Abstract
Background
Postoperative radiographs may be performed on different timelines after shoulder arthroplasty. Radiographs obtained in the post-operative recovery unit (PACU) are often of poorer quality. The purpose of the current study was to explore and compare the quality of PACU radiographs and radiographs performed in the radiology suite on post-operative Day 1 (POD1), as well as determine their impact on changes in post-operative management.
Methods
Our series included 50 consecutive anatomic total shoulder arthroplasties (TSA) for which post-operative radiographs were obtained in the PACU and 50 consecutive TSA for which post-operative radiographs were obtained in the radiology suite on POD 1. TSA radiographs were blinded and reviewed by 3 authors and graded on their quality using criteria described using previously published methods. The weighted kappa was used to describe the intra-rater agreement and inter-rater agreement between two raters.
Results
There was no difference in age, sex, BMI, and comorbidities between cohorts. Intra-observer reliability was moderate to substantial with weighted kappa values of 0.65±0.07 (p<0.001), 0.58±0.09 (p<0.001), and 0.67±0.07 (p<0.001). Inter-observer reliability was moderate to substantial with weighted kappa values of 0.605±0.07 (p<0.001), 0.66±0.07 (p<0.001), and 0.65±0.08 (p<0.001). When assessing quality of radiographs, 30% of radiographs obtained in PACU were deemed quality while 57% of radiographs obtained in the radiology suite were deemed quality (p<0.001).
Conclusion
Post-operative radiographs in the PACU do not alter patient management and are often inadequate to serve as baseline radiographs. Conversely, radiographs obtained in the radiology suite are of higher quality and can serve as a superior baseline radiograph.
Level of Evidence: IV
Keywords: total shoulder arthroplasty, radiographs, post-anesthesia care unit (PACU), quality
Introduction
Radiographs in the immediate post-operative period after shoulder arthroplasty serve several purposes. They are used to judge component positioning and to evaluate for possible complication including periprosthetic fracture or dislocation.1-4 Post-operative radiographs can also be shown to patients for educational purposes, potentially increasing patient satisfaction and compliance with postoperative protocols. As such, post-operative radiographs are ubiquitous in shoulder arthroplasty practice.
Many surgeons perform radiographs in the recovery room or post-anesthesia care unit (PACU). Images from the PACU offer immediate feedback regarding operative complications and implant placement. They can aid in that patient’s care and inform the surgeon on operative technique, which has the potential to improve future surgical decision-making. These PACU radiographs, though, are often underpenetrated and can be difficult to interpret, particularly for films that are taken with some degree of technical error.5 This is likely due to the inherent nature of the PACU with drowsy patients making positioning difficult, portable radiography machines having decreased resolution, among other difficulties.
Literature in total hip arthroplasty has repeatedly shown PACU radiographs to be inferior in quality to radiographs performed in a radiology suite.6-8 This has also been evaluated in total knee arthroplasty, where PACU radiographs are found to be difficult to interpret, often underpenetrated, obscured by bulky dressings, and not of high enough quality to serve as baseline radiographs.9 Namdari et al. evaluated the quality of PACU radiographs in shoulder arthroplasty and concluded that these radiographs are both costly and of poor quality. In addition, they found in their series that no treatment changes were made based on PACU radiographs.3
Some surgeons only obtain post-operative radiographs in the formal radiology suite. In this scenario, alert patients and radiology technicians can optimize positioning, increase resolution of the study, and obtain higher quality radiographs to serve as post-operative evaluation and baseline films for future comparison. The purpose of the current study was to explore and compare the quality of PACU radiographs and the immediate postoperative radiographs performed in the radiology suite, as well as determine their impact on potential changes in post-operative management.
Methods
This study was approved by the Institution’s IRB (IRB# #202106409). We retrospectively reviewed 392 consecutive shoulder arthroplasties performed between January 2020 and July 2021. Patients were identified using current procedural terminology (CPT) 23472 for total shoulder arthroplasty. All reverse shoulder arthroplasty cases, 234 in total, were excluded. Thus 158 anatomic total shoulder arthroplasty cases were included for final analysis. There are two shoulder & elbow fellowship-trained physicians at our institution. One surgeon obtains post-operative radiographs (AP, Grashey, Scapular Y) in the PACU and again at two weeks, 6 weeks, 3 months, 6 months, and yearly (AP, Grashey, Axillary Lateral) post-operatively, while the other surgeon obtains postoperative radiographs (AP, Grashey, Axillary Lateral) in the radiology suite on post-operative day (POD) 1 that are meant to serve as baseline and does not repeat radiographs until one year post-operatively.
Our series included 50 consecutive anatomic total shoulder arthroplasties (TSA) for which post-operative radiographs were obtained in the PACU and 50 consecutive TSA for which post-operative radiographs were obtained in the radiology suite on POD 1 prior to discharge, that were selected from the total sample.
Single view, true AP TSA radiographs were blinded and reviewed by 3 authors (JVN, BMP, TDH) and graded on their quality. For patients that had radiographs obtained in the PACU, two week post-operative radiographs were also reviewed and graded. Quality was based on prior description by Alolabi et al. who defined radiographic criteria including: less than 2mm overlap of the humeral head at the level of the osteotomy surface, greater tuberosity and calcar in profile with minimal overlap of the prosthesis and lateral or medial bone (Figure 1).2,10 Criteria and quality examples were provided during the review process. Radiographs were reviewed independently. A second review was completed approximately one month following the first review. Reviewers were asked to score “yes” or “no” if the radiograph met the pre-determined quality criteria.
Figure 1A-1B.
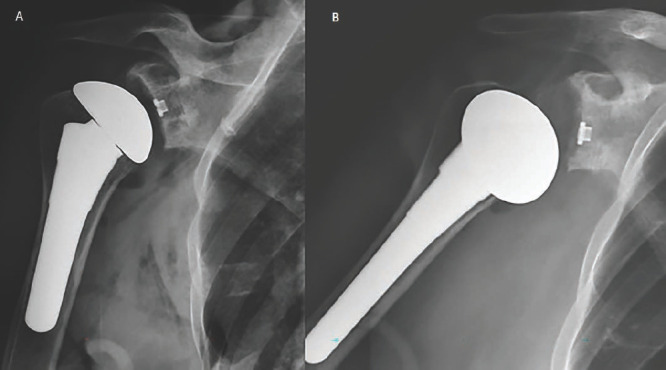
(A) True AP high quality radiograph. (B) low quality radiograph.
TSA radiographs were also reviewed for evidence of fracture or dislocation and final radiology reads were also reviewed for fracture or dislocation. The weighted kappa was used to describe the intra-rater agreement and inter-rater agreement between two raters. The inter-rater agreement for all three raters was completed using the SAS MAGREE macro. Between group comparisons in age was evaluated using independent t-tests while BMI and comorbid conditions were compared between groups using Wilcoxon Rank Sum tests. Radiographic quality was scored as “Yes” or “No” and results were compared with chi-squared test. All analyses were completed using SAS statistical software version 9.4 (SAS Institute, Inc., Cary NC).
Results
There was no statistical difference in age, sex, BMI, and number of comorbidities between all groups (Table I). No patients were discharged same day. Intra-observer reliability was moderate to substantial with weighted kappa values of 0.65±0.07 (95% CI 0.51-0.80, p<0.001), 0.58±0.09 (95% CI 0.41-0.75, p<0.001), and 0.67±0.07 (95% CI 0.53-0.82), p<0.001). Inter-observer reliability was moderate to substantial with weighted kappa values of 0.605±0.07 (95% CI 0.46-0.75, p<0.001), 0.66±0.07 (95% CI 0.52-0.81, p<0.001), and 0.65±0.08 (95% CI 0.50-0.80, p<0.001).
Table I.
Patient Characteristics
| PACU | POD 1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Min | Max | Mean | SD | Min | Max | Mean | SD | p-value |
| Age | 47 | 80 | 65.4 | 7.6 | 48 | 93 | 66.6 | 8.8 | 0.4518 |
| Sex (n, % female) | 26 (52%) | 28 (56%) | 0.6882 | ||||||
| BMI | 19.7 | 52.8 | 31.6 | 7.6 | 21.2 | 52.1 | 31.9 | 6.5 | 0.6516 |
| Comorbidities1 | 1 | 29 | 8.9 | 5.6 | 0 | 30 | 8.4 | 5.4 | 0.7115 |
1 Comorbidities: obesity, hyperlipidemia, Diabetes Mellitus, acute blood loss.
When assessing quality of radiographs, 30% of radiographs obtained in the PACU were deemed to be of adequate quality while 57% of radiographs obtained in the radiology suite were deemed to be of adequate quality, which was statistically significant (p<0.001). Of the 50 patients who received two week post-operative radiographs, 60% were deemed to be sufficient to serve as baseline radiographs which was significantly improved from PACU radiographs (p<0.001) but not radiology suite radiographs (p=0.64).
When reviewing final radiology reports, two patients’ final radiology read reported possible fracture on PACU films. On review of these radiographs the possible fracture was determined by the reviewers to be the lesser tuberosity osteotomy site (Figure 2). There were no changes in patient’s post-operative courses including weightbearing status, therapy protocol, or return trip to the operating room based on imaging findings.
Figure 2.

X-Ray showing the minimally displaced lesser tuberosity osteotomy site.
The cost of PACU and POD1 radiographs were compared. Professional billing (radiologist read) and hospital billing costs were equal for PACU radiographs and for radiographs taken in the radiology suite (POD1 and 2-week postoperative). Nevertheless, since there are no special rates for outpatient radiographs, all radiographs taken are billable, thus patients that receive radiographs at PACU and then again at 2-weeks following surgery have a two-fold increased billable cost.
Discussion
Historically, many institutions have routinely obtained immediate post-operative portable radiographs in the PACU following arthroplasty procedures. Based on published literature, these studies are often of poor quality and potentially should not serve as baseline radiographs. Surgeons at our institution vary in their preferences for postoperative radiographs. This conveniently allows for the comparison of these radiographs in a largely homogenous patient population. The results obtained in our study show that immediate post-operative radiographs are often of poorer quality than those obtained in the radiology suite on POD 1. This study also showed that there was no difference in patient management based on when radiographs were obtained.
There are multiple studies in the total hip arthroplasty (THA) and total knee arthroplasty (TKA) literature that question the cost-effectiveness and quality of immediate post-operative radiographs. Glaser completed a two part study in which 200 patients had immediate post-operative radiographs with a total cost of $36,000, and only 36% were determined to have sufficient quality to act as baseline radiographs.11 In their second part, 550 patients prospectively received first post-operative radiographs at two weeks. They determined that there was no change in management based on immediate post-operative radiographs.
Ndu reported on 632 consecutive PACU radiographs following THA. 17% of their series was determined to be inadequate to detect technical issues and only 2 (0.3%) impacted inpatient management.6 They concluded that routine inpatient radiographs should be obtained in the radiology suite. Novack reviewed 195 readmissions within 90 days of uncomplicated TKA to evaluate if there was evidence of abnormality that may have prevented readmission.12 There was no evidence of fracture or other abnormality that could have predicted readmission. They determined that the cost associated with identifying a single fracture in 2,415 patients was $1,072,260. Hassan reviewed 624 consecutive TKA over a 34-month period and concluded that early post-operative radiographs did not change routine post-operative management.13
There is a paucity of literature regarding immediate post-operative imaging following shoulder arthroplasty. Namdari did report on shoulder arthroplasty patients who received a single view (88% true AP) in the PACU compared to a second group of patients who obtained a full series after discharge. They concluded that routine PACU radiographs may result in poor-quality images and elimination of these radiographs may reduce cost without changing clinical care.3 Their series however did not evaluate the utility and quality of post-operative x-rays completed prior to discharge in the radiology suite.
Some advantages of PACU radiographs are that they offer immediate feedback not only on possible complications, but also on operative techniques. Some surgeons find advantageous to analyze the postoperative radiograph the same day of the surgery, in order to potentially improve future surgical techniques or decisions, and for teaching purposes as well. Despite of this, PACU radiographs tend to be of low quality and they usually do not serve as high quality baseline images for follow up. On the contrary, there are multiple advantages to obtaining radiographs in the radiology suite on POD 1. Radiographs were found to be of higher quality when compared to portable PACU films. Obtaining baseline radiographs prior to discharge can also streamline postoperative clinic visit efficiency by negating the need to routinely obtain baseline radiographs at the first postoperative visit. Quality baseline radiographs within the first few days of the procedure are also more useful in scrutinizing surgical technique than obtaining them weeks following the procedure.
This study is limited by its retrospective nature. First, we reviewed post-operative preferences for the two surgeons at our institution and understand there are many other post-operative imaging protocols which could be applied. Second, we chose to review the past 100 consecutive TSA cases. Our study population may not have been large enough to capture radiographs that would have changed patient management.
While no patient’s post-operative course was altered based on radiographs in our study, there is a potential liability for missing a dislocation or fracture if radiographs are not obtained prior to discharge. Optimally, imaging would be performed prior to a patient being awakened from anesthesia to allow for any needed intervention prior to leaving the operating room. As this is often infeasible, we feel that, for this reason, radiographs should at least be completed and reviewed prior to discharge. If patients are undergoing same day discharge shoulder arthroplasty, we would recommend PACU radiographs followed by a complete series at their first post-operative visit to act as baseline radiographs. Alternatively, patients undergoing same day discharge may be able to obtain higher quality radiographs in the radiology suite prior to discharge depending on institutional capabilities. If patients are being admitted for observation, this study supports the practice of obtaining radiographs in the radiology suite on POD 1 rather than PACU radiographs.
Conclusion
Radiographs obtained in the post-anesthesia care unit (PACU) are often of poor quality and do not often alter decision making following shoulder arthroplasty. The results of this study support the use of x-rays obtained prior to patient discharge, in the radiology suite when possible. These x-rays are of higher quality and serve as better baseline radiographs following anatomic total shoulder arthroplasty.
References
- 1.Barwood S, Setter KJ, Blaine TA, Bigliani LU. The incidence of early radiolucencies about a pegged glenoid component using cement pressurization. J Shoulder Elbow Surg. 2008;17(5):703–8. doi: 10.1016/j.jse.2008.01.147. [DOI] [PubMed] [Google Scholar]
- 2.Chalmers PN, Granger EK, Orvets ND, Patterson BM, Chamberlain AM, Keener JD, et al. Does prosthetic humeral articular surface positioning associate with outcome after total shoulder arthroplasty? J Shoulder Elbow Surg. 2018;27(5):863–70. doi: 10.1016/j.jse.2017.10.038. [DOI] [PubMed] [Google Scholar]
- 3.Namdari S, Hsu JE, Baron M, Huffman GR, Glaser D. Immediate postoperative radiographs after shoulder arthroplasty are often poor quality and do not alter care. Clin Orthop Relat Res. 2013;471(4):1257–62. doi: 10.1007/s11999-012-2551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Combes D, Lancigu R, Desbordes de Cepoy P, Caporilli-Razza F, Hubert L, Rony L, et al. Imaging of shoulder arthroplasties and their complications: a pictorial review. Insights Imaging. 2019;10(1):90. doi: 10.1186/s13244-019-0788-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teo TL, Schaeffer EK, Mulpuri K. Need for Higher Quality Evidence to Determine the Utility of Postoperative Radiography. JAAOS Global Research & Reviews. 2018;2(8):e026. doi: 10.5435/JAAOSGlobal-D-18-00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ndu A, Jegede K, Bohl DD, Keggi K, Grauer JN. Recovery room radiographs after total hip arthroplasty: tradition vs utility? J Arthroplasty. 2012;27(6):1051–6. doi: 10.1016/j.arth.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 7.Mulhall KJ, Masterson E, Burke TE. Routine recovery room radiographs after total hip arthroplasty: Ineffective for screening and unsuitable as baseline for longitudinal follow-up evaluation1 1No benefits or funds were received in support of this study. The Journal of Arthroplasty. 2004;19(3):313–7. doi: 10.1016/j.arth.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 8.Niskanen RO. Early repetitive radiography is unnecessary after an uncomplicated cemented hip or knee arthroplasty for osteoarthritis. Acta Orthop Belg. 2005;71(6):692–5. [PubMed] [Google Scholar]
- 9.Longenecker AS, Kazarian GS, Boyer GP, Lon-ner JH. Radiographic Imaging in the Postanesthesia Care Unit is Unnecessary After Partial Knee Arthroplasty. The Journal of Arthroplasty. 2017;32(5):1431–3. doi: 10.1016/j.arth.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Alolabi B, Youderian AR, Napolitano L, Szerlip BW, Evans PJ, Nowinski RJ, et al. Radiographic assessment of prosthetic humeral head size after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(11):1740–6. doi: 10.1016/j.jse.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Glaser D, Lotke P. Cost-effectiveness of immediate postoperative radiographs after uncomplicated total knee arthroplasty: a retrospective and prospective study of 750 patients. J Arthroplasty. 2000;15(4):475–8. doi: 10.1054/arth.2000.4338. [DOI] [PubMed] [Google Scholar]
- 12.Novack TA, Patel JN, Koss J, Mazzei C, Harrington CJ, Wittig JC, et al. Is There a Need for Recovery Room Radiographs Following Uncomplicated Primary Total Knee Arthroplasty? Cureus. 2021;13(4):e14544. doi: 10.7759/cureus.14544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hassan S, Wall A, Ayyaswamy B, Rogers S, Mills SP, Charalambous CP. Is there a need for early post-operative x-rays in primary total knee replacements? Experience of a centre in the UK. Ann R Coll Surg Engl. 2012;94(3):199–200. doi: 10.1308/003588412X13171221501780. [DOI] [PMC free article] [PubMed] [Google Scholar]


