and offsite factors, complicating standardization. 72 Collaborative funding, strategic collaborations, government subsidies, and open‐source platforms can improve healthcare affordability. Ethical responsibilities include ensuring the safety and quality of 3D‐printed procedures, adhering to protocols, thorough testing, and ongoing monitoring. Conducting extensive risk‐benefit analyses prioritizes patient safety.
5.6. Navigating public perception in 3D printing integration in healthcare
3D printing's potential to revolutionize healthcare is undeniable, but its integration faces excitement and skepticism. Currently, technology is concentrated in advanced research centers in developed countries like the US and China, limiting widespread use and understanding of public perception. 73 Despite potential, reports suggest some patients prefer traditional prosthetics over 3D‐printed ones due to durability and reliability concerns. 74
Misconceptions about 3D printing, such as producing only small parts or being a universal solution, need addressing. It's a tool in the healthcare arsenal, requiring careful implementation, including ethical considerations related to risk factors, clinical trials, and regulatory framework. 75
Successful integration depends on navigating public perception, societal acceptance, and ethical considerations to ensure safe, effective use of technology for patient care and innovation.
In 3D bioprinting, understanding religious perspectives is crucial. Religious beliefs influence acceptance of bioprinting, with ethical or moral concerns regarding 3D bioprinted organs. Addressing concerns through dialogue with religious leaders aids technology implementation. A culturally sensitive approach improves patient satisfaction and treatment outcomes when religious concerns are addressed by healthcare providers.
6. FUTURE DIRECTIONS AND EMERGING TRENDS IN 3D PRINTING FOR PLASTIC SURGERY
6.1. Bioprinting and tissue engineering
Recent strides in tissue engineering and bioprinting have transformed plastic surgery possibilities. Miller et al. pioneered a bioprinting process capable of creating precise, multicellular structures, promising significant advancements in regenerative medicine and organ transplantation. 76 This innovation opens avenues for rejuvenation and reconstruction treatments, including skin, cartilage, and bone grafts.
Plastic surgery has evolved with 3D printing integration, empowering surgeons in preoperative planning and custom tool creation. 13 , 77 Surgical guides aid complex procedures like mandibular angle ostectomy and hand surgery bone reduction, augmenting outcomes. 12 , 78
6.2. Integration with artificial intelligence and automation
In plastic surgery, the fusion of 3D printing, AI, and automation marks a captivating advance. AI algorithms enhance surgical planning and optimization, as evidenced in mandibular condylar neck fracture management. 79 Integrating 3D printing and AI improves surgical precision and outcomes, as demonstrated in fracture reduction cases. 76
6.3. Patient‐specific treatment planning and precision medicine
Automating manufacturing processes in 3D printing reduces errors and enhances effectiveness. Johnson et al. explored robotic automation in tissue engineering, improving printing speed, precision, and reproducibility of anatomical structures. 80 Automated fabrication expedites patient care and streamlines plastic surgery workflows.
7. CURRENT KNOWLEDGE GAPS AND POTENTIALS FOR FUTURE STUDIES
Although 3D printing shows promise in plastic surgery, further research is needed to address knowledge gaps. Identifying suitable raw materials is challenging due to limited data on their biocompatibility and long‐term effects. Economic analyses comparing 3D printing costs with traditional methods are also understudied and necessary for policymakers to understand its economic implications. Current data on 3D printing is mostly from small case series, requiring validation in larger cohorts to ensure efficacy and safety. Longitudinal studies on patient outcomes and postoperative complications are important before routine clinical implementation. Additionally, standardized regulatory frameworks for secondary care hospitals need more research to provide clear guidelines on material quality and manufacturing processes. Further research in these areas will significantly advance 3D printing in plastic surgery. Plastic surgery can improve through regenerative medicine, bioprinting, and tissue engineering. Integrating AI and automation enhances surgical planning and fabrication, while precision medicine and patient‐specific treatments improve outcomes.
8. STUDY LIMITATIONS
This review has limitations, including a potentially narrow scope due to rapidly evolving technology and the selection bias of only including English articles. The lack of formal quantitative analysis may impact objectivity, and the results may not be generalizable across different populations or healthcare settings.
9. CONCLUSION
This review comprehensively covers 3D printing applications, benefits, limitations, and future directions in plastic surgery and prosthetic devices. It highlights 3D printing's role in preoperative planning, improving surgical precision and outcomes, and its transformative impact on prosthetics. The review also addresses economic, ethical, and technical challenges, providing valuable insights for healthcare stakeholders. By summarizing advancements and identifying research gaps, this review supports the advancement of 3D printing in plastic surgery, guiding researchers, practitioners, and policymakers towards enhancing patient care and quality of life.
AUTHOR CONTRIBUTIONS
Muhammad Jawad Zahid: Conceptualization; writing—review and editing; supervision; validation; writing—original draft; methodology; data curation. Parit Mavani: Conceptualization; validation; writing—review and editing; supervision; writing—original draft; methodology; data curation. Wireko Andrew Awuah: Writing—review and editing; writing—original draft; data curation; visualization. Mohammad Alabdulrahman: Writing—original draft; writing—review and editing; visualization; data curation. Rachana Punukollu: Writing—original draft; writing—review and editing; visualization; data curation. Arnab Kundu: Writing—original draft; writing—review and editing; visualization; data curation. Arpit Mago: Writing—original draft; writing—review and editing; visualization; data curation. Karam Maher: Writing—original draft; writing—review and editing; visualization; data curation. Favour Tope Adebusoye: Writing—original draft; writing—review and editing; visualization; supervision; data curation. Tehreem Naseer Khan: Writing—original draft; writing—review and editing; visualization; data curation.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Favour Tope Adebusoye affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Zahid MJ, Mavani P, Awuah WA, et al. Sculpting the future: a narrative review of 3D printing in plastic surgery and prosthetic devices. Health Sci Rep. 2024;7:e2205. 10.1002/hsr2.2205
Muhammad Jawad Zahid and Parit Mavani have contributed equally to this project
DATA AVAILABILITY STATEMENT
No additional data is available. All authors have read and approved the final version of the manuscript. Favour Tope Adebusoye had full access to all of the information presented in this study and takes complete responsibility for the integrity and accuracy of the content.
REFERENCES
- 1. Chae MP, Rozen WM, McMenamin PG, Findlay MW, Spychal RT, Hunter‐Smith DJ. Emerging applications of bedside 3D printing in plastic surgery. Front Surg. 2015;2:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schubert C, Van Langeveld MC, Donoso LA. Innovations in 3D printing: a 3D overview from optics to organs. Br J Ophthalmol. 2014;98:159‐161. [DOI] [PubMed] [Google Scholar]
- 3. Yang P, Ju Y, Hu Y, Xie X, Fang B, Lei L. Emerging 3D bioprinting applications in plastic surgery. Biomater Res. 2023;27:1‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dodziuk H. Applications of 3D printing in healthcare. Pol J Cardio‐Thorac Surg. 2016;3:283‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hecker A, Tax L, Giese B, et al. Clinical applications of three‐dimensional printing in upper extremity surgery: a systematic review. J Pers Med. 2023;13:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang Z, Han W, Kim BS, et al. Three‐dimensional printing technologies in craniofacial plastic surgery: an institutional experience. J Craniofac Surg. 2023;34:820‐825. [DOI] [PubMed] [Google Scholar]
- 7. Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem. 2014;86:3240‐3253. [DOI] [PubMed] [Google Scholar]
- 8. Ventola CL. Medical applications for 3D printing: current and projected uses. P T: J Formul Manag. 2014;39:704‐711. [PMC free article] [PubMed] [Google Scholar]
- 9. Dey M, Ozbolat IT. 3D bioprinting of cells, tissues and organs. Sci Rep. 2020;10:14023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ursan ID, Chiu L, Pierce A. Three‐dimensional drug printing: a structured review. J Am Pharm Assoc. 2013;53:136‐144. [DOI] [PubMed] [Google Scholar]
- 11. Brix F, Lambrecht JT. [Preparation of individual skull models based on computed tomographic information]. Fortschr Kiefer Gesichtschir. 1987;32:74‐77. [PubMed] [Google Scholar]
- 12. Fuller SM, Butz DR, Vevang CB, Makhlouf MV. Application of 3‐dimensional printing in hand surgery for production of a novel bone reduction clamp. J Hand Surg [Am]. 2014;39:1840‐1845. [DOI] [PubMed] [Google Scholar]
- 13. Chae M, Hunter‐Smith D, De‐Silva I, Tham S, Spychal R, Rozen W. Four‐dimensional (4D) printing: a new evolution in computed tomography‐guided stereolithographic modeling. Principles and application. J Reconstr Microsurg. 2015;31:458‐463. [DOI] [PubMed] [Google Scholar]
- 14. Shen C, Yao CA, Magee W, Chai G, Zhang Y. Presurgical nasoalveolar molding for cleft lip and palate: the application of digitally designed molds. Plast Reconstr Surg. 2015;135:1007e‐1015e. [DOI] [PubMed] [Google Scholar]
- 15. Mäkitie AA, Salmi M, Lindford A, Tuomi J, Lassus P. Three‐dimensional printing for restoration of the donor face: a new digital technique tested and used in the first facial allotransplantation patient in Finland. J Plast Reconstr Aesthet Surg. 2016;69:1648‐1652. [DOI] [PubMed] [Google Scholar]
- 16. Wen X, Gao S, Feng J, Li S, Gao R, Zhang G. Chest‐wall reconstruction with a customized titanium‐alloy prosthesis fabricated by 3D printing and rapid prototyping. J Cardiothorac Surg. 2018;13(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhou G, Jiang H, Yin Z, et al. In vitro regeneration of patient‐specific ear‐shaped cartilage and its first clinical application for auricular reconstruction. EBioMedicine. 2018;28:287‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Luo H, Xie WG, Zhang W, et al. [Design and manufacture of a utility artificial hand for a burned child by three‐dimensional printing technology and its application]. Zhonghua shao shang za zhi = Zhonghua shaoshang zazhi = Chin J Burns. 2018;34:526‐528. [DOI] [PubMed] [Google Scholar]
- 19. Liu P, Hu Z, Huang S, et al. Application of 3D printed models of complex hypertrophic scars for preoperative evaluation and surgical planning. Front Bioeng Biotechnol. 2020;8:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. He L, Liu X, Khatter NJ, et al Treatment of progressive hemifacial atrophy by cartilage graft and free adipofascial flap combined with 3D planning and printing. Plast Reconstr Surg. 2020;153(3):679‐688. [DOI] [PubMed] [Google Scholar]
- 21. D'Urso PS, Effeney DJ, Earwaker WJ, et al. Custom cranioplasty using stereolithography and acrylic. Br J Plast Surg. 2000;53:200‐204. [DOI] [PubMed] [Google Scholar]
- 22. Tepper OM, Sorice S, Hershman GN, Saadeh P, Levine JP, Hirsch D. Use of virtual 3‐dimensional surgery in post‐traumatic craniomaxillofacial reconstruction. J Oral Maxillofac Surg. 2011;69:733‐741. [DOI] [PubMed] [Google Scholar]
- 23. Lazarus P, Pire E, Sapa C, et al. Design and evaluation of a new synthetic wrist procedural simulator (Wristsim®) for training of distal radius fracture fixation by volar plating. Hand Surg Rehabil. 2017;36:275‐280. [DOI] [PubMed] [Google Scholar]
- 24. Michielsen M, Van Haver A, Vanhees M, van Riet R, Verstreken F. Use of three‐dimensional technology for complications of upper limb fracture treatment. EFORT Open Rev. 2019;4:302‐312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yang L, Grottkau B, He Z, Ye C. Three dimensional printing technology and materials for treatment of elbow fractures. Int Orthop. 2017;41:2381‐2387. [DOI] [PubMed] [Google Scholar]
- 26. Suszynski TM, Serra JM, Weissler JM, Amirlak B. Three‐dimensional printing in rhinoplasty. Plast Reconstr Surg. 2018;141:1383‐1385. [DOI] [PubMed] [Google Scholar]
- 27. Guevara C, Matouk M. In‐office 3D printed guide for rhinoplasty. Int J Oral Maxillofac Surg. 2021;50:1563‐1565. [DOI] [PubMed] [Google Scholar]
- 28. Chouhan D, Dey N, Bhardwaj N, Mandal BB. Emerging and innovative approaches for wound healing and skin regeneration: current status and advances. Biomaterials. 2019;216:119267. [DOI] [PubMed] [Google Scholar]
- 29. Fayyazbakhsh F, J. Khayat M, C. Leu M. 3D‐printed gelatin‐alginate hydrogel dressings for burn wound healing: a comprehensive study. Int J Bioprint. 2022;8:618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. He P, Zhao J, Zhang J, et al. Bioprinting of skin constructs for wound healing. Burns Trauma. 2018;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kang HW, Lee SJ, Ko IK, Kengla C, Yoo JJ, Atala A. A 3D bioprinting system to produce human‐scale tissue constructs with structural integrity. Nature Biotechnol. 2016;34:312‐319. [DOI] [PubMed] [Google Scholar]
- 32. Mori N, Morimoto Y, Takeuchi S. Skin integrated with perfusable vascular channels on a chip. Biomaterials. 2017;116:48‐56. [DOI] [PubMed] [Google Scholar]
- 33. Ma J, Wu J, Zhang H, et al 3D printing of diatomite incorporated composite scaffolds for skin repair of deep burn wounds. Int J Bioprint. 2022;8(3):580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Binder KW, Zhao W, Aboushwareb T, Dice D, Atala A, Yoo JJ. In situ bioprinting of the skin for burns. J Am Coll Surg. 2010;211:S76. [Google Scholar]
- 35. Jang KS, Park SJ, Choi JJ, et al. Therapeutic efficacy of artificial skin produced by 3D bioprinting. Materials. 2021;14:5177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Michael S, Sorg H, Peck CT, et al. Tissue engineered skin substitutes created by laser‐assisted bioprinting form skin‐like structures in the dorsal skin fold chamber in mice. PLoS One. 2013;8:e57741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Park JH, Jung HW, Jang WY. The usefulness of a three‐dimensional printed segmental scapula prosthesis for recovering shoulder function in a patient with scapula chondrosarcoma: a case report. Medicine. 2021;100:e24817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zou Y, Yang Y, Han Q, et al. Novel exploration of customized 3D printed shoulder prosthesis in revision of total shoulder arthroplasty: a case report. Medicine. 2018;97:e13282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cabibihan JJ. Patient‐specific prosthetic fingers by remote collaboration–a case study. PLoS One. 2011;6:e19508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Azuma M, Yanagawa T, Ishibashi–Kanno N, et al. Mandibular reconstruction using plates prebent to fit rapid prototyping 3‐dimensional printing models ameliorates contour deformity. Head Face Med. 2014;10(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Michaels R, Witsberger CA, Powell AR, et al. 3D printing in surgical simulation: emphasized importance in the COVID‐19 pandemic era. J 3D Print Med. 2021;5:5‐9. 10.2217/3dp-2021-0009 [DOI] [Google Scholar]
- 42. Tsoulfas G, Bangeas PI, Suri J, eds . 3D Printing: application in Medical Surgery E‐Book. Els Health Sci. 2020;1:1‐6. [Google Scholar]
- 43. Porpiglia F, Verri P, Checcucci E, Amparore D, Fiori C. Role of 3D technology in simulationIn: Biyani CS, Van Cleynenbreugel B, Mottrie A, eds. Practical Simulation in Urology. Springer International Publishing; 2022:445‐464. eds,. 10.1007/978-3-030-88789-6_26 [DOI] [Google Scholar]
- 44. Choo A, Richard MJ. The role of 3D custom implants in upper extremity surgery. J Orthop Trauma. 2024;38(4S):S30‐S36. 10.1097/BOT.0000000000002760 [DOI] [PubMed] [Google Scholar]
- 45. Aimar A, Palermo A, Innocenti B. The role of 3D printing in medical applications: a state of the art. J Healthc Eng. 2019;2019:5340616. 10.1155/2019/5340616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lee JY, Tan WS, An J, et al. The potential to enhance membrane module design with 3D printing technology. J Membr Sci. 2016;499:480‐490. [Google Scholar]
- 47. Shahrubudin N, Koshy P, Alipal J, Kadir MHA, Lee TC. Challenges of 3D printing technology for manufacturing biomedical products: a case study of Malaysian manufacturing firms. Heliyon. 2020;6:e03734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhang K, Bai X, Yuan Z, et al. Cellular nanofiber structure with secretory activity‐promoting characteristics for multicellular spheroid formation and hair follicle regeneration. ACS Appl Mater Interfaces. 2020;12:7931‐7941. [DOI] [PubMed] [Google Scholar]
- 49. Bose S, Vahabzadeh S, Bandyopadhyay A. Bone tissue engineering using 3D printing. Mater Today. 2013;16:496‐504. [Google Scholar]
- 50. Egan P, Ferguson SJ, Shea K. Design and 3D printing of hierarchical tissue engineering scaffolds based on mechanics and biology perspectives. In: International design engineering technical conferences and computers and information in engineering conference. Vol 50190. American Society of Mechanical Engineers; 2016:V007T06A002. [Google Scholar]
- 51. Zimmerer RM, Ellis E, Aniceto GS, et al. A prospective multicenter study to compare the precision of posttraumatic internal orbital reconstruction with standard preformed and individualized orbital implants. J Craniomaxillofac Surg. 2016;44:1485‐1497. [DOI] [PubMed] [Google Scholar]
- 52. Claudia Y, Zopf DA, Ozkan M, Francia RD, Hu W. Current use of 3D printing in plastic surgery. Ann 3D Print Med. 2023;11:100119. 10.1016/j.stlm.2023.100119 [DOI] [Google Scholar]
- 53. Colasante C, Sanford Z, Garfein E, Tepper O. Current trends in 3D printing, bioprosthetics, and tissue engineering in plastic and reconstructive surgery. Curr Surg Rep. 2016;4(2):6. 10.1007/s40137-016-0127-4 [DOI] [Google Scholar]
- 54. Malik HH, Darwood ARJ, Shaunak S, et al. Three‐dimensional printing in surgery: a review of current surgical applications. J Surg Res. 2015;199:512‐522. [DOI] [PubMed] [Google Scholar]
- 55. Tack P, Victor J, Gemmel P, Annemans L. 3D‐printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Morrison RJ, Kashlan KN, Flanangan CL, et al. Regulatory considerations in the design and manufacturing of implantable 3D‐printed medical devices. Clin Transl Sci. 2015;8:594‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hoang D, Perrault D, Stevanovic M, et al Surgical applications of three‐dimensional printing: a review of the current literature & how to get started. Ann Transl Med. 2016;4(23):456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Martelli N, Serrano C, van den Brink H, et al. Advantages and disadvantages of 3‐dimensional printing in surgery: a systematic review. Surgery. 2016;159:1485‐1500. [DOI] [PubMed] [Google Scholar]
- 59. Frontiers . 3D printing for surgical simulation and training: Innovative materials and approaches. Accessed 2023 Oct 5 https://www.frontiersin.org/research-topics/25107/3d-printing-for-surgical-simulation-and-training-innovative-materials-and-approaches
- 60. Duke Surgery . 3D printing lab. https://surgery.duke.edu/education-and-training/training-sites-and-laboratories/3d-printing-labAccessed 2023 Oct 5 Accessed 2023 Oct 5.
- 61. Stratasys . 3D printing for surgical training. Accessed 2023 Oct 5 https://www.stratasys.com/en/resources/case-studies/fusetec/
- 62. Javaid M, Haleem A, Singh RP, Suman R. 3D printing applications for healthcare research and development. Glob Health J. 2022;6(4):217‐226. [Google Scholar]
- 63. Giannopoulos AA, Steigner ML, George E, et al. Cardiothoracic applications of 3‐dimensional printing. J Thorac Imaging. 2016;31:253‐272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Knoedler L, Knoedler S, Kauke‐Navarro M, et al. Three‐dimensional medical printing and associated legal issues in plastic surgery: a scoping review. Plast Reconstr Surg Glob Open. 2023;11:e4965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Knight R. Additive manufacturing of medical devices: maintaining innovation, protecting patients and avoiding regulatory duplication. Fed Cts L Rev. 2015;9:125. [Google Scholar]
- 66. Park MH. For a new heart, just click print: the effect on medical and products liability from 3‐D printed organs. U Ill JL Tech Pol'y. 2015;187. [Google Scholar]
- 67. Ballardini RM, Mimler M, Minssen T, Salmi M. 3D printing, intellectual property rights and medical emergencies: in search of new flexibilities. IIC Int Rev Ind Prop Copyr Law. 2022;53:1149‐1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. US Food and drug administration and center for devices and radiological health additive manufacturing working group, “3D printing medical devices at point of care”. American Society of Mechanical Engineers; 2020. https://www.fda.gov/medical-devices/3d-printing-medical-devices/3d-printing-medical-devices-point-care-discussion-paper [Google Scholar]
- 69. Capron A (Almost) everything you ever wanted to know about informed consent Review of: Faden, RR and Beauchamp, TL. A history and theory of informed consentMed Humanit Rev1. Oxford University Press; 1986:78‐82. [PubMed] [Google Scholar]
- 70. Caulfield T, Murdoch B. Genes, cells, and biobanks: yes, there's still a consent problem. PLoS Biol. 2017;15:e2002654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Serrano C, Fontenay S, van den Brink H, Pineau J, Prognon P, Martelli N. Evaluation of 3D printing costs in surgery: a systematic review. Int J Technol Assess Health Care. 2020;36:349‐355. [DOI] [PubMed] [Google Scholar]
- 72. Yang H, Chung JKH, Chen Y, Li Y. The cost calculation method of construction 3D printing aligned with Internet of things. EURASIP J Wirel Commun Netw. 2018;2018:1‐9. [Google Scholar]
- 73. Ding Z, Tang N, Huang J, Cao X, Wu S. Global hotspots and emerging trends in 3D bioprinting research. Front Bioeng Biotechnol. 2023;11:1169893. 10.3389/fbioe.2023.1169893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Copeland C, Reyes CC, Peck JL, Srivastava R, Zuniga JM. Functional performance and patient satisfaction comparison between a 3D printed and a standard transradial prosthesis: a case report. Biomed Eng Online. 2022;21(1):7. 10.1186/s12938-022-00977-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Gilbert F, O'Connell CD, Mladenovska T, Dodds S. Print me an organ? Ethical and regulatory issues emerging from 3D bioprinting in medicine. Sci Eng Ethics. 2018;24(1):73‐91. 10.1007/s11948-017-9874-6 [DOI] [PubMed] [Google Scholar]
- 76. Miller JS, Stevens KR, Yang MT, et al. Rapid casting of patterned vascular networks for perfusable engineered three‐dimensional tissues. Nat Mater. 2012;11:768‐774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tan H, Yang K, Wei P, et al. A novel preoperative planning technique using a combination of CT angiography and three‐dimensional printing for complex toe‐to‐hand reconstruction. J Reconstr Microsurg. 2015;31:369‐377. [DOI] [PubMed] [Google Scholar]
- 78. Ye N, Long H, Zhu S, Yang Y, Lai W, Hu J. The accuracy of computer image‐guided template for mandibular angle ostectomy. Aesthetic Plast Surg. 2015;39:117‐123. [DOI] [PubMed] [Google Scholar]
- 79. Ying K, Wang L, Zhu YW, Li QQ, Mao B. Clinical application of virtual surgery combined with guide plate in reduction and fixation of condylar neck fracture in 7 patients. Shanghai J Stomatol. 2023;32(1):105. [PubMed] [Google Scholar]
- 80. Johnson BN, Lancaster KZ, Zhen G, et al. 3D printed anatomical nerve regeneration pathways. Adv Funct Mater. 2015;25:6205‐6217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data is available. All authors have read and approved the final version of the manuscript. Favour Tope Adebusoye had full access to all of the information presented in this study and takes complete responsibility for the integrity and accuracy of the content.


