Abstract
Background and Aims:
The objective of the study was to evaluate the performances of qCON and qNOX indices in pediatric populations undergoing surgery under general anesthesia (GA), focusing on the induction and recovery periods. Both the indices are derived from electroencephalogram (EEG) and implemented in the CONOX monitor (Fresenius Kabi, Germany).
Material and Methods:
After approval of the institutional ethics committee, this prospective observational study was conducted in pediatric patients of either sex in the age group of 1–12 years belonging to the American Society of Anesthesiology (ASA) grade I and II undergoing elective surgery under GA. Anesthetic technique was GA with or without regional analgesia (RA). All patients underwent inhalation induction and maintenance using sevoflurane. Patients were monitored with the use of a CONOX monitoring system (Fresenius Kabi, Germany), connected via a set of electrodes placed over the forehead. qCON and qNOX scores were recorded during awake (on operating table premedicated with oral midazolam 0.5 mg/kg), at induction, at loss of eyelash reflex, intubation/laryngeal mask airway (LMA) insertion, before and after regional anesthesia, surgical incision, at cessation of anesthesia, emergence, extubation, and eye-opening. Registered results were also analyzed compared with the minimum alveolar concentration of sevoflurane (MAC).
Results:
A total of 46 pediatric patients were enrolled in the study with a mean age of 5.6 years. All the patients were either ASA I or II. There was a simultaneous fall and rise of qCON and qNOX upon induction and recovery, respectively. There was a rise in qNOX with surgical incision irrespective of RA. However, there was a greater rise in qNOX following surgical incision in those who did not receive RA (P = 0.33) Also both qCON (P = 0.06) and qNOX (P = 0.41) were poorly correlated with MAC values of sevoflurane during GA in the pediatric population.
Conclusions:
Both qCON and qNOX values change predictably with changes in the conscious level and with different noxious stimuli. Further studies are required to confirm the findings taking into account the postoperative assessment of delirium and recall of intraoperative events.
Keywords: General anesthesia, pediatric surgery, qCON, qNOX
Introduction
Depth of anesthesia is the degree to which the central nervous system (CNS) is depressed by an anesthetic agent at a well-defined concentration in which it is administered.[1] An inadequate dosage of general anesthetic (GA) drugs can cause unintended awareness. On the other hand, unwanted effects of anesthetic drugs lead to complications such as postoperative vomiting, respiratory complications, laryngospasm, delayed extubation, shivering, agitation, and delirium.[2] There are commercially available devices that can measure the end-tidal concentration of volatile anesthetic agents or predict the plasma concentration of intravenous anesthetic agents, but they do not measure the effects of these drugs on brain activity. Hence, an electroencephalogram (EEG)-based device may be useful for monitoring the anesthetic depth. They also enable a safe, and cost-effective anesthetic procedure. qCON and qNOX are parameters extracted from the raw EEG using an adaptive neuro-fuzzy inference system (ANFIS), which generates the output on a 0–99 scale. Previous studies in adults established that the qCON is a biomarker of the hypnotic effect under GA and that the qNOX might be a surrogate measure of the effects of opioids and nociception on the EEG activity.[3] The objective of the study was to evaluate the performances of qCON and qNOX indices in pediatric patients receiving GA for various surgical procedures, by focusing on the induction and recovery periods. After estimating the qCON and qNOX values below which the loss of consciousness and loss of response to nociceptive stimulation are achieved, the fall and rise values of qCON and qNOX were noted in association with the regional analgesia (RA) provided. This study was conducted to provide a deeper analysis of the behavior of the qCON and the qNOX as indices of consciousness and probability of response to nociceptive stimulation in the pediatric population under GA.
Material and Methods
After obtaining institutional ethics committee’s approval (IEC no: 164/2020, dated: 10 Dec 2020) and written informed consent, this prospective observational study was conducted in a tertiary care hospital and in accordance with applicable consort guidelines. This study is also registered under the Clinical Trial Registry of India (CTRI), Registration No. CTRI/2021/03/032092, dated 17/03/2021. A total of 46 pediatric patients of both sexes, the American Society of Anesthesiology (ASA) grade I and II and age group of 1 to 12 years undergoing surgeries under GA were enrolled from Jun 1, 2021 to Jun 31, 2022. The primary objective of the study was to clinically evaluate qCON and qNOX indices for depth of anesthesia and the response of the patient to noxious stimulus, respectively, in pediatric population. The secondary outcomes were to study the correlation between qCON index with the consciousness level and MAC of anesthetic drug to track changes in the effects of anesthetics in the brain and the qNOX index with the response of the patient to noxious stimulus.
The anesthetic technique was GA with or without RA. All children were premedicated with midazolam 0.5 mg/kg orally 20–30 min prior to the proposed time of induction. All patients underwent inhalation induction using sevoflurane (incremental induction) until loss of eyelash reflex (LOER), with a mean induction time of 1–2 min. Fentanyl 1–2 μg/kg and neuromuscular block with atracurium 0.5 mg/kg were given to facilitate tracheal intubation or laryngeal mask airway (LMA) insertion. Anesthesia was maintained using sevoflurane (minimum alveolar concentration [MAC] 0.7–1.2). If no contraindication exists, RA in the form of caudal epidural or thoracic epidural was provided on a case-to-case basis. Bupivacaine 0.25% and volume as per the Armitage formula[4] was given in caudal block, and a bolus dose of bupivacaine 0.25% at 0.3 mL/kg followed by continuous infusion of bupivacaine 0.1% with fentanyl 1 μg/mL at 0.3 mL/kg/h was given in thoracic epidural.
Apart from the demographic profile of the patient, operative data included heart rate (HR), blood pressure (BP), mean arterial pressure (MAP), pulse oximetry reading (SpO2), and end-tidal concentration of sevoflurane. Each patient was monitored with the use of the CONOX-37128 monitoring system (Fresenius Kabi, Germany). Both qCON and qNOX indices were recorded during awake, induction, at the loss of verbal command, LOER, intubation/LMA insertion, surgical incision, at the cessation of anesthesia, extubation, eye-opening, and emergence (defined as spontaneous breathing and eye-opening for more than 5 s). The EEG was recorded with the CONOX monitor. The EEG was automatically stored in a binary file while the indices of qCON, qNOX, electromyography (EMG), and signal quality index (SQI) were stored in a text file. Any EEG-derived qCON and qNOX data, which have poor signal quality (defined as SQI <50) were rejected.
All the intraoperative data collected were entered into an Excel sheet and analyzed using a statistical package for the social sciences (SPSS) software (IBM SPSS Statistics 21, Chicago IL). A study by Jensen et al. (2014)[3] showed that the difference between the mean of qCON before and after the loss of consciousness under GA was 10 with a standard deviation (SD) of 20. According to Sullivan[5] with these conditions the necessary sample size is 42 with a power of 0.9 and a level of significance of 0.05. The sample size arrived at 46 by adding 10% for loss of compounding.
The distribution of the continuous data was tested with the Kolmogorov–Smirnov one-sample test. Continuous variables with a normal distribution have been expressed as means ± SD. Dichotomous data have been expressed as numbers and percentages. Continuous data were analyzed using Student’s t test while Chi-square test was used for categorical variables. Obtained laboratory data were analyzed using a one-way ANOVA test. The Pearson correlation was also used to measure the strength of the linear relationship between qCON and MAC of sevoflurane. Any P value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS software.
LOER was assessed during the transition from awake to anesthetized, defining the state of LOC. The values for qCON and qNOX awake were the mean qCON and qNOX values of 1-min interval immediately before starting the inhalational induction while the anesthetized value was the mean taken over the 1-min interval immediately after the loss of consciousness (LOC). The changes in values of qCON and qNOX were noted over the 1-min post-LMA insertion, laryngoscopy, or tracheal intubation and surgical incision. The mean value and the SD for the qCON and qNOX were calculated.
Results
All the pediatric patients admitted for surgeries were enrolled from Jun 1, 2021 to Jun 31, 2022. A total of 72 patients underwent surgery under GA. Twenty-two patients were excluded from the study on account of various reasons as listed in Figure 1. The most common surgeries were urogenital (20), followed by gastrointestinal (13), musculoskeletal (6), and others (7).
Figure 1.
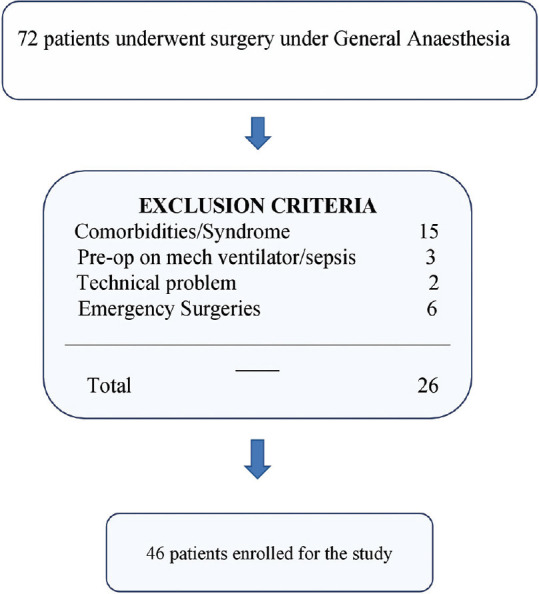
Consort diagram
The demographic profile of patients is listed in Table 1. The mean age was 5.6 ± 3.6 years, and the male sex was predominant with 26 out of 46 patients. The airway was secured using laryngeal mask airway (LMA) in 33 patients and with an endotracheal tube in 13 patients. The use of LMA was statistically significant with a P value of 0.003 in comparison with endotracheal intubation. RA was given to 21 (43.8%) patients, and most of whom underwent urogenital surgeries.
Table 1.
Patient demographic characteristics and baseline intraoperative variables P<0.05* is considered significant
| Parameters | n=46 | RA + | RA − | t/Chi-square value* | P | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean (%) | ±SD/ | n=21 | n=25 | ||||
| Age (years) | 5.6 | 3.6 | 5±2.7 | 6.1±4.1 | −1.1 | 0.28 | |
| Sex (Male) | 28 (60.9%), P=0.14 | 12 (57.1%) | 16 (64%) | 0.23* | 0.63 | ||
| Weight (kg)* | 21.5 | 10.3 | 20.8±9.8 | 22±10.9 | −0.42 | 0.68 | |
| ASA Category | |||||||
| I | 24 (52.2%) | 13 (61.9%) | 11 (44%) | 2.02* | 0.36 | ||
| II | 22 (47.8%) | 8 (38.1%) | 14 (56%) | ||||
| Regional Anesthesia | 21 (43.8%) | 0.35 | 0.56 | ||||
| Airway (for use of supraglottic airway Vs ETT; P=0.003) | |||||||
| I-Gel (supraglottic) | 33 (71.7%) | 17 (81%) | 16 (64%) | 1.62* | 0.20 | ||
| Endotracheal tube | 13 (28.3%) | 4 (19%) | 9 (36%) | ||||
| qCON (Baseline) | 96.6 | 5.4 | 95±7.5 | 98±2 | −1.8 | 0.08 | |
| qNOX (Baseline) | 96.7 | 3.7 | 96.9±3.9 | 97±3.7 | −0.16 | 0.87 | |
| Difference in qCON before and after LOER | 14.7 | 10.3 | - | - | 9.7 | <0.001 | |
| - | - | 30.4±16.6 | 24.4±14.3 | 1.3 | 0.2 | ||
| Difference in qCON before and after extubation | 31.9 | 23.7 | - | - | −13.6 | <0.001 | |
| - | - | 31.2±12.5 | 32.4±18.4 | −0.27 | 0.79 | ||
| Difference in qNOX before* and after RA | - | - | 6.9±14.3 | - | 0.04 | ||
| Difference in qNOX before* and after Surgical incision | 5.2 | 24.3 | - | - | 1.5 | 0.15 | |
| - | - | 1.5±19.8 | 8.4±27.6 | −0.98 | 0.33 | ||
RA, regional analgesia; ASA, American Society of Anesthesiology; ETT, endotracheal tube; LOER, loss of eyelash reflex; *P value of <0.05 considered significant
The mean values for qCON for awake and LOC were 96.6 and 81.9, respectively. The difference in qCON value before and after the loss of eyelash reflex is 14.7 with a P value of <0.001, which was statistically significant. Similarly, the difference in qCON before and after extubation was 31.9 with an SD of 23.7 and a significant P value of <0.001. However, the mean qCON value before and after giving RA were 30.4 and 24.4 with a P value of 0.2, which was not statistically significant. The mean value for qNOX for awake was 96.7 with an SD of 3.7. A significant fall in qNOX after giving RA was noted with a difference in qNOX of 6.9 with SD of 14.3 before and after RA (P = 0.004).
There was a simultaneous fall and rise of qCON and qNOX upon induction and recovery, respectively, but it poorly correlated with the MAC of sevoflurane upon induction and recovery with a P value of 0.06 (qCON) and 0.41 (qNOX) and there was no significant correlation between qCON and qNOX with MAC noted as in Figure 2.
Figure 2.
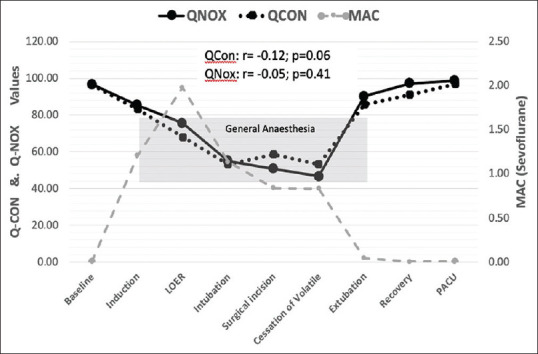
qCON and qNOX indices compared with Minimum Alveolar Concentration (MAC) of sevoflurane during general anesthesia
The effect of RA was compared with intraoperative parameters such as HR, BP, MAP, and MAC of sevoflurane along with qCON and qNOX. There was a statistically significant fall in HR (P = 0.01) and qNOX (P = 0.04) after RA was noted as listed in Table 2. At the same time, there was no significant fall in systolic, diastolic, and mean arterial blood pressure noted after RA [Figure 3].
Table 2.
Effect of Regional Analgesia (only patients receiving RA)
| n=21 | Before RA | After RA | t | P |
|---|---|---|---|---|
|
| ||||
| Mean±S | ||||
| Heart Rate (HR) beats/min | 106.7±18.5 | 98.9±18.5 | 2.7 | 0.01* |
| Systolic Blood Pressure (SBP) mmHg | 91.6±10.7 | 88.9±7.3 | 1.8 | 0.09 |
| Diastolic Blood Pressure (DBP) mmHg | 53.2±9.1 | 50.6±5.6 | 1.9 | 0.07 |
| Mean Arterial Pressure (MAP) mmHg | 66.6±8.5 | 63.9±5.5 | 2.3 | 0.03 |
| qCON | 50.8±8.4 | 49.5±8.3 | 0.8 | 0.43 |
| qNOX | 45.4±14.3 | 38.5±9.1 | 2.2 | 0.04* |
| Minimum Alveolar Concentration of Sevoflurane (MAC) | 0.97±0.2 | 0.95±0.2 | 0.7 | 0.52 |
RA, regional analgesia; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; MAC, minimum alveolar concentration; t value, Student’s t test; *P<0.05 considered significant
Figure 3.
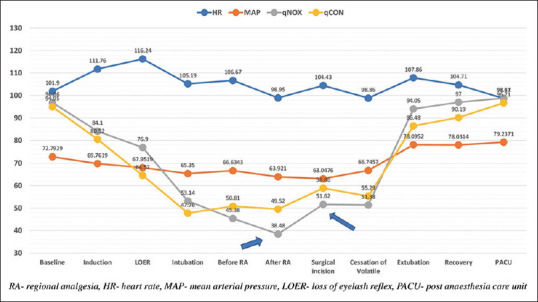
Effect of RA ( Only patients receiving RA)
A Pearson correlation was run to determine the relationship between qCON and MAC of sevoflurane during GA. There was a weak, negative correlation between them, which was statistically not significant (r = −0.115, P = 0.06) as shown in Figure 4.
Figure 4.
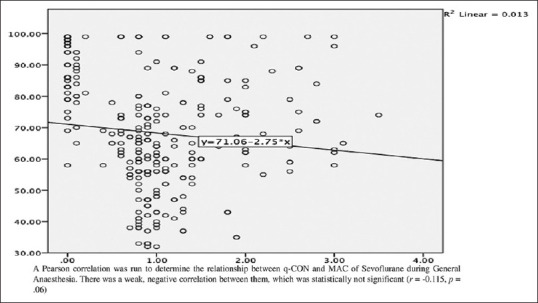
Scatter plot showing weak association between qCON and MAC
Discussion
It is important to monitor the depth of general anesthesia to deliver the optimal dose of general anesthetic to patients, thereby preventing unintended intraoperative awareness and side effects due to an overdose of anesthetic agents. The EEG-based depth of general anesthesia monitors provides noninvasive monitoring of brain neurophysiology under general anesthesia, as the amplitude and frequency of EEG are inversely related to the anesthetic dose administered.[6] Several trials evaluated the benefits of devices such as the Bispectral Index (BIS), Entropy, Narcotrend, Cerebral State Index (CSI), etc., during GA in adults. However, only limited studies reliably evaluated the performance of the depth of anesthesia monitors in children.[7,8,9] qCON and qNOX are newer indices shown to change predictably with changes in conscious level and noxious stimulation, respectively, in the adult population.[10] Studies suggest that the performance of qCON is comparable with BIS in adults.[11]
Melia et al.[10] conducted a study on 160 adult patients and found that the fall of qCON during induction was faster than qNOX and the rise of qNOX was faster than qCON during recovery from anesthesia. However, in this study, there was an almost simultaneous fall in both qCON and qNOX indices upon induction and a rise while recovery. Probably, a larger sample size could be more forthcoming on the fall and rise of the indices in the pediatric population. A reduction in the mean value of about 20 from the baseline was noted during LOER and an increase in the mean value of about 41 during tracheal extubation/recovery from GA was observed in qCON indices (P < 0.001). This implies that qCON was successfully following the neural pattern of general anesthesia and its value changes predictably during both loss of consciousness and recovery from GA.
Jensen et al.[3] conducted a study on 60 adult patients and concluded that there was a significant increase in both qCON and qNOX as a response to noxious stimulation. However, in this study, no change in qCON was noted in response to surgical incision irrespective of whether the patient received successful regional analgesia or not. qNOX did increase with surgical incision, though the rise was less in patients receiving RA. It was observed that there was a significant fall in qNOX following RA (45.4 vs 38.5, P = 0.04) as shown in Table 2. This indicates that qNOX does follow the pain sensation perceived by the patient and any reduction in pain is accompanied by a reduction in qNOX values. qCON on the other hand failed to respond to either perceived pain or relief of pain.
The influence of age on indices, namely, Entropy, Narcotrend, BIS, qCON/qNOX, and Treaton MGA-06 was evaluated by Obert et al[12]. They found that all indices significantly increased with patient’s age except Narcotrend.[11] This might lead to the use of a high dose of anesthetic, especially in elderly patients. But the trend of these indices in the pediatric population has still not been studied. Beekoo et al.[7] conducted a study on 135 patients in the age group of 0–80 years undergoing GA with sevoflurane and concluded that BIS values are misleading in the pediatric age group of 0–6 years. We on the other hand found that in the pediatric age group, LOC happened at qCON values of 70–80 as against the values of 40–60 for LOC in adult patients. Also, from many other studies in the pediatric age group, it is evident that EEG-based monitors such as BIS values have interindividual variation and end-tidal sevoflurane correlation compared with adults.[8,9] Even in this study, the mean values of qCON and qNOX are greater than those for adults during LOC and recovery from anesthesia, but both indices were able to follow LOC and recovery with significant fall and rise.
Bergmann et al.[13] studied surgical pleth index (SPI) in 170 adult patients undergoing orthopedic surgeries and concluded that SPI monitoring has reduced the consumption of propofol and remifentanil intraoperative and also early postoperative recovery. Soral et al.[14] evaluated analgesia nociception index (ANI) in 102 adult patients undergoing procedural sedation and found that reduced opioid consumption and no impact on propofol and ketamine consumption. Many other studies on pupillary pain index (PPI), nociception level index (NOL), and surgical stress index (SSI) suggested a reduction in intraoperative opioid consumption and post-op adverse events[15] Few studies have clearly indicated that parameters such as HR and BP are poor indicators of noxious stimuli, especially in children.[16,17] qNOX is derived from raw EEG and EMG reading from the patient, it is independent of factors such as heart rate, blood pressure, peripheral vascular tone, etc., Also, significant changes in qNOX after RA and surgical incision were noted in our pediatric cases. It signifies that the qNOX value changes predictably in accordance with noxious stimuli in the pediatric age group.
Even though this study does not have a control group to compare the intraoperative opioid consumption with the qNOX index, there was a rise observed in qNOX with the surgical incision. As described earlier, there was a greater rise in qNOX following surgical incision in patients who did not receive RA (P = 0.33). This is an indication that qNOX could not only be a reliable indicator of nociceptive stimulus but could also measure the adequacy of analgesia, which might help prevent an overdose of opioids.
Makkar et al.[18] conducted a study on 42 children of age group 1–8 years undergoing surgery under GA using desflurane and LMA placement with or without regional analgesia. They compared the MACBIS50 values of the group, which received RA and those who did not receive RA. They found that the RA group had a lesser MACBIS50 value for maintenance compared with the non-RA group. In a study by Aantaa et al.,[19] it was found that ED50 of sevoflurane is lesser for LMA insertion compared with endotracheal intubation. Another study in children found a significant decrease in sevoflurane requirements to maintain BIS ≤ 50 during combined anesthesia (general + regional). This study has demonstrated a fall in the qNOX index after RA but no significant change in sevoflurane requirement irrespective of RA.
MAC of inhalational agents such as sevoflurane and desflurane is reduced by the use of balanced anesthesia (use of muscle relaxant), regional analgesia, and also LMA placement. In this study, muscle relaxant was given to all the patients and most of the patients were inserted with LMA and a significant number of cases were given RA as well. These factors might have led to lower consumption of sevoflurane and lesser MAC values and its insignificant correlation between the MAC of sevoflurane and qCON and qNOX indices.
Many studies have compared the qCON and qNOX indices with intravenous anesthetic agents such as propofol and remifentanil and only a few studies compared the qCON index with inhalational agents such as sevoflurane and desflurane. In this study, we compared the qCON and qNOX indices with the MAC of sevoflurane. MAC values are well-established and are the guiding tool to assess unconsciousness, eye-opening, and autonomic responses during general anesthesia.[20] Pantalacci et al.[21] conducted a prospective observational study to evaluate qCON and qNOX variations during outpatient laparoscopic cholecystectomy using remifentanil and desflurane without muscle relaxants and compared these indices with analgesia nociception index (ANI) and MAC. In their study, qCON correlated with MAC as well as with ANI, also a weak correlation between qNOX and the remifentanil infusion rate was noted. Surprisingly, this study failed to show any significant correlation of MAC values with either qCON or qNOX (P value >0.05) indices concerning the loss of consciousness and recovery as shown in Figures 3 and 4. This could be explained due to the use of muscle relaxants, as muscle relaxants are known to affect EEG parameters such as BIS.[22]
We evaluated the indices in the pediatric age group, which is not validated by BIS monitoring. We also evaluated a novel index for analgesia viz. qNOX. The same monitor gives both monitoring, i.e., depth and analgesia. The limitation of our study was the use of electro-cautery that influenced the qCON and qNOX reading significantly. This was minimized by restricting the use to burst cautery by surgeons. Moreover, reading with SQI <50 was rejected. Also, this study did not compare the qCON and qNOX index with BIS, which is considered the gold standard for depth of anesthesia monitoring. We used balanced general anesthesia, i.e., the use of benzodiazepines, opioids, and muscle relaxants along with sevoflurane, the MAC value may not be used as a sole measure of anesthetic effect in such cases.[21] Hence, comparing the qCON and qNOX with MAC of sevoflurane during general anesthesia with muscle relaxant might have resulted in an insignificant correlation between both. Since, to our knowledge, this is the first study of qCON and qNOX in pediatric cases, our interpretation applies only to ASA I and II. Further studies are required to validate these indices in ASA III and above class patients.
Conclusion
Both qCON and qNOX values change predictably with changes in the conscious level and with different noxious stimuli in pediatric patients. Further studies are required to confirm the findings taking into account the postoperative assessment of delirium and recall of intraoperative events.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kissin I. Depth of anesthesia and bispectral index monitoring. Anesth Analg. 2000;90:1114–7. doi: 10.1097/00000539-200005000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Pawar D. Common post-operative complications in children. Indian J Anaesth. 2012;56:496–501. doi: 10.4103/0019-5049.103970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jensen EW, Valencia JF, Lo´pez A A, Anglada T, Agustı´ M, Ramos Y, et al. Monitoring hypnotic effect and nociception with two EEG-derived indices, qCON and qNOX, during general anaesthesia. Acta Anaesthesiol Scand. 2014;58:933–41. doi: 10.1111/aas.12359. [DOI] [PubMed] [Google Scholar]
- 4.The 1978 Annual Scientific Meeting. Anaesthesia. 1979;34:390–434. [Google Scholar]
- 5.Sullivan LM. Estimation from samples. Circulation. 2006;114:445–9. doi: 10.1161/CIRCULATIONAHA.105.600189. [DOI] [PubMed] [Google Scholar]
- 6.Sloan TB. Anesthetic effects on electrophysiologic recordings. J Clin Neurophysiol. 1998;15:217–26. doi: 10.1097/00004691-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Beekoo D, Yuan K, Dai S, Chen L, Di M, Wang S, et al. Analyzing electroencephalography (EEG) waves provides a reliable tool to assess the depth of sevoflurane anesthesia in pediatric patients. Med Sci Monit. 2019;25:4035–40. doi: 10.12659/MSM.915640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sullivan CA, Egbuta C, Park RS, Lukovits K, Cavanaugh D, Mason KP. The use of bispectral index monitoring does not change intraoperative exposure to volatile anesthetics in children. J Clin Med. 2020;9:2437. doi: 10.3390/jcm9082437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim HS, Oh AY, Kim CS, Kim SD, Seo KS, Kim JH. Correlation of bispectral index with end-tidal sevoflurane concentration and age in infants and children. Br J Anaesth. 2005;95:362–6. doi: 10.1093/bja/aei196. [DOI] [PubMed] [Google Scholar]
- 10.Melia U, Gabarron E, Agustí M, Souto N, Pineda P, Fontanet J, et al. Comparison of the qCON and qNOX indices for the assessment of unconsciousness level and noxious stimulation response during surgery. J Clin Monit Comput. 2017;31:1273–81. doi: 10.1007/s10877-016-9948-z. [DOI] [PubMed] [Google Scholar]
- 11.Muller JN, Kreuzer M, Garcia PS, Schneider G, Hautmann H. Monitoring depth of sedation: Evaluating the agreement between the Bispectral Index, qCON and the entropy module's state entropy during flexible bronchoscopy. Minerva Anestesiol. 2017;83:563–73. doi: 10.23736/S0375-9393.17.11262-9. [DOI] [PubMed] [Google Scholar]
- 12.Obert DP, Schweizer C, Zinn S, Kratzer S, Hight D, Sleigh J, et al. The influence of age on EEG-based anaesthesia indices. J Clin Anesth. 2021;73:110325. doi: 10.1016/j.jclinane.2021.110325. [DOI] [PubMed] [Google Scholar]
- 13.Bergmann I, Göhner A, Crozier TA, Hesjedal B, Wiese CH, Popov AF, et al. Surgical pleth index guided remifentanil administration reduces remifentanil and propofol consumption and shortens recovery times in outpatient anaesthesia. Br J Anaesth. 2013;110:622–8. doi: 10.1093/bja/aes426. [DOI] [PubMed] [Google Scholar]
- 14.Soral M, Altun GT, Dinçer PÇ, Arslantas MK, Aykaç Z. Effectiveness of the analgesia nociception index monitoring in patients who undergo colonoscopy with sedo-analgesia. Turk J Anaesthesiol Reanim. 2020;48:50–7. doi: 10.5152/TJAR.2019.45077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rogobete AF, Bedreag OH, Papurica M, Popovici SE, Bratu LM, Rata A, et al. Multiparametric monitoring of hypnosis and nociception-antinociception balance during general anesthesia-a new era in patient safety standards and healthcare management. Medicina (Kaunas) 2021;57:132. doi: 10.3390/medicina57020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Julien-Marsollier F, Rachdi K, Caballero MJ, Ayanmanesh F, Vacher T, Horlin AL, et al. Evaluation of the analgesia nociception index for monitoring intraoperative analgesia in children. Br J Anaesth. 2018;121:462–8. doi: 10.1016/j.bja.2018.03.034. [DOI] [PubMed] [Google Scholar]
- 17.Park JH, Lim BG, Kim H, Lee IO, Kong MH, Kim NS. Comparison of surgical pleth index-guided analgesia with conventional analgesia practices in children: A randomized controlled trial. Anesthesiology. 2015;122:1280–7. doi: 10.1097/ALN.0000000000000650. [DOI] [PubMed] [Google Scholar]
- 18.Makkar JK, Dwivedi D, Kuberan A, Kumar B, Bala I. Minimum alveolar concentration of desflurane for maintaining BIS below 50 in children and effect of caudal analgesia on it. Anesth Essays Res. 2018;12:512–6. doi: 10.4103/aer.AER_51_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aantaa R, Takala R, Muittari P. Sevoflurane EC 50 and EC 95 values for laryngeal mask insertion and tracheal intubation in children. Br J Anaesth. 2001;86:213–6. doi: 10.1093/bja/86.2.213. [DOI] [PubMed] [Google Scholar]
- 20.Aranake A, Mashour GA, Avidan MS. Minimum alveolar concentration: Ongoing relevance and clinical utility. Anaesthesia. 2013;68:512–22. doi: 10.1111/anae.12168. [DOI] [PubMed] [Google Scholar]
- 21.Pantalacci T, Allaouchiche B, Boselli E. Relationship between ANI and qNOX and between MAC and qCON during outpatient laparoscopic cholecystectomy using remifentanil and desflurane without muscle relaxants: A prospective observational preliminary study. J Clin Monit Comput. 2023;37:83–91. doi: 10.1007/s10877-022-00861-x. [DOI] [PubMed] [Google Scholar]
- 22.Messner M, Beese U, Romstöck J, Dinkel M, Tschaikowsky K. The bispectral index declines during neuromuscular block in fully awake persons. Anesth Analg. 2003;97:488–91. doi: 10.1213/01.ANE.0000072741.78244.C0. [DOI] [PubMed] [Google Scholar]


