Abstract
Background
In an individual, the development and severity of Non-Communicable Diseases (NCDs) are determined by the presence or absence of clustering of NCD risk factors in them. We aimed to determine the prevalence and the factors associated with clustering of risk factors of NCDs in the district of Puducherry in India.
Methodology
We conducted a community-based cross-sectional survey among the adult population (18–69 years) of Puducherry district (N = 1114) between February 2019 and February 2020. Ten risk factors of NCDs (behavioral, physical measurements and biochemical) were assessed. Individuals having ≥ 3 risk factors were regarded as having clustering of risk factors. Categorical variables are summarized using proportions (95% CI). Adjusted prevalence ratio was estimated using weighted forward stepwise generalized linear modelling.
Results
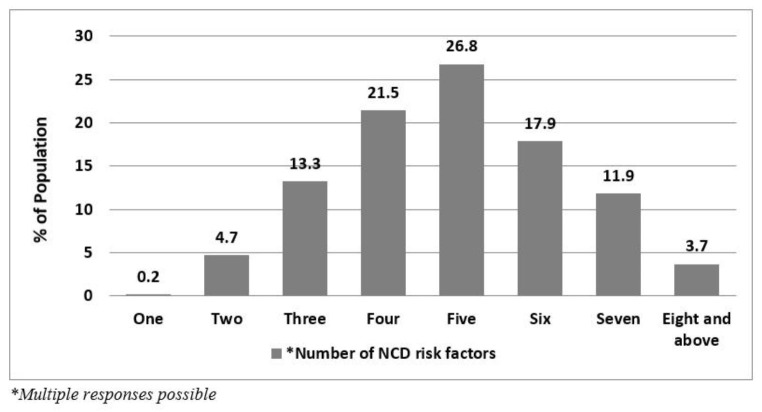
Clustering of NCD risk factors was present in majority (95.2%, 95% CI: 93.8–96.3) of the population. The presence of clustering was significantly higher among women (97.1%, 95% CI: 95.9–98.3) and the urban population (97.2%, 95% CI: 96.1–98.3). The risk factors that primarily drove the high prevalence of clustering were raised salt intake and inadequate intake for fruits and vegetables in nine out of 10 people in the district. Nearly 1 in 10 (13.3%, 95% CI: 11.3–15.3), 1 in 5 (21.5%, 95% CI: 19.1–23.8) and 1 in 4 (26.8%, 95% CI: 24.1–29.4) participants had three, four and five risk factors, respectively.
Conclusion
We highlight the urgent need for population-based health promotion interventions in the district of Puducherry targeting the highly prevalent NCD risk factors, especially among the women and urban populations.
Keywords: Non communicable Diseases, Risk factors, WHO STEPS, Cluster analysis, Epidemiology
Introduction
Non-communicable diseases (NCDs) are the leading cause of morbidity and mortality, causing 71% of all deaths globally. Low and middle-income countries share a disproportionately higher burden (85%) of premature deaths due to NCDs [1]. In India, the disease burden due to NCDs rose from 48 to 75% between 1990 and 2016. Currently, three of the country’s top five causes for morbidity and mortality are NCDs [2].
NCDs are primarily caused by tobacco and alcohol use, unhealthy diet, physical inactivity, elevated blood pressure, elevated blood lipid level, diabetes mellitus, and abdominal obesity [1]. Population-level control of these risk factors could prevent the development of NCDs in the population and achieve India’s target of achieving a 25% relative reduction in NCDs by 2025. World Health Organization (WHO) also recognizes investment for preventing and controlling these risk factors as ‘best buys’ strategies in controlling the NCD epidemic [3].
Risk factors of NCDs tend to co-exist in an individual [4]. This phenomenon of the presence of more than two risk factors in an individual is termed as clustering of risk factors [5]. Identifying individuals with clustered risk factors gains importance as emerging evidence suggests that the development and severity of NCDs are determined by the presence or absence of clustered risk factors [6, 7].
In India, various national and sub-national surveys have quantified the prevalence of individual risk factors of NCDs [8, 9]. However, in a country like India, where more than half of morbidity and mortality is attributed to NCDs, evidence of the clustering of risk factors is scarce. Studies carried out in Mexico, Bangladesh, Bhutan, and Nepal have documented the prevalence of clustered risk factors [10–12]. It is therefore crucial to estimate the prevalence of clustered risk factors sub-nationally in India, given the geographic variations in the prevalence of NCD risk factors in the country. The insights gained would facilitate identifying at-risk population groups for implementing targeted public health interventions to reduce the burden of NCDs in the population. This also makes it feasible to undertake the multiple risk factors approach recommended by the National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases & stroke (NPCDCS) which implements prevention, early identification, management, and surveillance of NCD risk factors in an integrated manner rather than the individual risk factor-based strategies [13, 14].
Over the years, rapid urbanization has been well recognized as one of the main drivers for NCDs, especially in low and middle-income countries like India [15]. Puducherry being one of the country’s highly urbanized states with more than two-thirds of the population residing in urban areas, substantially high prevalence of various individual risk factors of NCDs has already been documented in the district [16]. Currently, there is a lack of evidence on the prevalence of clustering of risk factors in the district that is crucial for devising population-based public health interventions. Therefore, keeping this rationale, we analyzed data from an NCD risk factors survey conducted in the district of Puducherry in India to estimate the prevalence of clustering of NCD risk factors and its determinants in the adult population aged 18 and 69 years.
Methods
Study design and study setting
We surveyed NCD risk factors using WHO STEPS guidelines in the district of Puducherry from Feb 2019 to Feb 2020. The survey included a total of 2560 individuals aged between 18 and 69 from urban and rural areas (50 clusters in each) of Puducherry district through a multi-stage cluster random sampling method. The detailed methodology has been published elsewhere [16]. However, we have presented the methodology that is relevant to estimating the clustering of NCD risk factors in detail in the forthcoming sub-sections.
Puducherry is one of the four districts of the Union Territory of Puducherry located along the eastern coast of South India. Puducherry district has a population of 0.95 million, with majority (68.33%) residing in the urban areas [17].
In Puducherry, healthcare for NCDs is delivered by public and private providers, as in any other state in the country. Public healthcare is provided by a network of public health care facilities i.e., 52 sub-centers, 27 Primary Health Centres (12 urban and 15 rural), and two community health centres. In addition, there are nine medical colleges and several private hospitals. In accordance with NPCDCS program, a population-based screening to diagnose selected NCDs such as diabetes, hypertension, and three common cancers (cervical, oral & breast) is being carried out with the help of Auxiliary Nurses Midwives (ANMs) and Accredited Social Health Activists (ASHAs) at the primary health centres. They also conduct health education programs periodically in the community on common risk factors of NCDs, prevention of key risk factors, the importance of screening for risk factors, and early diagnosis of NCDs.
In each public healthcare facility, at the level of PHC and above, NCD clinic is being conducted on a particular day of each week. At the clinic, health education on NCDs and its risk factors, diagnostic tests, treatment for NCDs, and follow-up consultations are provided to the patients with free monthly distribution of drugs.
Sample size and sampling method
From the WHO STEPS survey participants, we included 1114 participants for this study for whom information on ten NCD risk factors was available. Therefore, the prevalence of clustering of risk factors was estimated from this sub-group of the survey participants. However, we calculated the sample size of 1010 using the formula n = z2 [P(1-P)]/e2 [18] by considering 73% prevalence (P) of clustered risk factors in the current study setting [5], 95% confidence interval (e = 0.05), design effect of 1.5 and response rate of 90%. This sample was sufficient to provide a district-wide representative estimation of clustered risk factors by residence (urban/rural) stratification.
In the WHO STEPS survey, we employed multi-stage, geographically clustered random sampling method using Census 2011 as the baseline. We used three and two-staged sampling in the urban and rural areas of the district, respectively. In the first stage, out of 92 urban wards and 62 revenue villages, we chose 50 clusters in both urban and rural areas, respectively. In the second stage, from each selected urban ward, one Census Enumeration Block (CEB) was chosen. From each selected CEB and village, 36 and 16 households were chosen using systematic random sampling. From each selected household, one individual aged 18–69 years who had resided for the last six months was chosen randomly using the KISH technique [16].
In the survey, information on various behavioral and biological risk factors was collected from the participants in three stages. The first and second stages involved assessing behavioral risk factors of NCDs and physical measurements for all 2560 participants. In the subsequent stage, the third stage, every alternate participant (i.e., 1207 individuals) was invited to participate in the estimation of biochemical risk factors of NCDs. [16] Consequently, a total of 1177 individuals (97.5%; (1177/1207) * 100) participated in this stage. Among these participants, a subset of 1114 (94.6%; (1114/1177) * 100) individuals had complete information available for all ten NCD risk factors, and thus this subset of survey participants was included for this analysis.
Data collection procedure
Behavioral risk factors, physical measurements such as height, weight, waist circumference, blood pressure, and biochemical risk factors such as raised fasting blood glucose, and hypercholesterolemia were assessed as per the WHO STEPS guidelines [19]. An individual who used tobacco (smoke/smokeless) during the last thirty days and consumed alcohol during the last year was considered a tobacco and alcohol user, respectively. Intake of fewer than five servings of fruits/vegetables per day and less than 150 min of physical activity per week were considered inadequate intake of fruits and vegetables and physical inactivity, respectively.
Participants’ height and waist circumference was measured using SECA constant tape at the nearest 0.1 cm. Weight was measured in kilogram (kg) using digital weight scale. Body Mass Index of participants were calculated using the formula weight (kg) / (Height in meter)2. Three blood pressure (BP) readings were measured using a digital automatic blood pressure monitor (OMRON M16) in the seating position. The last two were averaged to get the final BP reading of the participant.
Parameters such as plasma glucose and total cholesterol were estimated from a five ml of fasting blood sample of participants collected in the early morning. A urine sample of 10 ml was collected from each participant to estimate the levels of urinary sodium (Na) and urinary Creatinine (Cr). The samples were transported to the biochemistry lab of the institute for parameters estimation. Dietary salt intake (gm) of participants per day was estimated using the predictive equation by Tanaka that uses participants information such as age (years), weight (kg), height (cm), urinary Na (mmol/l) and Cr (mg/dL) in the formula: 2.54 ÷ 1000 × 23 × 21.98 × (spot Na (mmol/l)/[spot Cr (mg/dL) × 10] × [− 2.04 × age (years) + 14.89 × weight (kg) + 16.14 × height (cm) − 2244.45])0.392 [16].
The institutional Ethics committee (Human studies) of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) has approved the study (vide letter No. JIP/IEC/2018/0246 dated 03/10/2018).
Operational definition
The prevalence of clustering of risk factors was estimated from ten major risk factors of NCDs assessed in the STEPS survey. The risk factors included were tobacco use, alcohol use, inadequate intake of fruits and vegetables, high dietary salt intake, physical inactivity, overweight/obesity, abdominal obesity, raised blood pressure, raised fasting blood glucose, and hypercholesterolemia. Presence of three or more risk factors in an individual was considered as the presence of clustering of risk factors. All risk factors used for estimating clustering were defined as per the definitions followed for estimating various NCD risk factors in the STEPS survey [16, 20].
Statistical analysis
We cleaned and analyzed data using IBM SPSS version 22 (IBM Corp., Armonk, NY, USA) and STATA version 14.1 (StataCorp LP, College Station, TX, USA). Prevalence of NCD risk factors clustering is presented using proportion and 95% Confidence Interval. Initially, the univariate logistic regression model was developed to determine the participant characteristics (socio-demographic) associated with the prevalence of clustered NCD risk factors. Predictors that were statistically associated (p < 0.10) with the prevalence of clustered NCD risk factors were used for developing multi-variate model. Adjusted prevalence ratio for each predictor was estimated using weighted forward stepwise generalized linear modelling using ‘Poisson’s regression’. In the regression model, P ≤ 0.05 were considered statistically significant.
Results
In the study, participants’ mean (SD) age was 45 (14) years. The majority were women 609 (54.7%) and belonged to urban areas 789 (70.6%). Nearly half (49.9%) of the participants had received primary/secondary education, and about 14.5% were educated up to graduation and above. Nearly half (47.8%) of participants were employed in government/ non-government/self-employed (Table 1).
Table 1.
Socio-demographic profile of study participants (N = 1114)
| Variables | Men (n = 461) n (%) |
Women (n = 653) n (%) |
Both Gender (N = 1114) n (%) |
|---|---|---|---|
| Age* categories (in years) | |||
| 18–44 | 188 (40.8) | 317 (48.5) | 505 (45.3) |
| 45–69 | 273 (59.2) | 336 (51.5) | 609 (54.7) |
| Residence | |||
| Urban | 315 (68.3) | 471 (72.1) | 789 (70.6) |
| Rural | 146 (31.7) | 182 (27.9) | 328 (29.4) |
| Educational status | |||
| No formal education | 26 (5.6) | 104 (15.9) | 130 (11.7) |
| Less than primary | 59 (12.8) | 69 (14.7) | 155 (13.9) |
| Primary education | 146 (31.7) | 181 (27.7) | 327 (19.4) |
| Secondary/ Higher Secondary | 158 (34.3) | 182 (27.9) | 340 (30.5) |
| Graduation and above | 71 (15.4) | 90 (13.8) | 161 (14.5) |
| Refused to answer | 1 (0.2) | 0 | 1 (0.1) |
| Religion | |||
| Hindu | 435 (94.4) | 608 (93.1) | 1043 (93.6) |
| Christian | 17(3.7) | 32 (4.9) | 49 (4.4) |
| Muslim | 9 (2) | 12 (1.8) | 21 (1.9) |
| Others | 0 | 1 (0.2) | 1 (0.1) |
| Marital status | |||
| Never married | 83 (18) | 38 (5.8) | 121 (10.9) |
| Currently married | 363 (78.7) | 498 (76.3) | 861 (77.3) |
| Divorced/Separated | 4 (0.9) | 12 (1.8) | 16 (1.4) |
| Widowed | 11 (2.4) | 105 (16.1) | 116 (10.4) |
| Occupation | |||
| Government employee | 22 (4.8) | 9 (1.4) | 31 (2.8) |
| Non-Government employee | 145 (31.5) | 80 (12.3) | 225 (20.2) |
| Self employed | 185 (40.1) | 91 (13.9) | 276 (24.8) |
| Student | 19 (4.1) | 12 (1.8) | 31 (2.8) |
| Homemaker | 9 (2) | 411 (62.9) | 420 (37.7) |
| Retired | 34 (7.4) | 6 (0.9) | 40 (3.6) |
| Unemployed (able to work) | 15 (3.3) | 17 (2.6) | 32 (2.9) |
| Unemployed (Unable to work) | 32 (6.9) | 27 (4.1) | 59 (5.3) |
*Mean (SD) age: Men 46 (15) years; Women 45 (13) years
Clustering of NCD risk factors was present in majority of the population (95.2%, 95% CI: 93.8–96.3). None of the study participants was free from all the ten NCD risk factors assessed. The prevalence of clustered risk factors was significantly higher among women (97.1%, 95% CI: 95.9–98.3) when compared to men (92.4%, 95% CI: 89.8–94.8). Similarly, the prevalence of clustered risk factors was significantly higher among the urban population (97.2%, 95% CI: 96.1–98.3) when compared to the rural population (90.2%, 95% CI: 86.9–93.3). The probability of women and urban population having clustered risk factors was significantly higher by 5% (PR: 1.05, 95% CI: 1.02–1.08) and seven% (PR: 1.07, 95% CI: 1.03–1.1) respectively, when compared to their counterparts (Table 2).
Table 2.
Determinants of clustering of NCD risk factors in the population of Puducherry district: (N = 1114)
| Variable | N | Clustering of risk factors+ | aPR (95% CI) | p-value | |
|---|---|---|---|---|---|
| Present n (%) |
Absent n (%) |
||||
| Gender | |||||
| Men | 461 | 426 (92.4) | 35 (7.6) | 1 | 0.01* |
| Women | 653 | 634 (97.1) | 19 (2.9) | 1.05 (1.02–1.08) | |
| Residence | |||||
| Rural | 328 | 296 (90.2) | 32 (9.8) | 1 | 0.01* |
| Urban | 786 | 764 (97.2) | 22 (2.8) | 1.07 (1.03–1.1) | |
| Age (in years) | |||||
| 18–44 | 505 | 473 (93.7) | 32 (6.3) | 1 | 0.05* |
| 45–69 | 609 | 587 (96.4) | 22 (3.6) | 1.03 (0.99–1.06) | |
| Education | |||||
| Up to primary education | 612 | 582 (95.1) | 30 (4.9) | 1 | |
| Secondary education | 340 | 327 (96.2) | 13 (3.8) | 1.02 (0.99–1.04) | 0.14 |
| Graduation and above | 161 | 150 (93.2) | 11 (6.8) | 1.01 (0.96–1.05) | 0.7 |
| Marital status | |||||
| Currently married | 861 | 830 (96.4) | 31 (3.6) | 1 | |
| Never married | 121 | 105 (86.8) | 16 (13.2) | 0.93 (0.87–0.99) | 0.02* |
| Widowed/divorced | 132 | 125 (94.7) | 7 (5.3) | 0.97 (0.92–1.01) | 0.18 |
| Occupation | |||||
| Home maker | 451 | 439 (97.3) | 12 (2.7) | 1 | |
| Government/ Non-government employee | 225 | 213 (94.7) | 12 (5.3) | 1.02 (0.98–1.05) | 0.3 |
| Self-employed | 276 | 260 (94.2) | 16 (5.8) | 1 (0.97–1.04) | 0.6 |
| others | 162 | 148 (91.4) | 14 (8.6) | 0.98 (0.94–1.03) | 0.52 |
*Significant results: p ≤ 0.05, aPR: Adjusted Prevalence Ratio, CI: Confidence Interval, +Clustering of risk factors: Presence of three or more risk factors of NCDs in an individual
In the study, 1 in 8 (13.3%, 95% CI: 11.3–15.3) participants had three risk factors, 1 in 5 (21.5%, 95% CI: 19.1–23.8) had four risk factors, and 1 in 4 (26.8%, 95% CI: 24.1–29.4) participants had five risk factors (Fig. 1). The high prevalence of clustered risk factors (≥ 3 risk factors) was mainly driven by high prevalence of raised salt intake (98.7%), inadequate intake of fruits and vegetables (86.8%), abdominal obesity (68.2%), and overweight/obesity (63.7%).
Fig. 1.
Prevalence of clustering of NCD risk factors in the district of Puducherry (n = 1114)
Considering that almost 95.2% of the population was estimated to have clustering of risk factors, we re-estimated its prevalence after excluding the risk factor of inadequate intake of fruits and vegetables, which used the most subjective form of assessment compared to all other risk factors assessed in the study. Therefore, when nine risk factors were considered, the prevalence of clustering of risk factors marginally increased to 95.9% (95% CI: 94.7–97). Here, 1 in 6 (16.2%) participants had three risk factors, 1 in 3 (30.1%) had four risk factors, and 1 in 4 (22.8%) participants had five risk factors.
Discussion
In the district of Puducherry, clustering of NCD risk factors was present among the majority of the population, with none being free from all ten risk factors assessed. The presence of clustering was significantly higher among women and the urban population.
In India, several studies have documented the prevalence of individual risk factors of NCDs through national and sub-national risk factor surveys [8, 9, 21, 22]. But, evidence on the prevalence of clustering of risk factors is scarce. The district of Puducherry, being one of the highly urbanized districts in the country with high level of individual risk factors [17], it becomes essential to gain better understating of the prevalence and determinants of clustered NCD risk factors. This would help public health authorities of the district to devise population-based public health interventions for the identified targeted groups with an integrated approach for NCD prevention, rather than the less effective older practice of individual risk factors approach [13, 14]. It has also been well documented that NCD risk factors are interrelated and act synergistically to cause NCDs in individuals, emphasizing the need to target individuals for public health intervention based on the magnitude of clustered risk factors in them [12, 23].
In the current study, almost all (95.2%) had clustered risk factors. A study carried out in 2014 from an urban area of Puducherry reported three-fourths of the population (73%) to have clustered risk factors [5]. Studies from the neighboring states such as Karnataka (56.3%) and Kerala (47.1%) showed that nearly half of them had clustered risk factors [24, 25].
A multi-centric study carried out across five Asian cities documented the prevalence of clustered risk factors among men and women to be 17.7% and 24.7%, respectively [4]. Studies conducted in other South Asian countries such as Bangladesh, Nepal and Bhutan have also documented higher prevalence of coexisting NCD risk factors [10–12].
Compared to the above studies, the prevalence obtained from the current study is substantially higher. The discrepancies in the prevalence, compared to other studies could be primarily attributed to the differences in study population, the time when those studies were conducted, and number of risk factors assessed across studies for estimating the clustering of risk factors (ten risk factors in the present study). Nevertheless, substantially high prevalence of clustered risk factors in the district of Puducherry, and relatively high prevalence reported from other South Asian countries that are socio-economically similar to India indicate an impending rise in the burden of NCDs in the population. Therefore, countries that have identified substantial burden of clustering of risk factors in their populations need to implement population-based public health interventions through multi-sectoral partnerships at the national / regional level with sectors other than health to control and prevent the rising burden of clustered risk factors in its populations [26].
In the current study, the high prevalence of clustered risk factors was primarily driven by higher prevalence of NCD risk factors such as raised salt intake, and inadequate intake for fruits and vegetables that were present in around 9 out of 10 study subjects. Higher prevalence of clustering contributed by unhealthy diet, and physical inactivity is consistent with other studies carried out in the states of Karnataka, Kerala, and neighboring countries such as Bangladesh, Nepal, and Bhutan [10–12, 24, 25]. This finding serves the public health authorities of Puducherry, and other geographic settings compared to reorienting the ongoing community-based health promotion programs to address these highly prevalent risk factors in priority basis, and introduce newer NCD prevention and control interventions for reducing the prevalence of clustered risk factors in these geographic regions. Such interventions shall be designed by following the proven integrated approach for NCD prevention which already has been demonstrated to produce a cumulative effect in reducing the NCD risk in the population [13, 14].
In the current study, being women and residing in urban areas were significant predictors of clustered risk factors. This finding is consistent with studies carried out in other settings [5, 12]. Based on the current study finding, implementing primary prevention strategies for NCD risk factors by targeting women and the urban residents at the community level through health promotion interventions could be a prudent approach in halting the rising prevalence of clustered risk factors in the population.
Strength and limitations
We conducted this study in a representative sample of Puducherry district by following standard guidelines (STEPS methodology) as prescribed by WHO for population-based NCD risk factors assessment. This increases the generalizability of study findings. The study might also have certain limitations. Majority of individual risk factors of NCDs assessed in the study were based on participants’ ability to recall, which could carry a certain degree of recall bias. There could be an underestimation of a few behavioral risk factors such as tobacco use, alcohol consumption, and physical inactivity due to socially desirable responses that tend to occur in interview-based surveys. However, use of standard questionnaire, investigators trained in data collection techniques, and use of show cards would have helped to minimize the recall and social desirability biases. Physical inactivity levels were estimated using a widely accepted GPAQ scale. However, recent evidence presents underestimation of physical inactivity levels, especially those of household and leisure activities [27, 28]. This could have caused underestimation of physical inactivity. The potential underestimation of various individual risk factors could have led to underestimation of the prevalence of clustered risk factors estimated in the study.
Conclusion
Clustering of risk factors for NCDs was present in nine out of ten people (95.2%) in the district of Puducherry. The clustering was significantly higher among women and the urban population (97.2%) than its counterparts. Nearly one-tenth (13.3%), one-fifth (21.5%), and one-fourth (26.8) of the population had three, four and five risk factors, respectively. We highlight the urgent need for population-based health promotion interventions in the district of Puducherry targeting the highly prevalent NCD risk factors, especially among the women and urban populations of the district.
Authors’ contributions
PS, JPS, SL, ZB, JA and SSK conceptualized the study design and methodology. PS conducted the field data collection. All authors contributed to the analysis plan of the manuscript, and PS carried out the analysis. PS wrote the first draft of the manuscript with inputs from SKK and JPS. All authors reviewed the manuscript, provided information for data interpretation, and approved its final version.
Funding
Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) institute, India [Grant Number: JIP/Dean (R)/Intramural/Phs 1/2019-20] has funded this project through the intramural funding for Ph.D. studies.
Declarations
Ethics approval
The study was approved by the Ethics Committee of institute ‘Jawaharlal Institute of Postgraduate Medical Education and Research’ (No: JIP/IEC/2018/0246).
Consent for publication
Not applicable.
Competing interests
We declare no competing interests.
Data sharing
The data underlying this manuscript could be shared by the corresponding author upon reasonable request (email: drsitanshukar@gmail.com).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.“Global status report on noncommunicable diseases 2010,” World Health Organization, World Health Organization Regional Office, Geneva. ISBN 978 92 4 068645 8, 2011. [Online]. Available: https://www.who.int/nmh/publications/ncd_report_full_en.pdf.
- 2.Indian Council of Medical Research, Public Health Foundation of India, and Institute for Health Metrics and Evaluation., “India: Health of the Nation’s States: The India State-Level Disease Burden Initiative,” New Delhi, ISBN: 978-0-9976462-1-4, 2017. Accessed: Oct. 21, 2020. [Online]. Available: https://phfi.org/the-work/research/the-india-state-level-disease-burden-initiative/.
- 3.Organization WH. “From Burden to ‘Best Buys’: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries,” World Health Organization, Geneva, Switzerland. [Online]. Available: https://www.who.int/nmh/publications/best_buys_summary.pdf.
- 4.Ahmed SM et al. “Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants,” Glob. Health Action, vol. 2, no. 1, p. 1986, Nov. 2009, 10.3402/gha.v2i0.1986. [DOI] [PMC free article] [PubMed]
- 5.Selvaraj K, Kar SS, Ramaswamy G, Premarajan KC, Saya GK, Kalidoss V. “Clustering of cardiovascular disease risk factors - Syndemic approach: Is sit a time to shift toward integrated noncommunicable disease clinic?” Indian J. Public Health, vol. 63, no. 3, pp. 186–193, Sep. 2019, 10.4103/ijph.IJPH_158_18. [DOI] [PubMed]
- 6.Yusuf S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet Lond Engl. Sep. 2004;364:937–52. 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed]
- 7.Gupta R, Misra A, Pais P, Rastogi P, Gupta VP. “Correlation of regional cardiovascular disease mortality in India with lifestyle and nutritional factors,” Int. J. Cardiol, vol. 108, no. 3, pp. 291–300, Apr. 2006, 10.1016/j.ijcard.2005.05.044. [DOI] [PubMed]
- 8.Anjana RM, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585–96. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 9.National Institute of Medical Statistics and Council of Medical Research., “Integrated Disease Surveillance Project (IDSP): Non-Communicable Disease Risk Factors Survey, Phase 1 states of India, 2007-08,” New Delhi, 2009. Accessed: May 29, 2018. [Online]. Available: http://www.who.int/ncds/surveillance/steps/2007_STEPS_Report_India_7States.pdf.
- 10.Pelzom D, Isaakidis P, Oo MM, Gurung MS, Yangchen P. “Alarming prevalence and clustering of modifiable noncommunicable disease risk factors among adults in Bhutan: a nationwide cross-sectional community survey,” BMC Public Health, vol. 17, no. 1, p. 975, Dec. 2017, 10.1186/s12889-017-4989-x. [DOI] [PMC free article] [PubMed]
- 11.Aryal KK, et al. The Burden and Determinants of non communicable Diseases Risk factors in Nepal: findings from a nationwide STEPS Survey. PLoS ONE. Aug. 2015;10:e0134834. 10.1371/journal.pone.0134834. no. 8. [DOI] [PMC free article] [PubMed]
- 12.Zaman MM, et al. Clustering of non-communicable diseases risk factors in bangladeshi adults: an analysis of STEPS survey 2013. BMC Public Health. Jul. 2015;15(1):659. 10.1186/s12889-015-1938-4. [DOI] [PMC free article] [PubMed]
- 13.Directorate General of Health Services and Ministry of Health. & Family welfare, “National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke (NPCDCS): Operational Guidelines (Revised: 2013-17),” New Delhi, 2013. Accessed: Jan. 09, 2020. [Online]. Available: https://main.mohfw.gov.in/sites/default/files/Operational%20Guidelines%20of%20NPCDCS%20%28Revised%20-%202013-17%29_1.pdf.
- 14.Narain JP. “Integrating Services for Noncommunicable Diseases Prevention and Control: Use of Primary Health Care Approach,” Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med, vol. 36, no. Suppl1, pp. S67–S71, Dec. 2011, 10.4103/0970-0218.94712. [DOI] [PMC free article] [PubMed]
- 15.“World Health Organization Regional Office for the Western. Global status report on noncommunicable diseases 2010 [Internet]. Geneva: World Health Organization. ; 2011 p. 164. Report No.: ISBN 978 92 4 068645 8. Available from: https://www.who.int/nmh/publications/ncd_report_full_en.pdf”.
- 16.Sivanantham P, Sahoo J, Lakshminarayanan S, Bobby Z, Kar SS. Profile of risk factors for non-communicable Diseases (NCDs) in a highly urbanized district of India: findings from Puducherry district-wide STEPS Survey, 2019-20. PLoS ONE. 2021;16(1):e0245254. doi: 10.1371/journal.pone.0245254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Census of India., “Puducherry (Pondicherry) District Population Census 2011–2020, Puducherry literacy sex ratio and density,” Population Census 2011, 2011. https://www.census2011.co.in/census/district/482-puducherry.html (accessed May 26, 2020).
- 18.Metcalfe C, “Biostatistics: A Foundation for Analysis in the Health Sciences. 7th edn. Wayne W. Daniel, Wiley. 1999. No. of. pages: xiv + 755 + appendices. Price: £28.95. ISBN 0-471-16386-4,” Stat. Med, vol. 20, no. 2, pp. 324–326, 2001, . [DOI]
- 19.Organization WH, “WHO STEPS Surveillance Manual. : STEPwise Approach to Non Communicable Disease risk factors surveillance,” World Health Organization, Geneva, Jan. 2017. Accessed: Feb. 12, 2019. [Online]. Available: http://www.who.int/ncds/surveillance/steps/en/.
- 20.Thakur JS, et al. Non-communicable diseases risk factors and their determinants: a cross-sectional state-wide STEPS survey, Haryana, North India. PLoS ONE. 2019;14(11):e0208872. doi: 10.1371/journal.pone.0208872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thakur JS, et al. Non-communicable diseases risk factors and their determinants: a cross-sectional state-wide STEPS survey, Haryana, North India. PLoS ONE. Nov. 2019;14(11):e0208872. 10.1371/journal.pone.0208872. [DOI] [PMC free article] [PubMed]
- 22.Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Prasad R. Urban rural differences in diet, physical activity and obesity in India: are we witnessing the great indian equalisation? Results from a cross-sectional STEPS survey. BMC Public Health. 18 2016;16(1):816. 10.1186/s12889-016-3489-8. [DOI] [PMC free article] [PubMed]
- 23.Patel SA, et al. Chronic disease concordance within indian households: a cross-sectional study. PLOS Med. Sep. 2017;14(9):e1002395. 10.1371/journal.pmed.1002395. [DOI] [PMC free article] [PubMed]
- 24.Sarma PS, et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. Nov. 2019;9(11):e027880. 10.1136/bmjopen-2018-027880. [DOI] [PMC free article] [PubMed]
- 25.Sarveswaran G, Kulothungan V, Mathur P. “Clustering of noncommunicable disease risk factors among adults (18–69 years) in rural population, South-India,” Diabetes Metab. Syndr, vol. 14, no. 5, pp. 1005–1014, Oct. 2020, 10.1016/j.dsx.2020.05.042. [DOI] [PubMed]
- 26.“Ministry of Health and Family Welfare. National multisectoral action plan for prevention and control of common noncommunicable diseases (2017–2022) [Internet]. New Delhi: Ministry of Health and Family Welfare; 2017 Oct [cited 2020 Jun 5] p. 52. Available from: https://main.mohfw.gov.in/sites/default/files/National%20Multisectoral%20Action%20Plan%20%28NMAP%29%20for%20Prevention%20and%20Control%20of%20Common%20NCDs%20%282017-22%29_1.pdf”.
- 27.Yadav K, Krishnan A. “Changing patterns of diet, physical activity and obesity among urban, rural and slum populations in north India,” Obes. Rev. Off. J. Int. Assoc. Study Obes, vol. 9, no. 5, pp. 400–408, Sep. 2008, 10.1111/j.1467-789X.2008.00505.x. [DOI] [PubMed]
- 28.Armstrong T, Bull F. “Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ),” J. Public Health, vol. 14, no. 2, pp. 66–70, Apr. 2006, 10.1007/s10389-006-0024-x.