The last decade has been marked by reduction in incidence rates of ST-elevation myocardial infarction (STEMI) and increase in non-ST-elevation myocardial infarction (NSTEMI) in the United States.(1) These changes have been attributed not only to standardized STEMI protocols designed to optimize care, but also to demographic changes – less smoking, more statins prescribed in seniors, low dose aspirin use relatively widespread in this group, and diabesity epidemic resulting in more diffuse and more-often non-obstructive coronary artery disease (CAD).(2) In an era of improved control of traditional risk factors, plaque erosion rather than rupture appears to have increasing clinical importance. While diagnosis of Type I MI (T1MI) due to obstructive CAD is well described in terms of pathophysiology, prognosis and treatment, less is known about Type II MI (T2MI) despite a clearly increasing incidence and prevalence.(3)
In this week’s issue of JACC, the report by McCarthy(4) and colleagues codifies the outcome of this demographic change, e.g. prospective, well-characterized analysis of T2MI in a relatively small sample size using coronary computed tomography angiography (CCTA) to assess extent and composition of coronary atherosclerosis and noninvasive fractional flow reserve (FFR) testing. Using rigorous diagnostic criteria consistent with the 4th Universal Definition of MI and adjudication of T2MI as precipitated events causing an imbalance in myocardial oxygen supply and demand, the investigators enrolled patients with no prior history of obstructive CAD to undergo coronary calcium scoring and CCTA. Participants, half female, were middle aged or elderly, predominantly White, and had a high burden of cardiovascular risk factors. There was a high prevalence (>90%) of coronary atherosclerosis, mostly non-calcified plaque, and a majority (68%) had at least one coronary vessel with distal FFRCT≤ 0.80. Hemodynamically significant focal stenosis was present in only 26% of the participants. The authors concluded that the pathogenesis of ischemia is likely multifactorial among patients with T2MI, leading us to question what might be the multifactorial pathogenesis?
While the authors adjudicated “causes” of the T2MI, e.g., identification of preceding triggers of increased demand in 81%, these are not actually etiological. More than three decades of work in the Women’s Ischemia Syndrome Evaluation (WISE) program has led us to conclude that risk factor conditions (hypertension, obesity, dyslipidemia, dysglycemia, estrogen loss and aging, often in combination) lead to cardiometabolic burden and promote a pro-inflammatory state, rendering the microvasculature and myocardium vulnerable to endothelial dysfunction, myocardial ischemia-related injury, and myocardial scar formation in women presenting with signs and symptoms of ischemia in the setting of no obstructive coronary arteries (INOCA).(5) Indeed, unusual in cardiovascular disease registries and trials, women comprised 50% of the current cohort – T2MI is a recognized equal opportunity MI! Thus, looking at prior pathogenesis work in ischemic heart disease in women offers insights to develop next step T2MI investigation and treatment targets.
To understand the etiology in the three out of four nonobstructive CAD in T2MI reported in McCarthy et al,(4) a review of findings in INOCA women in the WISE studies are instructive. Initial evaluation of WISE women with signs and symptoms of INOCA demonstrated a major adverse cardiovascular event (MACE) rate of 16.0%, including 3.9% MI, at 5-year follow-up.(6) Concomitant investigation with invasive coronary flow reserve and coronary blood flow testing demonstrated that coronary microvascular dysfunction (CMD) predicted adverse events,(7) thus stimulating additional study of determinants of CMD. Indeed, studies demonstrate CMD is most often present and a strong contributor to MACE in not only ischemic heart disease, but also heart failure with preserved ejection fraction (HFpEF).(8)
How do these etiologies described in women provide pathogenesis insight into T2MI in nonobstructive CAD? Subsequent WISE investigation has demonstrated myocardial scar measured by cardiac magnetic resonance imaging (CMRI) late-gadolinium enhancement (LGE) is present in ~8% of WISE INOCA participants tested at enrollment, most without a history of clinical MI despite often multiple chest pain evaluations and repeated coronary angiograms.(5) Importantly, new LGE was observed at a rate ~1% per year. These data, dominantly obtained before the introduction of high-sensitivity troponins which offer improved MI detection in women, suggest that T2MI incidence is an underestimate. In settings of catecholamine excess, activation of the renin-angiotensin system, oxidative stress and dysfunctional autoregulation of the coronary vasculature, the coronary microvasculature is unable to increase blood supply relative to demand.(8) However, because intracoronary imaging with intravascular ultrasound or optical coherence tomography and CMRI were not performed in this current study, mechanisms of T1MI such as atherosclerotic plaque rupture, plaque erosion with thrombosis, embolization, and dissection cannot be ruled out.(9)
We seek to understand pathogenesis to develop treatment strategies. Sadly, but perhaps not surprisingly, McCarthy and team observed low rates (<20%) of cardiology consultation and new statin prescription in the non-obstructive CAD group.(4) Diagnostic uncertainty begets therapeutic uncertainty. A diagnosis of “no obstructive CAD” is known to lead to therapeutic equipoise, including pulling patients off effective preventive therapies,(10) while imaging of coronary atherosclerosis now easily seen with CCTA leads to initiation of preventive therapies as well as improved outcomes of lower rates of MI.(11) Accordingly, these new results combined with the putative pathophysiological understanding address our current knowledge gaps regarding etiology and therefore treatment of T2MI. Indeed, the WISE work exclusively in women, along with other studies dominantly in women, have led to new diagnostic chest pain guidelines(12) and billing codes(13) to fill these diagnostic gaps. The Women’s IschemiA TRial to Reduce Events In Non-ObstRuctive CAD (WARRIOR) is a multicenter, prospective, randomized, blinded outcome evaluation of a pragmatic strategy of intensive medical therapy of high intensity statin, low dose aspirin and maximally tolerated ACE-I/ARB vs usual care in 4,422 symptomatic women with INOCA (NCT03417388) for reduction of MACE.(14)
What is next for T2MI? Current guidelines indicate statin with or without low dose aspirin therapy is indicated for evident coronary or other vascular bed atherosclerosis.(15) CCTA demonstrates coronary atherosclerosis easily for cardiologists and non-cardiologists. Do we have sufficient knowledge currently to create guidelines for basic T2MI diagnosis and treatment? Understanding T2MI pathophysiologies demonstrated by the WISE and other studies suggest that we may. Thank goodness for the women!
Figure 1. Coronary Artery Disease in Type II Myocardial Infarction(T2MI).
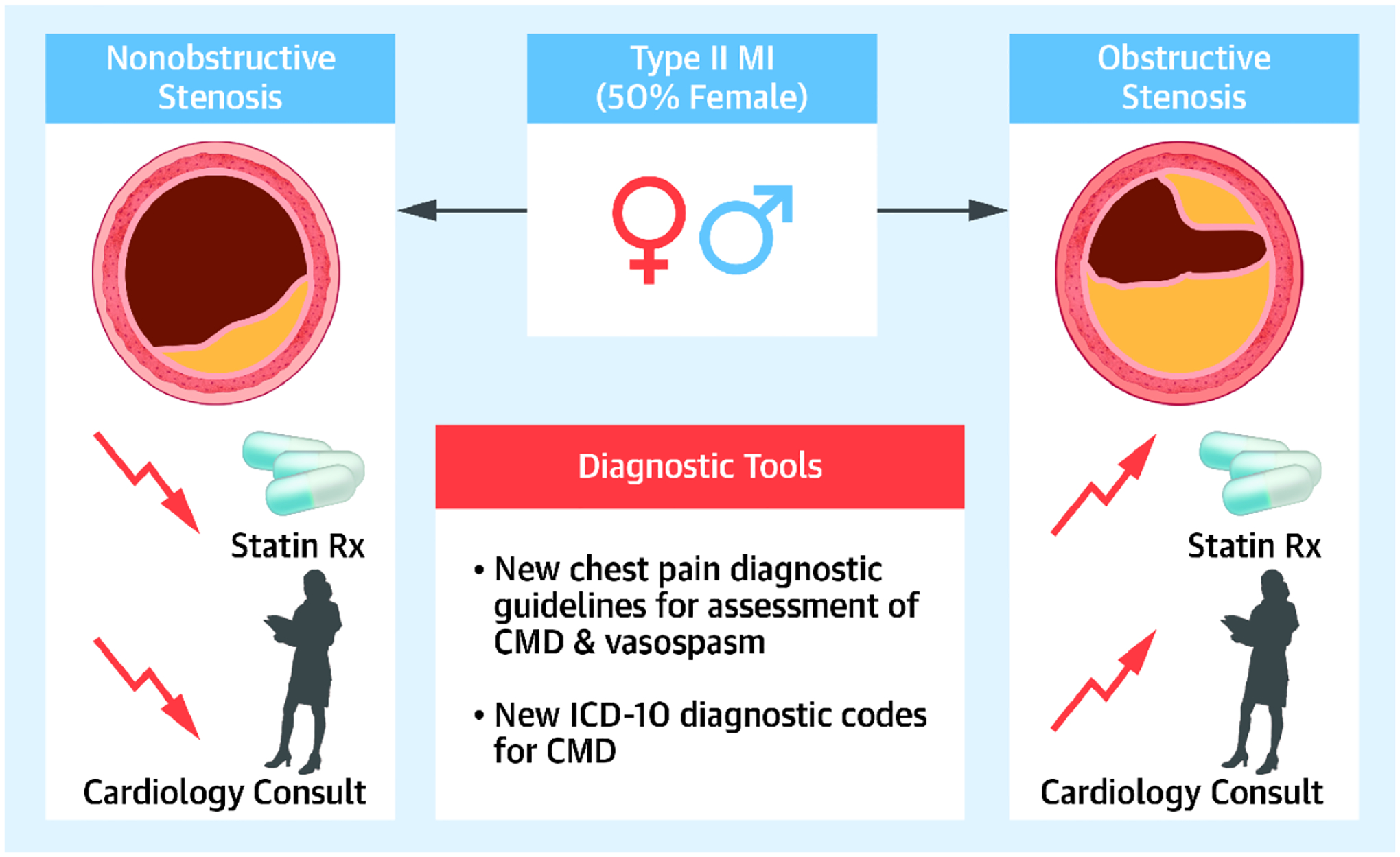
Type II Myocardial Infarction (T2MI) is associated with both obstructive and non-obstructive coronary artery disease (CAD). Nonobstructive CAD is associated with a lower use of statin treatment and lower rates of cardiac consultation. The 2021 AHA/ACC Chest Pain Guidelines provide an algorithm for evaluation of coronary microvascular disease (CMD) and vasospasm. New ICD-10 diagnostic codes for CMD are expected in the fall of 2023.
CMD= Coronary microvascular disease; MI= Myocardial infarction
Funding:
This research was supported by the National Heart, Lung, and Blood Institute (NHLBI) under grant numbers N01HV68161, N01HV68162, N01HV68163, N01HV68164, U01HL64829, U01HL64914, U01HL64924, R01HL090957, R01HL33610, R01HL056921, R01HL146158; R03AG032631, U54AG065141, M01RR000425; UL1TR000124, UL1TR000064, UL1TR001427. This work was also supported by the Barbra Streisand Women’s Cardiovascular Research and Education Program, the Linda Joy Pollin Women’s Heart Health Program, the Erika J. Glazer Women’s Heart Research Initiative Los Angeles, CA.
Footnotes
Conflict statement: Dr. Bairey Merz serves on the board of directors for iRhythm and has received consulting fees from Abbott Diagnostics and Sanofi. Dr. Gulati served as consultant for Novartis and speaker for Siemens. Dr. Wei served on an advisory board for Abbott Vascular.
References
- 1.Tsao CW, Aday AW, Almarzooq ZI et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 2023;147:e93–e621. [DOI] [PubMed] [Google Scholar]
- 2.Libby P, Pasterkamp G, Crea F, Jang IK. Reassessing the Mechanisms of Acute Coronary Syndromes. Circ Res 2019;124:150–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raphael CE, Roger VL, Sandoval Y et al. Incidence, Trends, and Outcomes of Type 2 Myocardial Infarction in a Community Cohort. Circulation 2020;141:454–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCarthy CP, Murphy SP, Amponsah DK et al. Coronary Fractional Flow Reserve Assessment by Computerized Tomography in Patients with Type 2 Myocardial Infarction. J Am Coll Cardiol. 2023;XX:XXXX. [DOI] [PubMed] [Google Scholar]
- 5.Wei J, Bakir M, Darounian N et al. Myocardial Scar Is Prevalent and Associated With Subclinical Myocardial Dysfunction in Women With Suspected Ischemia But No Obstructive Coronary Artery Disease: From the Women’s Ischemia Syndrome Evaluation-Coronary Vascular Dysfunction Study. Circulation 2018;137:874–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gulati M, Cooper-DeHoff RM, McClure C et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women’s Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med 2009;169:843–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AlBadri A, Bairey Merz CN, Johnson BD et al. Impact of Abnormal Coronary Reactivity on Long-Term Clinical Outcomes in Women. J Am Coll Cardiol 2019;73:684–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and No Obstructive Coronary Artery Disease (INOCA): Developing Evidence-Based Therapies and Research Agenda for the Next Decade. Circulation 2017;135:1075–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reynolds HR, Maehara A, Kwong RY et al. Coronary Optical Coherence Tomography and Cardiac Magnetic Resonance Imaging to Determine Underlying Causes of Myocardial Infarction With Nonobstructive Coronary Arteries in Women. Circulation 2021;143:624–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maddox TM, Stanislawski MA, Grunwald GK et al. Nonobstructive coronary artery disease and risk of myocardial infarction. Jama 2014;312:1754–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Investigators S-H, Newby DE, Adamson PD et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N Engl J Med 2018;379:924–933. [DOI] [PubMed] [Google Scholar]
- 12.Gulati M, Levy PD, Mukherjee D et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021. Nov 30;78(22):2218–2261. [DOI] [PubMed] [Google Scholar]
- 13.The Centers for Medicare and Medicaid Services; the National Center for Health Statistics. ICD-10-CM Official Guidelines for Coding and Reporting. 2023.
- 14.Handberg EM, Merz CNB, Cooper-Dehoff RM et al. Rationale and design of the Women’s Ischemia Trial to Reduce Events in Nonobstructive CAD (WARRIOR) trial. Am Heart J 2021;237:90–103. [DOI] [PubMed] [Google Scholar]
- 15.Arnett DK, Blumenthal RS, Albert MA et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019. Sep 10;74(10):e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]


