Abstract
Objectives:
To assess fracture union rates using novel intramedullary plate technique. Post-operative humeral neck-shaft angles, patient range of motion and complication profile were secondary outcomes of interest.
Methods:
Single surgeon, retrospective case series of surgical technique at major trauma centre in Scotland. A 2.0mm mini-fragment plate was secured to the humeral head to act as an intramedullary strut during fixation in complex proximal humerus fractures. Fracture union and neck-shaft angle were assessed radiologically, whilst range of motion and complication profiles were assessed clinically.
Results:
Twelve patients were followed up for an average of 10 months post-operatively. All achieved bony union with a mean neck-shaft angle of 128°. Mean range of motion values were 100° forward elevation, 83° abduction, 60° internal rotation and 37° external rotation. Four patients required further surgical intervention- two for hardware prominence, one for adhesive capsulitis and one for subsequent rotator cuff failure. There were no cases of avascular necrosis or infection.
Conclusion:
This novel technique addresses the established biomechanical propensity of proximal humerus fractures to fail in varus collapse and screw cut-out. This method provides an alternative to arthroplasty in the most severe proximal humerus fractures and is readily adopted via standard orthopaedic kit.
Key Words: Calcar, Complex, Proximal humeral fracture, Varus collapse
Introduction
Proximal humerus fractures are a common orthopaedic injury with a bimodal distribution: low energy falls in the elderly, or direct trauma to the shoulder in younger. They are typically classified by the Neer system, 1 with head splitting fractures and fracture-dislocations as additional entities. The majority of fractures in the elderly with a congruent glenohumeral joint can be treated non-operatively as recent evidence demonstrates equal outcomes to fixation.2 In higher functioning, patients operative management may be pursued with internal fixation via anatomical locking plate or, where this is not feasible, arthroplasty including reverse polarity prostheses. Advances in design have improved screw purchase within the humeral head however proximal cut-out remains an issue.3,4 A lack of a medial calcar buttress is thought to be a key contributing factor to screw cut-out, and its restoration is a key operative step.5 When calcar comminution is present this medial buttress is lost and the likelihood of fixation failure increases.6 The standard technique to address this issue involves placement of an inferomedial calcar screw through the locking plate.7 Some surgeons have opted for intra-medullary fibular strut augmentation, though this does not appear to have been widely adopted, perhaps due to the additional resources required.8 Here we present an alternative technique using an intramedullary plate to provide medial support in the presence of calcar comminution.
Materials and Methods
This is a retrospective case series from a major trauma centre in Scotland over an eight-year period. Patients were selected on the basis of having an isolated proximal humerus fracture treated by open reduction internal fixation with augmentation of the medial calcar by intramedullary plate. All patients were operated on by a single surgeon (AJ) with a specialist interest in upper limb trauma. Fracture configuration and the presence of medial calcar comminution was determined from pre-operative CT scans in all cases.
The primary study outcome was fracture union, with post-operative humeral neck-shaft angles, patient range of motion and complication profile as secondary outcomes of interest. Radiographic union and neck-shaft angles were assessed from final post-operative clinic x-rays. Range of motion and patient complications were determined from clinic records. Patients were excluded if lost to follow up.
Range of motion was deemed satisfactory if patients achieved 90° forward elevation and abduction, and 40° internal and external rotation. These values were chosen based on previously published ranges permitting activities of daily living.9 Humeral neck-shaft angle was calculated on final clinic x-rays based on a previously described method by Paavolainen, with results graded as “good” (130° +/- 10), “fair” (100-120°) or “poor” (<100°). 10
Operative Technique
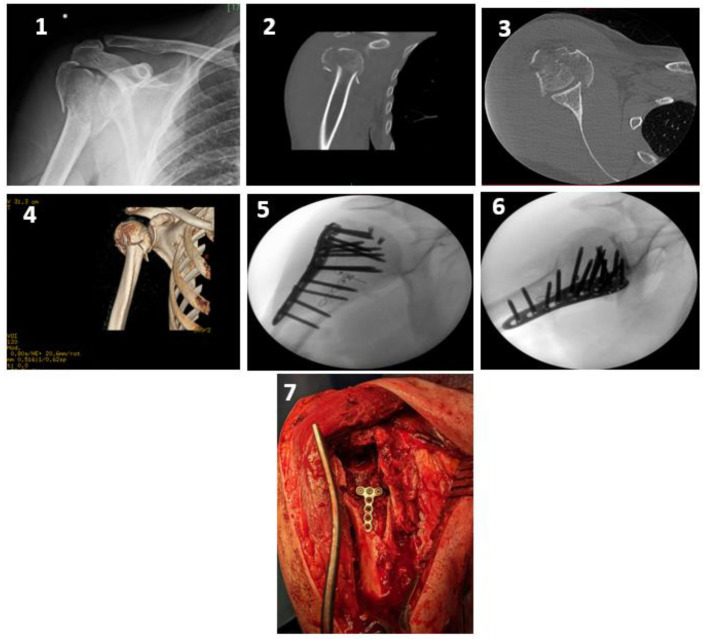
All operations were performed through a deltopectoral approach. Fracture fragments were mobilised to allow access to the intramedullary canal and humeral head fragment. A 2.0mm mini fragment T plate was cut to length and contoured. This was fixed proximally into the residual calcar region of the humeral head via locking screws. In the absence of sufficient proximal bone stock screws were placed in a divergent subchondral manner avoiding articular penetration. Thereafter the humeral head-plate construct was reduced onto the shaft but not fixed distally which allowed the plate to function as an intramedullary peg. The remaining fracture fragments were reduced and a lateral locking plate (PHILOS- Synthes) applied. If further fragments required stabilising these were addressed via additional plate(s). A case example is shown below [Figure 1-7].
Figure 1-7.
Four part proximal humerus fracture (with head split). Intra-operative images showing intramedullary plate augmentation to aid medial stability. Intra-op photograph showing intramedullary plate positioning
The post-operative protocol consisted of two weeks of restricted motion in a polysling, followed by early mobilisation- two weeks passive, two weeks active assisted, and thereafter active motion. This was overseen by a physiotherapist, with regular clinic follow up with an orthopaedic surgeon.
Results
A total of thirteen patients (eight women and five men) underwent internal fixation with intra-medullary plate augmentation. The mean patient age was 53 (range of 36 - 73). All patients had 4 part fractures with loss of medial column support, with one also having a head split (fixed with headless compression screws). One patient died in the perioperative period from an unrelated duodenal perforation. The remaining twelve patients were following up for an average of 10 months (range 3 - 24 months).
All patients achieved bony union without loss of reduction. The mean humeral neck shaft angle calculated by Paavolainen method was 128° (range 114-141°), with eight patients achieving a “good” result and the remaining four a “fair” result.
Four patients required further surgical intervention- two for hardware prominence, one for adhesive capsulitis and one for subsequent rotator cuff failure. One patient with metalwork removal had subacromial impingement caused by the lateral locking plate, whilst the other patient had articular screw penetration secondary to early fracture subsidence. The single case of adhesive capsulitis underwent arthroscopic release. Lastly the patient with rotator cuff failure had an initial period of functional recovery before developing this pathology in the months following injury and was treated with arthroscopic cuff repair. There were no cases of avascular necrosis and no cases of superficial or deep infection.
Complete range of motion for each patient is detailed in [Table 1]. A satisfactory functional result was achieved by eight of twelve patients (90° elevation, 90° abduction, 40° external & 40° internal rotation). Mean values were 100° forward elevation, 83° abduction, 60° internal rotation and 37° external rotation.
Table 1.
Patient demographics, radiological & functional outcomes, and complications. (NSA = neck shaft angle; Elev= forward elevation; Ab= abduction; IR = internal rotation; ER = external rotation). Follow up in months
| Sex | Age | NSA | Elev | Ab | IR | ER | FU | Complication |
|---|---|---|---|---|---|---|---|---|
| Mean | 53 | 128 | 96 | 82 | 40 | 35 | 10.58 | |
| F | 70 | 135 | 70 | 70 | 70 | 25 | 3 | Adhesive capsulitis |
| F | 52 | 141 | 40 | 30 | 30 | 30 | 12 | |
| M | 36 | 140 | 90 | 90 | 50 | 50 | 13 | |
| F | 67 | 119 | 140 | 110 | 90 | 45 | 6 | |
| F | 55 | 120 | 130 | 110 | 90 | 45 | 8 | |
| M | 41 | 127 | 100 | 90 | 45 | 45 | 5 | |
| F | 52 | 114 | 80 | 70 | 20 | 20 | 12 | Removal metalwork |
| M | 51 | 132 | 100 | 90 | 50 | 40 | 24 | |
| M | 31 | 125 | 90 | 90 | 90 | 40 | 3 | |
| F | 66 | 119 | 80 | 45 | 0 | 10 | 15 | Cuff failure |
| F | 73 | 125 | 130 | 90 | 90 | 45 | 10 | |
| M | 43 | 136 | 150 | 110 | 90 | 45 | 16 | Removal metalwork |
Discussion
The medial calcar functions as a critical supporting column in proximal humeral fractures, preventing varus malunion and subsequent failure. Jung reported increased rates of non-union, head collapse and metalwork cut-out in fractures with disrupted medial support (37% vs 11% in those with an intact medial column).5 This is in line with earlier published series showing fixation failure rates of between 11% and 22%.11,12 A recent systematic review of seventy-six studies demonstrated a combined rate of 13.1% for varus collapse, malunion and metalwork failure related to the PHILOS proximal humerus plate.3 Biomechanical studies have demonstrated lower load to failure when medial calcar support is absent,6 and various solutions have been proposed. Gardner was one of the first to recognise this challenge and suggested the placement of an inferomedial locking screw to provide sufficient support for fracture healing.7 He later proposed the use of an intramedullary fibular strut to improve medial support, though the technique is technically demanding and requires available allograft.8 Other suggested methods include humeral head impaction, cementation, and bone block augmentation.6,13 More recently, supplementary anterior plating or extra-medullary medial plating has been proposed in small scale studies.14,15
Restoration of an adequate neck-shaft angle was achieved intra-operatively in all cases, and subsequent measurement at final follow up demonstrated preservation of this relationship. The majority of patients achieved a satisfactory functional range of motion.9 Those who did not had a recognisable complication: metalwork impingement, adhesive capsulitis or massive rotator
cuff tear. It is not possible to directly compare these results to other studies as patient reported outcome measures were not collected in our study.
Intramedullary plating seeks to directly address the biomechanical deficit of these complex proximal humerus fractures. It functions as a strut or peg, allowing load transfer to the inferior humeral head and preventing varus failure of fracture fixation. We believe this improves fracture union and prevents screw cut-out. Omission of distal fixation allows for fine adjustments during subsequent reduction of the tuberosity fragments without undue stress on a fixed head-shaft position.
Avascular necrosis is known to increase with fracture complexity and loss of medial hinge.16 The rates of reported avascular necrosis (AVN) vary significantly depending on fracture complexity and duration of follow up. Older studies variously report rates of between 5-16% in individual series.17,18 Gerber et al looked specifically at complex proximal humerus fractures, an injury cohort comparable to our study population, and found AVN occurrence in 35% of patients.19 Within our series there were no cases of AVN, which may be as a result of the improved fracture stability achieved, although this remains a hypothesis at present.
The complications encountered in this case series are well recognised in existing literature. Screw penetration can occur though excessive screw length or through fracture subsidence where the lateral locking plate abuts comminuted bone. This occurred in one patient though the fracture subsequently united with maintenance of the neck-shaft angle and removal of the screws resolved symptoms. Sub-acromial impingement was the causative reason for metalwork removal another case. This has been documented extensively with proximal humerus plates, and is caused by an excessively cephalad position of the plate. Whilst this is usually an avoidable technical error, it is representative of the complexity of fractures within our series and compromise between plate positioning and screw purchase. Finally, post-traumatic adhesive capsulitis is encountered in both operative and conservatively managed proximal humerus fractures. At our institution a programme of intensive physical therapy is pursued first, with arthroscopic release reserved for cases that fail to improve as was experienced by one patient.
Notwithstanding the above, we believe the technique has merit for several reasons. Firstly, the technique focuses on fracture stability, preventing varus failure and screw cutout. Secondly, it achieves this in a more time and resource efficient manner than proposed by Gardner- avoiding allograft use and using only a standard 2.0mm plate. Lastly, this surgical technique preserves bone stock and avoids arthroplasty, particularly in young, active patients. Proximal humerus fractures treated with hemiarthoplasty have mixed results at best, with frequent complications such as tuberosity non-union and head subluxation.20 Overall satisfaction with the procedure is expectedly low and hence it is seen as a last resort option. 21
It must be recognised that this study has a range of limitations. It is a small scale, retrospective case series of radiographic and functional data only, and therefore caution must be taken in extrapolation to the wider patient population. As the study contains only twelve cases and lacks a control group, it is not possible to ascribe either positive or negative outcomes solely to the novel intramedullary plate. Lastly, no patient reported outcome measures were available.
Conclusion
In conclusion, we present a novel technique of supplementary intramedullary plate fixation in proximal humerus fractures with medial comminution. We believe this addresses the established biomechanical propensity of these fractures to fail in varus collapse and screw cut-out. Our series of twelve cases has shown excellent radiographic outcome and reasonable functional results. This technique provides an alternative to arthroplasty in the most severe proximal humerus fractures and is readily adopted via standard orthopaedic kit.
Acknowledgment
Not applicable
Conflict of interest:
None
Funding:
None
References
- 1.Neer CS 2nd. Displaced proximal humeral fractures I Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 2.Handoll H, Brealey S, Rangan A, et al. The ProFHER (PROximal Fracture of the Humerus: Evaluation by Randomisation) trial – a pragmatic multicentre randomised controlled trial evaluating the clinical effectiveness and cost-effectiveness of surgical compared with non-surgical treatment for proximal fracture of the humerus in adults. Health Technol Assess (Rockv). 2015;19(24):1–280. doi: 10.3310/hta19240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oldrini LM, Feltri P, Albanese J, Marbach F, Filardo G, Candrian C. PHILOS Synthesis for Proximal Humerus Fractures Has High Complications and Reintervention Rates: A Systematic Review and Meta-Analysis. Life (Basel). 2022;12(2):311. doi: 10.3390/life12020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McMillan TE, Johnstone AJ. Primary screw perforation or subsequent screw cut-out following proximal humerus fracture fixation using locking plates: a review of causative factors and proposed solutions. Int Orthop. 2018;42(8):1935–1942. doi: 10.1007/s00264-017-3652-6. [DOI] [PubMed] [Google Scholar]
- 5.Jung WB, Moon ES, Kim SK, Kovacevic D, Kim MS. Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskelet Disord. 2013;14(1):102 . doi: 10.1186/1471-2474-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katthagen JC, Schwarze M, Meyer-Kobbe J, Voigt C, Hurschler C, Lill H. Biomechanical effects of calcar screws and bone block augmentation on medial support in locked plating of proximal humeral fractures. Clinical Biomechanics. 2014;29(7):735–741. doi: 10.1016/j.clinbiomech.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The Importance of Medial Support in Locked Plating of Proximal Humerus Fractures. J Orthop Trauma. 2007;21(3):185–191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 8.Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Indirect Medial Reduction and Strut Support of Proximal Humerus Fractures Using an Endosteal Implant. J Orthop Trauma. 2008;22(3):195–200. doi: 10.1097/BOT.0b013e31815b3922. [DOI] [PubMed] [Google Scholar]
- 9.Doorenbosch CAM, Harlaar J, Veeger DHEJ. The globe system: an unambiguous description of shoulder positions in daily life movements. J Rehabil Res Dev. 2003;40(2):147–155. [PubMed] [Google Scholar]
- 10.Paavolainen P, Björkenheim JM, Slätis P, Paukku P. Operative Treatment of Severe Proximal Humeral Fractures. Acta Orthop Scand. 1983;54(3):374–379. doi: 10.3109/17453678308996587. [DOI] [PubMed] [Google Scholar]
- 11.Frangen T, Dudda M, Martin D, et al. Operative und klinische Erfahrungen mit winkelstabilen Implantaten bei proximalen Humerusfrakturen - Wirklich alles besser? Zentralbl Chir. 2007;132(1):60–69. doi: 10.1055/s-2006-958639. [DOI] [PubMed] [Google Scholar]
- 12.Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R. A New Locking Plate for Unstable Fractures of the Proximal Humerus. Clin Orthop Relat Res. 2005;430:176–181. doi: 10.1097/01.blo.0000137554.91189.a9. [DOI] [PubMed] [Google Scholar]
- 13.Schöbel T, Schleifenbaum S, Nitsch V, Hepp P, Theopold J. Primary stability of cement augmentation in locking plate fixation for proximal humeral fractures: A comparison of absorbable versus non-absorbable cement. Clin Biomech (Bristol, Avon). 2022;91:105516. doi: 10.1016/j.clinbiomech.2021.105516. [DOI] [PubMed] [Google Scholar]
- 14.Warnhoff M, Jensen G, Dey Hazra RO, Theruvath P, Lill H, Ellwein A. Double plating - surgical technique and good clinical results in complex and highly unstable proximal humeral fractures. Injury. 2021;52(8):2285–2291. doi: 10.1016/j.injury.2021.05.047. [DOI] [PubMed] [Google Scholar]
- 15.Park SG, Ko YJ. Medial Buttress Plating for Humerus Fractures with Unstable Medial Column. J Orthop Trauma. 2019;33(9):e352–e359. doi: 10.1097/BOT.0000000000001515. [DOI] [PubMed] [Google Scholar]
- 16.Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13(4):427–433. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 17.Plecko M, Kraus A. Die winkelstabile Plattenosteosynthese bei Frakturen am proximalen Humerus mit der LPHP (Locking Proximal Humerus Plate) Oper Orthop Traumatol. 2005;17(1):25–50. doi: 10.1007/s00064-005-1120-8. [DOI] [PubMed] [Google Scholar]
- 18.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical Treatment of Three and Four-Part Proximal Humeral Fractures. J Bone Joint Surg Am. 2009;91(7):1689–1697. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]
- 19.Gerber C, Werner CML, Vienne P. Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br. 2004;86-B(6):848–855. doi: 10.1302/0301-620x.86b6.14577. [DOI] [PubMed] [Google Scholar]
- 20.Mighell MA, Kolm GP, Collinge CA, Frankle MA. Outcomes of hemiarthroplasty for fractures of the proximal humerus. J Shoulder Elbow Surg. 2003;12(6):569–577. doi: 10.1016/s1058-2746(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 21.Kontakis G, Koutras C, Tosounidis T, Giannoudis P. Early management of proximal humeral fractures with hemiarthroplasty. J Bone Joint Surg Br. 2008;90-B(11):1407–1413. doi: 10.1302/0301-620X.90B11.21070. [DOI] [PubMed] [Google Scholar]