Abstract
Background:
Historically, overdose mortality rates among Hispanics have been lower than non-Hispanics. The purpose of this analysis was to characterize the U.S. overdose crisis among Hispanics compared to non-Hispanics.
Methods:
We used the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiological Research (WONDER) platform to obtain drug overdose mortality rates per 100,000 population between 2010-2021 for Hispanics and non-Hispanics. We examined the relative percent change and specific drug involvement (2010-2021) and state-level disparities (2010-2020) among Hispanics versus non-Hispanics. We calculated rate ratios by state and annual percent change in total and for each specific drug. Statistical analyses were performed using R software version 4.0.3 (R Project for Statistical Computing).
Results:
Nationally, from 2010 to 2021, Hispanic overdose rates rose from 5.6 to 21.7 per 100,000, an increase of 287.5% compared to 13.5 to 35.1 per 100,000, an increase of 160% among non-Hispanics. The average annual percent change was 12% for Hispanics and 9% for non-Hispanics. The three most common drug classes involved in overdose deaths among both groups included: Fentanyls and synthetic opioids; cocaine; and prescription opioids. Hispanic overdose rates were higher than non-Hispanic rates in New Mexico, Colorado, Massachusetts, and Pennsylvania in 2020, versus only Michigan in 2010.
Conclusions:
We observed disparities in overdose mortality growth among Hispanics compared to non-Hispanics from 2010 to 2021. These disparities highlight the urgency to develop community-centered solutions that take into consideration the social and structural inequalities that exacerbate the effects of the opioid overdose crisis on Hispanic communities.
Keywords: Overdose, Opioids, Hispanic, Fentanyl, Cocaine
1. Introduction
In the United States, overdose mortality rates have historically been lower among Hispanic individuals compared to other racial and ethnic groups (Centers for Disease Control and Prevention, 2022). Previous studies have documented increased overdose mortality rates in certain Hispanic subgroups (i.e. specific metropolitan areas or age groups) (Friedman et al., 2022; Hoopsick et al., 2021; Lippold and Ali, 2020). Heterogeneity in overdose rates among non-Hispanic groups is also documented in the literature (Friedman et al., 2022; Hoopsick et al., 2022; Humphreys et al., 2022). However, unexplored is an analysis of trends in overdose deaths among Hispanics by drug type and state. We, therefore, focus on comparing the rate of change between Hispanics and non-Hispanics. We sought to examine the relative percent change, specific drug involvement, and state-level disparities to characterize the overdose crisis in the U.S. Hispanic population.
2. Methods
Using the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiological Research (WONDER) platform, we obtained age-adjusted drug overdose mortality rates per 100,000 population between 2010-2021 for Hispanic and non-Hispanic individuals. In order to obtain the most updated data, we used WONDER’s provisional mortality file for 2021. We also obtained national and state-level crude overdose mortality rates per 100,000 population for 2010 and 2020 for Hispanic and non-Hispanic individuals (Supplemental Table 1). We defined drug overdose deaths using the International Classification of Diseases 10th Edition (ICD-10) codes, which have been used for mortality coding in the U.S. since 1999 (Centers for Disease Control and Prevention, 2015), for drug poisoning underlying causes of death, including unintentional, suicide, homicide, or undetermined intent (X40-44, X60-64, X85, 44 or Y10-14, respectively) without restricting to specific drugs, and stratified by year, Hispanic origin, and state. To analyze drug overdose rates by specific drug type, we then used WONDER’s Multiple Cause of Death file to select overdose deaths with ICD-10 codes for opium, heroin, other opioids, methadone, other synthetic narcotics (mainly fentanyl and fentanyl analogs) (Georgia Department of Public Health, n.d.), cocaine, and psychostimulants with abuse potential (T40.0 – T40.5 and T43.6, respectively) (Supplemental Table 2). Throughout this piece, we use the term “fentanyls” to refer to fentanyl and fentanyl analogs. In addition to a national analysis, we examined how the disparity in overdose deaths between Hispanics and non-Hispanics has changed over time in each state. To do so, we calculated, for each state, the relative rate of drug overdose death comparing Hispanics to non-Hispanics in each year for 2010, 2015, and 2020. We calculated the annual percent change in total and for each specific drug. Finally, as a supplemental analysis, we compared the annual rate of change stratified by both race and Hispanic ethnicity. We performed statistical analyses using R software version 4.0.3 (R Project for Statistical Computing).
3. Results
In 2010, the age-adjusted overdose mortality rate was 5.6 per 100,000 for Hispanic individuals and 13.5 for non-Hispanic individuals (annual rate ratio (RR) Hispanic vs non-Hispanic = 0.41). By 2021, age-adjusted overdose mortality had grown by 287.5% to 21.7 per 100,000 for Hispanic individuals. By contrast, the age-adjusted overdose mortality rate grew by 160% for non-Hispanic individuals to 35.1 per 100,000 (RR = 0.62) (Fig. 1). The average annual percent change among Hispanics was 12% compared to 9% for non-Hispanics using the arithmetic mean, or 9% versus 7% using the geometric mean. Among Hispanics versus non-Hispanics between 2010 and 2021, there was a larger percent increase in mortality attributed to fentanyls and synthetic opioids (7,150% versus 2,052%), cocaine (522% versus 450%), heroin (200% versus 163.6%), and prescription opioids (66.7% versus 15.4%), respectively. In contrast, the percent increase in methamphetamine (1,200% versus 1,716.7%) and methadone (16.7% versus 29.4%) was larger for non-Hispanics.
Fig. 1.
The drug-related overdose death rate for Hispanics has risen since 2015. (a) Death rate per 100,000 population for Hispanic individuals relative to non-Hispanic individuals for fentanyls and synthetic opioids and total national overdose deaths, 2010-2021. (b) Annual percent change for fentanyls and synthetic opioids and total national annual percent change, 2010-2021.
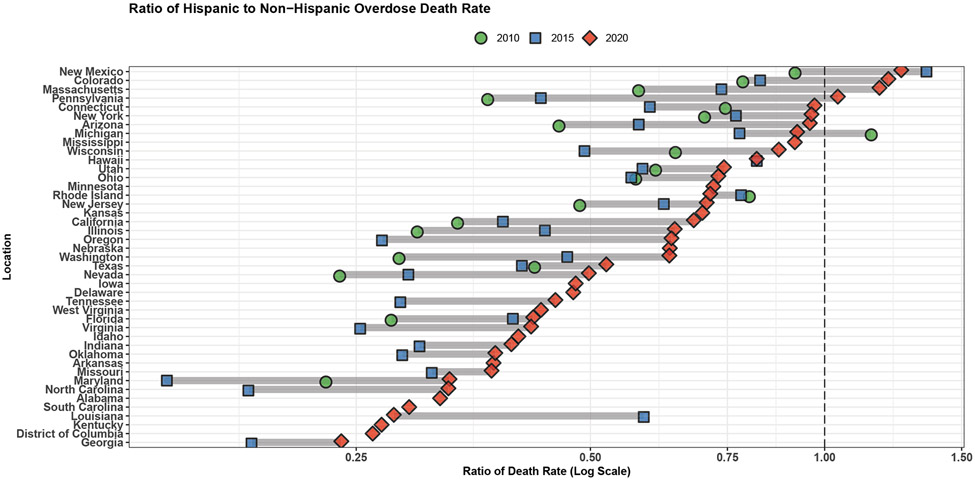
Between 2019 and 2020, as overdose death rates spiked during the COVID-19 pandemic, Hispanic individuals saw larger percent increases in overdose rates compared to non-Hispanic individuals for all classes of drugs assessed except heroin, for which there was a more negative decrease among non-Hispanics compared to Hispanics in 2020 (Supplemental Fig. 1). This was also true between 2020 and 2021 for fentanyls and synthetic opioids, methamphetamine, and prescription opioids (Supplemental Fig. 1). With respect to heroin, there was a smaller percent decrease in overdose deaths among Hispanics compared to non-Hispanics from 2020 to 2021 (Supplemental Fig. 1). At the state level, overdose rates among Hispanic individuals grew at a faster rate than those among non-Hispanic individuals between 2015 and 2020 in 26 of 30 (86.7%) of states where comparisons could be made. In 2020 Hispanic overdose rates were higher than non-Hispanic rates in four (New Mexico, Colorado, Massachusetts, and Pennsylvania) of 43 states assessed in 2020, compared to only one state (Michigan) in 2010 (Fig. 2).
Fig. 2.
Ratio of drug-related overdose mortality per 100,000 population for Hispanic individuals relative to non-Hispanic individuals, by state, 2010-2020. Values over 1 indicate the states where the ratio of overdose rates is higher among Hispanics compared to non-Hispanics. *Some states do not have one or more of the three data points.
In a supplemental analysis stratified by both race and Hispanic ethnicity, we found that for all racial groups (American Indian or Alaska Native, Asian or Pacific Islander, Black or African American, White), the growth rate in crude overdose mortality was higher among Hispanics compared to non-Hispanics over the analysis period (Supplemental Fig. 2). As with the overall comparison, the base rates and magnitude of change in terms of lives lost per year were higher among non-Hispanics of all races.
4. Discussion
Although Hispanic individuals have historically seen lower overdose mortality rates than other groups, we find that fatal overdose rates among Hispanics rose considerably faster than among non-Hispanic individuals in the 2010-2021 period. These trends were noted for the majority of US states, and across numerous classes of involved substances, including fentanyl and other synthetic opioids, cocaine, and prescription opioids. We found that in 2020, Hispanic overdose rates were higher in New Mexico Colorado, Massachusetts, and Pennsylvania. One state-level characteristic associated with this includes the size of the Hispanic population in each state - New Mexico has the largest Hispanic population, followed by Colorado, Massachusetts, and Pennsylvania (US Census, 2022). An additional factor includes the drug supply in the Northeast since there is a high prevalence of illicitly-manufactured fentanyl as an adulterant, substitute, and contaminant in their drug supply (Cano, 2022). In Massachusetts, inequalities in education, housing, and access to treatment among Hispanic men who died from an opioid overdose have been identified as causes of disparities in overdose mortality for Hispanic men (Cano, 2022).
Between 2020 and 2021, we observed large percent increases among Hispanics compared to non-Hispanics in overdose deaths involving fentanyls and synthetic opioids and methamphetamine (Supplemental Fig. 1). This is of particular importance considering that these two drug classes now account for the majority of overdose deaths in the United States. These findings should be taken into consideration when developing harm reduction strategies tailored to Hispanic communities.
Despite the widespread, and worsening, effects of the introduction of potent synthetic opioids into the drug supply, and accompanying increases in fatal overdose that have only worsened since the COVID-19 pandemic, access to effective opioid use disorder (OUD) treatment is still sparse and this is most often true for communities of color (Friedman et al., 2022; Humphreys et al., 2022; Jackson et al., 2022; Andraka-Christou, 2021;). Evidence from other studies suggests that the faster rise of overdose mortality among Hispanic individuals relative to their non-Hispanic counterparts is likely related to limited access to naloxone and other harm reduction resources, barriers to effective substance use disorder treatment (e.g., clinics not accepting Medicaid, fear of prosecution), and stigma surrounding substance use disorder among Hispanic communities (Friedman et al., 2022; Humphreys et al., 2022; Goodman-Meza et al., 2022; Jackson et al., 2022; Andraka-Christou, 2021; Lippold and Ali, 2020).
Take for example, a study of a naloxone standing order from 2014-2018 in Massachusetts, one of the states where overdose rates were higher among Hispanic individuals in 2020, where researchers found that communities with larger Hispanic populations were less likely to dispense any naloxone under the standing order (Chatterjee et al., 2022). This indicates that simply making naloxone available under a standing order is insufficient: more efforts are needed to expand overdose prevention access and use in Hispanic communities. With respect to treatment for OUD, buprenorphine has historically been less available in predominantly Hispanic and Black neighborhoods compared to methadone, which is highly regulated and stigmatized (Andraka-Christou, 2021; Jackson et al., 2021). Limited access to resources for OUD is just one example of the effects of social and structural determinants of health in the U.S.—their role in the opioid overdose crisis must be addressed.
Fentanyl test strips and more detailed drug checking programs could play a crucial role in minimizing the risk of overdose, particularly for people not intending to use fentanyl. One study based in Mexicali, Mexico offered this service and noted that participants demonstrated positive behavior changes (e.g. used less or did not use at all) in response to the discovery of fentanyl in their drugs (Goodman-Meza et al., 2022). However, the legality of drug checking devices varies by state, making drug checking efforts difficult in some areas. In two of the four states where Hispanics have higher overdose mortality compared to non-Hispanics, drug checking materials are illegal (Pennsylvania) or only allowed in the context of a syringe exchange (New Mexico) (Davis et al., 2022). Across the U.S., the legality of the possession and distribution of drug checking equipment is similarly unclear and complicated (Davis et al., 2022). Changing policies to allow and expand access to the full range of evidence-based overdose prevention tools is key.
In light of the large-magnitude increases found here, targeted, culturally-appropriate, and community-led efforts are needed to expand overdose prevention resources and treatment among Hispanic communities.
Supplementary Material
References
- Andraka-Christou B., 2021. Addressing Racial And Ethnic Disparities In The Use Of Medications For Opioid Use Disorder. Health Affairs 40(6). 10.1377/hlthaff.2020.02261 [DOI] [PubMed] [Google Scholar]
- Cano M, Agan A, Bandoian L, & Larochelle L, 2022. Individual and County-Level Disparities in Drug and Opioid Overdose Mortality for Hispanic Men in Massachusetts and the Northeast United States. Substance Use and Misuse 57(7), 1131–1143. https://doi.org/ 10.1080/10826084.2022.2064507 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention., 2022. National Center for Health Statistics. National Vital Statistics System, Mortality 1999-2020 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files, 1999-2020, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10.html on Oct 25, 2022 4:07:18 PM [Google Scholar]
- Centers for Disease Control and Prevention., 2022. National Center for Health Statistics. National Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are from the final Multiple Cause of Death Files, 2018-2020, and from provisional data for years 2021-2022, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10-provisional.html on Oct 25, 2022 4:08:58 PM [Google Scholar]
- Centers for Disease Control and Prevention. 2015. International Classification of diseases, (ICD-10- CM/PCS) Transition. Centers for Disease Control and Prevention. Accessed at https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm on Jan 24, 2023 [Google Scholar]
- Chatterjee A, Yan S, Xuan Z, Waye KM, Lambert AM, Green TC, Stopka TJ, Pollini RA, Morgan JR, Walley AY, 2022. Broadening access to naloxone: Community predictors of standing order naloxone distribution in Massachusetts. Drug Alcohol Depend 230. doi: 10.1016/j.drugalcdep.2021.109190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CS, Lieberman AJ, O'Kelley-Bangsberg M, 2022. Legality of drug checking equipment in the United States: A systematic legal analysis. Drug Alcohol Depend 234. DOI: 10.1016/j.drugalcdep.2022.109425 [DOI] [PubMed] [Google Scholar]
- Friedman JR, Beletsky L, Jordan A, 2022. Surging Racial Disparities in the U.S. Overdose Crisis. The American Journal of Psychiatry 179(2). doi: 10.1176/appi.ajp.2021.21040381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgia Department of Public Health. n.d. Drug overdose/opioid mortality definitions. OASIS Web Query Tool. Accessed at https://oasis.state.ga.us/oasis/webquery/help/DefMortDrugOD.html#:~:text=The%20following%20ICD%2D10%20code,prescription%20or%20illicitly%2Dmanufactured on Jan 24, 2023 [Google Scholar]
- Goodman-Meza D, Arredondo J, Slim S, Angulo L, Gonzalez-Nieto P, Loera A, Shoptaw S, Cambou MC, Pitpitan EV, 2022. Behavior change after fentanyl testing at a safe consumption space for women in Northern Mexico: A pilot study. Int J Drug Policy 106. doi: 10.1016/j.drugpo.2022.103745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoopsick R, Homish G, Leonard K, 2021. Differences in Opioid Overdose Mortality Rates Among Middle-Aged Adults by Race/Ethnicity and Sex, 1999-2018. Public Health Reports 136(2). doi: 10.1177/0033354920968806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, Shover CL, Andrews CM, Bohnert ASB, Brandeau ML, Caulkins JP, Chen JH, Cuéllar M-F, Hurd YL, Juurlink DN, Koh HK, Krebs EE, Lembke A, Mackey SC, Larrimore Ouellette L, Suffoletto B, Timko C, 2022. Responding to the opioid crisis in North America and beyond: recommendations of the Stanford–Lancet Commission. The Lancet 399(10324), 555–604. 10.1016/S0140-6736(21)02252-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson DS, Nguemeni Tiako MJ, Jordan A, 2022. Disparities in Addiction Treatment: Learning from the Past to Forge an Equitable Future. Med Clin North Am 106(1), 29–41. doi: 10.1016/j.mcna.2021.08.008 [DOI] [PubMed] [Google Scholar]
- Lippold K, Ali B, 2020. Racial/ethnic differences in opioid-involved overdose deaths across metropolitan and non-metropolitan areas in the United States, 1999-2017. Drug Alcohol Depend 212. doi: 10.1016/j.drugalcdep.2020.108059 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.