Abstract
Background:
Long-distance running is a popular form of cardiovascular exercise with many well-described health benefits, from improving heart health to the management of obesity, diabetes, and mental illness. The impact of long-distance running on joint health in recreational runners, however, remains inconclusive.
Hypothesis:
The prevalence of osteoarthritis in runners is not associated with an athlete’s running-related history, including the number of marathons completed, cumulative years of running, average weekly mileage, and average running pace.
Study Design:
Prospective cohort study.
Level of Evidence:
Level 3.
Methods:
A survey was distributed to all participants registered for the 2019 or 2021 Chicago marathon (n = 37,917). Surveys collected runner demographics and assessed for hip/knee pain, osteoarthritis, family history, surgical history, and running-related history. Running history included the number of marathons run, number of years running, average running pace, and average weekly mileage. The overall prevalence of osteoarthritis was identified, and a multivariable logistic regression model was used to identify variables associated with the presence of hip and/or knee osteoarthritis.
Results:
Surveys were completed by 3804 participants (response rate of 10.0%). The mean age was 43.9 years (range, 18-83 years) and participants had completed on average 9.5 marathons (median, 5 marathons; range, 1-664 marathons). The prevalence of hip and/or knee arthritis was 7.3%. A history of hip/knee injuries or surgery, advancing age, family history, and body mass index (BMI) were risk factors for arthritis. Cumulative number of years running, number of marathons completed, weekly mileage, and mean running pace were not significant predictors for arthritis. The majority (94.2%) of runners planned to run another marathon, despite 24.2% of all participants being told by a physician to do otherwise.
Conclusion:
From this largest surveyed group of marathon runners, the most significant risk factors for developing hip or knee arthritis were age, BMI, previous injury or surgery, and family history. There was no identified association between cumulative running history and the risk for arthritis.
Keywords: hip and knee pain, long-distance running hip and knee arthritis, marathon running
Long-distance running is a popular pastime and form of exercise, with more than 1.1 million marathon participants globally in 2018. 5 The benefits of running and maintaining cardiovascular fitness are widely described, including for prevention of hypertension, obesity, type 2 diabetes, and mental illness.14,21,29,30 Although current dogma highlights arthritis as a potential adverse effect of long-term running, the cumulative effect of repetitive high-impact activities, such as long-distance running, has yet to be fully understood. 26 If running does increase lifetime risk of developing hip or knee arthritis, then current recommendations to avoid these activities are warranted. However, previous studies found mixed results: some identify a higher prevalence of arthritis among long-distance runners, and other studies find that running may lower arthritis risk.3,15,19,20,28 These inconsistencies lead many runners to query their healthcare providers about the impact of running on their joint health. 25
Previous studies investigating this relationship suffer from 2 related problems: small cohort sizes and a focus on elite-level atheltes.2,20,27 The literature lacks data from the broader, general population of runners. In the absence of these data, healthcare providers are forced to rely on inapplicable and underpowered evidence when counseling casual runners about the role of running in developing arthritis. Whereas typically, casual runners would be difficult to identify, large-scale, publicly accessible marathons concentrate this population in a single venue. The present study addresses this gap in the literature by surveying a large, cross-sectional cohort of runners who participated in a large-city marathon in the United States. We hypothesized that the prevalence of osteoarthritis in runners is not associated with a person’s running-related history, including the number of marathons completed, cumulative years of running, average weekly mileage, and average running pace.
Methods
Participants
An electronic survey was distributed to participants registered for the 2019 or 2021 Bank of America Chicago Marathon (n = 37,917) to collect information related to their hip and knee health and running history. By studying a large-city marathon, we hoped to capture a wide swath of runners, from beginners to high-volume marathon runners. The study was approved by the institutional review board at Northwestern University.
Questionnaire
The survey included 30 questions (Appendix) targeted at assessing demographic information, running history, and hip/knee health, with portions of the survey utilizing questions previously used in a study evaluating hip/knee health in runners. 20 Demographic information collected included age, sex, height, weight, country of? origin, and occupation. Running-related history included number of years running, average weekly mileage over the past year, average running pace during training runs, number of marathons completed (including ultramarathons), and participation with cross-training (ie, swimming, biking, or weight training) or with other sporting activities. Questions targeting joint health inquired about the occurrence of hip or knee pain over the past year that prevented running, a history of hip or knee injuries that required a break in running, family history of hip and/or knee arthritis, and surgical procedures performed on the hip or knee. The prevalence of hip or knee arthritis was assessed by asking participants “Have you ever been diagnosed by a doctor with hip or knee arthritis (worn out cartilage)?” This question was used by a previous study investigating the prevalence of arthritis in runners. 20 The authors designed the question based on epidemiological studies performed by the US National Center for Health Statistics targeted at assessing the prevalence of arthritis in the US population. Participants were also asked if a doctor had ever advised them to stop or reduce their running, whether they are still running at the time of questionnaire completion, and whether they plan to run another marathon.
Survey Administration
All potential participants were contacted by email for study recruitment, and responses were collected between November 1 and December 31, 2021. Study data were collected and managed using REDCap electronic data capture tools hosted at Northwestern University.6,7 Participation was on a voluntary basis, and all participants completed an informed consent before starting the survey. Multiple languages were available for the survey, including English, Spanish, and Mandarin Chinese. No identifiable data were collected with the surveys, and responses were only identified by participant identification number. Surveys were included in the final analysis only if all questions were completed; no partially completed surveys were included.
Statistical Analysis
Continuous variables were compared using independent-samples t tests. Dichotomous variables were compared using either chi-squared or Fisher exact tests depending on cell count. We estimated a unique multivariable logistic regression model for each of our outcomes of interest, hip and/or knee pain that prevented running and hip and/or knee arthritis. Multivariable analysis results are reported as odds ratios (ORs) with 95% CI. To address concerns for multiplate comparisons, a Bonferroni corrected a priori alpha level of 0.0042 was used to determine statistical significance. Analyses were performed by J.E.T. and M.J.H. using JMP Pro, Version 16.0, SAS Institute Inc, 1989-2021.
Results
Runner Demographics
Surveys were completed by 3804 participants. Surveys were partially completed by 187 participants; these were not included in the analysis. The average age was 43.9 years (range, 18-83 years), 52.2% were male, and the mean body mass index (BMI) was 23.8 kg/m2 (range, 15.5-42.6 kg/m2). Participants had been running for a mean of 14.7 years (range, 1-67 years) and ran a mean of 27.9 miles per week (median, 25 miles/week; range, 0-180 miles/week) at an average pace of 8 minutes and 52 seconds per mile during their training runs (Table 1).
Table 1.
Runner characteristics and prevalence of hip and/or knee pain and arthritis
| Demographic Characteristics | All Marathoners | Pain a | Arthritis b | ||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| n = 3804 | n = 1383 (36.4%) | n = 2421 (63.6%) | n = 277 (7.3%) | n = 3527 (92.7%) | |
| Age c | 43.9 ± 11.4 (18-83) | 42.3 ± 11.5 (18-77)* | 44.7 ± 11.2 (18-83) | 51.7 ± 10.8 (25-75)** | 43.2 ± 11.2 (18-83) |
| Sex d | |||||
| Male | 1984 (52.2) | 615 (44.5)* | 1369 (56.6) | 160 (57.8) | 1824 (51.7) |
| Female | 1816 (47.7) | 766 (55.4)* | 1050 (43.4) | 117 (42.2) | 1699 (48.2) |
| Prefer not to say | 4 (0.1) | 2 (0.1)* | 2 (0.1) | 0 (0.0) | 4 (0.0) |
| BMI, kg/m2 c | 23.8 ± 3.5 (15.5-42.6) | 24.0 ± 3.6 (16.2-42.6) | 23.7 ± 3.4 (15.5-42.3) | 24.5 ± 3.6 (17.3-36.6)** | 23.8 ± 3.5 (15.5-42.6) |
| No. of marathons c e | 9.5 ± 18.6 (1-664) | 7.5 ± 10.8 (1-120)* | 10.7 ± 21.7 (1-664) | 13.4 ± 20.2 (1-172)** | 9.2 ± 18.4 (1-664) |
| Duration of running, y c | 14.7 ± 11.0 (1-67) | 14.0 ± 10.3 (1-55)* | 15.2 ± 11.3 (1-67) | 19.4 ± 12.8 (1-55)** | 14.4 ± 10.7 (1-67) |
| Mileage, miles/week c | 27.9 ± 15.5 (0-180) | 25.7 ± 14.2 (0-130)* | 29.2 ± 16.0 (0-180) | 26.6 ± 14.3 (0-85) | 28.0 ± 15.5 (0-180) |
| Pace for training runs, average ± SD, minutes:seconds/mile | 8:52 ± 1:38 | 9:02 ± 1:42* | 8:46 ± 1:34 | 9:12 ± 1:45 | 8:50 ± 1:37 |
| Family history of hip/knee arthritis d | 993 (26.1) | 408 (29.5)* | 585 (24.2) | 123 (44.4)** | 870 (24.7) |
| History of hip/knee injury that prevented running d | 1892 (49.7) | 948 (68.6)* | 944 (39.0) | 238 (85.9)** | 1654 (46.9) |
| History of hip/knee surgery d | 413 (10.9) | 210 (15.2)* | 203 (8.4) | 130 (46.9)** | 283 (8.0) |
| Hip | 43 (1.1) | 27 (2.0) | 16 (0.7) | 13 (4.7) | 30 (0.9) |
| Knee | 370 (9.7) | 183 (13.2) | 187 (7.7) | 117 (42.2) | 253 (7.2) |
| Cross-train d | 2873 (75.5) | 1050 (75.9) | 1823 (75.3) | 214 (77.3) | 2659 (75.4) |
| Participate in other sports d | 1470 (38.6) | 532 (38.5) | 938 (38.7) | 107 (38.6) | 1363 (38.6) |
BMI, body mass index.
History of hip and/or knee pain within the past year that prevented running.
History of hip and/or knee arthritis.
Values are given as mean and SD, with range in parentheses.
Values are given as number of runners, with percentage in parentheses.
Includes ultramarathon distance events.
P < 0.05 compared with patients without hip/knee pain.
P < 0.05 compared with patients without hip/knee arthritis.
Marathons Completed
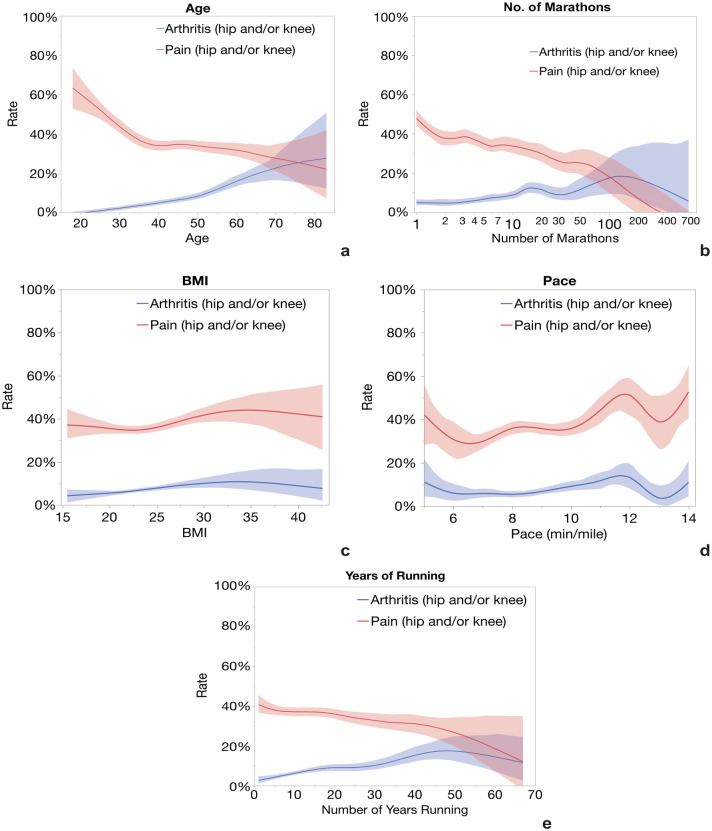
Participants completed an average of 9.5 marathons (median, 5 marathons; range, 1-664 marathons) (Table 1), although most of the runners (54.4%, n = 2070) had completed ≤5 marathons (Figure 1). This marathon was the first marathon for 650 (17.1%) participants and the >100th marathon for 25 (0.7%) participants.
Figure 1.
Distribution of participants by number of marathons completed.
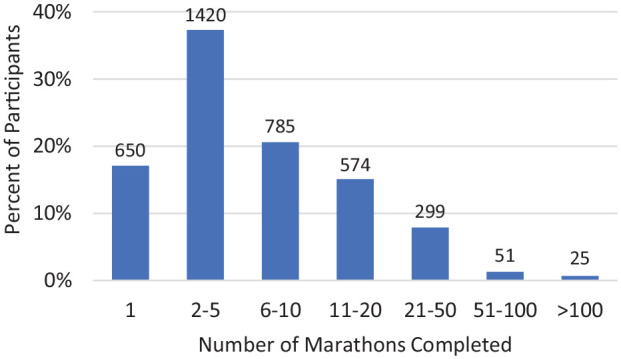
Hip and Knee Health
Hip and/or knee pain that prevented running over the past year was reported by 36.4% (n = 1383) of participants, consisting of 52.6% knee pain (n = 728), 27.7% hip pain (n = 383), and 19.7% (n = 272) with both hip and knee pain. Hip and/or knee arthritis was reported by 7.3% (n = 277) of participants, consisting of 70.0% knee arthritis (n = 194), 20.2% hip arthritis (n = 56), and 9.7% hip and knee arthritis (n = 27). The prevalence of hip and/or knee arthritis stratified by age can be seen in Figure 2. The overall prevalence of arthritis by joint was 5.1% for the knee, 1.5% for the hip, and 0.7% for both hip and knee arthritis. The average age at diagnosis was 44.2 years for knee, 46.9 years for hip, and 48.4 years for hip and knee arthritis. The prevalence of arthritis in those ≥65 years of age was 21.7% (34 of 157) and 6.7% (243 of 3647) for those <65 years of age.
Figure 2.
Overall prevalence of hip and/or knee arthritis by age.
Overall, 26.1% (n = 993) of participants reported a family history of hip and/or knee arthritis and 49.7% (n = 1892) reported a history of hip and/or knee injuries that prevented them from running at any point their past. Most of the participants participated in some form of cross training (75.5%), and 38.6% noted participation in other sports activities.
A history of hip and/or knee surgery was reported by 10.9% (n = 413) of runners, with 89.6% being knee-related (370 of 413) and 10.4% being hip-related (43 of 413). The most common knee procedures included knee arthroscopy/meniscal surgery (66.8%), anterior cruciate ligament (ACL) reconstruction (13.0%), and a combination of ACL reconstruction and meniscal surgery (10.0%). The most common hip procedures included hip arthroscopy (51.2%) and hip fracture repair (14.0%). Seven patients reported knee arthroplasty and 8 patients reported hip arthroplasty. Additional reported procedures can be found in Table 2.
Table 2.
Surgical procedures reported by all runners
| Body Region | Condensed Procedure List | No. | Percent |
|---|---|---|---|
| Knee | Knee arthroscopy/meniscal surgery | 247 | 66.8 |
| ACLR | 48 | 13.0 | |
| ACLR, meniscal surgery | 37 | 10.0 | |
| Knee arthroplasty | 7 | 1.9 | |
| Patella tendon surgery/repair | 6 | 1.6 | |
| Proximal tibia fracture repair | 4 | 1.1 | |
| Multiligamentous knee injury repair | 2 | 0.5 | |
| Patellar instability surgery | 2 | 0.5 | |
| Cartilage repair of the knee | 1 | 0.3 | |
| Quad tendon surgery/repair | 1 | 0.3 | |
| Other - knee | 15 | 4.0 | |
| Hip | Hip arthroscopy | 22 | 51.2 |
| Hip arthroplasty | 8 | 18.6 | |
| Hip fracture repair | 6 | 14.0 | |
| Hip dislocation | 2 | 4.6 | |
| Proximal hamstring injury repair | 2 | 4.6 | |
| Other - hip | 3 | 7.0 |
ACLR, anterior cruciate ligament reconstruction.
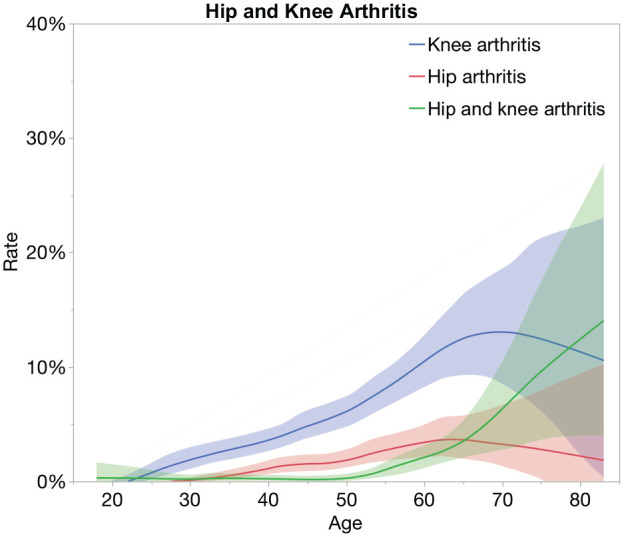
Risk Factors for Joint Pain and Arthritis
The multivariable analysis revealed multiple risk factors for pain and/or arthritis of the hip/knee (Table 3). A history of a hip/knee injury that prevented running was a strong risk factor for both pain (OR, 3.30 [95% CI, 2.85-3.83]; P < 0.01) and arthritis (OR, 5.04 [95% CI, 3.45-7.34], P < 0.01). A history of hip/knee surgery was also a strong predictor for pain (OR, 1.50 [95% CI, 1.20-1.87], P < 0.01) and arthritis (OR, 5.85 [95% CI, 4.33-7.92], P < 0.01). Age appeared to have an opposite effect on the rate of pain and arthritis (Figure 3a), as age, per year, reduced the odds of having pain (OR, 0.99 [95% CI, 0.98-0.99], P < 0.01) and increased the odds of having arthritis (OR, 1.08 [1.06-1.10], P < 0.01). Sex was not a risk factor for arthritis, but female sex did increase the odds of hip/knee pain (OR, 1.43 [95% CI, 1.20-1.70], P < 0.01). For hip/knee pain, increasing weekly mileage and number of completed marathons had a small but significant reduction in the odds of having hip/knee pain (OR, 0.99 [95% CI, 0.98-0.99], P < 0.01 for weekly mileage and OR, 0.99 [95% CI, 0.98-0.99], P < 0.01 for number of marathons) (Figure 3b). Additional risk factors for arthritis included a family history of hip/knee arthritis (OR, 3.47 [95% CI, 2.52-4.79], P < 0.01) and increasing BMI (OR, 1.10 [95% CI, 1.05-1.15], P < 0.01) (Figure 3c). Notably, neither the number of marathons completed, running pace, weekly running mileage nor the reported number of years running were found to increase the risk of hip/knee arthritis (Table 3, Figure 3).
Table 3.
Multivariable logistic regression analysis of risk factors for hip and/or knee pain and arthritis
| Pain a | Arthritis b | |||
|---|---|---|---|---|
| Risk Factor | OR | P value | OR | P value |
| History of hip/knee surgery | 1.50 (1.20-1.87) | <0.01* | 5.85 (4.33-7.92) | <0.01* |
| Age, per year | 0.99 (0.98-0.99) | <0.1* | 1.08 (1.06-1.10) | <0.01* |
| History of hip/knee injury that prevented running | 3.30 (2.85-3.83) | <0.01* | 5.04 (3.45-7.34) | <0.01* |
| Family history of hip/knee arthritis | 1.16 (0.98-1.37) | 0.12 | 3.47 (2.52-4.79) | <0.01* |
| BMI, per kg/m2 | 1.02 (0.99-1.05) | 0.05 | 1.10 (1.05-1.15) | <0.01* |
| Pace for training runs, per minute/mile | 1.04 (0.98-1.10) | 0.19 | 0.88 (0.79-0.99) | 0.03 |
| Female sex, compared with men | 1.43 (1.20-1.70) | <0.01* | 1.41 (0.99-2.01) | 0.08 |
| Participation in other sports | 1.04 (0.90-1.21) | 0.59 | 0.87 (0.64-1.17) | 0.35 |
| Weekly mileage, per mile | 0.99 (0.98-0.99) | <0.01* | 0.99 (0.98-1.01) | 0.36 |
| No. of marathons, per marathon | 0.99 (0.98-0.99) | <0.01* | 1.00 (0.99-1.01) | 0.56 |
| Duration of running, per year | 1.00 (0.99-1.01) | 0.64 | 1.00 (0.98-1.01) | 0.66 |
| Cross training | 0.88 (0.74-1.04) | 0.14 | 0.98 (0.69-1.40) | 0.91 |
BMI, body mass index; OR, odds ratio.
History of hip and/or knee pain within the past year that prevented running.
History of hip and/or knee arthritis.
Significant after Bonferroni correction (P < 0.01).
Figure 3.
Prevalence of hip and/or knee arthritis and pain by (a) age, (b) number of marathons completed, (c) BMI, (d) average pace during training runs, and (e) number of years running. BMI, body mass index.
Healthcare Provider Advice
Nearly 1 in 4 runners (24.2%) were advised by their physician to either reduce the amount that they run or eliminate running all together, yet the majority of all participants in this study (94.2%) plan to run another marathon. A similar trend was seen in the subset of patients with arthritis. These runners were twice as likely (50.2%) to have had a physician advise them to reduce or limit their running, yet 91.4% of those with arthritis plan to run another marathon.
Discussion
Using data from the largest cohort of runners to date, the present study found a low prevalence of arthritis (7.3%) among recreational marathon runners. Although the cumulative number of years running, the number of marathons completed, weekly running mileage, and running pace were not statistically significantly associated with a diagnosis of arthritis, many of the runners (24.2%) in this study who discussed running with their healthcare provider were suggested to either stop or reduce their amount of running. In keeping with our hypothesis, a history of hip and/or knee injuries that prevented running, previous surgery on the hip or knee, advanced age, family history, and BMI were significantly associated with a diagnosis of arthritis.20,29
Older age is widely accepted as a major contributor to the development of osteoarthritis,12,18 with cohort studies of the general population estimating that 26% of US adults ≥45 years of age have symptomatic hip or knee osteoarthritis.10,11 Long-distance runners are not immune to the effect of age on the development of arthritis. Ponzio et al 20 investigated the prevalence of hip and knee arthritis in high-volume marathon runners and identified a 24.5% prevalence in marathon runners ≥65 years of age, compared with a prevalence of 8.9% in all runners. A history of hip and/or knee injuries and surgical procedures on the hip and/or knee were the strongest predictors of arthritis and pain in the current study.
Injuries alone can result in damage to the cartilaginous surface of the joint, or in altered joint biomechanics that may hasten joint degeneration. Surgical interventions for many injuries may help improve pain and restore function, but do not necessarily reduce the risk of joint degeneration. Meniscal surgery and ACL reconstructions were the surgeries most commonly reported in the current study and it is widely understood that whereas surgery can improve pain and function after these injuries, it does not reduce the risk for arthritis.1,4 Other predictors for arthritis found in the current study, BMI and family history, have similarly been found to increase the risk for arthritis in runners.20,29 In a survey study of runners, Williams 29 identified a 5.0% increased risk for hip osteoarthritis and 9.8% increased risk for hip replacement per kg/m2.
Importantly, we identified multiple variables associated with a person’s running history that did not have a statistically significant association with joint pain or arthritis. It seems intuitive that the cumulative number of years someone has been running, number of completed marathons, number of miles run per week, or running pace should have a direct relationship with pain and arthritis, but this was not found in the current study. In a study of high-volume marathon runners who completed a mean of 76 marathons per runner, the number of marathons completed was not a significant risk factor for hip or knee arthritis. 20 A systematic review and meta-analysis of running and knee osteoarthritis in fact found a history of running as providing a protective effect, with a >50% reduced risk for knee surgery due to osteoarthritis. 27 Collectively, these studies, combined with results from the current study, suggest that running to some degree may likely be beneficial for joint health.
Several basic science and imaging-based studies have found evidence to support the positive impact of running on joint health. Hyldahl et al 9 evaluated knee synovial fluid contents before and after runners completed a 30-minute run and compared the contents to knees that were unloaded for 30 minutes. The authors found running decreases the concentration of intra-articular pro-inflammatory cytokines and aids in the movement of cartilage oligomeric matrix proteins from the joint space into the serum. Horga et al 8 used high-resolution magnetic resonance imaging (MRI) to evaluate the knees of healthy middle-aged adults 6 months before and 2 weeks after running their first full-length marathon. MRI scans completed before training demonstrated signs of knee damage in the majority of subjects; however, after the marathon, there was a reduction in the radiological score of damage in the subchondral bone marrow of the tibia and the femur. There was an increase in damage to the lateral patella and soft tissue structures, including the semimembranosus tendon, iliotibial band, and prepatellar bursa. Additional basic science and imaging studies are needed to better understand how running and weightbearing exercises potentially improve the overall health of hip and knee joints.
A strength of the current study is the large sample size that represents a wide spectrum of long-distance runners, from beginners to high-volume marathon runners. The majority of the runners (67.1%) were beginners who had run ≤5 marathons, whereas on the experienced end of the spectrum there were 25 runners who had run >100 marathons. Most of the studies to date investigating the role of running with arthritis were on small cohorts that focused on elite and high-volume marathon runners, limiting the applicability of the findings to patients most often encountered in the healthcare setting.2,13,16,20,23,24,28 Despite clear evidence that running provides positive health benefits, and a growing body of evidence suggesting running does not hasten joint degeneration, many patients, with or without arthritis, are being advised by their physician to reduce their running or eliminate it from their routine altogether.
This study had several important limitations. First, the diagnosis of arthritis in this study was self-reported; therefore, the true incidence of arthritis in this population is unknown. The survey-based nature of this study prohibited the ability to perform clinical and radiographic evaluations of arthritis. The survey question used to query for the presence of arthritis was, however, designed based on questions used in epidemiological studies to survey the general public for arthritis. This has been validated as an effective means to inquire about arthritis via health surveys and has been used in previous studies evaluating the prevalence of arthritis in runners, which allows a basis for comparison of our results with those in the literature.17,20,22 Second, we were unable to fully identify and account for the additional variables that are known to influence the development of osteoarthritis, such as bone deformities, joint malalignment, trauma, genetics, or metabolic conditions that affect bone metabolism. 12 In addition, we did not capture the full cohort of runners to whom this survey was distributed; therefore, the study cohort may not reflect the entire group of Chicago marathon runners. We did, however, collect information from a wide spectrum of runners representing beginners to high-volume marathon athletes.
Conclusion
The present study found a low prevalence of self-reported hip and/or knee arthritis among recreational marathon runners and did not find a dose-response relationship between running history and risk of arthritis. These results stand in contrast to long-established dogma suggesting that running increases the risk of developing hip or knee arthritis. As a result, these findings can be used by healthcare providers across the care spectrum to inform discussions with patients about the risks and benefits of running and as a basis for re-examining existing guidelines around running and joint health.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381231190876 for Does Running Increase the Risk of Hip and Knee Arthritis? A Survey of 3804 Marathon Runners by Matthew J. Hartwell, Joseph E. Tanenbaum, George Chiampas, Michael A. Terry and Vehniah K. Tjong in Sports Health
Acknowledgments
The authors would like to acknowledge Steven Dayton, MD and Samuel Rosenberg, MD for their contributions in helping design the participant survey used in this study.
Footnotes
The author declared potential conflicts of interest: M.A.T. has received consulting and speaking fees from Arthrex and Smith+Nephew. V.K.T. has received consulting and speaking fees from Smith+Nephew.
References
- 1. Abram S, Judge A, Beard D, Carr A, Price A. Long-term rates of knee arthroplasty in a cohort of 834 393 patients with a history of arthroscopic partial meniscectomy. Bone Joint J. 2019;101-B(9):1071-1080. [DOI] [PubMed] [Google Scholar]
- 2. Alentorn-Geli E, Samuelsson K, Musahl V, et al. The association of recreational and competitive running with hip and knee osteoarthritis: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2017;47(6):373-390. [DOI] [PubMed] [Google Scholar]
- 3. Cheng Y, Macera C, Davis D, Ainsworth BE, Troped PJ, Blair SN. Physical activity and self-reported, physician-diagnosed osteoarthritis: is physical activity a risk factor? J Clin Epidemiol. 2000;53(3):315-322. [DOI] [PubMed] [Google Scholar]
- 4. Everhart J, Jones M, Yalcin S, et al. The clinical radiographic incidence of posttraumatic osteoarthritis 10 years after anterior cruciate ligament reconstruction: data from the MOON nested cohort. Am J Sports Med. 2021;49(5):1251-1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Galic B. 84 marathon statistics every runner should know. Livestrong. https://www.livestrong.com/article/13763749-marathon-statistics/. Accessed April 16, 2022.
- 6. Harris P, Taylor R, Minor B, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Horga LM, Henckel J, Fotiadou A, et al. Can marathon running improve knee damage of middle-aged adults? A prospective cohort study. BMJ Open Sport Exerc Med. 2019;5(1):e000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hyldahl R, Evans A, Kwon S, et al. Running decreases knee intra-articular cytokine and cartilage oligomeric matrix concentrations: a pilot study. Eur J Appl Physiol. 2016;116(11-12):2305-2314. [DOI] [PubMed] [Google Scholar]
- 10. Jordan J, Helmick C, Renner J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34(1):172-180. [PubMed] [Google Scholar]
- 11. Jordan J, Helmick C, Renner J, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009;36(4):809-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katz J, Arant K, Loeser R. Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA. 2021;325(6):568-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Konradsen L, Hansen E, Søndergaard L. Long distance running and osteoarthrosis. Am J Sports Med. 1990;18(4):379-381. [DOI] [PubMed] [Google Scholar]
- 14. Lee D, Brellenthin A, Thompson P, Sui X, Lee IM, Lavie CJ. Running as a key lifestyle medicine for longevity. Prog Cardiovasc Dis. 2017;60(1):45-55. [DOI] [PubMed] [Google Scholar]
- 15. Lo G, Musa S, Driban J, et al. Running does not increase symptoms or structural progression in people with knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol. 2018;37(9):2497-2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Marti B, Knobloch M, Tschopp A, Jucker A, Howald H. Is excessive running predictive of degenerative hip disease? Controlled study of former elite athletes. BMJ. 1989;299(6691):91-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Murphy L, Cisternas M, Greenlund K, et al. Defining arthritis for public health surveillance: methods and estimates in four US population health surveys. Arthritis Care Res. 2017;69(3):356-367. [DOI] [PubMed] [Google Scholar]
- 18. Oliveria S, Felson D, Reed J, Cirillo P, Walker A. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38(8):1134-1141. [DOI] [PubMed] [Google Scholar]
- 19. Panush R, Schmidt C, Caldwell J, et al. Is running associated with degenerative joint disease? JAMA. 1986;255(9):1152-1154. [PubMed] [Google Scholar]
- 20. Ponzio DY, Syed UAM, Purcell K, et al. Low Prevalence of hip and knee arthritis in active marathon runners. J Bone Joint Surg Am. 2018;100(2):131-137. [DOI] [PubMed] [Google Scholar]
- 21. Roeh A, Lembeck M, Papazova I, et al. Marathon running improves mood and negative affect. J Psychiatr Res. 2020;130:254-259. [DOI] [PubMed] [Google Scholar]
- 22. Sacks J, Harrold L, Helmick C, et al. Validation of a surveillance case definition for arthritis. J Rheumatol. 2005;32(2):340-347. [PubMed] [Google Scholar]
- 23. Sohn R, Micheli L. The effect of running on the pathogenesis of osteoarthritis of the hips and knees. Clin Orthop Relat Res. 1985:1985(198)106-109. [PubMed] [Google Scholar]
- 24. Spector T, Harris P, Hart D, et al. Risk of osteoarthritis associated with long-term weight-bearing sports: a radiologic survey of the hips and knees in female ex-athletes and population controls. Arthritis Rheum. 1996;39(6):988-995. [DOI] [PubMed] [Google Scholar]
- 25. Spiker A, Johnson K, Cosgarea A, Ficke J. A primer on running for the orthopaedic surgeon. J Am Acad Orthop Surg. 2020;28(12):481-490. [DOI] [PubMed] [Google Scholar]
- 26. Theis K, Murphy L, Guglielmo D, et al. Prevalence of arthritis and arthritis-attributable activity limitation - United States, 2016-2018. MMWR Morb Mortal Wkly Rep. 2021;70(40):1401-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Timmins KA, Leech RD, Batt ME, Edwards KL. Running and knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2017;45(6):1447-1457. [DOI] [PubMed] [Google Scholar]
- 28. Tveit M, Rosengren B, Nilsson J, Karlsson M. Former male elite athletes have a higher prevalence of osteoarthritis and arthroplasty in the hip and knee than expected. Am J Sports Med. 2012;40(3):527-533. [DOI] [PubMed] [Google Scholar]
- 29. Williams P. Effects of running and walking on osteoarthritis and hip replacement risk. Med Sci Sports Exerc. 2013;45(7):1292-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams PT. Lower prevalence of hypertension, hypercholesterolemia, and diabetes in marathoners. Med Sci Sports Exerc. 2009;41(3):523-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381231190876 for Does Running Increase the Risk of Hip and Knee Arthritis? A Survey of 3804 Marathon Runners by Matthew J. Hartwell, Joseph E. Tanenbaum, George Chiampas, Michael A. Terry and Vehniah K. Tjong in Sports Health