Inequalities and inequities in health have long been central to the concerns of public health. Governments in several countries, including the United Kingdom, have recently shown renewed interest in tackling these issues.1 Concerted attempts have also been made to push them up the global health policy agenda,2–4 and at the same time international agencies and donors are giving priority to efforts to reduce poverty. In this article we provide an overview of the current debates around inequity, inequalities, poverty, and health, drawing together current international understandings of the problem.
Poverty and health: powerful connection
Although targeting “the poor” is clearly important, inequalities and inequities in health are not only about the plight of the most deprived in each society. In many low income countries, over half the population may be living in poverty and those who are not will still be living in circumstances that contribute to the poor health of the country as a whole. Even in high income countries, where there is little absolute poverty, there are fine and graduated inequalities in health status that span the full socioeconomic spectrum. For example, in a study of 300 000 men in the United States, mortality declined progressively across 12 categories of household income from less than $7500 (£5000) to more than $32 499.5
Although not all governments perceive inequalities in wealth and health to be something the public sector can or should address, all governments are interested in improving economic growth. Under the leadership of Gro Harlem Bruntland, the World Health Organization now argues forcibly that health is key to reducing poverty and to development. If improving health can have a positive effect on economic growth, then health should become a central priority of every government: “Because ill-health traps people in poverty, sustained investment in the health of the poor could provide a policy lever for alleviating persistent poverty.”6
Recent advances
There is currently a wave of international and national interest in tackling health inequalities and poverty
Per capita expenditure on health does not determine life expectancy in a country
Intelligent and equitable investment in social policy can improve health, even in poor countries with low economic growth
Comparisons of inequalities in health internationally are complicated by debates over measurement and adequacy of data
The aetiological mechanisms driving socioeconomic differences in health depend on disease and context
Effective action depends on a better understanding of the full scope of current scientific, conceptual, and policy debates
This emphasis on the potential causal link running from ill health to poverty, rather than vice versa, is contentious.7 The evidence base to support the wealth creating potential of improved health is far less substantial than the evidence relating poor health to poverty. Nevertheless, the causal links between poverty and health clearly must run in both directions to some degree and can generate a vicious or virtuous cycle. This complexity needs to be accounted for in conceptual models linking health with wealth or poverty and needs to inform strategies aimed at improving health and reducing poverty and inequalities in wealth. However, it is important not to lose sight of the intrinsic value of alleviating poverty and ill health. Poverty and ill health impair the capability of individuals to realise their own goals—and redressing that damage cannot be reduced to the economics of wealth creation.8
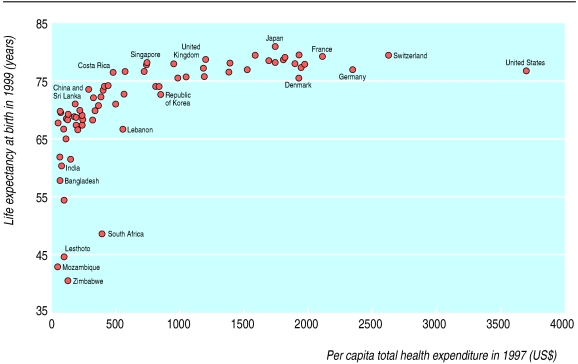
This leads to the question of the best economic strategy for improving health and welfare. Positions are divided. One argument is that priority should be given to promoting economic growth so as to accumulate sufficient wealth to then (and only then) invest adequately in programmes to tackle ill health and poverty. A second argument advocates a “support led” strategy. Even in countries where economic growth is minimal, intelligent and equitable investment in social policies can improve health and welfare.9 This view is consistent with the strikingly high life expectancy in countries such as China, Sri Lanka, and Costa Rica, where per capita wealth and expenditure on health are low by international standards (fig).
The figure provides a powerful summary of global inequalities in life expectancy and inequities in health expenditure. It also suggests that, between countries, per capita health expenditure bears little relation to life expectancy. The world is divided in two. Just over half the countries shown have an annual per capita expenditure of less than $500, one seventh of that of the United States. In this group of low spending countries there is huge variation in life expectancy. Conversely, in medium and high expenditure countries, there is huge variation in per capita expenditure, which shows almost no relation to life expectancy. Much of the international variation in mortality has to be accounted for by factors determining differences in occurrence of disease. This will include the effects of investment in the social sector, particularly in education, as well as in public health over the long term.
Contrasting perceptions
Health inequalities and inequities within countries are not understood in the same way throughout the world (box). In countries such as the United Kingdom, Sweden, and the Netherlands, much of the research on inequalities in health has focused on the mechanisms that generate socioeconomic gradients in ill health and mortality. From this perspective, inequalities in health are mainly a function of the aetiology of disease, and the policy solutions that arise are around primary prevention. In low and middle income countries, by contrast, people working on inequalities in health tend to see the problem as one of devising policies to ensure more equitable provision of health care.
Definitions of inequality and inequity
Inequality
Inequalities in health, formally defined, refer to a broad range of differences in both health experience and health status between countries, regions, and socioeconomic groups. Most inequalities are not biologically inevitable but reflect population differences in circumstances and behaviour that are in the broadest sense socially determined. However, in industrialised countries such as the United Kingdom, the term “inequalities in health” has tended to refer to differences in health status between regions and population subgroups that are regarded as inequitable.
Inequity
Health inequities, formally defined, are avoidable inequalities that are unfair and unjust. In reality, however, the term is mainly applied to unfair and unjust differences in access to health services between regions and population subgroups within a country. In developing countries, inequities in access have been the dominant preoccupation of those working on health inequalities and inequities.
There are exceptions to this. For example, in the United States, concern about equity of access to adequate health care runs alongside an active research base on the determinants of inequalities in incidence of disease. Nevertheless, in many high income countries, as in western Europe, access to health services is relatively universal and not strongly dependent on socioeconomic circumstances or geography. In developing countries, however, the issue of organising and funding the health sector has been more central to inequalities in health. This has partly been a response to the pressure from international financial institutions to reduce government expenditure on health and to reorganise the health sector. Many people have seen the pressure as a major threat to equity.11
Focusing on equity of provision of health care in the developing world therefore has a compelling logic. Nevertheless, the forces producing inequalities in health status in developing countries need to be given more attention than they are at present. By the same token, the issue of access to health services must receive more attention in developed countries. Much healthcare reform the world over has been driven by a set of technocratic principles that emphasise efficiency and effectiveness and give little consideration to equity.12
Measuring inequalities in health status
From an international perspective, there are problems in making valid comparisons of inequalities in health between socioeconomic groups defined in various ways, including occupational social class or educational level.13 Despite these difficulties, research has established real international variations in the magnitude of socioeconomic differences in health status and mortality for specific diseases. This shows that socioeconomic variation is not a fixed and inevitable feature of society.14
Despite the achievements of the large body of research based on analysis of social groups, it has recently been proposed that this approach should be abandoned.15 Gakidou et al advocate that, rather than looking at the way in which health or disease rates vary between socioeconomic groups, we should measure the distribution of health across all individuals in a population.16 This approach is analogous to measuring inequality in income and would estimate the spread of health (at an individual or household level) across the population.
Although superficially attractive, this approach has major limitations.17 Health is not like income. It is not possible to assign to each individual in a population an objective “health” index akin to their income. Aside from such technical issues, there is also a fundamental point of principle. The approach would effectively remove from the picture the reality that health is socially patterned. Although measures of the distribution of individual health status have a role, they cannot provide insight into the social and biological mechanisms that shape the distribution of health within populations, or what specific interventions are needed to make them more equitable.
Conceptual and methodological difficulties in the measurement of inequalities in health are compounded by the problem that only high income countries have the necessary infrastructure to collect the relevant routine data. Even in countries where basic demographic data on population and mortality and health are collected, they often do not exist in a form that allows the distribution of health status within countries to be estimated. However, there are encouraging signs that some progress is being made. Data from sample surveys carried out by the World Bank in a large number of developing countries were recently used for the first time to make comparable estimates of socioeconomic differences in self reported health.18
Aetiological understandings
Our understanding of the aetiological mechanisms that drive socioeconomic differences in health varies according to disease and context. Some of the links between absolute poverty and ill health are well understood. For example, poor housing, sanitation, and hygiene can lead to increased exposure to communicable diseases, and malnourishment reduces resistance to infection. However, even among those living in absolute poverty, there seem to be differences in the extent to which parents are able to use their scant resources to influence their children's morbidity and mortality.19 This underlines the need to develop people's capacities and resourcefulness within broader strategies to reduce the effects of absolute deprivation on health.
Understanding inequalities in the occurrence of non-communicable diseases such as cancer and heart disease has been more challenging. Although contemporary socioeconomic differences in mortality from lung cancer are explained by historical differences in tobacco smoking, explanations of socioeconomic gradients for other non-communicable diseases such as cardiovascular disease have been more problematic. Various competing theories have been developed. One important area of debate concerns how far socioeconomic gradients in health are due to deprivation generating a “general susceptibility” to a wide range of diseases. The contrasting view is that specific explanations are required for the socioeconomic gradients of each individual disease.
General susceptibility has also been used to explain the hypothesised direct association between income inequality and mortality in high income countries.20 Inequality in income and its correlates (such as level of social capital and cohesion) are thought to generate a range of ill health and disease, partly through a psychosocial stress mechanism. This hypothesis has been challenged,21 not least because it effectively denies the observed heterogeneity of socioeconomic gradients and the existence of distinct (even if overlapping) aetiologies for specific diseases.
Recently, interest has been increasing in the role of influences that operate throughout life.22 The imprints of these influences will not all be equally visible in adulthood and hence may be overlooked by studies that have information about individuals only in middle and old age. The lifecourse approach emphasises the aetiological specificity of different conditions23 and throws light not only on inequalities within countries but also on those between countries.24
The emphasis on factors operating across the lifecourse highlights a neglected question that has potentially major policy implications. Little thought has been given to considering the timescale over which changes in the circumstances of different socioeconomic groups could translate into differences in health status. If there are substantial lag periods between exposure and onset of disease, as seems to be the case for many non-communicable diseases, policy induced changes in conditions today may take years or even decades to produce reductions in inequalities in health. This, however, is not a counsel of despair; it should motivate clearer thinking about the timescales over which policies can be realistically expected to yield benefits and thus lead to effective strategies that are better insulated from the short term pressures to which politicians and policy makers are subject.
Conclusions
The issues we have highlighted reflect the complexity of the scientific, conceptual, and policy issues inherent in addressing the issues of poverty, inequality, and health. The way that the problem is perceived, the priority given to it, and the solutions advanced vary widely according to ideology, country, and region. To be effective, action must be rooted in better understanding of the full scope of current knowledge.
Figure.
Life expectancy at birth in 1999 by per capita total health expenditure in 1997 in 70 countries for which the world health report indicated that data on life expectancy and expenditure were reliable10
Footnotes
Funding: None
Competing interests : None declared.
References
- 1.Acheson D. Report of independent inquiry into inequalities in health. London: Stationery Office; 1998. [Google Scholar]
- 2.Whitehead M, Evans T, Diderichsen F, Bhuiya A, eds. Challenging inequities in health: from ethics to action. New York: Oxford University Press, (in press).
- 3.Leon DA, Walt G, editors. Poverty, inequality and health: an international perspective. Oxford: Oxford University Press; 2000. [Google Scholar]
- 4.Special issue on inequalities in health. Bull World Health Org. 2000;78:1–152. [Google Scholar]
- 5.Smith GD, Neaton JD, Wentworth D, Stamler R, Stamler J. Socioeconomic differentials in mortality risk among men screened for the multiple risk factor intervention trial: I. White men. Am J Public Health. 1996;86:486–496. doi: 10.2105/ajph.86.4.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. World health report 1999. Making a difference. Geneva: WHO; 1999. p. 7. [Google Scholar]
- 7.Ruger JP, Jamison DT, Bloom DE. Health and the economy. In: Merson M, Black R, Mills A, editors. International public health. Gaithersburg: Aspen; 2001. pp. 617–666. [Google Scholar]
- 8.Sen A. Development as freedom. Oxford: Oxford University Press; 2001. [Google Scholar]
- 9.Sen A. Economic progress and health. In: Leon DA, Walt G, editors. Poverty, inequality and health: an international perspective. Oxford: Oxford University Press; 2000. pp. 333–345. [Google Scholar]
- 10.World Health Organization. World health report 2000. Geneva: WHO; 2000. [Google Scholar]
- 11.Stott R. The World Bank. BMJ. 1999;318:822–823. doi: 10.1136/bmj.318.7187.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilson L. In defence and pursuit of equity. Soc Sci Med. 1999;47:1891–1896. doi: 10.1016/s0277-9536(98)00217-2. [DOI] [PubMed] [Google Scholar]
- 13.Kunst AE, Groenhof F, Borgan JK, Costa G, Desplanques G, Faggiano F, et al. Socio-economic inequalities in mortality. Methodological problems illustrated with three examples from Europe. Rev Epidemiol Sante Publique. 1998;46:467–479. [PubMed] [Google Scholar]
- 14.Kunst AE, Groenhof F, Andersen O, Borgan JK, Costa G, Desplanques G, et al. Occupational class and ischemic heart disease mortality in the United States and 11 European countries. Am J Public Health. 1999;89:47–53. doi: 10.2105/ajph.89.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray CJ, Gakidou EE, Frenk J. Health inequalities and social group differences: what should we measure? Bull World Health Org. 1999;77:537–543. [PMC free article] [PubMed] [Google Scholar]
- 16.Gakidou EE, Murray CJ, Frenk J. Defining and measuring health inequality: an approach based on the distribution of health expectancy. Bull World Health Org. 2000;78:42–54. [PMC free article] [PubMed] [Google Scholar]
- 17.Braveman P, Krieger N, Lynch J. Health inequalities and social inequalities in health. Bull World Health Org. 2000;78:232–234. [PMC free article] [PubMed] [Google Scholar]
- 18.Gwatkin DR. Health inequalities and the health of the poor: what do we know? What can we do? Bull World Health Org. 2000;78:3–18. [PMC free article] [PubMed] [Google Scholar]
- 19.Lanata CF. Children's health in developing countries: issues of coping, child neglect and marginalization. In: Leon DA, Walt G, editors. Poverty, inequality and health: an international perspective. Oxford: Oxford University Press; 2000. pp. 137–158. [Google Scholar]
- 20.Wilkinson RG. Unhealthy societies: the afflictions of inequality. London: Routledge; 1996. [Google Scholar]
- 21.Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuh D, Ben-Shlomo Y. A life course approach to chronic disease epidemiology. Oxford: Oxford University Press; 1997. [PubMed] [Google Scholar]
- 23.Davey Smith G, Gunnell DJ, Ben-Shlomo Y. Lifecourse approaches to socio-economic differentials in case-specific adult mortality. In: Leon DA, Walt G, editors. Poverty, inequality and health: an international perspective. Oxford: Oxford University Press; 2000. pp. 88–124. [Google Scholar]
- 24.Leon DA. Common threads: underlying components of inequalities in mortality between and within countries. In: Leon DA, Walt G, editors. Poverty, inequality and health: an international perspective. Oxford: Oxford University Press; 2000. pp. 58–87. [Google Scholar]