Abstract
Background:
Anterior cruciate ligament (ACL) injuries are among the most common injuries in adolescent athletes and result in significant financial and physical morbidity. Evidence-based programs designed to prevent ACL injury are effective. However, their adoption remains low. We sought to evaluate the awareness, evidence-based implementation, and barriers to implementation of ACL injury prevention programs (ACL-IPP) among youth athletic coaches.
Hypothesis:
Higher education level of the coach, higher level of training, number of teams coached, and coaching female teams would be associated with ACL-IPP implementation.
Study Design:
Cross-sectional survey
Level of Evidence:
Level 4.
Methods:
We conducted an email survey sent to all 63 school districts within Section VI of the New York State Public High School Athletic Association. We employed descriptive statistics and tests of correlation to identify factors associated with ACL-IPP implementation.
Results:
A total of 73% of coaches said they were aware of ACL-IPP, and only 12% of coaches implemented ACL-IPP according to best evidence. Coaches of higher competitive levels were more likely to adopt ACL-IPP (P = 0.01), more likely to use them multiple times per week (P = 0.03), and for ≥1 seasons (P = 0.02). Coaches of multiple teams were more likely to adopt ACL-IPP (P = 0.01). There were no differences in evidence-based implementation of ACL-IPP with gender coached or level of education of the coach.
Conclusion:
Overall awareness, adoption, and evidence-based implementation of ACL-IPP remain low. These results suggest that coaches at higher levels of play and multiple teams tend to use ACL-IPP more often. Gender coached and level of education do not appear to be associated with awareness or implementation.
Clinical Relevance:
Evidence-based ACL-IPP implementation remains low. Targeting coaches of younger athletes and fewer teams with local outreach programs and ACL-IPP may increase the implementation of ACL-IPP.
Keywords: anterior cruciate ligament, youth sports, injury prevention
Tears of the ACL occur in approximately 69 per 100,000 person-years annually, and approximately 200,000 ACL reconstruction surgeries are performed annually in the United States.11,21 Adolescents between the ages of 16 and 18 years are at increased risk for these injuries and, when injured, are at a heightened risk to experience long-term consequences. 11 ACL injuries result in significant time missed from sports and school, and result in considerable economic burden of acute and future health care costs. 11
Up to 78% of ACL injuries occur as a result of noncontact mechanisms such as twisting, cutting, or pivoting. 15 Female athletes are at a particularly high risk of sustaining ACL injuries as a result of a noncontact mechanism. The trend of increased female athlete participation in organized sports since the introduction of Title IX has been accompanied by an increased in annual incidence of ACL injuries among high school and college athletes. 4 Injury rates in these populations have increased despite significant advances in ACL injury prevention research demonstrating the ability to reduce the rates of noncontact ACL injuries in select groups by ≥50%.1,7,10,12
Many evidence-based ACL injury prevention programs (ACL-IPP) exist and typically include strengthening of the posterior chain musculature, core strengthening, general flexibility, and integrative neuromuscular training (NMT).7,8,10,19,22 Injury prevention programs should include 20-minute sessions, ≥3 times per week, 24 and include 4 to 6 weeks of preseason training.1,6 Despite the wealth of individual studies and pooled data reports regarding evidence-based use of ACL-IPP,12,19,20,24-26 ACL injuries still remain among the most common knee injuries in youth athletes.4,27 We believe this may be caused by a translational gap in reach, adoption, implementation, and maintenance of ACL-IPP, especially among younger and less “elite” teams. 25
Though ACL-IPPs may be effective in reducing the risk of ACL rupture, little has been reported on the actual prevalence of their adoption and implementation in youth sports. While efficacy is important, the actual willingness and ability for coaches to use these programs is necessary for these programs to work. O’Brien and Finch 16 laid out in their 2014 systematic review of interventional trials of injury prevention exercise programs (IPEP) how most of the current literature has been focused on efficacy, with only a small number of papers were focused on other factors included in the RE-AIM framework (Reach, Efficacy, Adoption, Implementation, and Maintenance). In their review, they highlight the necessity to understand the intended audience to promote widespread adoption. 16 In another paper, they also identified high agreement among coaches and physical therapist regarding the necessity for IPEPs like FIFA 11+, yet found relatively low implementation and maintenance rates. This low level of use was attributed largely to lack of variation, progression, and the need for more challenging content according to the respondents. 17
We sought to describe the current barriers to the reach, adoption, and implementation of ACL-IPP among youth athlete coaches. In this study, we surveyed coaches regarding their current awareness of ACL-IPP, whether they adopted ACL-IPP, and how well they were able to implement them according to current evidence-based standards. In addition, we aimed to describe the characteristics of coaches who are more likely to use ACL-IPP. We hypothesized that there would be a high rate (ie, >66% of respondents) of awareness and adoption of ACL-IPP, but a relatively low rate (<50% of coaches reporting awareness and adoption of ACL-IPP) of evidence-based implementation (heretofore referred to as implementation). We further hypothesized that coaches who had higher educational level and higher physical training level, coached multiple teams, and coached female athlete-only teams would be more likely to adopt ACL-IPP strategies, and do so in a manner that best aligns with current injury prevention guidelines.
Methods
We conducted a survey of all school districts within Section VI of the New York State Public High School Athletic Association (NYSPHSAA-VI), representing 63 school districts, in the summer of 2021. An email survey using Google Forms was sent to all athletic directors within NYSPHSAA-VI, asking them to distribute the survey to all coaches within their school district. The survey questions and answer choices are presented in Table 1. Coaches were asked to respond within 1 month of receipt. Two weeks after the initial participation request, a reminder email was sent to the Athletic Directors for distribution among their school district with the included response deadline. Coaches of any level of play (eg, Modified/Middle School, Junior Varsity, Varsity, College, and Club) and gender were invited to participate. Distribution by each athletic director was voluntary, as was the participation by coaches who received the survey. We were, therefore, unable to directly quantify how many coaches received this survey. Coaches were asked at the end of the survey to list the names of the teams they coach to determine the number of teams they coached and to determine whether they were any duplicate responses for teams. A response that was determined to be from the same team was kept if the coach reported working with other, unique team. The coach with no unique teams or no other teams coached in this situation has his/her answers assigned to the duplicate team in question. In this case, the coach’s responses were counted only for the unique teams he or she was coaching. If a duplicate response was the result of 2 coaches reporting only 1 team, then the first response received was kept and the second was not recorded. Erroneously entered data, such as answering a question with the qualifier “if yes to the question above. . .,” and the respondent had answered “no” to the previous question were omitted. Responses were also omitted if the discipline of sport was considered to be low risk for ACL-IPP by the authors. Disciplines excluded from our analysis include swimming and diving, cross country, track and field, golf, bowling, color guard, air rifle, and bowling. A response from a coach reporting multiple disciplines was included if they coached ≥1 moderate-to-high risk discipline. After reviewing responses for duplicate and err1ous answers, the data were entered into Microsoft Excel as deidentified, numeric responses where appropriate.
Table 1.
Individual survey questions and answer choices
| Question | Answer |
|---|---|
| 1. Are you aware that there are specific exercises that reduce the risk of ACL injury? | A. Yes B. No |
| 2. Do you routinely use ACL injury-specific exercises in your practices? | A. Yes B. No |
| 3. How long have you been using ACL injury prevention exercises in your practices? | A. Less than 1 season B. 1 season C. Multiple seasons D. I do not use ACL injury prevention exercises in my practices |
| 4. Do you have your athletes perform ACL injury prevention exercises prior to the start of the season? | A. Yes B. No |
| 5. If YES to the prior question, how far in advance of the beginning of the season do you advise the start performing these exercises? | A. 2 weeks or less B. Between 2 and 6 weeks C. 6 weeks or more D. I do not use ACL injury prevention exercises in my practices |
| 6. How often are you using ACL injury prevention exercises while in season? | A. A few times per season B. Once per week C. 2-3 times per week D. Every practice, or nearly every practice E. I do not use ACL injury prevention exercises in my practices |
| 7. How did you first learn about ACL injury prevention exercises? | A. Open-ended, short answer |
| 8. If you are NOT currently using ACL injury prevention exercises, what barriers prevent you from using these exercises? | A. Requires too much time B. Lack of resources/equipment C. I do not feel as if I am properly trained to use these D. I do not feel that it is worth the effort. E. Other, please explain |
| 9. What level of athletic do you coach? Please select all that apply. | A. Grade school E. High school (Club)B. Modified (Middle school) F. College (NCAA) C. High school (Freshman, or JV) G. College (Club) D. High school (Varsity) H. Premier or Elite-level youth club |
| 10. What gender athletes do you coach? | A. Males only B. Females only C. Both males and females |
| 11. What is your highest level of education? | A. High school or equivalent (ie GED) B. Associate degree C. Bachelor’s degree D. Master’s degree E. Doctorate or other professional degree |
| 12. What level of training do you have that directly pertains to physical education or athletic performance? | A. NY State Coaching Class B. Athletic Trainer Certification (ATC) C. Associate’s degree D. Bachelor’s degree E. Graduate’s degree or other professional degree |
| 13. What sports disciplines do you coach? Check all that apply. | A. Soccer A. Rugby B. Lacrosse B. Basketball C. Hockey C. Swimming D. Football D. Wrestling E. Volleyball E. Baseball F. Track and field F. Softball G. Tennis G. Other, please specifyH. Field hocket |
| 14. What team(s) do you coach (ie, Springville Men’s Soccer) example changed for anonymous review | A. Open-ended, short answer |
JV, Junior Varsity.
Basic descriptive statistics were applied to describe awareness, adoption, and implementation of ACL-IPP. We then used comparative statistics to identify coaching characteristics and their association with awareness, adoption, and implementation. First, we compared coaches who supervised younger, less trained athletes (grade, middle, junior varsity), with older and/or more elite athletes (varsity, club, collegiate) or a combination of the 2. Second, we compared coaches who supervised male, female, or both male and female teams. We also included number of teams coached in our secondary analysis. When comparing appropriateness among these groups, we defined implementation as performing the exercises at least 2 to 3 times per week and ≥6 weeks before the start of the season. Chi-squared tests were used to compare all binary and categorical responses and a P value <0.05 indicated statistically significant differences.
This study was reviewed approved by the University at Buffalo institutional review board and noncommittee review. It was determined that the research is exempt according 45 CFR Part 46.104
Results
Of the 171 responses to our survey received, 21 were duplicate responses and therefore omitted. Another 24 responses were not included on the basis of low-risk for ACL injury (7 for swimming and diving, 14 for cross country or track and field, 1 each for bowling, air rifle, and golf). The remainder of the responses included at least 1 or more of the following disciplines: soccer, volleyball, basketball, gymnastics, lacrosse, field hockey, cheer, ice hockey, tennis, baseball, and softball. We did not receive any responses from coaches of only wrestling or rugby although these were included among coaches of multiple team disciplines. As a result, 126 individual coaches of unique teams were included in our final analysis. This corresponded to 23 individual school districts among the 63 school districts within NYSPHSAA-VI. This represents a 36.5% response rate based on school districts alone. The level of play and gender of athlete coached is described in Table 2. Varsity, Elite Club, and/or College coaches made up the largest group of coaches (42.1%), with those coaching Grade School, Modified (ie, Middle School), and/or Junior Varsity making up (27.8%) of the responses and those coaching a mix of the 2 groups making up the remainder (30.1%). Roughly one-third of coaches trained male-only teams (30.2%), with the rest coaching female-only teams (32.5%) or a combination of male and female teams each (37.3%). As this survey contains many “If YES, to the previous question,” prompt, therefore, narrowing down the number of respondents to later questions, we have represented this attritional effect in Figure 1.
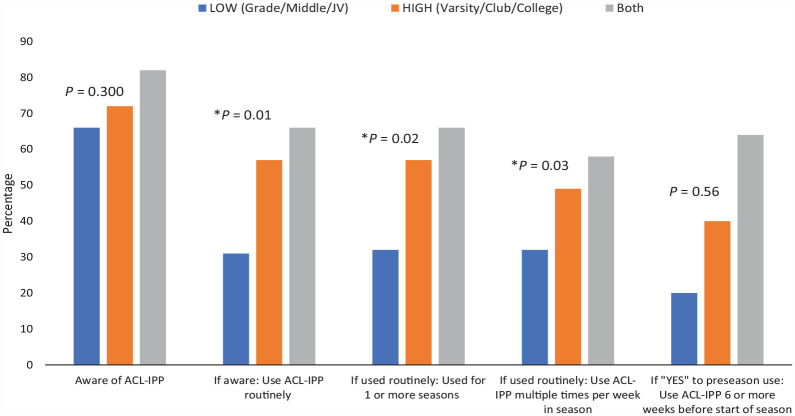
Figure 1.
Awareness, adoption, and implementation of ACL-IPP survey responses. ACL-IPP, ACL injury prevention programs.
Table 2.
Level of play and gender coached, among coaches, N = 126
| Level of Play | N (%) | Gender Coached | N (%) |
|---|---|---|---|
| Low (Grade, Modified, JV) | 35 (27.8) | Male | 38 (30.2) |
| High (Varsity, Elite Club, College) | 53 (42.1) | Female | 41 (32.5) |
| Both | 38 (30.1) | Both | 47 (37.3) |
JV, Junior Varsity.
Awareness, Adoption, and Implementation of ACL-IPP
Of the 126 coaches who participated in the survey, 73% (n = 92) said they were aware of specific exercises for ACL injury prevention. Overall, only 52.4% (n = 66) of the total survey respondents said they used ACL-IPP routinely. Of those using ACL-IPP exercises routinely, 89% (n = 59) performed these exercises 2 to 3 times per week or more. In addition, only 55% (n = 36 of 66) of coaches using ACL-IPP routinely said they employed these exercises in the preseason, with 44% of this subgroup (n = 16 of 36) reporting they used ACL-IPP >6 weeks in advance. When defining evidence-based use of ACL-IPP as an in-season frequency of greater ≥2 times per week and ≥6 weeks before the beginning of competitive play, we found that only 12% (n = 16 of 126) of those surveyed, or 17% of those reporting awareness of these exercises (n = 16 of 126) were using evidence-based best ACL-IPP practices. These results are illustrated in Figure 1.
Factors Associated With Awareness, Adoption, and Implementation of ACL-IPP
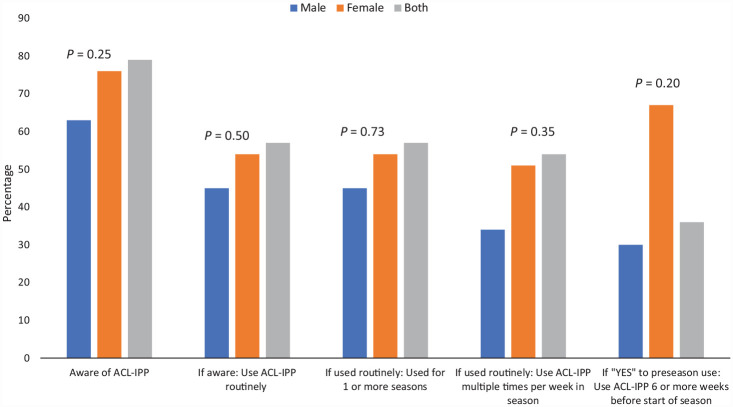
Neither gender coached nor level of competition coached were associated with differences in awareness of ACL-IPP programs (P = 0.30 for Skill Level, P = 0.24 for Gender Coached). Based on skill level coached, we found that coaches of Junior Varsity athletes or below were less likely than Varsity level and above or coaches of both levels to adopt ACL-IPP while in season with their teams (JV 31%; Varsity 57%; Both 66%; P = 0.01), less likely to implement them multiple times per week (JV 32%; Varsity 49%; Both 58%; P = 0.01), and for >1 season (JV 23%; Varsity 53%; Both 58%; P = 0.02). Our results also suggested a trend towards significance for coaches of more skilled athletes to be more likely to use preseason ACL-IPP (P = 0.06); however, there was no difference when the question was specified to query how far in advanced in the preseason ACL-IPP was used (P = 0.5). However, these results are difficult to interpret due to the relatively low numbers at this point in the survey. Only 36 total respondents out of the original 126 reported using preseason ACL-IPP at all. Our results according to skill level coaches are represented in Figure 2.
Figure 2.
ACL-IPP awareness, adoption, and implementation by level coached. ACL-IPP, ACL injury prevention programs; JV, Junior Varsity.
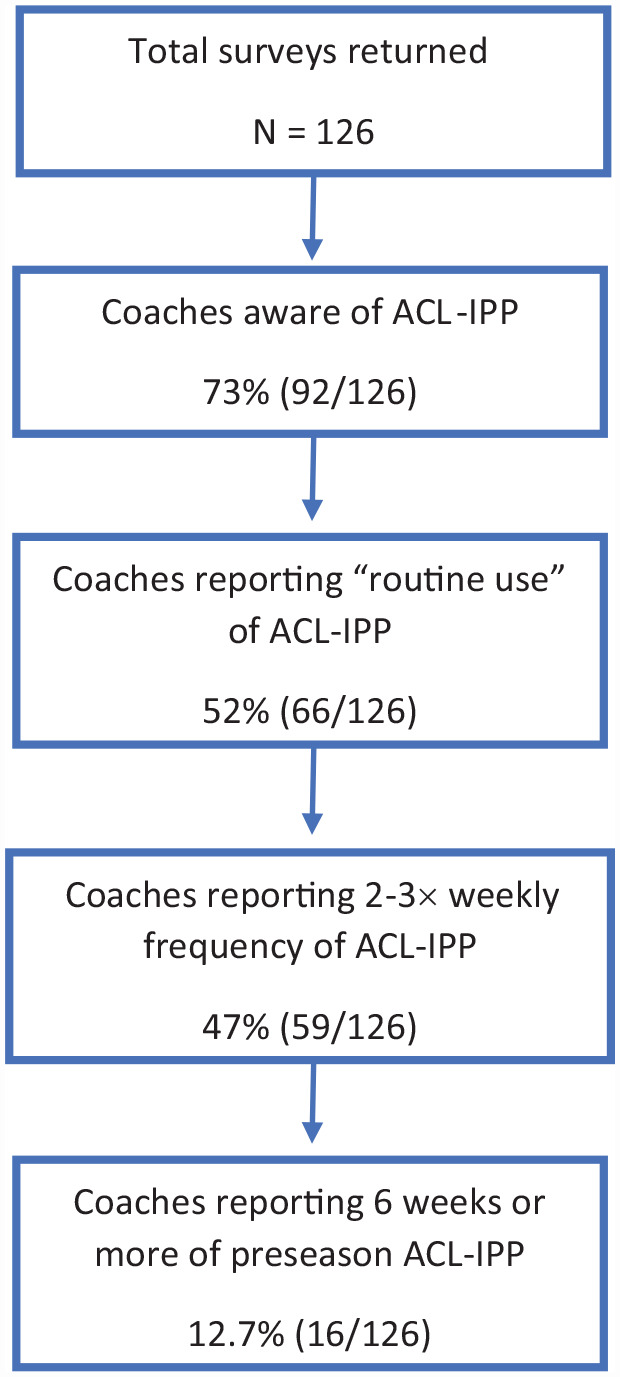
When adoption and implementation was compared against gender coached, we were unable to demonstrate any association. This included no differences in adoption (Yes, to “routine use”) (P = 0.49), number of seasons used (P = 0.72), preseason use (P = 0.93), and frequency of use (P = 0.35). Our results according to gender coached are represented in Figure 3. However, as stated above, the relatively low numbers of responses affirming preseason ACL-IPP may have affected our ability to find a difference in preseason use. Only 8 coaches of female-only teams, 3 male-only, and 5 coaches of male and female teams reported using ACL-IPP >6 weeks in advance of competitive play.
Figure 3.
ACL-IPP awareness, adoption, and implementation by gender coached. ACL-IPP, ACL injury prevention programs.
In addition, we found that the highest level of education and the highest level of physical-education specific training was not associated with the adoption of ACL-IPP strategies (P = 0.91, and P = 0.86, respectively). While 71% of our respondents indicated that their highest level of education was a master’s degree (90 of 126), a majority (75%, 89 of 118) of respondents indicated their highest level of physical education-specific training was limited to state-mandated requirements (New York State Coaching Class Certification).
Lastly, we evaluated the difference in adoption (“Yes” to “Routine Use”) based on number of individual teams coached. We used the open-ended question “what team(s) do you coach” as a correlate for number of teams coached (Table 1, Question 14). We compared adoption against 1, 2, and ≥3 teams coached. We found that coaches who coached multiple teams were more likely to adopt ACL-IPP (P = 0.01).
Barriers and Resources for ACL-IPP Adoption
At the end of the survey, coaches were asked to give more detail why they were or were not using ACL-IPP. The first question asked coaches what barrier prevented them from using these programs if they were not using ACL-IPP. These answers were divided into 5 categories: time, resources, appropriate training, effort, or “other.” Coaches were asked to select every response that applied. All the “other” responses (21%) were variations of “I already use ACL-IPP.” The most cited reasons included “lack of training” (63.2%), and “lack of resources” (15.8%). No coaches responded that time or effort were significant barrier to ACL-IPP adoption. The second question asked coaches who had adopted ACL-IPP to comment on where they learned about these programs. This was an open-ended question. These responses were divided post hoc into 4 categories: Athletic Trainer Certification (ATC) or other Allied Medical Professional, structure course, personal research, or due to a personal experience with an ACL injury or that of one of their athletes. The most common responses were ATC or other medical professional (37%), followed by structured course (29%), personal research (21%), and personal/player injury (13%).
Discussion
Our results confirm our primary hypothesis that a significant gap exists between the awareness and implementation of ACL-IPP. Of the 73% (n = 92 of 126) of coaches in our study population who were aware of ACL-IPP, only 72% (n = 66 of 92) adopted ACL-IPP. Our overall rate of ACL-IPP awareness and adoption rates of 73% and 52% is similar to 2018 results by Wilke et al. 28 However, these results are contrasted by the 2013 study of Utah female soccer teams and a 2016 study of Oregon soccer and basketball coaches, which reported only 19.8% and 21% implementation rate of ACL-IPP.9,14 The latter of these 2 studies was specifically targeted in an area where widespread outreach regarding ACL-IPP was not present, and found that only 52% of their respondents reported awareness of ACL-IPP. These differences in awareness and implementation may represent improving reach of ACL-IPP over the last decade but may also reflect the differences in interpretation of “adoption” or “routine use.”
Further compounding this problem, we found that coaches who had adopted ACL-IPP may not be using the exercises in accordance with evidence-based recommendations (ie, implementing). We found that 11% (n = 7 of 66) of coaches who adopted ACL-IPP only have their teams performing these exercises once per week or less. This is likely not enough to provide any meaningful benefit.10,24 In addition, about half (n = 36 of 66) of coaches who indicated that they had adopted ACL-IPP reported using ACL-IPP during preseason training. However, only 44% (16 of 36) of these coaches actually begin preseason ACL-IPP early enough to develop neuromuscular adaptations for ACL-IPP. 6 In our survey, only 12% of respondents and 17% of those reporting awareness of ACL-IPP successfully implemented it.
We found that coaching fewer teams and coaching younger or less skilled athletes was negatively correlated with awareness and adoption of ACL-IPP. Similarly, Sugimoto et al 23 found that high school coaches were more compliant to an NMT program than middle school coaches. This is likely explained by increased exposure to ACL injuries among athletes and increased access to resources and training opportunities specific to ACL-IPP. However, these coaches are likely intervening near the end or beyond the point of peak sensitivity. In a meta-analysis of 18 studies comprising >27,000 participants, Petushek et al 19 demonstrated that high school and middle school-aged athletes demonstrated a larger reduction in injury incidence compared with college- and professional-level athletes. In addition, the studies in this meta-analysis included training loads on average of 24 minutes and 2.5 times per week, consistent with our previously suggested training loads. Furthermore, in their meta-analysis, Sugimoto et al 24 found a significantly larger effect when ACL-IPP programs were used with younger teens (14-18 years) when compared with older teens (19-20 years). The authors also included a subgroup of athletes aged <14 years. Due to the relatively small number in this group, they were unable to find a statistically significant reduction in injury. However, this group also did show the lowest odds ratio for injury, leading the authors to conclude that earlier intervention (<14 years) may have benefit.
Female athletes are at a higher risk for ACL injury when compared with male athletes. 2 Knowing this, we would expect coaches of female athletes to be more likely to adopt and implement ACL-IPP as it is of higher value to their athletes. However, our study findings do not suggest differences in injury prevention between coaches of female, male, or both genders. This disconnect may either be due to a of lack of knowledge that females are at higher risk of injury, lack of knowledge of the increased effectiveness of ACL-IPP for female athletes, or the perception that the benefits of ACL-IPP are not sufficient to offset the costs of implementing ACL-IPP.
The level of the coach’s education in this study did not appear to have significant association with ACL-IPP adoption or implementation, even when we controlled for physical education specific qualifications. This may be explained by perceived benefit of ACL-IPP or other barriers preventing coaches from applying these exercises. In addition, we found a large discrepancy between the answer to the questions, “what is your highest level of education,” and “what level of training do you have that pertains directly to physical education.” That is, 90 of the 126 responses to the former question were master’s degrees, whereas 89 of 118 responses to the latter question reported high school level education only. This result highlights that coaches of youth athletes are most often teachers who have obtained professional degrees in education, and receive most, if not all, of their physical and health science education from state and national licensure courses. New York State (NYS) requires coaches to take ≥1 National Federation of State High School Associations (NFHS) sport-specific course in addition to a state-approved coaching course. Neither the state course nor the NFHS sports-specific courses include ACL-IPP education. Though the NFHS does offer a free 1-hour course in ACL-IPP, this is not required for coach to obtain licensure. This contrasts with the NYS requirements for concussion training. This finding suggests additional community outreach and education to youth athletic teams to reach these coaches and the parents of youth athletes would be beneficial.
We asked coaches who reported not using ACL-IPP routinely what barriers prevented them from implementing ACL-IPP. Among the options were time, effort, lack of resources, lack of appropriate training, or an open-ended “other” category. The most common response was lack of appropriate training followed by lack of resources. No coach responded that time or effort were significant barriers to implementation. Similar to lack of resources, Dix et al 5 found that, among women’s NCAA soccer coaches, cost was cited as the largest barrier to implementation of ACL-IPP. The authors mentioned that coaches also indicated that they believed ACL-IPP was the responsibility of ancillary staff such as Athletic Trainers and the coaches agreed that they would be more likely to implement ACL-IP if there were cost-free options. 5 These findings likely explain why we found that coaches of younger teams or at lower levels of competition were less likely to implement ACL-IPP as they would be less likely to have support staff such as Athletic Trainers. This is in contrast to Petersen et al, 18 as coaches in their study were concerned about exercises diverting training time away from the athletes. It may be encouraging that most coaches who are not currently using ACL-IPP appear to be enthusiastic about injury prevention but are not receiving the appropriate information to allow them to easily implement this. While there are many training programs and resources available commercially for ACL-IPP training, this sort of training may be cost-prohibitive to coaches of youth athletes who are the most responsive to this sort of training.
There are far more nonelite athletes than there are elite athletes who are at risk of ACL injury, simply by virtue of number of athletes who fall into each category. Programs such as FIFA 11+ have been developed with the ACL-IPP literature in mind to provide cost free and easy-to-use ACL-IPP exercises that do not require specialized equipment. However, although the concepts taught in FIFA 11+ can be generalized to other athletic disciplines, it may not appear this way to coaches of other disciplines as described by O’Brien and Finch.16,17
Limitations
Nonresponse bias was the most significant limitation in this study. Only 24 of the 63 school districts had ≥1 coach respond to our survey. In addition, we did not collect demographic data from the participants such as age, gender, or years of experience, or if the coach was a head coach or assistant coach. Furthermore, we were unable to reliably estimate how many individual teams received the survey. This study included youth teams as well as nonprofessional adult teams and did show a significantly higher use among those coaching youth teams.
Our study did not examine maintenance of ACL-IPP. Although 86% of coaches using ACL-IPP reported using it for multiple seasons, we were not able to differentiate this any further with our design. This is important, however, as maintenance has been indicated as a principal factor in the lack of effective translation of ACL-IPP from research into actual practice.3,13
While our survey reach included a relatively diverse selection of school districts within the Western New York region of NYS, this study is nevertheless limited to a specific geographical location and our results may not be generalizable to other populations.
Conclusion
Despite the large body of literature supporting ACL-IPP, its adoption and implementation using evidence-based guidelines in youth athletic populations most at risk are still low. Emphasis should be placed on providing coaches are parents with ACL-IPP tools and instruction that does not require ancillary staff. In addition, analyzing other characteristics associated with use of ACL-IPP such as sport discipline, school funding, and locoregional differences in practices may be helpful to better target at-risk populations.
Footnotes
The following author declared potential conflicts of interest: L.J.B. has received a grant from NIH.
References
- 1. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17(8):859-879. [DOI] [PubMed] [Google Scholar]
- 2. Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23(6):694-701. [DOI] [PubMed] [Google Scholar]
- 3. Arundale AJH, Silvers-Granelli HJ, Myklebust G. ACL injury prevention: where have we come from and where are we going? J Orthop Res. 2022;40(1):43-54. [DOI] [PubMed] [Google Scholar]
- 4. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3):e20161877. [DOI] [PubMed] [Google Scholar]
- 5. Dix C, Logerstedt D, Arundale A, Snyder-Mackler L. Perceived barriers to implementation of injury prevention programs among collegiate women’s soccer coaches. J Sci Med Sport. 2021;24(4):352-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476-1483. [DOI] [PubMed] [Google Scholar]
- 7. Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27(6):699-706. [DOI] [PubMed] [Google Scholar]
- 8. Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. Mechanisms, prediction, and prevention of ACL injuries: Cut risk with three sharpened and validated tools. J Orthop Res. 2016;34(11):1843-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Joy EA, Taylor JR, Novak MA, Chen M, Fink BP, Porucznik CA. Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches. J Strength Condit Res. 2013;27(8):2263-2269. [DOI] [PubMed] [Google Scholar]
- 10. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003-1010. [DOI] [PubMed] [Google Scholar]
- 11. Mather RC, III, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751-1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41(1):203-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Myklebust G, Skjølberg A, Bahr R. ACL injury incidence in female handball 10 years after the Norwegian ACL prevention study: important lessons learned. Br J Sports Med. 2013;47(8):476-479. [DOI] [PubMed] [Google Scholar]
- 14. Norcross MF, Johnson ST, Bovbjerg VE, Koester MC, Hoffman MA. Factors influencing high school coaches’ adoption of injury prevention programs. J Sci Med Sport. 2016;19(4):299-304. [DOI] [PubMed] [Google Scholar]
- 15. Noyes FR, Mooar PA, Matthews DS, Butler DL. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983;65(2):154-162. [DOI] [PubMed] [Google Scholar]
- 16. O’Brien J, Finch CF. The implementation of musculoskeletal injury-prevention exercise programmes in team ball sports: a systematic review employing the RE-AIM framework. Sports Med. 2014;44(9):1305-1318. [DOI] [PubMed] [Google Scholar]
- 17. O’Brien J, Finch CF. Injury prevention exercise programmes in professional youth soccer: understanding the perceptions of programme deliverers. BMJ Open Sport Exerc Med. 2016;2(1):e000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125(9):614-621. [DOI] [PubMed] [Google Scholar]
- 19. Petushek EJ, Sugimoto D, Stoolmiller M, Smith G, Myer GD. Evidence-based best-practice guidelines for preventing anterior cruciate ligament injuries in young female athletes: a systematic review and meta-analysis. Am J Sports Med. 2019;47(7):1744-1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320-1325.e6. [DOI] [PubMed] [Google Scholar]
- 21. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502-1507. [DOI] [PubMed] [Google Scholar]
- 22. Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football–a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18(5):605-614. [DOI] [PubMed] [Google Scholar]
- 23. Sugimoto D, Mattacola CG, Bush HM, et al. Preventive neuromuscular training for young female athletes: comparison of coach and athlete compliance rates. J Athl Train. 2017;52(1):58-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sugimoto D, Myer GD, Barber Foss KD, Pepin MJ, Micheli LJ, Hewett TE. Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis. Br J Sports Med. 2016;50(20):1259-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sugimoto D, Myer GD, Foss KD, Hewett TE. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med. 2015;49(5):282-289. [DOI] [PubMed] [Google Scholar]
- 27. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilke J, Niederer D, Vogt L, Banzer W. Is the message getting through? Awareness and use of the 11+ injury prevention programme in amateur level football clubs. PLoS One. 2018;13(4):e0195998. [DOI] [PMC free article] [PubMed] [Google Scholar]