Abstract
Physicians in the United States are increasingly working with physician assistants (PAs) and nurse practitioners (NPs), but little is known about how they perceive working with PAs and NPs affects their clinical practice. We used a new national survey to examine physicians’ perceptions of working with PAs and/or NPs on their patient volume, care quality, time use, and workload. Among our analytical sample of 5823 physicians, 59% reported working with PAs and/or NPs. Most reported that PAs and NPs positively affected their clinical practice. Among several findings, physicians working in medical schools and with higher incomes were more likely to indicate that PAs improve their clinical practices in all 4 aspects, while being in specialties with higher women's representation was associated with lower ratings for working with PAs. Native Hawaiian and Pacific Islander physicians and those with higher incomes were more likely to signify that NPs improved their clinical practices in all 4 aspects. These findings provide valuable insights, from the physicians’ perspective, on care delivery reform.
Keywords: physician assistant/associate, nurse practitioner, physician, interprofessional care, clinical practice
Introduction
With over 140 910 physician assistants (PAs) and 258 230 nurse practitioners (NPs) in the United States in 2022,1 physicians are increasingly working alongside these clinicians to provide patient care. In 2016, over one-quarter of primary care and subspecialty practices employed at least 1 PA or NP,2,3 and between 2013 and 2019, the proportion of Medicare visits delivered by a PA or NP increased from 14.0% to 25.6%.4 Among family physicians, 60%–70% report working with PAs and NPs,5,6 and those in rural settings have a higher likelihood of working with PAs and NPs compared with those working in nonrural settings.5 A large body of evidence demonstrates the positive impact of PA- and NP-delivered care on outcomes such as cost, access, and quality.7-9 Additionally, provider teams consisting of physicians and NPs or PAs outperform solo providers on measures of hypertension, hyperlipidemia, and type 2 diabetes management.10 Such teams have also been found to provide some benefits in meeting the complex needs of older adults.11 However, despite literature describing the benefits of these interprofessional provider configurations to care delivery, little is known about how physicians who work with PAs and NPs perceive the effects of these arrangements on their clinical practice.
While PAs and NPs fill similar roles in health care, some differences in their education and scope of practice (SOP), which is determined at the state level, exist. Physician assistant education is based on the medical (ie, physician) model of education with a generalist focus.12,13 Upon completion, individuals earn a master's degree and must pass a national certification exam to be eligible for state licensure. Physician assistants can practice across specialties. While PA practice regulations vary by state, physician supervision or collaboration is required upon initial licensure in all 50 states.14 Nurse practitioners are registered nurses who have received a bachelor’s of science in nursing followed by advanced didactic and clinical training through a master's or doctoral degree program.15 Nurse practitioners are educated within the nursing model of care, and training is focused on a population (eg, family, pediatrics, adult-gerontology) and setting (eg, primary care, acute care). Like PAs, NPs are nationally certified and licensed to practice at the state level. The NP SOP regulations also vary across states. Over half of the states allow for full practice authority for NPs, in which no formal written agreements for physician supervision or collaboration are required for licensure and practice. The remaining states require formal written or collaborative agreements with physicians for an NP to practice in the state.16 Although not required for practice, PAs and NPs are increasingly completing postgraduate training programs in specific specialties and settings.17
Prior research has identified various ways that PAs and NPs impact clinical practice. One study found increased physician Relative Value Units (RVUs) and overall revenue after the integration of PAs and NPs into a radiology practice.18 Another study involving nearly 28 000 family physicians found that including PAs or NPs was associated with significantly larger patient panel sizes and a greater number of patient care activities.6 However, these studies are limited by reporting practice-level outcomes associated with PA and NP employment and focusing on a single practice site or physician specialty. Few studies have provided evidence of individual physicians’ perspectives on working with PAs and NPs across settings and specialties. One study, although dated, examined the perceptions of 600 rural family physicians and found that, although there was a high level of confidence in PAs’ and NPs’ abilities, physicians were concerned about increasing workloads.19 The roles of PAs and NPs and their contributions to clinical practice have evolved significantly over the 25 years since that study was published.
This study fills that gap by using new nationally representative survey data to explore physicians’ perceptions of working with PAs and/or NPs on their own clinical practice. The research questions guiding this study were as follows: (1) Which types of physicians are more likely to work with PAs or NPs and (2) How do physicians perceive working with PAs and NPs impacts their clinical practice? This study enhances our understanding of PA and NP contributions to clinical practice and care delivery by generating knowledge about their influence on physicians’ clinical practice.
Data and methods
Data source
We used data from the Association of American Medical Colleges’ (AAMC's) National Sample Survey of Physicians (NSSP) 2022, which were collected between May 10 and November 9, 2022, and include demographic and professional information on a wide range of topics for 5917 active physicians in the United States. The NSSP 2022 dataset was collected using a 2-step method: (1) all eligible respondents from the NSSP 2019 survey were invited and (2) new invitees were selected via a stratified random sample with proportionate allocation, based on the physician's sex, specialty group, age group, and rural status. Postsurvey weights were adjusted for differential nonresponse using the NSSP 2022 survey invitees and calibrated back to known American Medical Association physician population characteristics. Additional details about the NSSP sampling and weighting strategies can be found on AAMC's website.20 This project was approved by the American Institutes for Research's Institutional Review Board.
Measures and outcomes
The NSSP 2022 respondents reported whether they routinely worked with PAs and NPs (prevalence) during the preceding 12 months and, if so, how many (intensity), using an integer ranging from 1 to 100 or more than 100 (see Appendix B for these distributions). Due to the extremely left-skewed distribution of reported values, we recategorized “more than 100” to 100. Respondents who worked with PAs or NPs were also asked about the impact these clinicians had on 4 areas of clinical practice (ie, outcomes of interest). This was done by assessing physicians’ level of agreement or disagreement that “working with PAs and NPs” (1) “allows me to care for more patients” (patient volume), (2) “improves my quality of care” (improved quality), (3) “helps me make better use of my time” (time use), and (4) “decreases my workload” (decreased workload). Ratings were reported on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Physicians also reported the percentage of time they spend providing patient care in rural, suburban, and urban areas. If a physician reported they spent 80% or more of their patient care time in rural areas, they were categorized as “high rural serving.” Annual income was reported on a 1 (≤$50 000) to 11 (≥$500 000) scale with $50 000 increments. Respondent physicians were categorized into 1 of 4 specialty groups, as detailed in Appendix A.
Statistical analysis
We conducted a set of 8 ordered logistic regressions to explore the relationships between the intensity of working with PAs or NPs and physicians’ perceptions of PAs’ or NPs’ impact on clinical practice. The outcomes of interest, treated as ordinal variables, were patient volume, improved quality, time use, and decreased workload. The independent variables were continuous measures of PA intensity (4 models) and NP intensity (4 models). Additional explanatory variables included physician characteristics (age, gender, and race), employment type (employed, owner, other), practice specialty (grouped), high-rural-serving status, full-time status, work setting, international medical graduate (IMG) status, and percentage of women at the specialty level. We also controlled for PA and NP state SOP regulation (1, restricted; 2, reduced; and 3, full practice) based on the physicians’ practice state using data from the American Association of Nurse Practitioners (AANP) and American Academy of Physician Associates (AAPA) in 2022.16,21 For NPs, these SOP categories were based on the 3 practice environment determinations used by the AANP.16 For PAs, we used the AAPA's Six Elements of a Modern PA Practice Act, which include full prescriptive authority and adaptable collaboration requirements,21 and consistent with prior analyses, categorized PA SOP into 3 groups based on the number of elements each state had enacted: 1–2 elements = restricted, 3–4 elements = reduced, and 5–6 elements = full practice.22,23 Postsurvey weights were adjusted in all analyses. Analyses were performed in Stata SE 17 (StataCorp, College Station, TX).
Limitations
This study is not without limitations. First, although a rigorous approach to sampling and weighting was used, the NSSP 2022 data may still suffer from selection and recall bias. Second, the data are self-reported, and thus, may be subject to respondent bias. Third, the data did not allow us to differentiate among various types of working relationships within practices that exist between physicians and PAs/NPs. Physician assistants/NPs often practice under policies set by their employers or organizations that restrict clinical practice more than what the state regulation allows. These organizational-level policies may have a stronger influence on how physicians perceive working with PAs/NPs.24 That is, in practices where a high level of physician oversight or supervision of PA/NP practice is required (eg, reviewing charts, signing orders), respondents may perceive different effects on the outcomes of interest than physicians who work in practices where they serve in a more consultative role and where PAs and NPs work more independently.25 Fourth, there are many other important aspects of interprofessional relationships that were not measured or controlled in our study, such as the length and frequency of working together, interpersonal dynamics, and role delineation.
Results
Study population
There were 5917 physicians in our analytical sample, of which 63% were men and 67% were White. Table 1 displays summary statistics for all independent variables included in the regression analyses.
Table 1.
Summary statistics for study variables.
| No. | Percentage (unweighted) | Percentage (weighted) | SD (weighted) | |
|---|---|---|---|---|
| Routinely worked with PA(s) (prevalence) | 5882 | 43 | 43 | 0.49 |
| Routinely worked with NP(s) (prevalence) | 5853 | 47 | 46 | 0.50 |
| Gendera | ||||
| Women | 1792 | 30 | 37 | 0.48 |
| Men | 4085 | 69 | 63 | 0.48 |
| Other | 40 | 0 | 0 | 0.05 |
| Race and ethnicity | ||||
| White | 5917 | 65 | 67 | 0.47 |
| African American/Black | 5917 | 3 | 2 | 0.15 |
| Asian | 5917 | 25 | 26 | 0.44 |
| Hispanic or Latinx | 5917 | 4 | 3 | 0.18 |
| American Indian and Alaska Native | 5917 | 1 | 1 | 0.07 |
| Native Hawaiian and Pacific Islander | 5917 | 0 | 0 | 0.05 |
| Other race and ethnicity | 5917 | 2 | 2 | 0.15 |
| Employer type (multiple selections) | ||||
| Employee | 5914 | 65 | 64 | 0.48 |
| Owner | 5914 | 25 | 26 | 0.44 |
| Independent contractor | 5914 | 9 | 09 | 0.28 |
| Other | 5914 | 0 | 0 | 0.11 |
| Specialty group | ||||
| Medical specialties | 5917 | 21 | 17 | 0.38 |
| Primary care | 5917 | 32 | 31 | 0.46 |
| Surgery | 5917 | 19 | 18 | 0.39 |
| Other | 5917 | 28 | 33 | 0.47 |
| Working full-time | 5917 | 83 | 82 | 0.38 |
| Practice setting (multiple selections) | ||||
| Medical school | 5917 | 6 | 7 | 0.25 |
| Teaching hospital | 5917 | 19 | 17 | 0.37 |
| Non-teaching hospital | 5917 | 7 | 7 | 0.25 |
| Group practice | 5917 | 20 | 20 | 0.40 |
| Government facility | 5917 | 3 | 3 | 0.18 |
| Health care system | 5917 | 15 | 16 | 0.36 |
| Private practice—solo | 5917 | 9 | 10 | 0.30 |
| Locum tenens | 5917 | 2 | 2 | 0.14 |
| Private practice—single specialty group | 5917 | 22 | 21 | 0.41 |
| Private practice—multi-specialty group | 5917 | 8 | 9 | 0.28 |
| Other setting | 5917 | 3 | 2 | 0.15 |
| International medical graduate | 5917 | 15 | 19 | 0.39 |
| High-rural serving | 5831 | 16 | 15 | 0.36 |
| No. | Mean (unweighted) | Mean (weighted) | SD (weighted) | |
|---|---|---|---|---|
| Number of PAs routinely worked with | 2551 | 7.62 | 7.68 | 16.76 |
| Number of NPs routinely worked with | 2775 | 6.05 | 5.74 | 12.93 |
| Age | 5917 | 52.00 | 53.88 | 10.84 |
| PA scope of practice (1 = most restrictive to 3 = most permissive) | 5864 | 1.97 | 1.96 | 0.75 |
| NP scope of practice (1 = most restrictive to 3 = most permissive) | 5864 | 1.91 | 1.90 | 0.84 |
| Proportion of women in specialty | 5771 | 36.07 | 36.27 | 14.73 |
| Annual income (categorized 1—11) | 5862 | 6.21 | 6.25 | 2.70 |
Abbreviations: AAMC, Association of American Medical Colleges; NP, nurse practitioner; PA, physician assistant.
Source: National Sample Survey of Physicians 2022, AAMC. Weight adjusted.
aFor Gender, “Women” includes trans-women, “Men” includes trans-men, and “Other” includes agender, genderqueer, nonbinary and other.
Prevalence of working with PAs or NPs
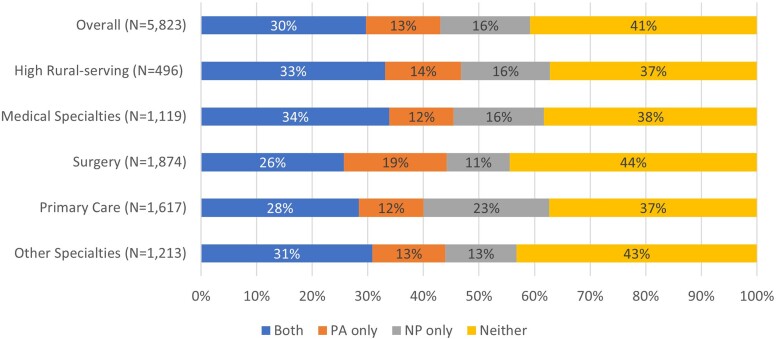
Overall, 59% of respondent physicians reported working with PAs and/or NPs (Figure 1): 30% reported working with both PA(s) and NP(s), 13% reported working with PA(s) only, and 16% reported working with NP(s) only. Forty-one percent of physicians reported that they did not work with PAs or NPs. Almost two-thirds (63%) of high-rural-serving physicians reported working with PAs and/or NPs. Across practice specialties, physicians in primary care and medical specialties were slightly more likely to report working with PAs and/or NPs (63% and 62%, respectively) compared with physicians in surgery (56%) or other specialties (57%). Notably, the specialty with the highest percentage of physicians who reported working only with NPs was primary care (23%), and physicians in surgery were the most likely to work with only PAs (19%).
Figure 1.
Proportions of physicians who report working with physician assistants (PAs) and/or nurse practitioners (NPs). Source: National Sample Survey of Physicians 2022, Association of American Medical Colleges (AAMC). Values are weight adjusted. A chi-square test was conducted to determine the significance of the differences among 4 groups of specialties (Pearson’s χ2[9] = 2.1e+04; p = 0.000). A chi-square test was conducted to determine the significance of the differences between high- and low-rural-serving (not shown in the figure) physicians. (Pearson’s χ2[3] = 546.1461; p = 0.000).
Physicians’ perceptions of working with PAs and NPs on clinical practice
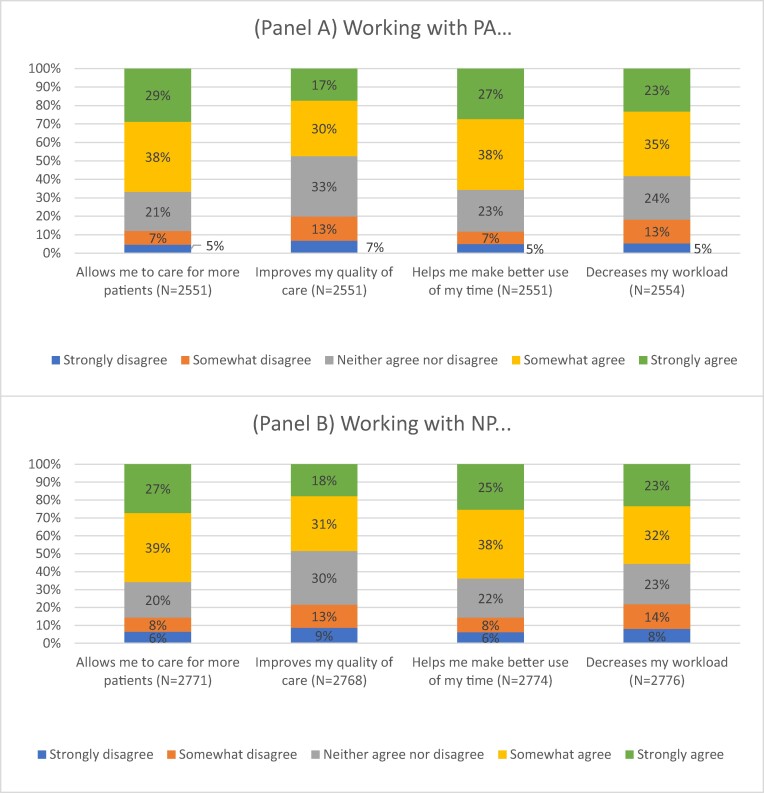
Most physicians reported that working with PAs and NPs positively affected their clinical practice (Figure 2). Across the 4 outcomes of interest, 47% to 67% of physicians somewhat agreed or strongly agreed that working with PA(s) positively impacted clinical practice (Figure 2A) and 49% to 66% of physicians somewhat agreed or strongly agreed that working with NP(s) did the same (Figure 2B). The greatest perceived impacts of working with PAs and/or NPs were on patient volume (67% and 66% agreement, respectively) and time use (65% and 63% agreement, respectively). There was less agreement among physicians that working with PAs and NPs improved quality of care and decreased workloads, with approximately 20% of physicians reporting disagreement (somewhat disagree, disagree) for each of these 2 outcomes.
Figure 2.
Physicians’ perceptions of working with physician assistants (PAs) and nurse practitioners (NPs) on clinical practice. Source: National Sample Survey of Physicians 2022, Association of American Medical Colleges (AAMC). Values are weight adjusted. Bar labels are outcomes of interest: “Allows me to care for more patients” (patient volume); “Improves my quality of care” (improved quality); “Helps me make better use of my time” (time use); and “Decreases my workload” (decreased workload). We conducted 2 series of 6 paired t tests (6 for PA statements and 6 for NP statements) to compare the means of agreement (including strongly agree and agree) in each pair of the 4 statements. Except for “PA patient volume” and “PA time use” (not significant), and “NP patient volume” and “NP time use” (p[T > t] = 0.001), all other 10 pairs showed a statistically significant difference in an agreement pattern with p < 0.000.
Estimated perceived impact of working with PAs and NPs on clinical practice
The following results discussion refers to Tables 2 and 3 that display the results of the ordinal logistic regressions for the associations between the 4 outcomes of interest (patient volume, improved quality, time use, decreased workload) and all independent variables. Overall, there were no statistically significant associations between the number of PAs (Table 2) or NPs (Table 3) with whom physicians worked and the outcomes.
Table 2.
Estimated perceived impact of working with PAs on clinical practice by physician demographic and work characteristics.
| Ordered logistic regression estimates | ||||
|---|---|---|---|---|
| Patient volume | Care quality | Time use | Decreased workload | |
| Intensity PA | 0.998 (−0.36) | 0.997 (−0.77) | 0.996 (−0.78) | 1.000 (0.04) |
| Age | 1.006 (0.94) | 1.003 (0.47) | 1.020** (2.99) | 1.007 (1.04) |
| Gendera | ||||
| Women (reference) | 1.0 | 1.0 | 1.0 | 1.0 |
| Men | 1.167 (1.07) | 1.130 (0.78) | 1.116 (0.75) | 1.132 (0.85) |
| Other | 0.661 (−0.30) | 0.891 (−0.10) | 1.177 (0.20) | 0.882 (−0.13) |
| Race and ethnicity | ||||
| White | 1.290 (0.50) | 1.726 (1.29) | 1.030 (0.06) | 0.752 (−0.53) |
| African American/Black | 1.189 (0.28) | 2.002 (1.45) | 1.438 (0.61) | 0.592 (−0.81) |
| Asian | 1.775 (1.12) | 2.175 (1.85) | 1.428 (0.72) | 1.001 (0.00) |
| Hispanic or Latino | 1.882 (1.11) | 3.252** (2.59) | 1.599 (0.85) | 1.283 (0.43) |
| American Indian and Alaska Native | 0.402 (−1.60) | 1.376 (0.71) | 0.619 (−0.80) | 0.407 (−1.39) |
| Native Hawaiian and Pacific Islander | 1.770 (0.53) | 1.005 (0.00) | 0.547 (−0.33) | 0.248 (−0.62) |
| Other race and ethnicity | 1.361 (0.49) | 2.809 (1.65) | 1.097 (0.15) | 1.112 (0.16) |
| Employer type | ||||
| Employee (reference) | 1.0 | 1.0 | 1.0 | 1.0 |
| Owner | 1.161 (0.65) | 0.866 (−0.66) | 0.973 (−0.12) | 1.038 (0.15) |
| Independent | 1.279 (1.00) | 1.284 (0.84) | 0.977 (−0.09) | 1.133 (0.41) |
| Other | 2.417 (1.54) | 1.834 (1.67) | 4.789** (2.85) | 2.454 (1.71) |
| High-rural serving | 0.823 (−1.11) | 0.971 (−0.16) | 0.993 (−0.04) | 1.006 (0.03) |
| Specialty group | ||||
| Medical specialties (reference) | 1.0 | 1.0 | 1.0 | 1.0 |
| Other | 0.926 (−0.41) | 0.811 (−1.10) | 1.134 (0.64) | 1.165 (0.80) |
| PCP | 0.833 (−1.04) | 0.800 (−1.32) | 0.803 (−1.25) | 0.960 (−0.24) |
| Surgery | 1.039 (0.19) | 1.668* (2.44) | 1.145 (0.64) | 1.157 (0.69) |
| Full-time status | 0.890 (−0.57) | 1.015 (0.07) | 0.906 (−0.50) | 0.940 (−0.32) |
| PA scope of practice (1 = most restrictive to 3 = most permissive) | 0.818* (−2.51) | 1.016 (0.19) | 0.948 (−0.66) | 1.035 (0.42) |
| Practice setting | ||||
| Medical school | 1.853* (2.25) | 2.641*** (3.72) | 3.078*** (4.31) | 2.768*** (3.86) |
| Teaching hospital | 1.015 (0.07) | 1.019 (0.08) | 1.139 (0.59) | 1.244 (1.01) |
| Non-teaching hospital | 0.577* (−2.09) | 0.867 (−0.52) | 0.862 (−0.53) | 0.781 (−0.88) |
| Group practice | 0.780 (−1.34) | 1.146 (0.71) | 0.905 (−0.50) | 0.926 (−0.37) |
| Government facility | 0.635 (−1.21) | 0.860 (−0.39) | 1.212 (0.50) | 1.027 (0.06) |
| Health care system | 1.041 (0.20) | 1.270 (1.18) | 0.989 (−0.05) | 1.123 (0.57) |
| Private practice—solo | 0.920 (−0.23) | 1.409 (0.89) | 0.983 (−0.05) | 1.136 (0.34) |
| Locum tenens | 0.471 (−1.89) | 0.478 (−1.94) | 1.039 (0.09) | 1.067 (0.14) |
| Private practice—single specialty group | 0.959 (−0.17) | 1.109 (0.41) | 1.354 (1.22) | 1.218 (0.70) |
| Private practice—multi-specialty group | 1.104 (0.38) | 1.403 (1.37) | 1.157 (0.58) | 1.394 (1.24) |
| Other setting | 0.516 (−1.53) | 0.759 (−0.61) | 0.660 (−0.87) | 1.035 (0.08) |
| International medical graduate | 0.741 (−1.63) | 0.615** (−2.63) | 0.623* (−2.44) | 0.668* (−2.11) |
| Women's representation at own specialty | 0.987* (−2.49) | 0.988* (−2.40) | 0.989* (−2.18) | 0.986** (−2.68) |
| Income level | 1.125*** (3.63) | 1.080* (2.25) | 1.162*** (4.60) | 1.152*** (4.46) |
| Ordered logistic regression cutpoint 1 | 0.0619*** (−3.51) | 0.179* (−2.32) | 0.239 (−1.86) | 0.117* (−2.40) |
| Ordered logistic regression cutpoint 2 | 0.177* (−2.18) | 0.629 (−0.64) | 0.622 (−0.62) | 0.500 (−0.80) |
| Ordered logistic regression cutpoint 3 | 0.712 (−0.43) | 3.189 (1.58) | 2.693 (1.28) | 1.727 (0.63) |
| Ordered logistic regression cutpoint 4 | 4.124 (1.79) | 15.37*** (3.69) | 17.11*** (3.64) | 9.559** (2.61) |
| n | 2406 | 2406 | 2406 | 2408 |
Abbreviations: PA, physician assistant; PCP, primary care provider.
Values are exponentiated coefficients; t statistics in parentheses. Weight adjusted. *P < .05; **P < .01; ***P < .001.
aFor Gender, “Women” includes trans-women, “Men” includes trans-men, and “Other” includes agender, genderqueer, nonbinary and other.
Table 3.
Estimated perceived impact of working with NPs on clinical practice by physician demographic and work characteristics.
| Ordered logistic regression estimates | ||||
|---|---|---|---|---|
| Patient volume | Care quality | Time use | Decreased workload | |
| Intensity NP | 1.000 (−0.09) | 0.998 (−0.27) | 0.998 (−0.49) | 0.992 (−1.54) |
| Age | 1.001 (0.18) | 1.009 (1.42) | 1.010 (1.63) | 1.005 (0.84) |
| Gendera | ||||
| Women (reference) | 1.0 | 1.0 | 1.0 | 1.0 |
| Men | 1.315 (1.87) | 1.065 (0.42) | 1.254 (1.59) | 1.224 (1.44) |
| Other | 1.326 (0.12) | 0.172** (−3.03) | 1.433 (0.20) | 3.569 (1.02) |
| Race and ethnicity | ||||
| White | 2.223* (2.02) | 1.807 (1.26) | 0.623 (−1.32) | 2.012 (1.82) |
| African American/Black | 1.808 (1.11) | 1.619 (0.89) | 0.668 (−0.86) | 1.332 (0.57) |
| Asian | 2.159 (1.92) | 1.894 (1.33) | 0.652 (−1.17) | 2.152 (1.94) |
| Hispanic or Latino | 2.382 (1.90) | 3.087* (2.30) | 1.183 (0.41) | 2.339* (2.02) |
| American Indian and Alaska Native | 0.589 (−1.01) | 0.951 (−0.07) | 0.511 (−1.21) | 1.543 (0.58) |
| Native Hawaiian and Pacific Islander | 59.99*** (3.43) | 146.7*** (4.57) | 19.03* (2.50) | 93.97*** (3.92) |
| Other race and ethnicity | 3.730* (2.18) | 3.560 (1.83) | 0.592 (−0.97) | 3.309* (2.07) |
| Employer type | ||||
| Employee (reference) | 1.0 | 1.0 | 1.0 | 1.0 |
| Owner | 1.422 (1.69) | 1.103 (0.48) | 1.103 (0.45) | 1.030 (0.14) |
| Independent | 0.910 (−0.27) | 0.584 (−1.61) | 0.581 (−1.58) | 0.815 (−0.61) |
| Other | 1.901 (1.71) | 0.428* (−2.10) | 2.220 (1.35) | 3.753* (2.53) |
| High-rural serving | 1.015 (0.10) | 0.877 (−0.82) | 0.978 (−0.13) | 1.059 (0.33) |
| Specialty group | ||||
| Medical specialties (reference) | 1.0 | 1.0 | 1.0 | 1.0 |
| Other | 0.715 (−1.73) | 0.723 (−1.69) | 0.863 (−0.78) | 1.188 (0.97) |
| PCP | 0.732* (−1.96) | 0.657** (−2.60) | 0.697* (−2.17) | 1.070 (0.42) |
| Surgery | 0.693 (−1.88) | 1.008 (0.04) | 1.014 (0.07) | 1.165 (0.76) |
| Full-time status | 0.757 (−1.34) | 0.726 (−1.42) | 0.647* (−2.05) | 0.666* (−2.10) |
| NP scope of practice (1 = most restrictive to 3 = most permissive) | 0.813** (−2.67) | 0.945 (−0.74) | 0.880 (−1.66) | 0.960 (−0.55) |
| Practice setting | ||||
| Medical school | 1.909* (2.56) | 1.630 (1.91) | 1.474 (1.55) | 2.525*** (3.60) |
| Teaching hospital | 1.153 (0.71) | 1.098 (0.48) | 1.127 (0.62) | 1.184 (0.88) |
| Non-teaching hospital | 0.644 (−1.56) | 0.686 (−1.32) | 0.745 (−1.08) | 0.660 (−1.50) |
| Group practice | 0.942 (−0.29) | 0.940 (−0.32) | 0.761 (−1.38) | 0.876 (−0.67) |
| Government facility | 0.738 (−0.85) | 0.660 (−1.18) | 0.895 (−0.32) | 0.781 (−0.75) |
| Health care system | 1.323 (1.35) | 1.020 (0.10) | 1.070 (0.35) | 1.035 (0.18) |
| Private practice—solo | 1.031 (0.09) | 0.915 (−0.29) | 0.881 (−0.36) | 1.144 (0.43) |
| Locum tenens | 0.857 (−0.35) | 0.584 (−1.33) | 0.983 (−0.04) | 0.855 (−0.37) |
| Private practice—single specialty group | 1.256 (0.97) | 0.947 (−0.24) | 1.326 (1.21) | 1.374 (1.37) |
| Private practice—multi-specialty group | 1.424 (1.33) | 1.111 (0.47) | 1.445 (1.40) | 1.300 (1.09) |
| Other setting | 0.949 (−0.11) | 0.861 (−0.37) | 0.562 (−1.33) | 0.929 (−0.14) |
| International medical graduate | 0.875 (−0.73) | 0.855 (−0.94) | 0.893 (−0.66) | 1.104 (0.60) |
| Women's representation at own specialty | 0.997 (−0.67) | 0.995 (−1.07) | 0.995 (−1.02) | 0.996 (−0.78) |
| Income level | 1.118*** (3.93) | 1.062* (2.06) | 1.124*** (4.13) | 1.141*** (4.49) |
| Ordered logistic regression cutpoint 1 | 0.145* (−2.58) | 0.166* (−2.26) | 0.0604*** (−3.76) | 0.386 (−1.29) |
| Ordered logistic regression cutpoint 2 | 0.369 (−1.34) | 0.485 (−0.91) | 0.155* (−2.57) | 1.320 (0.38) |
| Ordered logistic regression cutpoint 3 | 1.232 (0.28) | 2.035 (0.90) | 0.567 (−0.79) | 3.989 (1.87) |
| Ordered logistic regression cutpoint 4 | 7.099** (2.63) | 9.743** (2.88) | 3.298 (1.67) | 18.33*** (3.91) |
| n | 2639 | 2637 | 2642 | 2644 |
Abbreviations: NP, nurse practitioner; PCP, primary care provider.
Values are exponentiated coefficients; t statistics in parentheses. Weight adjusted. *P < .05; **P < .01; ***P < .001.
aFor Gender, “Women” includes trans-women, “Men” includes trans-men, and “Other” includes agender, genderqueer, nonbinary and other.
Although physician characteristics, such as gender, age, and race/ethnicity, explained very little of their perceptions working with PAs or NPs, some exceptions emerged: older physicians had higher odds of agreeing that working with PAs helps make better use of their time (odds ratio [OR] = 1.020, P < .01); physicians reporting their gender identity as “other” had lower odds of agreeing that working with NPs improves their quality of care (OR = 0.172, P < .01); Hispanic and Latino physicians had higher odds of agreeing that working with PAs and NPs increases their quality of care (OR = 3.252, P < .01, and OR = 3.087, P < .05), and they were also more likely to agree that working with NPs decreases their workload (OR = 2.339, P < .05); White physicians had higher odds agreeing that working with NPs improved patient volume (OR = 2.223, P < .05); and Native Hawaiian and Pacific Islander physicians had higher odds of agreeing that working with NPs improved all aspects of their clinical practices (ORs ranged from 19.03 to 146.7, P < .05–.001). Also, physicians of other races and ethnicities had higher odds agreeing that working with NPs increased patient volume (OR = 3.730, P < .05) and decreased workload (OR = 3.309, P < .05).
Compared with physicians who are employees, physicians reporting “other” employment status had higher odds of agreeing that working with PAs improved the use of their time (OR = 4.789, P < .01) and that working with NPs decreased their workload (OR = 3.753, P < .05), but they had lower odds of agreeing that working with NPs improved their quality of care (OR = 0.428, P < .05). Physicians’ perceived impact of working with PAs and NPs on their clinical practice did not significantly differ by rural-serving status.
Compared with physicians in medical specialties, surgeons had higher odds (OR = 1.668, P < .05) of agreeing that working with PAs improved quality of care. Physicians in primary care had lower odds of agreeing that working with NPs improved patient volume (OR = 0.732, P < .05), quality of care (OR = 0.657, P < .01), and time use (OR = 0.697, P < .05).
Physicians working full time, compared with those working part-time, reported lower odds of agreeing that working with NPs helped them make better use of their time (OR = 0.647, P < .05) or decreased their workload (OR = 0.666, P < .05). Both PA and NP SOPs were negatively associated with patient volume (OR = 0.818, P < .05, and OR = 0.813, P < .01, respectively). That is, physicians working in states with less-restrictive SOP regulations for PAs or NPs had lower odds of agreeing that working with a PA or NP increased the number of patients they could see. No other clinical practice outcome was statistically related to SOP.
In terms of work settings, physicians who work in medical schools had higher odds of agreeing that working with PAs improved all 4 outcomes: increased volume (OR = 1.853, P < .05), quality of care (OR = 2.641, P < .001), time use (OR = 3.078, P < .001), and decreased workload (OR = 2.768, P < .001). Physicians who work in medical schools also reported higher odds of agreeing that working with an NP increased patient volume (OR = 1.909, P < .05) and decreased workload (OR = 2.525, P < .001).
International medical graduates had lower odds of agreeing that working with a PA increased quality of patient care (OR = 0.615, P < .01) or time use (OR = 0.628, P < .05) or decreased workload (OR = 633, P < .05). Also, as the proportion of women represented in a specialty increased, physicians were less likely to agree that working with a PA improved patient volume, quality of care, time use, and workload. Finally, as reported annual income increased, physicians were more likely to agree that working with PAs and NPs had a positive impact on all aspects of their clinical practices.
Discussion
Using new, nationally represented physician survey data, the results of this study update the literature on the contributions of PAs and NPs to clinical practice. We found that primary care and high-rural-serving physicians were the most likely to report regularly working with PAs and/or NPs, which aligns with existing literature,26 although we were surprised to find no reported impact on practice for high-rural-serving physicians. Considering that primary care is the most common practice area for NPs, our finding that primary care physicians were the most likely to report working with only NPs was not surprising. Additionally, surgeons were the most likely to report working with PAs, which aligns with a 2022 report indicating that surgery is a top practice setting for PAs.27 Although approximately one-half to two-thirds of physicians reported that working with PAs or NPs positively impacted aspects of their clinical practice (Figure 2), we did not find any statistically significant relationships between the number of PAs or NPs with whom a physician works and our outcomes of interest, suggesting that other factors are more salient to improved clinical practice than the mere quantity of PAs and NPs. We did separate physicians’ perceptions of working with PAs from their perceptions of work with NPs, which produced some insights that may be uniquely relevant to PA or to NP practice.
The statistically significant but very modest association between older physician age and greater agreement that PAs improved time use indicates that greater experience with PAs may contribute to more productive working relationships. Our finding that physicians who work in medical schools had higher odds of agreeing that working with PAs and NPs improved their clinical practice may also reflect greater familiarity with the roles of PAs and NPs. A majority of medical schools require interprofessional education (AAMC),28 which involves learning about the roles and responsibilities of other health care professionals as well as best practices for effective collaboration.29 As a result, physicians who are affiliated with or work in medical schools may be better prepared than other physicians to engage in productive working relationships with PAs and NPs. Our finding that IMGs are less likely to report that working with PAs improves their clinical practice extends this notion, since IMGs may lack familiarity with the PA role and the interprofessional work environment in the United States.30
Our results that primary care physicians were less likely to agree that NPs positively contribute to quality of care and time use may partly stem from the fact that, in primary care, NPs provide many of the same services that physicians provide.31 That is, NPs may be spending less time providing care that complements or expands physician services than in other specialties. Also, while PAs in primary care also provide many of the same services that physicians do,10,32 state SOP laws allow for greater NP autonomy in more than half the states.16 Thus, NPs may be more likely than PAs to be working independently. Relatedly, our finding that physicians working in states with less-restrictive PA/NP SOP were less likely to agree that PAs or NPs improved patient volume may reflect that, in these states, NPs and PAs may be more likely to be viewed as working alongside rather than under the supervision of physicians.
Small studies that focused on the contributions of PAs to surgical practices have shown that their employment was associated with reduced resident workloads33 and surgeons’ direct procedural time, allowing the surgeon to engage in other patient care activities.34 Similarly, we found a positive relationship between surgeons’ agreement that working with PAs positively contributes to their clinical practice, specifically quality of care. Surgical training is required for all PA students,31 and while just 5.4% of PAs complete additional postgraduate specialty training, which is optional, postgraduate surgical programs are among those most frequently pursued.35 Thus, surgeons’ positive perceptions of working with PAs on quality of care may reflect both their familiarity with PAs as well as PA surgical training.
Interestingly, we found that physicians who work in specialties with a higher representation of women had lower agreement that working with PAs improved clinical practice in all 4 aspects. Women's representation in the practice environment has been receiving increasing attention as a factor affecting physician outcomes, ranging from income,34 income equity,36-38 and workplace safety.39 Although this relationship warrants further research, the finding that women's representation in a specialty was associated with a reduced odds of agreeing that PAs positively contribute to their clinical practice may reflect the fact that PAs receive relatively less training in specialties with high proportions of women physicians (eg, pediatrics and OBGYN [obstetrics/gynecology]). While PA education requires training in these specialty areas, relatively few optional postgraduate programs for PAs focus on them.17 Furthermore, less than 2% of PAs practice in women's health, and just over 3% practice in general pediatrics or a pediatric subspecialty.35 Notably, no significant associations (positive or negative) were found between women's representation in the specialty and perceptions of NP influence on clinical practice. While proportions of NPs certified in these areas of practice are just slightly higher, as previously noted, there are twice as many NPs as PAs in the United States. Additionally, unlike PA education, NP education is population-focused, with options that include a focus on neonatology, pediatrics, or women's health.40
Last, that high physician income was associated with greater agreement that PAs and NPs improved clinical practice for our 4 outcomes of interest suggests that PAs and NPs may perform tasks that complement or expand physician services, allowing these physicians and their organizations to expand services, increase productivity, and improve care delivery overall. For example, in surgical specialties (the highest-paying physician specialty41), while PAs and NPs can assist and perform many pre- and postoperative tasks, they cannot perform major surgery.42,43 Thus, incorporating PAs and NPs into practices has the potential to free up physicians to perform procedures that lead to greater practice revenue and physicians’ earnings.44 Consequently, this defined role delineation and labor allocation within practices may positively impact various aspects of physicians’ clinical practices.
Conclusion
Health care is becoming increasingly complex, demand for services continues to grow, and the PA and NP professions are rapidly expanding.45 As a result, physicians will increasingly be working with these advanced-practice clinicians. This study adds to the growing body of literature focused on PA and NP contributions to the health care system. Although physician perceptions of working with PAs and NPs is just one way to measure their contributions to clinical practice, our results can be useful for policymakers and administrators to inform approaches to effective care delivery reform. Patient and care delivery outcomes are positive with PA- and NP-delivered care, and our study shows that physicians who work with PAs and NPs view these working relationships as positive to their own clinical practice. Adding PAs and NPs to the clinical staff across settings and specialties can improve care delivery and patient outcomes, as well as contribute to improving the workload of other clinicians in the same practice. While our study results reveal that most physicians had positive perceptions of PA and NP influence on at least some aspect of their clinical practice, some differences emerged that warrant additional study. Further research on interprofessional dynamics, the impact of clinician role delineation across specialties and settings and care delivery models, physician exposure to PAs and NPs, and PA or NP postgraduate training is needed.
Supplementary Material
Acknowledgments
Data collection of the National Sample Survey of Physicians was sponsored by the Association of American Medical Colleges (AAMC). The authors thank Merle Haberman and Jonathan Jaffery at the AAMC for their insightful input in reviewing the draft and Chris Tracy at the AANP for her help with the SOP data collection.
Contributor Information
Xiaochu Hu, Association of American Medical Colleges, Workforce Studies, Washington, DC 20001, United States.
Bettie Coplan, Northern Arizona University, College of Health and Human Services, Phoenix, AZ 85004, United States.
Hilary Barnes, Widener University, School of Nursing, Chester, PA 19013, United States.
Noël Smith, American Academy of Physician Associates, Research Department, Alexandria, VA 22314, United States.
Alison Essary, Northern Arizona University, College of Health and Human Services, Phoenix, AZ 85004, United States.
Michael Dill, Association of American Medical Colleges, Workforce Studies, Washington, DC 20001, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Notes
- 1. Bureau of Labor Statistics . May 2022 National Occupational Employment and Wage Estimates. Occupational Employment and Wage Statistics. Accessed October 16, 2023. https://www.bls.gov/oes/current/oes_nat.htm#29-0000
- 2. Barnes H, Richards MR, McHugh MD, Martsolf G. Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Aff (Millwood). 2018;37(6):908–914. 10.1377/hlthaff.2017.1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martsolf GR, Barnes H, Richards MR, Ray KN, Brom HM, McHugh MD. Employment of advanced practice clinicians in physician practices. JAMA Intern Med. 2018;178(7):988–990. 10.1001/jamainternmed.2018.1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patel SY, Auerbach D, Huskamp HA, et al. Provision of evaluation and management visits by nurse practitioners and physician assistants in the USA from 2013 to 2019: cross-sectional time series study. BMJ. 2023;382:e073933. 10.1136/bmj-2022-073933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peterson LE, Blackburn B, Petterson S, Puffer JC, Bazemore A, Phillips RL. Which family physicians work routinely with nurse practitioners, physician assistants or certified nurse midwives. J Rural Health. 2014;30(3):227–234. 10.1111/jrh.12053 [DOI] [PubMed] [Google Scholar]
- 6. Dai M, Ingham RC, Peterson LE. Scope of practice and patient panel size of family physicians who work with nurse practitioners or physician assistants. Fam Med. 2019;51(4):311–318. 10.22454/FamMed.2019.438954 [DOI] [PubMed] [Google Scholar]
- 7. Kleinpell RM, Grabenkort WR, Kapu AN, Constantine R, Sicoutris C. Nurse practitioners and physician assistants in acute and critical care: a concise review of the literature and data 2008-2018. Crit Care Med. 2019;47(10):1442–1449. 10.1097/CCM.0000000000003925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kurtzman ET, Barnow BS. A comparison of nurse practitioners, physician assistants, and primary care physicians’ patterns of practice and quality of care in health centers. Med Care. 2017;55(6):615–622. 10.1097/MLR.0000000000000689 [DOI] [PubMed] [Google Scholar]
- 9. Yang Y, Long Q, Jackson SL, et al. Nurse practitioners, physician assistants, and physicians are comparable in managing the first five years of diabetes. Am J Med. 2018;131(3):276–283.e2. 10.1016/j.amjmed.2017.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pany MJ, Chen L, Sheridan B, Huckman RS. Provider teams outperform solo providers in managing chronic diseases and could improve the value of care. Health Aff (Millwood). 2021;40(3):435–444. 10.1377/hlthaff.2020.01580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Auerbach DI, Levy DE, Maramaldi P, et al. Optimal staffing models to care for frail older adults in primary care and geriatrics practices in the US. Health Aff (Millwood). 2021;40(9):1368–1376. 10.1377/hlthaff.2021.00401 [DOI] [PubMed] [Google Scholar]
- 12. Physician Assistant Education Association; Chitwood R, Yuen C. By the Numbers: Program Report 35. Physician Assistant Education Association; 2020. 10.17538/PR35.2020 [DOI] [Google Scholar]
- 13. Cawley JF. Physician assistants and their role in primary care. AMA J Ethics. 2012;14(5):411–414. 10.1001/virtualmentor.2012.14.5.pfor2-1205 [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Physician Associates (AAPA). PA licensure, how does your state compare? Accessed January 17, 2024. https://www.aapa.org/advocacy-central/constituent-organizations/pa-licensure-state-compare/
- 15.American Association of Nurse Practitioners. What's a nurse practitioner (NP)? Accessed January 17, 2024. https://www.aanp.org/about/all-about-nps/whats-a-nurse-practitioner
- 16.American Association of Nurse Practitioners. Nurse practitioners state practice environment. Accessed September 15, 2023. https://www.aanp.org/advocacy/state/state-practice-environment
- 17. Morgan P, Barnes H, Batchelder HR, et al. Nurse practitioner and physician assistant transition to practice: a scoping review of fellowships and onboarding programs. J Am Assoc Nurse Pract. 2023;35(12):776–783. 10.1097/JXX.0000000000000932 [DOI] [PubMed] [Google Scholar]
- 18. Virarkar M, Coleman JA, Siddiqui ZA, et al. PAs and NPs improve patient care and productivity in a radiology consult practice. JAAPA. 2022;35(7):46–51. 10.1097/01.jaa.0000832596.64788.f1 [DOI] [PubMed] [Google Scholar]
- 19. Bergeson J, Cash R, Boulger J, Bergeron D. The attitudes of rural Minnesota family physicians toward nurse practitioners and physician assistants. J Rural Health. 1997;13(3):196–205. 10.1111/j.1748-0361.1997.tb00843.x [DOI] [PubMed] [Google Scholar]
- 20.Association of American Medical Colleges. AAMC National Sample Survey of Physicians 2022: Documentation for Sampling and Weights. 2023. Accessed January 17, 2024. https://www.aamc.org/media/71861/download?attachment
- 21.American Academy of Physician Associates (AAPA) . The six key elements of a modern PA practice act. 2017. Accessed April 26, 2024. https://www.aapa.org/wp-content/uploads/2017/01/Issue-brief_Six-key-elements_0117-1.pdf
- 22. Valentin VL, Najmabadi S, Everett C. Cross-sectional analysis of US scope of practice laws and employed physician assistants. BMJ Open. 2021;11(5):e043972. 10.1136/bmjopen-2020-043972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. White RD. Examining the influence of physician assistant/associate scope of practice reforms and individual characteristics on wages. Med Care Res Rev. 2023;80(4):386–395. 10.1177/10775587231165351 [DOI] [PubMed] [Google Scholar]
- 24. O’Reilly-Jacob M, Perloff J, Sherafat-Kazemzadeh R, Flanagan J. Nurse practitioners’ perception of temporary full practice authority during a COVID-19 surge: a qualitative study. Int J Nurs Stud. 2022;126:104141. 10.1016/j.ijnurstu.2021.104141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Poghosyan L, Boyd DR, Clarke SP. Optimizing full scope of practice for nurse practitioners in primary care: a proposed conceptual model. Nurs Outlook. 2016;64(2):146–155. 10.1016/j.outlook.2015.11.015 [DOI] [PubMed] [Google Scholar]
- 26. Willis J, Antono B, Bazemore A, et al. The State of Primary Care in the United States: A Chartbook of Facts and Statistics. Robert Graham Center; 2020. Accessed October 24, 2023. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook2021.pdf [Google Scholar]
- 27.National Commission on Certification of Physician Assistants (NCCPA). 2022 Statistical profile of board certified PAs. Accessed September 15, 2023. https://www.nccpa.net/wp-content/uploads/2023/04/2022-Statistical-Profile-of-Board-Certified-PAs.pdf
- 28.Association of American Medical Colleges (AAMC). Interprofessional education requirements at US medical schools. Accessed September 15, 2023. https://www.aamc.org/data-reports/curriculum-reports/data/interprofessional-education-requirements-us-medical-schools
- 29. van Diggele C, Roberts C, Burgess A, Mellis C. Interprofessional education: tips for design and implementation. BMC Med Educ. 2020;20(Suppl 2):455. 10.1186/s12909-020-02286-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chowdhury N, Ekpekurede M, Lake D, Chowdhury TT.. The alternative career pathways for international medical graduates in health and wellness sector. In: Tohid H, Maibach H, eds. International Medical Graduates in the United States: A Complete Guide to Challenges and Solutions. Springer International Publishing; 2021:293–325. 10.1007/978-3-030-62249-7_18 [DOI] [Google Scholar]
- 31. Torrens C, Campbell P, Hoskins G, et al. Barriers and facilitators to the implementation of the advanced nurse practitioner role in primary care settings: a scoping review. Int J Nurs Stud. 2020;104:103443. 10.1016/j.ijnurstu.2019.103443 [DOI] [PubMed] [Google Scholar]
- 32. Morgan PA, Smith VA, Berkowitz TSZ, et al. Impact of physicians, nurse practitioners, and physician assistants on utilization and costs for complex patients. Health Aff (Millwood). 2019;38(6):1028–1036. 10.1377/hlthaff.2019.00014 [DOI] [PubMed] [Google Scholar]
- 33. Dies N, Rashid S, Shandling M, Swallow C, Easson AM, Kennedy E. Physician assistants reduce resident workload and improve care in an academic surgical setting. JAAPA. 2016;29(2):41–46. 10.1097/01.JAA.0000476214.34937.50 [DOI] [PubMed] [Google Scholar]
- 34. Resnick CM, Daniels KM, Flath-Sporn SJ, Doyle M, Heald R, Padwa BL. Physician assistants improve efficiency and decrease costs in outpatient oral and maxillofacial surgery. J Oral Maxillofac Surg. 2016;74(11):2128–2135. 10.1016/j.joms.2016.06.195 [DOI] [PubMed] [Google Scholar]
- 35. Reh S, Van Quaquebeke N, Tröster C, Giessner SR. When and why does status threat at work bring out the best and the worst in us? A temporal social comparison theory. Organ Psychol Rev. 2022;12(3):241–267. 10.1177/20413866221100200 [DOI] [Google Scholar]
- 36. Wang T, Douglas PS, Reza N. Gender gaps in salary and representation in academic internal medicine specialties in the US. JAMA Intern Med. 2021;181(9):1255–1257. 10.1001/jamainternmed.2021.3469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Whaley CM, Arnold DR, Gross N, Jena AB. Practice composition and sex differences in physician income: observational study. BMJ. 2020;370:m2588. 10.1136/bmj.m2588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dill JS, Frogner BK. The gender wage gap among health care workers across educational and occupational groups. Health Aff Sch. 2024;2(1):qxad090. 10.1093/haschl/qxad090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hu X, Conrad S, Dill M. Specialty gender composition and prevalence of physician harassment. J Womens Health. 2022;32(4):409–415. [DOI] [PubMed] [Google Scholar]
- 40.American Association of Nurse Practitioners. The Path to Becoming a Nurse Practitioner (NP). Published November 10, 2020. Accessed November 10, 2023. https://www.aanp.org/news-feed/explore-the-variety-of-career-paths-for-nurse-practitioners
- 41. Bureau of Labor Statistics . Highest paying occupations: occupational outlook handbook: U.S. Bureau of Labor Statistics. Accessed January 25, 2024. https://www.bls.gov/ooh/highest-paying.htm#
- 42. Chalupa RL, Hooker RS. The education, role, distribution, and compensation of physician assistants in orthopedic surgery. JAAPA. 2016;29(5):1–7. 10.1097/01.JAA.0000482318.38700.d1 [DOI] [PubMed] [Google Scholar]
- 43. Thourani VH, Miller JI. Physicians assistants in cardiothoracic surgery: a 30-year experience in a university center. Ann Thorac Surg. 2006;81(1):195–199. 10.1016/j.athoracsur.2005.07.031 [DOI] [PubMed] [Google Scholar]
- 44. Barnes H, Martsolf GR, McHugh MD, Richards MR. Vertical integration and physician practice labor composition. Med Care Res Rev. 2022;79(1):46–57. 10.1177/1077558720972596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Association of American Medical Colleges (AAMC). The complexities of physician supply and demand: projections from 2021 to 2036. 2024. Accessed June 3, 2024. https://www.aamc.org/media/75236/download?attachment
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.