Abstract
Background:
Denervation techniques have increased in popularity for treatment of primary knee osteoarthritis. However, few clinical trials have been conducted on surgical knee denervation. This study was conducted to evaluate the safety and efficacy of a surgical denervation technique for the treatment of primary knee osteoarthritis.
Methods:
Patients were included in the trial if they had failed conservative management for osteoarthritis with corticosteroid injections and were not candidates for total knee arthroplasty. Patients were treated with a surgical knee denervation. Preoperative and postoperative scores were assessed to examine the improvement in pain, function, and quality of life.
Results:
Twenty-four knee denervation procedures were performed in 21 patients. The average follow-up time was 21 months, with a minimum follow-up of 12 months. Patients experienced an improvement in pain with a decrease in visual analogue scale pain scores from 8.7 to 2.9, an improvement in function with a decrease in Western Ontario McMaster Arthritis Score scores from 69 to 32, and an improvement in quality of life with an increase in European quality of life index from 0.183 to 0.646. A clinically significant improvement in pain occurred in 92% of patients, whereas 75% of patients had an improvement in function and 83% had an improvement in quality of life.
Conclusions:
The treatment of recalcitrant knee pain in nonarthroplasty candidates is a difficult issue. This trial suggests that a surgical denervation technique provides improvement in pain, function, and quality of life. Surgical denervation may be a beneficial treatment for patients with recalcitrant pain from primary knee osteoarthritis.
CLINICAL QUESTION/LEVEL OF EVIDENCE:
Therapeutic, IV.
Knee osteoarthritis is a common issue, with rapid increases in prevalence because of an aging population.1 Although total knee arthroplasty continues to provide significant improvement for many patients, an increasing number of patients are not arthroplasty candidates because of increasing issues with comorbidities, most commonly obesity (body mass index >40 kg/m2) and diabetes (hemoglobin A1C level >7%).2,3 Patients who are not arthroplasty candidates have limited options. Recently, the American Academy of Orthopedic surgeons changed recommendations on nonarthroplasty treatment options available for treatment of primary knee osteoarthritis.4 Both corticosteroid injections and hyaluronic acid injections have been downgraded in recommendations, with a suggestion to not use hyaluronic acid, and decreased evidence for the use of cortisone. This leaves many patients, especially those who have experienced failed injection therapy, with only nonsteroidal antiinflammatory or acetaminophen medication as primary treatment options. Therefore, there is a growing number of individuals who do not qualify for an arthroplasty procedure with rapidly decreasing options for treatment of their knee pain.5
In an effort to provide alternative pain management options, surgical denervation procedures that target the geniculate nerves (also known as retinacular nerves) have been developed.6–9 Radiofrequency ablation has been particularly successful and has been shown to be superior to both corticosteroid injections and hyaluronic injections in randomized trials.10,11 However, the effect is only temporary, and patients need to return for treatment every 6 to 12 months.12 Cryotherapy agents that target nerves by “freezing them” have also been developed.13 These drugs are currently being marketed for perioperative pain control in patients undergoing arthroplasty techniques.
Surgical denervation has been suggested for longer lasting pain relief. Dellon et al. have used knee denervation to treat posttraumatic arthritis and postsurgical knee pain.6,7,9 Shi et al., building on work from Dellon et al.,7 were able to use surgical denervation to significantly reduce knee pain in patients who continued to have pain following total knee arthroplasty.14 However, despite previous description of denervation procedures in the knee, there have been few attempts to treat the pain of primary osteoarthritis through a surgical denervation approach.
The present trial was undertaken as a small safety and efficacy trial to examine the role of surgical knee denervation for the treatment of the pain from primary osteoarthritis. Our hypothesis was that surgical denervation would provide equivalent pain control to radiofrequency and cryosurgical ablation, but with longer lasting results.
PATIENTS AND METHODS
Study Design and Inclusion Criteria
A prospective safety and efficacy trial was conducted following Strengthening the Reporting of Observational Studies in Epidemiology guidelines of surgical knee denervation between November of 2020 and February of 2022. Participants were recruited for inclusion in the trial if they had failed conservative management with corticosteroid injections and were not candidates for an arthroplasty procedure. The most common reason patients were not arthroplasty candidates was because of cutoffs at our institution, which include a body mass index greater than 40 kg/m2 and hemoglobin A1C value greater than 7.0%. Candidates also needed to have minimal knee deformity with varus/valgus angulation less than 30 degrees and a flexion contracture less than 30 degrees.
All patients who met initial screening underwent a preoperative diagnostic block with 1% lidocaine of the superomedial, superolateral, inferomedial, and inferolateral geniculate nerves. Inclusion in the trial required that a patient experience a greater than 50% reduction in their pain with diagnostic blocks and had a minimum of 12 months of follow-up. Twelve months of follow-up was selected as the minimum, as 12 months is the upper end of the length of treatment effect expected with radiofrequency ablation. We felt that to provide additional benefit over radiofrequency ablation, surgical denervation would need to have a longer lasting effect than radiofrequency ablation. Exclusion criteria included patients who received concurrent treatment for hip osteoarthritis or lower extremity radiculopathy or neuropathy. These patients were excluded after physical examination by study personnel, as any residual knee pain could be referred pain from the hip or radiculopathy/neuropathy.
The primary outcome measure of the study was improvement in pain measured by the visual analogue scale (VAS). Secondary outcome scores included improvement in function as measured by the Western Ontario McMaster Arthritis Score (WOMAC), and improvement in quality of life measured by the European quality of life index (EQ-5D). The WOMAC score is a composite score of overall knee function, and a decrease in the overall score represents an improvement in function. The EQ-5D is an overall health composite score that represents the general health and quality of life of the patient, and an increase in the score represents an improvement in quality of life. All measures were obtained preoperatively and postoperatively. The patient-reported outcome measures from the last clinical appointment with the longest follow-up available were used in the analysis. Complications were also tracked for the presence of perioperative issues and postoperative complications including infection. Need for revision surgery was also tracked.
Operative Protocol
An adaptation from prior denervation techniques was used for this clinical trial. Prior knee denervation procedures have been described by Shi et al. and Dellon et al.6,7,9,14 These have primarily been focused on secondary denervation procedures for failed prior surgery, with focus on removal of painful neuromas. However, direct open partial denervation of the knee has been described for posttraumatic arthritis by Dellon.6 We modified this technique for a broader approach to the vastus musculature and lateral knee capsule for increased exposure to allow for easy placement of the geniculate nerves into the vastus musculature. The technique targeted the superomedial, superolateral, inferomedial, and inferolateral geniculate nerves. The location of the superomedial and superolateral geniculate nerves adjacent to the medial and lateral vastus musculature provides an easy target for reinnervation.
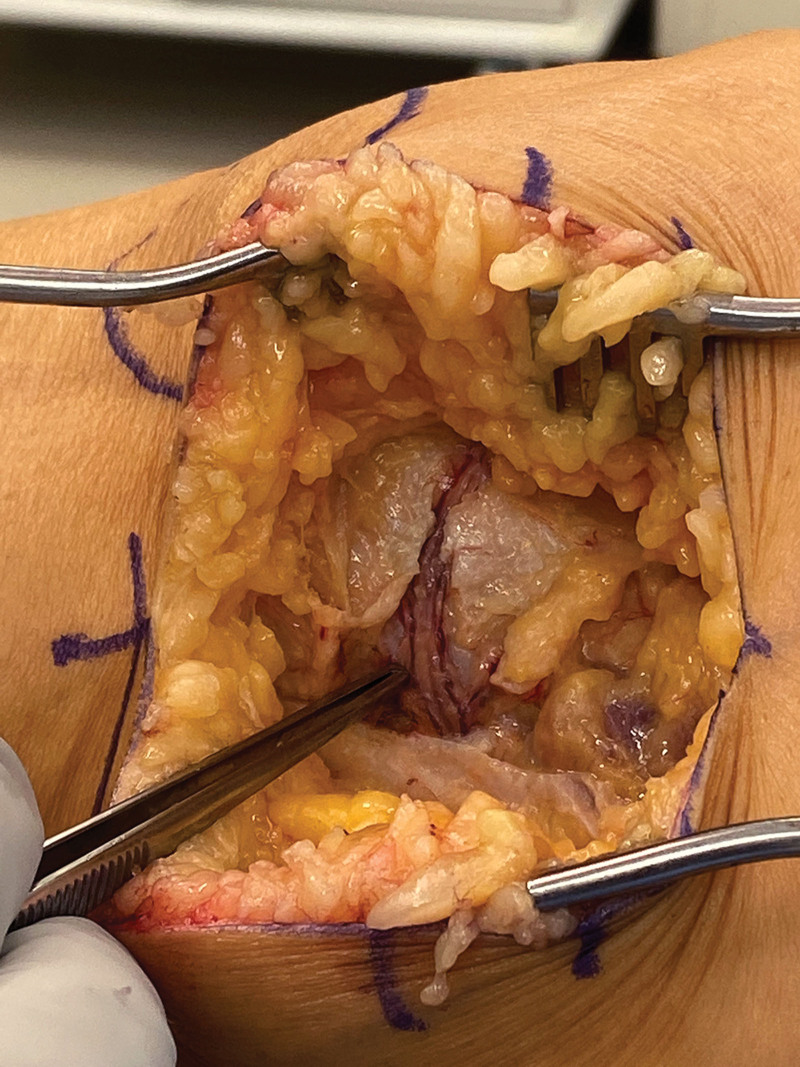
The procedure is conducted with the patient in the supine position with elevation of the operative leg and a bump under the hip. A tourniquet was used for all procedures. Medial and lateral incisions were made in the knee beginning at the distal aspect of the patella and extending 15 cm proximal. Dissection is taken down to the level of the fascia. The fascia is opened in line with the incision. The superomedial or superolateral geniculate nerve is identified just distal to the medial or lateral vastus musculature. It can be traced from its origin in the posterior distal portion of the vastus to its entry on the anterior distal portion of the knee capsule adjacent to the vastus (Fig. 1). The geniculate nerve is then carefully transected at the anterior portion of its entry into the knee capsule. A careful dissection of the nerve is then undertaken to elevate the nerve off the knee capsule without violating the capsule itself. The dissection is taken down to the posterior distal aspect of the vastus where the nerve dives deep in the posterior musculature. This careful dissection allows for an approximately 2.5-cm nerve pedicle that has ample length for placement into the distal vastus.
Fig. 1.
Operative photograph of superolateral geniculate nerve.
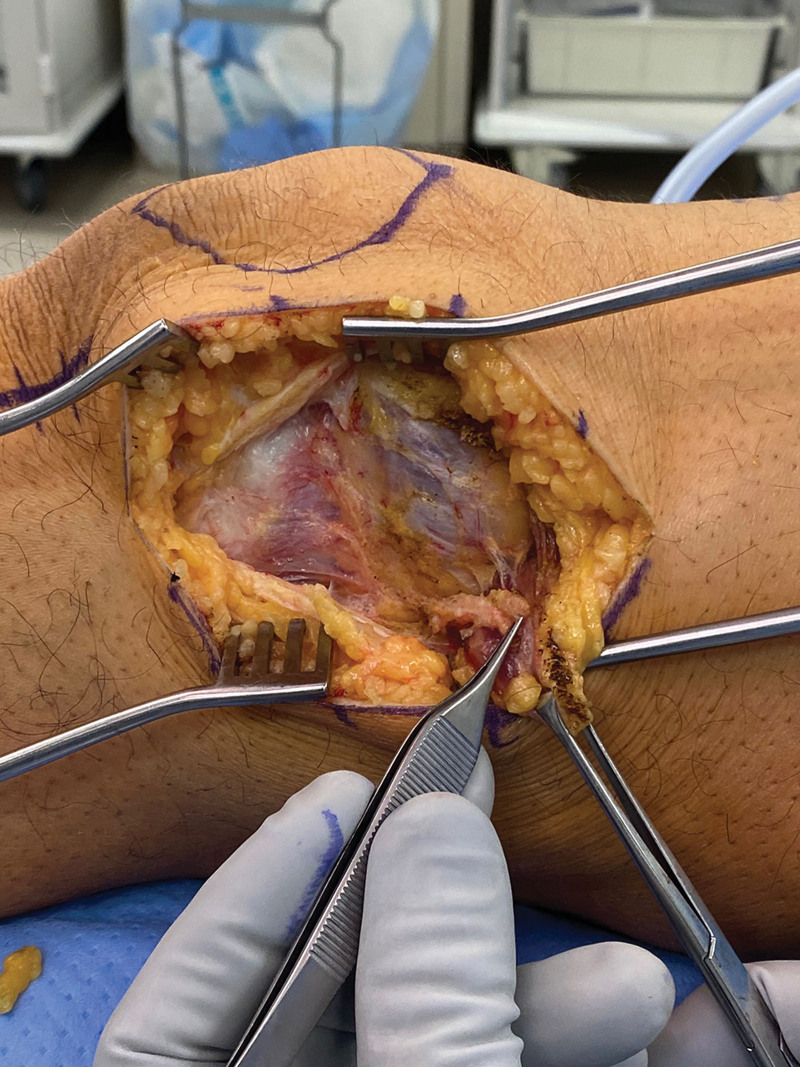
A cuff of the distal vastus musculature is then harvested beginning at the anterior distal aspect of the vastus, to protect the vascular pedicle to the musculature, that arises from the deep posterior portion of the vastus. An approximately 2-cm sleeve of musculature tissue is carefully elevated off of the knee capsule, with care to remain outside the knee joint. The muscle sleeve is elevated and in the process denervated from the surrounding muscle; however, the posterior vascular pedicle is maintained (Fig. 2). The geniculate nerve is then sewn into the distal vastus muscle cuff, and the cuff of muscle is then wrapped around the nerve end and sewn back into its original anatomical position (Fig. 3). This is conducted on both the superomedial and superolateral geniculate nerves. Once the superomedial and superolateral geniculate nerve transections have been successfully conducted, any remaining nerve fibers on the knee capsule are cauterized with the use of bipolar cautery to denervate any remaining nerve ends in the capsule.
Fig. 2.
Operative photograph of superolateral geniculate nerve pedicle.
Fig. 3.
Operative photograph of geniculate nerve placed into vastus muscle.
A separate incision is then made 2 cm anterior to the midline incision, beginning at the most distal aspect of the prior incision and carried down for an additional 3 cm. Dissection is taken down to the level of the fascia, with care to identify and transect the inferomedial and inferolateral geniculate nerves. These nerves tend to fan out in this area, and multiple nerve branches can be identified traversing the infrapatellar area. The fascial layers are then closed both medially and laterally in the midline incisions. The wound is then closed in layers, with the use of 2-0 Vicryl suture and 3-0 nylon horizontal mattress sutures.
Postoperatively, the patients are placed in a hinged knee immobilizer locked in extension to protect the medial and lateral incisions from wound breakdown from tension while bending the knee. Patients are weight bearing as tolerated but with the knee to remain in extension for the first 2 weeks. Patients return for suture removal at 2 weeks and immediately begin stretching and strengthening with physical therapy once incisions are fully healed. After 2 weeks, there are no additional restrictions on movement. Patients are weight bearing as tolerated throughout the entire postoperative rehabilitation.
Statistical Analysis
Descriptive statistics were used to describe the patient population. Paired t tests for parametric data were used to examine the differences between preoperative and postoperative VAS pain, WOMAC, and EQ-5D scores. Predetermined minimal clinically important difference (MCID) ratios were used from published literature to examine the percentage of patients who experienced a clinically significant improvement. The MCID values used in the study were chosen from the knee arthroplasty literature for postoperative improvement and were 2 for VAS,15 10 for WOMAC,16 and 0.085 for EQ-5D.17 The percentage of patients who exceeded the MCID was reported. Institutional review board approval was obtained for this study, and all participants provided consent to participate in the research study. IBM SPSS version 22 was used for all statistical analysis, with significance defined at P < 0.05.
RESULTS
Twenty-one patients (24 knees) participated in the research study; 54% were women, with an average age of 68 ± 10 years (range, 45 to 90 years). The average follow-up for the study population was 21 months (range, 12 to 27 months; with a minimum of 12 months). All patients had radiographic signs consistent with end-stage degenerative joint osteoarthritis and had failed conservative treatment including corticosteroid injections, but were not candidates for arthroplasty.
Patients in the study experienced an improvement in the primary outcome measure, the VAS for pain, from 8.8 ± 1.4 preoperatively to 2.9 ± 2.2 postoperatively (P < 0.05). Improvements were also seen in the secondary outcome measures, with an improvement in the WOMAC score, from 69.1 ± 23.8 preoperatively to 32 ± 27.4 postoperatively (P < 0.05), and an improvement in the EQ-5D from 0.183 preoperatively to 0.646 postoperatively (P < 0.05) (Table 1). No patients in the study experienced a postoperative complication, with no measured perioperative morbidity and no postoperative infections or revisions required.
Table 1.
Preoperative and Postoperative Patient-Reported Outcome Scores of Patients Treated with Open Denervation
| Outcome Measure | Preoperative Score (Mean ± SD) | Postoperative Score (Mean ± SD) | P |
|---|---|---|---|
| VAS pain | S8.8 ± 1.4 | 2.9 ± 2.2 | <0.05 |
| WOMAC | 69.1 ± 23.8 | 32.3 ± 27.4 | <0.05 |
| EQ-5D | 0.18 ± 0.24 | 0.65 ± 0.29 | <0.05 |
The percentage of patients surpassing the MCID threshold was calculated to determine the clinical significance of the research findings. Ninety-two percent of patients experienced clinically meaningful improvement in pain, 75% experienced clinically meaningful improvement in function, and 83% experienced clinically meaningful improvement in quality of life. Average improvements for the study population exceeded the MCID for each of the study variables (Table 2).
Table 2.
Average Scores of Outcome Variables, Published MCIDs, and Percentages of Patients Reaching MCID with Surgical Denervation
| Outcome Measure | Average Patient Score (Mean ± SD) | Published MCIDs | Patients Achieving MCID (%) |
|---|---|---|---|
| VAS pain | −5.8 ± 2.6 | −2 | 92 |
| WOMAC | −36.8 ± 30 | −10 | 70 |
| EQ-5D | 0.510 ± 0.330 | 0.085 | 83 |
DISCUSSION
This study was conducted to examine the effect of surgical knee denervation for the treatment of the pain from primary knee osteoarthritis. The surgical technique was shown to decrease pain, increase function, and improve quality of life. Notably, these results were found in patients in whom all other nonsurgical treatment options had failed and who were not candidates for arthroplasty. Patients reported continued pain relief throughout the postoperative recovery period, which has lasted on average 21 months.
These results suggest that surgical denervation may be considered a treatment option for patients whose alternative treatments for osteoarthritis have failed and who are not candidates for arthroplasty. Our results are similar to results seen with other nerve-related procedures at the knee, including radiofrequency ablation. In a randomized trial of radiofrequency ablation versus corticosteroid injection, Davis et al. found an average reduction of 4.8 points on the VAS pain scale for patients treated with radiofrequency ablation at 6 months.10 Our results of denervation show a larger benefit, with a decrease of 5.8 points on the VAS pain scale at an average of 21 months. Similarly, in another trial, Chen et al. showed a decrease of 33 points in WOMAC scores at 6 months with radiofrequency ablation.11 Our surgical denervation group experienced a decrease in WOMAC scores of 36 at 21 months. Although the outcome scores of radiofrequency ablation are similar to surgical denervation, the results of radiofrequency ablation are limited in their average return of symptoms. Treatment with radiofrequency ablation provides relief for an average of 6 to 12 months.12 Our study had an average follow-up of 21 months, with minimal return of symptoms, with the longest follow-up being 27 months. The time extent of pain relief with denervation is still unknown, but these data suggest that it may provide longer lasting pain relief than radiofrequency ablation and may be permanent. Longer-term studies are needed to examine the overall length of symptom relief. Randomized studies also may be conducted between radiofrequency or cryoablation and surgical denervation to determine the relative risks and benefits, and the costs associated with these procedures.
We sought to understand the clinical applicability of the study findings by examining the percentage of patients who surpassed minimal standards in clinical improvement as evidenced by MCID values. We chose the primary outcome of our study as pain, as that was the primary clinical concern in the population in whom all other treatment options had failed. We found that 92% of patients experienced an improvement in pain above the MCID for VAS, suggesting a significant and long-lasting pain relief following the procedure. We also found that 75% of patients experienced clinically meaningful improvements in function above the MCID for WOMAC, and 83% of patients experienced an improvement in quality of life above the MCID for EQ-5D. These values are similar to patients who have been treated with primary knee arthroplasty.17–21 The MCID ratios published in primary knee arthroplasty are 2 for VAS,15 10 for WOMAC,16 and 0.085 for EQ-5D.17 Our results show an average improvement above the MCID for all three study measures.
Our study had many limitations. We conducted only a small number of these cases. The surgical technique was devised based on prior anatomical and clinical studies but had not been fully tested in the target population. We therefore felt that it was most prudent to try a small number of these procedures in patients who did not have good alternatives and follow up these patients for a significant amount of time before conducting more studies. Therefore, this trial should be considered more of an initial safety and efficacy trial than an actual clinical trial. We are also limited in our postoperative radiographic follow-up. A majority of this study was conducted during the COVID-19 pandemic and we therefore had very few patients return for in-person clinical follow-up. We had originally planned to get 1-year radiographic follow-up on each patient but elected for only patient-reported outcome scores that could be reported over the phone because of the at-risk health status of many of the participants. Finally, we used patient-reported outcome scores as the primary outcome measure. These outcome scores are sensitive to patient emotional and psychosocial traits that have been shown to affect patient-reported scores in the arthroplasty literature.22–26 This relatively small cohort is particularly susceptible to selection and recall bias, given that they had no other option for the management of their pain. Despite these limitations, the results of this trial are promising, especially for at-risk patients who are not candidates for arthroplasty.
Furthermore, the exact nerve targets for denervation procedures and the resulting clinical outcomes may need additional study. The anatomical guidance we used for nerve blocks and surgery in this study was chosen based on a 2011 study by Choi et al. in the pain management literature.27 However, on additional study, we have noticed some discrepancies in the description of nerve targets. In reviewing their first article on radiofrequency ablation, we noticed that Choi et al. relied on the original knee joint innervation article by Horner and Dellon, which has neither the inferomedial or the inferolateral nerves in it.8 That is the article that named the medial and lateral retinacular nerves, which the pain management literature changed to the superomedial and superolateral genicular nerves, similar to the arteries in the same location. Although there are inferomedial and inferolateral geniculate arteries, there are no nerves in those locations. After noticing this discrepancy, we realize that the inferomedial nerve we removed was a saphenous nerve branch, and indeed, our patients had infrapatellar numbness postoperatively. The clinical applicability of this, and its associated results on patient-reported outcomes, remains unclear and should be further examined in future studies.
CONCLUSIONS
This study found that surgical knee denervation provides decreases in pain, improvement in function, and improvement in quality of life for patients with primary, recalcitrant osteoarthritis. Further studies are needed to examine treatment effects in larger populations, and in randomized controlled trials, especially in comparison to radiofrequency or cryoablation and arthroplasty. Our results suggest that patients undergoing surgical denervation may have equivalent outcomes as compared with radiofrequency ablation, with longer lasting results, limiting the need for continued retreatment seen with ablation. Surgical denervation may be a good treatment option for at-risk patients with recalcitrant primary knee osteoarthritis who are not candidates for arthroplasty.
DISCLOSURE
No author associated with this article has disclosed any potential or pertinent conflicts, which may be perceived to have impending conflict with this work.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Deshpande BR, Katz JN, Solomon DH, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res. 2016;68:1743–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gossec L, Paternotte S, Maillefert JF, et al.; OARSI-OMERACT Task Force “total articular replacement as outcome measure in OA.The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: an international cross-sectional study of 1909 patients. Report of the OARSI-OMERACT Task Force on total joint replacement. Osteoarthritis Cartilage 2011;19:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamaruzaman H, Kinghorn P, Oppong R. Cost-effectiveness of surgical interventions for the management of osteoarthritis: a systematic review of the literature. BMC Musculoskelet Disord. 2017;18:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Orthopaedic Surgeons. Management of osteoarthritis of the knee (nonarthroplasty) evidence-based clinical practice guideline. Available at: https://www.aaos.org/oak3cpg. Accessed May 15, 2023. [Google Scholar]
- 5.Dhawan A, Mather RC, Karas V, et al. An epidemiologic analysis of clinical practice guidelines for non-arthroplasty treatment of osteoarthritis of the knee. Arthroscopy 2014;30:65–71. [DOI] [PubMed] [Google Scholar]
- 6.Dellon AL. Partial joint denervation II: knee and ankle. Plast Reconstr Surg. 2009;123:208–217. [DOI] [PubMed] [Google Scholar]
- 7.Dellon AL, Mont MA, Krackow KA, Hungerford DS. Partial denervation for persistent neuroma pain after total knee arthroplasty. Clin Orthop. 1995;316:145–150. [PubMed] [Google Scholar]
- 8.Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop. 1994;301:221–226. [PubMed] [Google Scholar]
- 9.Dellon AL, Mont MA, Mullick T, Hungerford DS. Partial denervation for persistent neuroma pain around the knee. Clin Orthop. 1996;329:216–222. [DOI] [PubMed] [Google Scholar]
- 10.Davis T, Loudermilk E, DePalma M, et al. Prospective, multicenter, randomized, crossover clinical trial comparing the safety and effectiveness of cooled radiofrequency ablation with corticosteroid injection in the management of knee pain from osteoarthritis. Reg Anesth Pain Med. 2018;43:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen AF, Khalouf F, Zora K, et al. Cooled radiofrequency ablation compared with a single injection of hyaluronic acid for chronic knee pain: a multicenter, randomized clinical trial demonstrating greater efficacy and equivalent safety for cooled radiofrequency ablation. J Bone Joint Surg Am. 2020;102:1501–1510. [DOI] [PubMed] [Google Scholar]
- 12.Iannaccone F, Dixon S, Kaufman A. A review of long-term pain relief after genicular nerve radiofrequency ablation in chronic knee osteoarthritis. Pain Physician 2017;20:E437–E444. [PubMed] [Google Scholar]
- 13.Roth ZA, Sutton K, Wenende J, Pecka S. Preoperative cryoneurolysis for total knee arthroplasty: a case series. J Perianesthesia Nurs. 2023;38:33–38. [DOI] [PubMed] [Google Scholar]
- 14.Shi SM, Meister DW, Graner KC, Ninomiya JT. Selective denervation for persistent knee pain after total knee arthroplasty: a report of 50 cases. J Arthroplasty 2017;32:968–973. [DOI] [PubMed] [Google Scholar]
- 15.Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS. How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty 2018;33(Suppl):S71–S75.e2. [DOI] [PubMed] [Google Scholar]
- 16.Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. What is the minimum clinically important difference for the WOMAC index after TKA? Clin Orthop Relat Res. 2018;476:2005–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yapp LZ, Scott CEH, Howie CR, MacDonald DJ, Simpson AHRW, Clement ND. Meaningful values of the EQ-5D-3L in patients undergoing primary knee arthroplasty. Bone Joint Res. 2022;11:619–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Escobar A, Quintana JM, Bilbao A, Aróstegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage 2007;15:273–280. [DOI] [PubMed] [Google Scholar]
- 19.Giesinger JM, Hamilton DF, Jost B, Behrend H, Giesinger K. WOMAC, EQ-5D and Knee Society score thresholds for treatment success after total knee arthroplasty. J Arthroplasty 2015;30:2154–2158. [DOI] [PubMed] [Google Scholar]
- 20.Giesinger K, Hamilton DF, Jost B, Holzner B, Giesinger JM. Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthritis Cartilage 2014;22:184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der Wees PJ, Wammes JJG, Akkermans RP, et al. Patient-reported health outcomes after total hip and knee surgery in a Dutch university hospital setting: results of twenty years clinical registry. BMC Musculoskelet Disord. 2017;18:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams DP, Price AJ, Beard DJ, et al. The effects of age on patient-reported outcome measures in total knee replacements. Bone Joint J. 2013;95-B:38–44. [DOI] [PubMed] [Google Scholar]
- 23.Felix J, Becker C, Vogl M, Buschner P, Plötz W, Leidl R. Patient characteristics and valuation changes impact quality of life and satisfaction in total knee arthroplasty—results from a German prospective cohort study. Health Qual Life Outcomes 2019;17:180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Escobar A, Quintana JM, Bilbao A, et al. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology (Oxford) 2007;46:112–119. [DOI] [PubMed] [Google Scholar]
- 25.Kazarian GS, Anthony CA, Lawrie CM, Barrack RL. The impact of psychological factors and their treatment on the results of total knee arthroplasty. J Bone Joint Surg Am. 2021;103:1744–1756. [DOI] [PubMed] [Google Scholar]
- 26.Kim MS, Koh IJ, Choi KY, Seo JY, In Y. Minimal clinically important differences for patient-reported outcomes after TKA depend on central sensitization. J Bone Joint Surg Am. 2021;103:1374–1382. [DOI] [PubMed] [Google Scholar]
- 27.Choi WJ, Hwang SJ, Song JG, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain 2011;152:481–487. [DOI] [PubMed] [Google Scholar]