Abstract
A scoping review was conducted to explore support interventions for family members of a child treated with hematopoietic stem cell transplant (HSCT). Three databases (CINAHL, Embase, and Medline) were searched to answer the review question: What are the support interventions offered to family members of a child treated with HSCT and are they based on a family-centred care approach? Out of 665 screened articles, nine were selected for full review. Findings revealed two main types of family-centred support interventions: psychological face-to-face and technology-based interventions. The majority of interventions assisted in improving family members’ psychological well-being and included a portion of the core concepts from the Institute for Patient and Family-Centered Care Model in their approach. Based on the review findings, interventions that incorporate family-centred care concepts can enhance the psychological well-being and quality of life of family members whose child is undergoing HSCT treatment.
BACKGROUND
Although hematopoietic stem cell transplant (HSCT) can be lifesaving for children with hematological malignancies and disorders, it is also an intensive and aggressive treatment that may have detrimental effects on the psychological well-being of patients and family members (Kearney et al., 2015; Packman et al., 2010; Riva et al., 2014). On average, 20% of parents of a child treated with HSCT have clinically significant stress levels, while 66% of mothers have clinically significant depression and 50% have clinically significant anxiety (Packman et al., 2010). Stressors stem from the uncertainties of the child’s outcomes, treatment complications, and the financial and pragmatic challenges of being in the hospital with their child ‘twenty-four/seven’ for several months (Maziarz & Slater, 2015). The significant psychological complications are not only harmful to the parents, but research also shows that parental distress is indirectly detrimental to their child’s psychological well-being (Kearney et al., 2015).
Overall, what we know is that this treatment can be detrimental to both the family member’s and the child’s psychological well-being. However, how to best support these family members remains fairly unknown. Through a pediatric nursing lens this is concerning, as it is essential to provide care to the patient which encompasses all family members due to their impact on the child’s well-being. Thus, this scoping review aimed to examine the literature regarding supportive interventions for family members of children undergoing HSCT.
As noted above, this scoping review is written through a pediatric nursing lens. In pediatrics, family-centred care is the foundation for considering both the child and family members as the patient of concern. Shields, Pratt, and Hunter (2006) define family-centred care as “… a way of caring for children and their families within health services which ensures that care is planned around the whole family, not just the individual child/person, and in which all family members are recognized as care recipients” (p. 1318). This care involves a partnership between healthcare providers and family members (Kuo et al., 2012). Together this partnership assists in supporting families through the complicated process of having a sick child. As noted earlier, this care is essential, as family members are the main nurturers and caregivers for their child and, thus, have a significant impact on their quality of life and well-being (Kuo et al., 2012; Mackay & Gregory, 2011; Pettoello-Mantovani et al., 2009).
In this review, we utilized the Institute for Patient- and Family-Centered Care (IPFCC) model to evaluate the alignment between the supportive interventions and a family-centred care approach. The IPFCC came to life in 1992 as a non-profit organization that takes a leadership role in offering a central resource for understanding and practicing patient- and family-centred care. IPFCC built its care model on four core concepts of patient- and family-centred care from the work of Picker Institute and further developed through quality improvement projects aimed at advancing quality of care (Conway et al., 2006). This model of care delivery is highly respected throughout North America as a leader in family-centred care practice and, thus, has been adopted by many pediatric hospitals (Institute for Patient- and Family-Centered Care, 2021). For example, the MCG Health System from Georgia integrated this model into the development of its hospital and conducted a quality improvement project over three years which showed that the implementation of this type of care improved patient satisfactions scores from the 10th to the 95th percentile (Conway et al., 2006).
The IPFCC model incorporates the following four core concepts of patient- and family-centred care: dignity and respect, participation, information sharing and collaboration. Together these concepts create an approach to care that involves a partnership between healthcare and family members (Institute for Patient- and Family-Centered Care, 2021). Dignity and respect require healthcare providers to listen and honor families’ knowledge, values, beliefs, and cultural backgrounds in planning and delivering care. Participation requires the healthcare team to encourage and support families in participating in their child’s care at their comfort level. Information sharing refers to communication that is delivered timely, complete, unbiased, and accurate to families as they participate and decide on their child’s care. Finally, collaboration involves the partnership between family members and the healthcare team in policy, program development, implementation, and evaluation for facility design, research, professional education and delivery of care (Institute for Patient- and Family-Centered Care, 2021). Overall, hospitals that have integrated the IPFCC model of care into their policies and leadership, have improved health outcomes and satisfaction of care for patients and family members (Community on Hospital Care and Institute for Patient-and Family-Centered Care, 2021).
PURPOSE
This review examined the literature regarding supportive interventions for family members of children undergoing HSCT. Furthermore, we used the IPFCC model to evaluate supportive interventions with the objective to determine how well these interventions align with the principles of family-centred care. Our overall intention was to gain knowledge that could be used to improve family members psychological wellbeing throughout the HSCT treatment journey.
REVIEW QUESTION
The following question guided this scoping review: What are the support interventions offered to family members of a child treated with HSCT and are the interventions based on a family-centred care approach?
METHODS
This scoping review was guided by the Joanna Briggs Institute (JBI) framework (Peters et al., 2015) to provide a synthesis of knowledge methodology that is rigorous, trustworthy, and transparent (Aromataris & Munn, 2020). This methodology supported the following scoping review process by: 1) developing a search strategy to align with the research question; 2) describing the search process; 3) searching, selecting, extracting, and analyzing the evidence; and 4) presenting and summarizing findings while noting the implication for nursing practice. The Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Review (PRISMA-ScR) also guided the screening process (Tricco et al., 2018).
Search Strategy
A search was conducted in MEDLINE, Embase, and Cumulated Index to Nursing and Allied Health Literature (CINAHL) to identify published research that focused on supportive interventions offered to family members of a child treated with HSCT. These databases were searched from September to October 2021, with an updated search conducted in June 2023. The search strategy used key subject terms describing the population (family members of a child treated with HSCT), the concept (support interventions), and the context (family-centred care approach). The subject term for population included ‘Parents’, the pediatric population (‘Child’, ‘Infant’, and ‘Adolescent’) and HSCT (‘Stem Cell Transplant’, and ‘Hematopoietic Stem Cell Transplant’) and was combined with an extensive list of keywords, dependent on the database, using the Boolean operator OR. Similarly, the concept was represented by subject terms ‘social support’ and ‘disciplines, test, therapy, services’ and paired with keywords using the Boolean operator OR. The context was represented by subject terms ‘family-centred care’, and ‘family nursing’ and combined in the same manner. Finally, the population, concept and context subject and keyword terms were connected with the Boolean operator AND. In addition, all searches were limited to English written articles and any article published within the last 20 years. After the search was conducted, an initial screening was conducted to eliminate articles that focused on an adult population, discharge and/or long-term follow-up, bereavement and/or palliative, or did not focus on the caregivers and supportive interventions.
The search results from each database (i.e., full list of articles) were imported into Covidence for automatic identification and removal of duplicates. The selection process was conducted by one author (PL). The titles and abstracts were screened, and studies were deemed irrelevant if they did not include the above concept and/or population. Next, the same reviewer (PL) completed a full-text review of the remaining articles to ensure these met the inclusion criteria, i.e., study testing a supportive intervention, focusing on caregiver support, and not involving discharged and/or long-term follow-up of patients. Studies that met these selection criteria were included in the review.
Content data from each article were extracted utilizing both the Garrard Matrix Method (Garrard, 2017) and the four core concepts of the IPFCC model (Institute for Patient- and Family-Centered Care, 2021) to address the context of the above review question. Thus, 23 columns were included in the Matrix; population, theory, sampling, aim, type of study, inclusion, exclusion, sample characteristics, funding, intervention, outcome, methods, data collection, data analysis, study approval, coping/adapting strategies, limitations, next steps, future implications, dignity and respect, information sharing, participation, and collaboration.
The data were examined in terms of interventions type and their impact on families. Each study (i.e., intervention tested) was also appraised in relation to IPFCC model’s (2021) four core concepts. Thus, the data were first organized in the Garrard Matrix Method table. Followed an in-depth analysis of each study to examine how each intervention aligned with the IPFCC core concepts using thematic analysis.
RESULTS
Study Selection
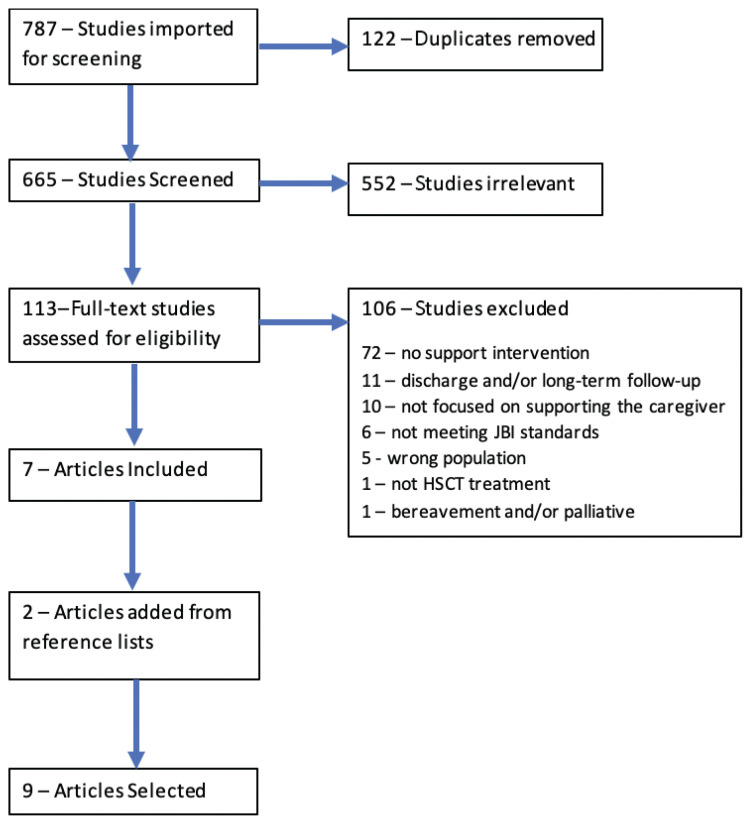
A total of 787 citations were identified. Of these, 122 were duplicates and eliminated from the reviewed results, for a total of 665 articles. Of those articles, 113 were included in the full-text review. Seven articles were included and from hand searching of these articles, two additional articles were added to the scoping review for a total of nine articles (see Figure 1). The Streisand et al. (2000) article was retrieved from the article by Lindwall et al. (2014) and the Manne et al. (2016) article was retrieved from the reference list in Sands et al. (2017). Thus, in total, nine articles met the inclusion criteria and aligned with the scoping review question.
Figure 1.
PRISMA-ScR Flow Diagram of Study Selection
Characteristics of the Studies and Participants
Of the nine articles, three presented randomized controlled trials (RCT) (Liu et al., 2020; Manne et al., 2016; Streisand et al., 2000), two secondary analyses of RCTs (Lindwall et al., 2014; Sands et al., 2017), one qualitative descriptive study (Runaas et al., 2017), one quasi-experimental study (Racine et al., 2018), one clinical trial (Fauer et al., 2019), and one pilot study (Holochwost et al., 2020). The majority of the studies were conducted in the United States of America (n = 7), with one in Canada (n = 1), and one in Taiwan (n = 1). Seven studies focused on face-to-face interventions (Holochwost et al., 2020; Lindwall et al., 2014; Liu et al., 2020; Manne et al., 2016; Racine et al., 2018; Sands et al., 2017; Streisand et al., 2000) and two focused on technology-based support interventions (Fauer et al., 2019; Runaas et al., 2017).
The face-to-face interventions included psychological support through support groups (Racine et al., 2018), massage (Lindwall et al., 2014) and relaxation training/sessions (Manne et al., 2016; Sands et al., 2017; Streisand et al., 2000), music therapy (Holochwost et al., 2020), and nurse-facilitated interventions (Liu et al., 2020). Table 1 provides a summary of the nine studies included in this scoping review.
Table 1.
Summary of Studies (N = 9)
| Authors | Supportive Intervention | Theory | Sample | Study Design, Objective | Summary of Findings |
|---|---|---|---|---|---|
| Streisand et al., 2000 | Psychological support (education, relaxation & communication) | N/A | 22 parents of a child scheduled to undergo inpatient BMT | Randomized Control Trial (RCT) – comparing psychological support with standard of care on parent’s stress over the course of treatment | Highest stress levels preadmission Intervention group utilized more intervention techniques vs controls & use them to assist in coping |
| Lindwall et al., 2014 | 3 Children + Parent targeted intervention (massage & relaxation training/sessions) | N/A | 171 patient-parent dyads from multiple hospitals in Canada & USA | Secondary analysis (RCT); to assess how the intervention affected parental adjustment | All interventions decreased emotional distress & increase positive adjustment No significant differences between all 3 interventions |
| Manne et al., 2016 | Parent Social-Cognitive Intervention Program (P-SCIP) include discussions on; stress, coping solvable/ unsolvable problems, social life & applying skills | Cognitive-Social Processing Theory of adjustment to traumatic events | 218 Parents of children scheduled for HSCT from 4 centers across USA | RCT (BPC or P-SCIP) 3 aims; 1) compare P-SCIP with Best Practice Psychosocial Care (BPC), 2) evaluate psychosocial & medical treatment moderators, 3) examine P-SCIP mechanisms |
Significant interaction between decreased depression & anxiety levels and increased coping techniques with P-SCIP at the beginning of the treatment process compared to BPC |
| Runaas et al., 2017 | Bone Marrow Transplant (BMT) Roadmap: Electronic resources: a) lab results b) medications lists c) clinical trials d) health care provider directory e) HSCT process f) discharge checklist | N/A | 10 caregivers (majority Caucasian mothers) of children undergoing first-time HSCT in Michigan | Qualitative Descriptive Study – explore how to improve the BMT Roadmap | Parents & health care members noted the application improved communication Parents used the laboratory results & wanted more communication tools |
| Sands et al., 2017 | Best Practice Care (BPC); provided information on HSCT, coping, caregiver issues, respite & walkie-talkie to communicate with child | Cognitive-Social Processing Theory of adjustment to traumatic events | 218 Parents of children scheduled for HSCT from 4 centers across USA | Secondary analysis of the Manne et al. (2016) RCT – focused on trajectories of psychological responses of the control group that received BPC | Maladaptive coping (self-blame, potential for suffering, holding back concerns and worry frequency) related to higher distress trajectories Problem solving & family support were the only 2 beneficial adaptive skills |
| Racine et al., 2018 | Support Group: 1hr support group facilitated by a social worker + one educational session | N/A | 10 Caregivers of children receiving HSCT treatment at Alberta Children’s hospital (Canada) | Quasi-experimental study - describing program development & evaluation | Majority parents had decreased distress, were satisfied with the sessions, and wanted more educational sessions |
| Fauer et al., 2019 | BMT Roadmap (Phase 2): lab results, medication, clinical trial enrollment, health care provider directory, and discharge checklist | N/A | 19 caregivers of a child undergoing their first HSCT in Michigan | Phase 2 of a Clinical Trial – Trialing the BMT Roadmap preliminary feasibility study and assessing parents’ mental health & quality of life Mental Health survey; increased vigor and decreased anxiety, distress, depression, & fatigue from baseline to discharge |
Quality of Life survey; depression, anxiety, & fatigue decreased until discharge |
| Holochwost et al., 2020 | Active Music Engagement (AME); caregivers & their child covering 3 components a) therapist-led music-based play activities/ sessions b) music play resource kit c) session planning & caregiver tip sheet | Robb’s Contextual Support Model of Music Therapy and Kazak’s Pediatric Medical Traumatic Stress Model | 4 Caregiver-Child dyads undergoing inpatient HSCT | Pilot study assessing the feasibility/ acceptability of the AME intervention & biological samples required when using single-case design | 84.4 % feasibility Caregiver’s + child’s emotional and physical distress improved during & after the AME sessions Decreased cortisol levels in both parent & child |
| Liu et al., 2020 | Nurse-facilitated support intervention provided at 3 times; a) sharing past experiences b) promoting support c) providing medical information relevant to each caregiver’s child d) reducing caregiver distress | Davidson’s Theory of facilitated sense-making | 43 caregivers of a child requiring allogeneic HSCT in Taiwan | Longitudinal RCT – Evaluate a nurse-facilitated caregiver’s support intervention for hospitalized pediatric HSCT patients | Caregiver anxiety & depression levels did not differ between intervention & control groups Perceived stress was significantly lower, & quality of life scores were higher for the intervention group |
Three of the seven face-to-face interventions demonstrated improvements in the family member’s psychological well-being (Holocowost et al., 2020; Manne et al., 2016; Racine et al., 2018) and one intervention (nurse-facilitated support group) improved their quality of life (Liu et al., 2022). By providing adaptive coping skills, the therapist-led Parent Social-Cognitive Processing Intervention Program (P-SCIP) showed improvement in caregivers’ anxiety levels, depression symptoms and traumatic distress compared to the standard of care (Manne et al., 2016). Lower caregiver distress and cortisol levels were also shown to decrease after music therapy sessions (Holocowost et al., 2020). Support groups run by social worker students and psychology residents were also found to positively impact distress in caregivers (Racine et al., 2018). Finally, caregiver’s quality of life significantly improved from nurse-facilitated interventions that provided support and education to caregivers (p < 0.01) (Liu et al., 2022).
Two studies (Fauer et al., 2019; Runaas et al., 2017) examined a technology-based support intervention, the Bone Marrow Transplant (BMT) Roadmap. This electronic resource was designed to support caregivers with their child’s treatment and included: real-time lab results, medications information, clinical trial updates, healthcare provider directory, treatment trajectory, and discharge checklists. The studies mainly assessed the BMT Roadmap’s feasibility (Runaas et al., 2017) and impact on parents’ psychological well-being through interviews and/or survey data (Fauer et al., 2019). The use of the BMT Roadmap by caregivers lowered their anxiety and fatigue levels, which in turn positively improved their quality of life from baseline to discharge (Faurer et al. 2019).
Overall, the interventions were in the early phases of their development (i.e., pilot RCT, feasibility study) and had only been tested on small sample sizes with homogenous populations and at single institutions. Thus, the generalizability of findings is limited. In fact, most authors discussed the need to test their interventions on more heterogenous populations and for multi-site studies.
Family-Centred Principles
Examining the studies in relation to the IPFCC Model (2021) principles showed that in the design of each intervention, two of the four family-centred core concepts were covered (Table 2). The psychological interventions included the concepts of dignity and respect by offering the opportunity for family members to be heard and honored for their knowledge, beliefs, values, and cultural backgrounds with the intent of supporting and assisting them in providing care for their child. These interventions also provided participation by encouraging and supporting the family members to take part in their child’s care through support groups, music therapy, massage, and relaxation/training sessions (Holochwost et al., 2020; Lindwall et al., 2014; Liu et al., 2020; Manne et al., 2016; Racine et al., 2018; Sands et al., 2017; Streisand et al., 2000). Whereas the studies testing the technology-based BMT Roadmap intervention encompassed the information sharing concept by communicating timely, complete, unbiased, and accurate information to the family members (Fauer et al., 2019; Runaas et al., 2017). The information communicated was key for family members to participate and decide on their child’s care. The BMT Roadmap also functioned as a communication tool between health care providers and family members and thus, promoted collaboration.
Table 2.
Family-Centred Care Principles in Relation to Reviewed Studies
| Authors | Dignity & Respect | Information Sharing | Participation | Collaboration |
|---|---|---|---|---|
| Streisand et al., 2000 | X | X | ||
| Lindwall et al., 2014 | X | X | ||
| Manne et al., 2016 | X | X | ||
| Sands et al., 2017 | X | X | ||
| Runaas et al., 2017 | X | X | ||
| Racine et al., 2018 | X | X | ||
| Fauer et al., 2019 | X | X | ||
| Holochwost et al., 2020 | X | X | ||
| Liu et al., 2020 | X | X |
DISCUSSION
This scoping review examined nine studies that offered eight different interventions. The psychological interventions, which demonstrated the IPFCC core concepts of dignity and respect and participation, resulted in overall decreased distress, anxiety, and depressive symptoms (Holochwost et al., 2020; Lindwall et al., 2014; Liu et al., 2020; Manne et al., 2016; Racine et al., 2018; Sands et al., 2017; Streisand et al., 2000), improved coping capabilities (Manne et al., 2016; Sands et al., 2017), and enhanced quality of life (Liu et al., 2020) of family members of children undergoing HSCT. However, one of the main limitations of these interventions was that family members were required to leave their child’s bedside to attend support sessions, which was often challenging due to their child’s everchanging condition and needs. On the other hand, the technology-based BMT Roadmap intervention had the benefit o f being easily accessible by parents at the convenience of their child’s bedside, and demonstrating how incorporating the information sharing and collaboration core IPFCC concepts can enhance its usability (Fauer et al., 2019; Runaas et al., 2017). The first study described the feasibility of the intervention which was deemed easy to use by both healthcare and family members (Runaas et al., 2017). While a subsequent study investigated the effect of the intervention on family members’ mental health and quality of life (Fauer et al., 2019). The studies found that the intervention improved the communication between both healthcare and family members, and enhanced the psychological well-being and quality of life for family members (Fauer et al., 2019; Runaas et al., 2017). Altogether, the face-to-face and technology-based interventions improved family members’ psychological well-being and quality of life, but none included all four core concepts. Each intervention targeted a specific aspect of care, which is why not all four core concepts were incorporated in every intervention. For example, the face-to-face interventions focused on supporting and listening to family members, whereas the technology-based intervention focused on efficient communication and information sharing between healthcare and family members.
As stated previously, the model developed by the IPFCC is based on four core concepts derived from previous research, which identified these approaches as beneficial for enhancing the quality of care for both families and patients (Conway et al., 2006). Together these four core concepts intertwine to support healthcare providers in providing care that empowers and increases the self-efficacy of family members, which then can reduce their anxiety and fears related to their child’s well-being (Salvador et al., 2019). A mixed-method descriptive study exploring family-centred care throughout parent’s experiences of having a child be hospitalized, noted that when healthcare members incorporated collaboration, participation, and information sharing core concepts into their care, parents were able to acquire knowledge, subsequently reducing their fears and anxieties concerning their child’s treatment. This knowledge is essential to enhance their ability to empower parents in fulfilling their role (Uhl et al., 2013). HSCT is an intensive treatment that can have many unpredictable and life-threatening complications such as, graft versus host disease and infections (SickKids, 2020). Thus, many parents are left with anxiety and fear of the unknown. The BMT Roadmap allowed for real-time updates and improved collaboration and information sharing for family members and, thus, reduced their sources of stress (Fauer et al., 2019). A unique aspect of pediatric HSCT treatment is that family members have to adjust to caregiving at the hospital for several months (Maziarz & Slater, 2015). Thus, it is essential for them to navigate their caregiving role in this new setting. The psychological interventions that targeted family members participation, such as the P-SCIP intervention by Manne et al. (2016), provided education on coping mechanisms to assist in caring for a sick child, empowering family members in their new caregiving role.
To assist in positive collaboration, information sharing and participation, Uhl et al. (2013) noted the importance of establishing a positive relationship between the healthcare provider and family member, as it empowers them and, thus, reduces their stress levels. An explorative qualitative study that examined nurses and family members of a hospitalized child perceptions on family-centred care, noted that nurses felt it was essential to acknowledge the importance in a positive nurse-family relationship (Wong et al., 2022). Nurses further noted that to create this relationship one must be aware and respectful of the diverse backgrounds of all family members, as well as their values and believes when providing care. This is essential for a beneficial HSCT treatment process, as family members are in the hospital for several month thus, benefit from positive relationships with multiple healthcare providers. Many of the above support group interventions allowed for the family members to voice their values and beliefs, while creating a positive healthcare provider and family member relationship (Holochwost et al., 2020; Lindwall et al., 2014; Liu et al., 2020; Manne et al., 2016; Racine et al., 2018; Sands et al., 2017; Streisand et al., 2000). The core concepts of family-centered care offer valuable support to family members, as they navigate an aggressive and intensive treatment journey with their child. Although, the interventions reviewed did not include all four concepts in their approach, it is evident that each IPFCC concept of family-centred care provides benefits to family members while their child is being hospitalized. It should also be noted that each core concept has the potential to support and enhance the others, resulting in improved care overall. For example, dignity and respect can promote positive relationships that support efficient collaboration, information sharing, and participation.
Future Research
As described above, the application of any of the family-centred care core concepts can benefit family and patient care. Yet, these concepts also intertwine to strengthen the care being delivered. Future research should strive to develop supportive interventions that incorporate and evaluate all four core concepts of IPFCC in their approach to care in the context of HSCT. Family members of a child treated with HSCT require not only assistance in supporting their psychological well-being with dignity and respect, and participation when caring for their child, but also need consistent communication and involvement through collaboration and information sharing. Fauer et al. (2019) suggested blending both collaboration and information sharing aspects of the BMT Roadmap with the development of families’ coping and problem-solving skills. This integration would provide the BMT Roadmap intervention with the additional principles of dignity and respect and participation, thus encompassing all four IPFCC family-centred care core concepts. Given the evidence on the benefits of the BMT Roadmap for these family members, future research can build on this foundational work by designing similar interventions that provide all four core concepts of family-centred care.
Nursing Implications
Studies have shown that HSCT significantly impacts family members and patients’ well-being, physical and psychological health (Kearney et al., 2015; Packman et al., 2010; Riva et al., 2014). With a lack of support, family members struggle to cope with their increasing levels of anxiety, depression, and post-traumatic stress (Packman et al., 2010). This is concerning because family members’ diminished psychological well-being can be detrimental to their child’s quality of life (Kearney et al., 2015). This scoping review sheds light on the importance of ensuring that nursing care is approached with the four IPFCC core concepts in mind. As noted previously, nurses can integrate these core concepts into their care by creating positive rapport with the family members by actively listening and honoring the family members diverse values and beliefs (Wong et al., 2022). Through these positive relationships, they can then provide and share personalized information with the family members to empower them and reduce their anxieties. Nurses can also assist families in developing their caregiver role within the hospital setting by supporting them to participate and collaborate in their child’s care. By implementing these actions, which encompass all four IPFCC core concepts, nurses may improve the HSCT treatment process by improving both the family members and patient’s psychological well-being and quality of life.
Limitations
The main limitation noted in this scoping review is the specificity of the question itself. Due to the question focusing on a specific treatment and population, the review had limited scope and evidence from which to make selections. Thus, there were limited data that could be collected and analyzed to address the scoping review question. Although it is a well recognized model, there was also limited data of the IPFCC model being implemented in pediatric hospitals themselves. Lastly, one reviewer conducted the literature search and review (PL), but the process was complemented by the assistance of an expert university librarian. Moreover, this work was carried out as part of a final graduate program scholarly project, ensuring supervision at every stage (MM, MR).
Very few interventions were identified thus, giving limited variability in their approach to family-centred care. In addition, findings were limited in their generalizability to assist implementation and change in practice. Further, studies were primarily conducted in the USA and were limited to those written in English. Study designs were primarily pilot RCTs including small samples, limiting the statistical power of the findings. Finally, the experiential perspective of HSCT family members when using these interventions was lacking.
CONCLUSION
The scoping review aimed to identify support interventions available to family members of children undergoing HSCT. The interventions identified in the literature were found to offer either psychological face-to-face or technology-based support. The face-to-face interventions exemplifying the dignity and respect, and participation principles to family-centred care, resulted in improvements in the psychological well-being, coping capabilities and quality of life of family members. In contrast, the technology-based intervention encompassing the information sharing and collaboration principles to family-centred care led to enhanced communication, psychological well-being, and quality of life of family members. Overall, the interventions showed promise in improving the psychological well-being and quality of life for both the family member and their child. The review also sheds light on the importance of all four core concepts of family-centred care in improving family members and patient’s well-being. Expanding the study and implementation of these interventions to multiple institutions while also improving them by incorporating all four components of family-centred care could lead to positive advancements in the holistic treatment process for children and their families going through hematopoietic stem cell transplant.
REFERENCES
- Chardon ML, Klages KL, Joffe NE, Pai AL. Family adjustment to pediatric hematopoietic stem cell transplant during COVID-19. Journal of Pediatric Psychology. 2021;46(10):1172–1181. doi: 10.1093/jpepsy/jsab092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Hospital Care and Institute for Patient-and Family-Centered Care. Patient-and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394–404. doi: 10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- Conway J, Johnson B, Edgman-Levitan S, Schlucter J, Ford D, Sodomka P, Simmons L. Partnering with patients and families to design a patient-and family-centered health care system: a roadmap for the future: A work in progress. Bethesda, MD: Institute for Family-Centered Care; 2006. [Google Scholar]
- Fauer AJ, Hoodin F, Lalonde L, Errickson J, Runaas L, Churay T, Seyedsalehi S, Seyedsalehi S, Warfield C, Chappell G, Brookshire K, Chaar D, Shin JY, Byrd M, Magenau J, Hanauer DA, Choi SW. Impact of a health information technology tool addressing information needs of caregivers of adult and pediatric hematopoietic stem cell transplantation patients. Supportive Care in Cancer. 2019;27(6):2103–2112. doi: 10.1007/s00520-018-4450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrad J. Health Sciences Literature Review Made Easy: The Matrix Method. 5th ed. Jones & Bartlett Learning; 2017. [Google Scholar]
- Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient-and family-centered care interventions in the ICU: A systematic review and meta-analysis. Critical care medicine. 2017;45(10):1751–1761. doi: 10.1097/CCM.0000000000002624. [DOI] [PubMed] [Google Scholar]
- Holochwost SJ, Robb SL, Henley AK, Stegenga K, Perkins SM, Russ KA, Jacob SA, Delgado D, Haase JE, Krater CM. Active music engagement and cortisol as an acute stress biomarker in young hematopoietic stem cell transplant patients and caregivers: Results of a single case design pilot study. Frontiers in Psychology. 2020;11:2865. doi: 10.3389/fpsyg.2020.587871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Patient- and Family-Centered Care. Patient- and Family-Centered Care. Institute for Patient-And Family-Centered Care; 2021. https://www.ipfcc.org/about/pfcc.html . [Google Scholar]
- Kearney JA, Salley CG, Muriel AC. Standards of psychosocial care for parents of children with cancer. Pediatric Blood & Cancer. 2015;62(S5):S632–S683. doi: 10.1002/pbc.25761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo DZ, Houtrow AJ, Arango P, Kuhlthau KA, Simmons JM, Neff JM. Family-centered care: Current applications and future directions in pediatric health care. Maternal and Child Health Journal. 2012;16(2):297–305. doi: 10.1007/s10995-011-0751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindwall JJ, Russell K, Huang Q, Zhang H, Vannatta K, Barrera M, Alderfer M, Phipps S. Adjustment in parents of children undergoing stem cell transplantation. Biology of Blood and Marrow Transplantation. 2014;20(4):543–548. doi: 10.1016/j.bbmt.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Wen Y, Weng P, Jaing T, Chen S. Effectiveness of a three-stage intervention in reducing caregiver distress during pediatric hematopoietic stem cell transplantation: A randomized controlled trial. Journal of Pediatric Oncology Nursing. 2020;37(6):377–389. doi: 10.1177/1043454220911358. [DOI] [PubMed] [Google Scholar]
- Manne S, Mee L, Bartell A, Sands S, Kashy DA. A randomized clinical trial of a parent-focused social-cognitive processing intervention for caregivers of children undergoing hematopoetic stem cell transplantation. Journal of Consulting and Clinical Psychology. 2016;84(5):389. doi: 10.1037/ccp0000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packman W, Weber S, Wallace J, Bugescu N. Psychological effects of hematopoietic SCT on pediatric patients, siblings and parents: A review. Bone Marrow Transplantation. 2010;45(7):1134–1146. doi: 10.1038/bmt.2010.74. [DOI] [PubMed] [Google Scholar]
- Racine NM, Smith A, Pelletier W, Scott-Lane L, Guilcher GM, Schulte F. Evaluation of a support group for parents of children hospitalized for cancer and hematopoietic stem cell transplantation. Social Work with Groups. 2018;41(4):276–290. [Google Scholar]
- Riva R, Forinder U, Arvidson J, Mellgren K, Toporski J, Winiarski J, Norberg AL. Patterns of psychological responses in parents of children that underwent stem cell transplantation. Psycho-oncology. 2014;23(11):1307–1313. doi: 10.1002/pon.3567. [DOI] [PubMed] [Google Scholar]
- Runaas L, Hanauer D, Maher M, Bischoff E, Fauer A, Hoang T, Munaco A, Sankaran R, Seyedsalehi S, Cohn A, An L, Tewari M, Choi SW. BMT roadmap: A user-centered design health information technology tool to promote patient-centered care in pediatric hematopoietic cell transplantation. Biology of Blood and Marrow Transplantation. 2017;23(5):813–819. doi: 10.1016/j.bbmt.2017.01.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvador Á, Crespo C, Barros L. The benefits of family-centered care for parental self-efficacy and psychological wellbeing in parents of children with cancer. Journal of Child and Family Studies. 2019;28:1926–1936. [Google Scholar]
- Sands SA, Mee L, Bartell A, Manne S, Devine KA, Savone M, Kashy DA. Group-based trajectory modeling of distress and well-being among caregivers of children undergoing hematopoetic stem cell transplant. Journal of Pediatric Psychology. 2017;42(3):283–295. doi: 10.1093/jpepsy/jsw064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SickKids. AboutKidsHealth: Blood and Marrow Transplant. 2020. https://www.aboutkidshealth.ca/BMT .
- Shields L, Pratt J, Hunter J. Family centred care: A review of qualitative studies. Journal of Clinical Nursing. 2006;15(10):1317–1323. doi: 10.1111/j.1365-2702.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- Streisand R, Rodrigue JR, Houck C, Graham-Pole J, Berlant N. Brief report: Parents of children undergoing bone marrow transplantation: Documenting stress and piloting a psychological intervention program. Journal of Pediatric Psychology. 2000;25(5):331–337. doi: 10.1093/jpepsy/25.5.331. [DOI] [PubMed] [Google Scholar]
- Uhl T, Fisher K, Docherty SL, Brandon DH. Insights into patient and family-centered care through the hospital experiences of parents. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2013;42(1):121–131. doi: 10.1111/1552-6909.12001. [DOI] [PubMed] [Google Scholar]
- Wong CL, Phiri PG, Chan CW, Tse M. Nurses’ and families’ perceptions and practices and factors influencing the implementation of family-centred care for hospitalised children and their families. Journal of Clinical Nursing. 2023;32(17–18):6662–6676. doi: 10.1111/jocn.16740. [DOI] [PubMed] [Google Scholar]