ABSTRACT
Active service members and Veterans with a combat-related traumatic brain injury (TBI) are four times more likely to attempt suicide than those without a TBI. TBIs are the signature injuries of the Post-9/11 conflicts and Combat Veterans (i.e., current and former service members who deployed in support of a combat mission) with these injuries are entitled to receive the Purple Heart medal. However, potentially tens of thousands of Combat Veterans did not receive, or were denied the Purple Heart during the first decade of the Global War on Terrorism because a TBI was not documented during the deployment. To our knowledge, this is the first study to explore the meaning of the Purple Heart and examine the impact of the Purple Heart on Army Combat Veterans with a combat-related TBI. Findings from this mixed methods study revealed that not receiving the Purple Heart is associated with increased suicide risk and lower quality of life after a brain injury. Additionally, thwarted belongingness, perceived burdensomeness, and perceived military institutional betrayal are associated with increased suicide risk in Army Combat Veterans with a TBI. This mixed methods study provides important insights into how Army culture is perceived and the power of the Purple Heart among this high-risk group of Combat Veterans.
KEYWORDS: Suicide risk, military, veteran, Purple Heart, traumatic brain injury, Post-9/11, Interpersonal theory of suicide, global war on terrorism, deployment
What is the public significance of this article?—This article discusses what the Purple Heart means to Post-9/11 Army Combat Veterans with a combat-related traumatic brain injury (TBI) and identifies that Army Combat Veterans who did not receive a Purple Heart for their combat-related TBI are at higher risk for suicide.
Background
High rates of suicide (29.0 per 100,000) are seen among Post-9/11 Combat Veterans (i.e., current and former service members who deployed in support of a combat mission) (Bullman et al., 2018). Among the various military branches, Army and Marine Combat Veterans have the highest rates of suicide at 30.3 per 100,000 (Bullman et al., 2018). This higher rate of suicide corresponds with these two branches that deployed the greatest number of ground troops to the Middle East in support of the Global War on Terrorism (GWOT) (Military Health System, 2020).
Traumatic brain injuries (TBI) are the signature injuries of the GWOT and are uniquely invisible relative to other combat injuries. Estimates suggest that more than 400,000 Post-9/11 Combat Veterans sustained a TBI (Military Health System, 2020). The symptoms of TBI have wide-ranging physical and psychological effects including physical, sensory, mood, cognitive, and behavioral symptoms (Brenner et al., 2009) that can persist for years after the injury occurred (Cernak, 2017). In addition to these symptoms, Combat Veterans with a deployment-related TBI are four-times more likely to attempt suicide than those without a TBI (Fonda et al., 2017). These high suicide rates persist, despite targeted suicide prevention efforts by the Veterans Administration (VA) and Department of Defense (DoD) over the last ten years (Veterans Suicide Prevention, 2019).
Suicide has a far-reaching impact, both emotionally and financially; on families, friends, fellow service members, and society (Cerel et al., 2015). It is devastating for families to welcome their Soldier home from combat, only to lose them to suicide (Giacomo, 2019). Consequently, suicide risk transfers to the family and friends because people who experience the loss of a loved one by suicide are more likely to contemplate suicide themselves (Cerel et al., 2015).
The Interpersonal Theory of Suicide was developed to help explain why people contemplate suicide, as well as how they develop the capability to do so. The components of the theory are thwarted belongingness, perceived burdensomeness, and the acquired capability for suicide (Joiner, 2005). Thwarted belongingness refers to feeling socially disconnected from other people and perceived burdensomeness is the feeling of being a burden or liability on others, to the point an individual believes their loved ones would be better off without them. According to the Interpersonal Theory of Suicide, thwarted belongingness and perceived burdensomeness contribute to suicidal ideation and require the capability to make a lethal attempt at suicide. The acquired capability for suicide develops when an individual has a lower threshold for pain or no longer fears death. This can occur as a result of experiencing violence, multiple painful events, or being involved in experiences that could have been fatal (Joiner, 2005), such as experiencing a blast-related TBI.
Research utilizing the Interpersonal Theory of Suicide among Combat Veterans
Military studies using the Interpersonal Theory of Suicide as a guiding framework show that Post-9/11 Combat Veterans have risk factors for suicide that are unique to their combat experiences (Martin et al., 2020). Thwarted belongingness (TB) directly correlates with combat experiences and is impacted by interpersonal experiences during and after combat deployments (Bryan et al., 2013a, 2013b; Martin et al., 2020). For example, Soldiers who experienced a transgression or betrayal while deployed had higher levels of TB, especially when they perceived having low levels of post-deployment support (Houtsma et al., 2017). Specific experiences in combat, such as killing an enemy, witnessing the injury or death of a fellow Soldier and/or enemy, or being wounded in combat, have been explored. The research shows that such experiences are strongly correlated with thwarted belongingness (not perceived burdensomeness) in Army service members (Butterworth et al., 2017).
Investigative efforts thus far provide important insights regarding relationships between combat experience and suicide. However, a recent integrative review of the literature (Moceri-Brooks et al., 2023) identified only nine published studies that were grounded in the Interpersonal Theory of Suicide (as measured by the Interpersonal Needs Questionnaire) to understand suicide risk exclusively among Combat Veterans (Allan et al., 2019; Bryan & Anestis, 2011; Bryan & Cukrowicz, 2011; Bryan et al., 2010, 2012; Butterworth et al., 2017; Houtsma et al., 2017; Martin et al., 2017, 2020). The limited number of studies using the Interpersonal Theory of Suicide to understand suicidal thoughts and behaviors within this high-risk group demonstrates that researchers have only just begun to explain why Army Combat Veterans think about or attempt suicide.
Extending the Interpersonal Theory of Suicide to Combat Veterans with a TBI
Some of the more prominent risk factors of suicide within the military, such as having a TBI (Fonda et al., 2017), have not been directly studied using the Interpersonal Theory of Suicide. Although some of the studies using the Interpersonal Theory of Suicide framework included participants with a self-reported combat-related TBI, there was no discussion of the Interpersonal Theory of Suicide in relation to the injury (Bryan & Anestis, 2011; Bryan et al., 2012). Thus, it is unclear what role, if any, TBIs played in the study findings (Bryan & Anestis, 2011; Bryan et al., 2012).
Regarding interpersonal experiences in combat, it is unclear how Combat Veterans experienced transgressions or betrayal while deployed (Houtsma et al., 2017; Martin et al., 2017). It is unknown whether any of these experiences were connected to events surrounding a brain injury, for example. Further, it unknown whether thwarted belongingness, perceived burdensomeness, and perceived post-deployment support levels were associated with the experience of having a TBI (such as how the injury occurred, recognition of the injury, and receiving care for the injury). These questions need to be explored to have a greater understanding of suicidal thoughts and behaviors in Combat Veterans with a TBI.
Toward a better understanding of military commendation and suicide risk
The Purple Heart is the only military medal to recognize a combat injury and is awarded during or after deployments. Service members with a TBI caused by enemy fire are eligible for the Purple Heart medal (Army Human Resources Command [AHRC], 2019). However, during the first decade of the GWOT (2001–2011), potentially tens of thousands of Post-9/11 Combat Veterans sustained a mTBI and returned to the fight without a medical evaluation of their injury (Miller & Zwerdling, 2010; Tanielian & Jaycox, 2008; Zwerdling & Miller, 2010). This occurred because universal screenings for TBIs were not in place until after 2007 (Tanielian & Jaycox, 2008) and the DoD directive for the management of mTBIs/concussions in the deployed setting was not implemented until 2012 (Department of Defense, 2012). Thus, blast-related concussive injuries, which accounted for over 80% of TBIs were overlooked, under-appreciated, and/or not documented (Tanielian & Jaycox, 2008; Zwerdling & Miller, 2010). Consequently, many service members received TBI diagnoses long after they returned home and were then denied the Purple Heart by the military because their injuries were either not documented during the deployment, or medical documents were lost or destroyed (ProPublica, 2012; personal communication, 2021).
espite the importance given to commendation in the military culture (Army Human Resources Command, 2019), very little is known about how military awards, recognitions, and promotions impact Army Combat Veterans, especially in the context of suicide. One study described the impact of the Purple Heart medal on Veterans, though it did not describe the relationship to suicide. This large-scale study (n = 10,255) examined mortality rates (from all causes) among Veterans who served in World War II and the Korean War (Kimbrell et al., 2011). Researchers compared the mortality rates between Veterans with and without PTSD who did, and did not, receive the Purple Heart medal. Veterans who received the Purple Heart medal (with and without PTSD) had a 50% lower mortality rate than Veterans who did not receive the medal (Kimbrell et al., 2011). This landmark study reveals that the Purple Heart medal may be a relevant variable to explore with Post-9/11 Combat Veterans.
Our study aims were as follows: 1) to determine the values, beliefs, and meaning of the Purple Heart medal among Post-9/11 U.S. Army Combat Veterans with a combat-related TBI, and 2) determine if there are differences in suicide risk (i.e., suicidal thoughts and behaviors) among Combat Veterans with a TBI who did, versus did not, receive a Purple Heart medal for their combat-related brain injury. Secondary aims of the study were to explore associations between the Purple Heart medal and the interpersonal constructs of the Interpersonal Theory of Suicide (thwarted belongingness and perceived burdensomeness), perceived military institutional betrayal, and quality of life after brain injury. We hypothesized that not receiving a Purple Heart for a combat-related TBI is associated with increased suicide risk. Findings from this study may provide insight as to why Army Combat Veterans with a TBI have higher suicide rates.
Method
Study design
This study used a convergent parallel mixed methods design to examine suicide risk among Post-9/11 Army Combat Veterans with a TBI, in context of military culture. The quantitative strand used a survey design, and the qualitative strand was employed as a focused ethnographic study. This qualitative approach was chosen because it is context-specific and can explain previously unknown phenomena within cultures and subcultures (Holloway & Galvin, 2017). Quantitative and qualitative data were collected concurrently and independently, and then merged to determine convergence or divergence of data. Given the fact that we believed we were introducing a new variable (Purple Heart) into the suicide literature, interview data was necessary to enhance our understanding of the survey findings.
Recruitment of study participants
Post-9/11 U.S. Army Combat Veterans with a suspected or confirmed combat-related TBI (being in or near a blast while deployed) were eligible to participate in the study. After receiving institutional review board approval, study participants were recruited from several Army installations and Veteran organizations (with the help of gatekeepers), and the snowball method through text messages, e-mails, and word of mouth across the United States and the globe. Participants in the qualitative strand contacted the primary investigator directly to set up an interview and then provided digital consent, completed a brief demographic survey online, and were interviewed via a secure web conference software. Combat Veterans interested in the anonymous study survey were directed to the study consent form (through a QR code or URL) to read and sign before accessing the survey. At the end of the survey, participants were automatically directed to a separate URL where they were presented with the option to enter their e-mail address to receive a $20 gift card via e-mail. The confidentiality of the survey participants was safeguarded through use of the separate URL to ensure their e-mail address, if they chose to provide it, was not connected to their survey. Further, all consent forms were securely stored separate from the databases and subject ID numbers were used in place of names of the participants who agreed to be interviewed.
Measures
Qualitative strand
Participants were interviewed using a semi-structured interview guide that was based upon Leininger’s Sunrise Model (Leininger & McFarland, 2006). This enabler guide provided a comprehensive view of the dimensions of culture, such as values and beliefs, social factors, and biological factors (Leininger & McFarland, 2006). All participants were asked to describe Army values, Army culture, the meaning of the Purple Heart, and beliefs about the medal. They also gave a detailed description of the combat event that caused their TBI, along with their experiences after the injury occurred. Saturation of the data was reached after fifteen interviews and two additional confirmatory interviews were conducted.
Quantitative strand
Thwarted belongingness and perceived burdensomeness
The Interpersonal Needs Questionnaire (INQ-15) (Van Orden et al., 2012) includes nine questions to measure thwarted belongingness (TB) and six questions to assess perceived burdensomeness (PB). Participants rate statements from 1 (not at all true for me) to 7 (very true for me). Scale scores are item sums; higher values indicate increased levels of TB (range 9–63) and PB (range 6–42). Higher TB and PB scores were associated with suicidal ideation in military samples (Anestis et al., 2015; Gutierrez et al., 2016). Internal consistency reliabilities in the present sample were α = 0.90 for TB and α = 0.96 for PB.
Institutional betrayal
The Institutional Betrayal Questionnaire-Health (IBQ-H) consists of 12 items used to identify if individuals feel, or have felt betrayed by healthcare institutions (Smith, 2017). For this study, the words “healthcare institution” were replaced with the words “military institution.” Respondents were asked to think about their experiences within the military institution related to their TBI and then for each item, indicated whether they believed the military institution (which included military units, clinics, and individuals) played a role. Items included experiences surrounding omission of care and the environment, such as “denying your experience in some way, making it difficult to share concerns, and create an environment where continuing to seek care was difficult for you” (Smith, 2017). Respondents could endorse between 0–12 items with higher scores reflecting a greater number of perceived instances of betrayal by the military institution. This measure demonstrated strong convergent and discriminant validity in two different samples of female Veterans (Monteith et al., 2021), however, the IBQ2 has not been psychometrically tested in male Combat Veterans. The internal consistency for IBQ2 in this study was α = 0.88.
Suicide risk
The Suicide Behavior Questionnaire-Revised (SBQ-R) is a 4-item tool that is used to measure suicide risk. It consists of four questions asking about the following: (1) lifetime suicide ideation and/or attempt, (2) frequency of suicidal ideation over the past 12 months, (3) threat of suicide attempt, and (4) self-reported likelihood of a future suicide attempt (Gutierrez et al., 2016). This instrument has been used to distinguish suicidal and non-suicidal individuals in civilian samples (Osman et al., 2001). Each item on the SBQ-R is rated on a five or six-point Likert scale with answers ranging from “never” to “very often/likely.” Scores range from 3–18, with higher scores indicating suicide risk level. The internal consistency of the instrument was stronger in the current sample of Army Combat Veterans (α = 0.84), when compared to a similar sample of Combat Veterans (α = 0.78; Bryan et al., 2013).
Quality of life after brain injury
The six-item Quality of Life After Brain Injury Scale (QOLIBRIS) measures the satisfaction level of an individual’s life since the brain injury occurred, with specific questions related to how satisfied they are with their memory (von Steinbüchel et al., 2010). Responses range from “not at all” to “very much” on a five-point Likert scale. Total scores range from 6–30, with higher scores revealing a higher (more positive) quality of life. Initial psychometric testing of this instrument demonstrated an internal consistency of α = 0.75 to 0.89 and test-retest reliability of α =0.78 to 0.85 in a cross-cultural civilian study (von Steinbüchel et al., 2010). To our knowledge, no psychometric testing of this instrument with a military population has been published. The internal consistency of the QOLIBRI scale in this study was α =0.91.
Data analysis
Qualitative data analysis
Leininger’s four phases of qualitative data analysis were used (Leininger & McFarland, 2006) to determine the values, beliefs, and meaning of the Purple Heart medal among Post-9/11 Army Veterans with a combat-related TBI. During phase one, the primary investigator (PI) reviewed transcribed interviews and field notes. In phase two, the PI coded and categorized the data using NVivo12 (computer assisted qualitative data analysis software). Phase three focused on identifying patterns from observations, interviews, and demographic questions. Finally, the PI and co-PI identified themes and highlighted findings (Leininger & McFarland, 2006). Although there are four phases to analyzing qualitative data, the collection and analysis occurred concurrently. Data collection ceased when no new themes were identified (i.e., data saturation occurred). The PI maintained an audit trail to indicate what and why decisions were made throughout the study. Once the qualitative data analysis was complete, the quantitative data was analyzed. This order of analysis is important to reduce the chance for bias during the qualitative analysis (Creswell & Plano Clark, 2018).
Quantitative data analysis
The quantitative data was analyzed using SPSS 28 and Jamovi 2.3.3. Data distributions were examined, and the data was transformed when appropriate. Means and standard deviations were used to describe continuous variables and proportions were used to describe categorical variables. Spearman’s Rho correlations were used to establish associations between the variables of interest (see Table 2). Generalized linear models were constructed with suicide behavior scores as the outcome variable and a maximum of five predictor variables (in keeping with our G-power analysis; Faul et al., 2009). For the exploratory analysis, traditional bivariate and multiple regression models were constructed with quality of life after a brain injury (QOLIBRI) as the outcome variable. Variables were entered into the regression model stepwise (or block type) to capitalize on chance and overfit the data (Schreiber, in press; Tabachnick & Fidel, 2001). Multicollinearity of variables was evaluated with variance inflation factor (VIF), autocorrelation was evaluated using Durbin-Watson, and residuals were examined with Mahalanobis distance and Center Leverage values, along with standardized residual plots (e.g., heteroscedasticity) (Schreiber, in press; Tabachnick & Fidel, 2001). The distribution of residuals was examined for normality and post-hoc analyses with a Bonferroni correction was used to confirm the significance of the findings.
Table 2.
Correlations among study variables and descriptive statistics.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| (1) TB | – | ||||
| (2) PB | 0.55*** | – | |||
| (3) Institutional Betrayal | 0.33* | 0.05 | – | ||
| (4) QOLIBRI | 0.56*** | 0.14 | 0.38** | – | |
| (5) Suicide Risk | 0.57*** | 0.54*** | 0.33** | −0.27* | – |
| Mean | 29.5 | 14.0 | 3.90 | 17.6 | 7.55 |
| SD | 12.9 | 8.66 | 3.60 | 5.79 | 4.05 |
| Minimum | 9.0 | 6.0 | 0 | 6.00 | 4.00 |
| Maximum | 56.0 | 38.0 | 12.0 | 29.0 | 18.00 |
| n | 57 | 57 | 60 | 60 | 60 |
*p < .05, **p < .01, ***p < .001, TB = thwarted belongingness, PB = perceived burdensomeness, QOLIBRI = quality of life after brain injury.
Results
Study participants
Interviews were conducted with 17 U.S. Army Combat Veterans and the survey was completed by 62 U.S. Army Combat Veterans. Due to the anonymity of the survey, it is not known how many qualitative participants also completed a survey. Combat Veteran characteristics for each strand are described in Table 1. Both strands of the study had similar demographics. The typical study participant was an active-duty, college educated, 40-year-old, married male. Although the military rank of the study participants varied, the majority were noncommissioned officers (E5-E9) with 14 years of service. Of interest, officers were more represented in both strands of this study than other Post-9/11 Combat Veteran studies (Bryan et al., 2012, 2013). Participants endorsed an average of two combat-related deployments and over two-thirds of the participants in each study strand did not receive the Purple Heart medal for their combat-related TBI(s). One-quarter of the survey sample applied for and were denied the Purple Heart for their combat-related TBI.
Table 1.
Sociodemographic characteristics of participants.
| Quantitative n = 62 |
Qualitative n = 17 |
|
|---|---|---|
| Military component | ||
| U.S. Army active duty U.S. Army Reserve U.S. Army National Guard |
84.7% (n = 53) 5.1% (n = 3) 10.2% (n = 6) |
88.2% (n = 15) 5.9% (n = 1) 5.9% (n = 1) |
| Military rank at time of the survey/interview | ||
| E1-E4 E5-E9 CW1-CW5 O1-O4 O5-O9 |
14.5% (n = 9) 55% (n = 34) 6.4% (n = 4) 16.1% (n = 10) 8% (n = 5) |
11.8% (n = 2) 47.1% (n = 8) - 29.4% (n =5) 11.8% (n = 2) |
| Age | ||
| Mean (SD) | 40.71(7.68) | 40.76(5.69) |
| Sex | ||
| Female Male |
1.7% (n = 1) 98.3% (n = 61) |
5.9% (n = 1) 94.1% (n = 16) |
| Race/Ethnicity | ||
| American Indian or Alaska Native Asian Black or African American Hispanic or Latino White/Caucasian Other |
3.3% (n = 2) 1.7% (n = 1) 16.7% (n = 11) 6.7% (n = 4) 70% (n = 43) 1.7% (n = 1) |
5.9% (n = 1) - 5.9% (n = 1) 5.9% (n = 1) 76.5% (n = 13) 5.9% (n = 1) |
| Relationship status | ||
| Married Divorced Separated Single/never married Partnered and/or engaged |
76.3% (n = 47) 8.5% (n = 6) 6.8% (n = 4) 6.8% (n = 4) 1.7% (n = 1) |
82.4% (n = 14) 11.8% (n = 2) - - 5.9% (n = 1) |
| Children (that depended on them) | ||
| Yes No |
22.4% (n = 14) 77.6% (n = 48) |
- - |
| Education | ||
| High school degree or equivalent (e.g., GED) Some college, but no degree Diploma or Technical Certification Associate degree Bachelor’s degree Master’s degree Doctorate |
3.3% (n = 2) 26.7% (n = 17) 5.0% (n = 3) 16.7% (n = 10) 20.0% (n = 12) 23.3% (n = 14) 5.0% (n = 3) |
- 5.9% (n = 1) - 11.8% (n = 2) 47.1% (n = 8) 35.3% (n = 6) - |
| Number of deployments | ||
| Mean (SD) | 2.89(1.63) | 2.35(1.28) |
| Number of blast exposures (i.e., TBI) | ||
| Mean (SD) | 5.58(3.84) | - |
| Purple Heart status | ||
| No Yes |
75.8% (n = 47) 24.2% (n = 15) |
64.7% (n = 11) 35.3% (n = 6) |
Qualitative results
The interview data resulted in 28 categories and seven patterns being identified. At the final step of the analyses, three themes emerged based upon the respondents’ perceptions of the Army, Army culture, and the Purple Heart: 1) the Army demands loyalty but does not always reciprocate loyalty, 2) the culture of the Army creates and promotes a sense of ambivalence around the Purple Heart, TBIs, and TBI care, and 3) the lasting power of the Purple Heart in healing.
The Army demands loyalty but does not always reciprocate loyalty
All the participants easily recited the Army value acronym LDRSHIP, with loyalty being the first value represented in the acronym followed by duty, respect, selfless service, honor, integrity, and personal courage. Combat Veterans described the sacrifices made to give their best effort in various jobs throughout their careers, describing the most important principle is to “never let my fellow Soldiers or the Army down,” When asked if the Army reciprocated the loyalty it required, the responses were mostly negative and/or ambiguous, “no, I do not feel the Army is loyal, they have screwed us over.” Participants also described feeling expendable, “If you’re not 100%, you’re zero.”
The Army culture creates and promotes a sense of ambivalence around the Purple Heart, TBIs, and TBI care
Participants had conflicting feelings about the Purple Heart medal. Several of the participants explained that, early in their military careers, the Purple Heart was negatively portrayed. When they entered the Army, they were taught by their immediate chain of command that it was an unfavorable medal, “It’s the award you don’t ever want to receive – because it means you are hurt.”
Participants also described stigma attached to being injured, “If you say I’m hurt, and I got these issues … you’re marked as a quitter.” Often in the same interview, participants would express conflicting feelings about the Purple Heart, “It’s a prestigious award.”
Participants expressed ambiguity surrounding whether they deserved the medal for their TBI. The “S” in the Army values acronym, “selfless service,” means that Soldiers are trained to think of others over themselves and not seek the spotlight. “Soldiers are either told they don’t deserve it by their chain of command or Soldiers refuse the Purple Heart because they think they are taking it from someone who deserves it.” Participants frequently compared their brain injury to others with visible injuries, “Other guys have it a lot worse.”
All participants shared details about their continued suffering from their brain injury that occurred up to 20 years prior to the study interview. Participants described symptoms such as, migraines, short-term memory loss, balance issues, dizziness, and light and noise sensitivity. Participants also described their hesitation seeking care for their brain injury, “I did not see a doctor for my TBI symptoms because it was still the era of ‘ … if you want to get promoted, then you have to be fully qualified and competitive. So, anyone with any mark against them was penalized … at least from 2006–2012.”
The lasting power of the Purple Heart in healing
Once participants talked through their ambiguity surrounding the Purple Heart medal, in keeping with always thinking of others, they were asked to set aside concerns about the stigma and/or their concern for other wounded Soldiers “who have it worse,” to reflect on either what the Purple Heart means to them personally or what it would mean to them. Most of the participants (n = 15) stated that the Purple Heart “validates,” “acknowledges,” or “legitimizes” their invisible injury. “The Purple Heart would provide closure for me.”
All participants stated that they believe that they either received care for their TBI because of receiving the Purple Heart or would have received care for their TBI sooner, or at all if they were given a Purple Heart. “We realize we are hurt when we have a Purple Heart.” “It is nearly impossible to get care for your TBI, you get treated like you are making it up … the Purple Heart was like an advocate for me, it gave me strength to speak up and fight for care – it made me know I could ask for help.”
Quantitative results
Descriptive analyses of the variables revealed non-normal distributions, except for quality of life after brain injury (QOLIBRI). Log transformations slightly improved the distributions of thwarted belongingness and perceived burdensomeness. Spearman’s Rho was used to calculate the following correlations: Thwarted belongingness (TB), perceived burdensomeness (PB), and betrayal were positively correlated with suicide risk. Quality of life after brain injury (QOLIBRI) scores were negatively correlated with suicide risk, TB, and betrayal. TB was positively correlated with PB and perceived military institutional betrayal. As expected, TB and PB were highly intercorrelated (see, Table 2).
The distribution of SBQ-R scores was positively skewed, with a negative binomial distribution. Therefore, a generalized linear model for negative binomial distributions was constructed, with suicide behavior scores as the outcome variable. The quality of life after a brain injury variable (QOLIBRI) was the only normally distributed variable. Multicollinearity of variables were evaluated using VIF, Durbin-Watson, Mahalanobis distance and Center Leverage values, along with standardized residual plots (e.g., heteroscedasticity) (Schreiber, in press; Tabachnick & Fidel, 2001). Listwise deletion removed a total of five cases (n = 57) from each of the regression analyses.
Suicide behaviors: Negative binomial regression
Independent variables were added using a forward step approach to model selection where we first identified the variable with the highest loglikelihood ratio (thwarted belongingness) and then added only the variables that improved model fit up to our pre-determined maximum (according to the loglikelihood ratio, Akaike Information Criterion (AIC), and r-squared values). As each additional variable was added to the model, the AIC decreased from 272.21 to 260.60 and the r-square increased from 0.37 to 0.56.
Initially, significant independent variables in the regression model were thwarted belongingness (TB), perceived burdensomeness (PB), institutional betrayal, and number of blast wave exposures (i.e., TBIs). The model confirmed that TB, PB, and perceived military institutional betrayal were associated with increased suicide risk. The number of blast wave exposures were associated with slightly decreased suicide risk. Purple Heart status was then added to the equation, which further improved model fit (r2 = 0.56) and revealed that not having a Purple Heart was associated with increased suicide risk in the presence of thwarted belongingness, perceived burdensomeness, perceived institutional betrayal, and number of blast waves exposures (i.e., TBIs) (see, Table 3 for details).
Table 3.
Suicide risk: Negative binomial regression coefficients and loglikelihood ratio.
| 95% Exp(B) Confidence Interval |
|||||||
|---|---|---|---|---|---|---|---|
| Independent Variables | Estimate | SE | exp(B) | Lower | Upper | z | |
| (Intercept) | 1.2 | 0.11 | 3.32 | 2.68 | 4.07 | 11.26 | |
| Thwarted Belongingness | 1.3 | 0.49 | 3.67 | 1.43 | 9.73 | 2.68 | |
| Purple Heart Status (Yes) | −0.48 | 0.2 | 0.62 | 0.42 | 0.91 | −2.4 | |
| Perceived Burdensomeness | 1.17 | 0.37 | 3.22 | 1.55 | 6.75 | 3.13 | |
| Institutional Betrayal | 0.07 | 0.02 | 1.08 | 1.03 | 1.13 | 3.08 | |
| Number of Blasts (TBIs) |
|
−0.06 |
0.02 |
0.94 |
0.9 |
0.99 |
−2.47 |
| Model r2 | 0.56 | ||||||
N = 57.
Quality of life after brain injury: Exploratory bivariate and multiple regression
A significant relationship between receiving the Purple Heart and higher quality of life after brain injury (QOLIBRI) scores was revealed (r2=0.11). Next, block wise entering of variables demonstrated that perceived burdensomeness negatively impacted the model (due to multicollinearity), thus it was removed. The final model with Purple Heart status, thwarted belongingness, institutional betrayal, and QOLIBRI was strong, accounting for over 50% of the variance. The traditional multiple regression results indicated that receiving a Purple Heart was associated with higher QOLIBRI scores. Feeling betrayed by the military institution and higher levels of thwarted belongingness were negatively associated with QOLIBRI (see, Table 4 for coefficients). In both the traditional linear and multiple regression analyses, all residuals were under the Cook’s, centered leverage, and Mahalanobis cutoff values and the assumption of homoscedasticity were met.
Table 4.
Quality of life after a TBI: Hierarchical regression.
| Variable | B | SE | t | Stand β | r2 |
|---|---|---|---|---|---|
| Step 1 | 0.11 | ||||
| Intercepta | 16.93 | 0.81 | 20.83 | ||
| Purple Heart Status (Yes) | 4 | 1.58 | 2.53 | 0.73 | |
| Step 2 | 0.52 | ||||
| Intercept a | 34.71 | 3.15 | 11.02 | ||
| Purple Heart Status (Yes) | 2.804 | 1.22 | 2.31 | 0.51 | |
| Thwarted Belongingness | −10.79 | 2.24 | −4.82 | −0.47 | |
| Institutional Betrayal | −0.54 | 0.16 | −3.48 | −0.35 |
N = 57.
Mixed methods data analysis
As a final analytic step, the results from each study strand were compared and an abstracted pictorial model was developed (see Figure 1). The qualitative results provided rich cultural context for the quantitative results deepening our understanding of the associations identified in the quantitative analyses.
Figure 1.
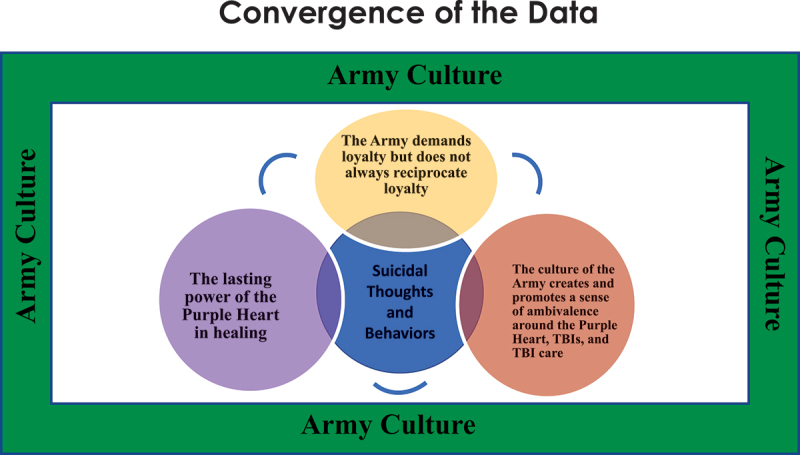
Abstracted pictorial model.
The relationship between Purple Heart status and suicide risk
The relationship between Purple Heart status and increased suicide risk can be explained by the theme, the lasting power of the Purple Heart in healing. Recognition is a significant part of Army culture and is mainly accomplished through awards and medals. Participants explained that awards are given to Soldiers when they complete training, graduate from an Army school, move to another location, make a significant contribution on their job, engage in combat action with the enemy overseas, and for a heroic act. Often, these awards are given during a ceremony with friends and family invited to attend. Frequently the family is involved, with spouses, parents, and/or children pinning the award on their Soldier’s uniform. This ceremony helps families see the importance of their Soldiers contribution and/or provides “closure,” according to interview participants (n = 3). These awards are added to the Soldier’s permanent Army record and are proudly displayed on their Army dress uniforms, with larger racks of awards signifying more years of service and/or greater contributions in service to the nation. According to the study participants, some awards/medals have greater meaning than others. The Purple Heart was frequently described as holding more importance to the participants than other medals or awards.
The participants explained that although Soldiers are trained to think of others over themselves, they are conditioned by Army culture to expect an award/medal based upon merit or entitlement. The Purple Heart has a prominent role among Army Combat Veterans because it is the only way the Army officially acknowledges a combat injury. When combat injuries are invisible and not officially recognized, it creates a personal ambiguity for the Combat Veteran regarding the severity or significance of their injury. This ambiguity prevented some of the participants from seeking and/or receiving care. The participants described that the Purple Heart helps to resolve feelings of ambiguity either because it provides certainty that the TBI symptoms they are experiencing (memory loss, ringing in the ears, light sensitivity, headaches, anger) are real, and/or is a reminder that their sacrifice is important and worthy of care. As a result, the Purple Heart was identified by most of the participants (n = 16) as being a conduit for Combat Veterans to receive medical care and rehabilitation, and “validates” or adds visibility to this uniquely invisible combat injury. Participants who received a Purple Heart described it has being a catalyst for support from family and friends, and the survey findings indicated that receipt of the Purple Heart was associated with higher quality of life scores and lower suicide risk.
Military institutional betrayal and suicide risk
The association between perceived military institutional betrayal and increased suicide risk in Army Combat Veterans connects to the theme describing unreciprocated loyalty. All members of the Army agree to follow the Army LDRSHIP values, as described previously. However, when Army leadership and/or Army medical professionals did not demonstrate or reciprocate these values to Combat Veterans, it was perceived as the institution not fulfilling its obligation, a betrayal. “The Army did not fulfill their obligation to care for us,” “they sweep things under the rug.”
One-quarter of the interview sample (28%, n = 4) described being called a “quitter” by Army leaders when they decided to transition out of the Army. The participants described how it felt to be called “quitters” and how it hurt to have their leaders “turn their backs” on them when they were injured. One participant said, “I got to the point where, you know, I locked and loaded my weapon” with intent to end their life.
Other interview participants described betrayal by Army medical professionals when they did not receive care for their injury, being told “you’re fine,” despite blacking-out when their military vehicle was catastrophically destroyed after rolling over an improvised explosive device, or “flying 10 feet in the air” when a mortar struck nearby. They also described their exhausting battle advocating for their own care after returning home from their combat deployment. They described the frustration in trying to convince physicians within the military institution to appreciate how their TBI symptoms are negatively impacting their life. “They didn’t believe me … ”
Finally, several participants (n = 3) described experiencing institutional betrayal when their leaders would not allow them to receive a Purple Heart, citing their own criteria for the medal such as, “it is given to those who bleed.” Other participants who applied for the Purple Heart once they exited the Army were turned down because they did not have documentation of the injury from a medic or other health care provider while in the operational theater. These participants expressed frustration that the Army’s intra-theater medical documentation requirement does not account for the fact that the TBI management guidance was not in place when their injuries occurred, nor the unique circumstances of the GWOT combat environments. Participants described serving in combat outposts embedded in remote villages far from formal medical care.
Purple Heart denials based solely upon timing or location of the TBI diagnosis was perceived as “perplexing” to these Combat Veterans because they are required to include other corroborating documents in their applications, such as two sworn statements from eyewitnesses of the blast/injury, a combat action award narrative describing the event in which they were injured (signed by senior Army leaders), and proof of their VA disabilities (with ratings as high as 100%) for their combat-related TBI. Study participants believe that the Army makes applying for the Purple Heart difficult “to discourage us [them] from applying.”
Thwarted belongingness and suicide risk
Participants with and without the Purple Heart agreed that “there’s comradery among Purple Heart recipients.” Participants with a Purple Heart said they felt safe “to talk about their injury with other Purple Heart recipients.” Civilians also recognize the Purple Heart as a medal of importance. Private businesses and VA clinics and hospitals have dedicated parking spaces for Purple Heart recipients. “Purple Heart recipient” is often included in formal introductions of Combat Veterans and on employment biographies. Many States have Purple Heart license plates and highways named to honor Purple Heart recipients; the Purple Heart has a place of honor in society. Participants without the Purple Heart described a “sting” when they see the license plates, drive past a parking space, hear the introductions, or watch emotional vignettes on TV about Purple Heart recipients. The Purple Heart is synonymous with combat wounded, so the participants without a Purple Heart wondered where they fit in, “It feels shitty,” “I just hang my head.” They described feeling left out.
Perceived burdensomeness and suicide risk
Interview participants described how being a burden is counter to military culture which explains the relationship between perceived burdensomeness and increased suicide risk. “The last thing you want to do is to be the guy who is not pulling his weight.” Many participants described not wanting to leave their teammates to see a medic after a concussion injury because it would leave the team with one less Soldier on a mission or convoy, possibly placing the team at a greater risk of harm. Yet, participants described how having a brain injury inhibits their ability to “pull their own weight.” “Being a burden on my family made me want to kill myself, I was going to kill myself if I didn’t get better, the symptoms are exhausting, and the guilt and shame are unbearable after angry outbursts.”
The relationship between the Purple Heart status, thwarted belongingness, betrayal, and quality of life after brain injury
The explanation for the variables impacting a Combat Veteran’s quality of life after brain injury is woven throughout the data convergence findings in the previous sections. The qualitative narratives provide clear understanding of how respondents’ assessment of their quality of life after a TBI (overall satisfaction with their physical condition, how their brain is working, their emotions, ability to carry out daily activities, personal and social life, and current situation and future prospects) is negatively impacted by not receiving the Purple Heart, perceived military institutional betrayal, and thwarted belongingness.
Discussion
To our knowledge, this study is the first to describe the values, beliefs, and meaning of the Purple Heart among Post-9/11 Army Combat Veterans and added military commendation as an important new variable in suicide research. Findings from the study confirmed our hypothesis that not receiving a Purple Heart for a combat-related TBI is associated with increased suicide risk among Army Combat Veterans. Further, the Purple Heart variable strengthened the model of known suicide risk factors (thwarted belongingness and betrayal) (Martin et al., 2017). Our exploratory analyses also found that Purple Heart status is positively associated with quality of life after brain injury. The convergence of the two strands of scholarly inquiry provide insights as to why Army Combat Veterans with a TBI have unique suicide risks. Data from this study are congruent with other Combat Veteran studies that identified associations between thwarted belongingness, betrayal, and suicidal thoughts and behaviors (Allan et al., 2019; Bryan & Anestis, 2011). The present study also confirms the lone study grounded in the Interpersonal Theory of Suicide that found that perceived burdensomeness levels are associated with suicidality in Combat Veterans (Bryan et al., 2012).
Moreover, Post-9/11 Army Combat Veterans with a TBI in this study endorsed higher mean SBQ-R scores than other military samples (Anestis & Bryan, 2013). This highlights the importance of focusing inquiry on homogeneous military samples (i.e., Army Combat Veterans with a TBI), to identify potential suicide prevention interventions that meet the cultural needs unique to each military branch. Future studies grounded in the Interpersonal Theory of Suicide should build upon the current study by asking questions specific to Army Combat Veterans and the experience of having a TBI. Such exploration will enhance our understanding of why this population continues to be high risk for suicide. Studies should also investigate why there may be a slightly negative association between number of blast exposures and suicidal behavior scores. It is possible that surviving multiple life-threatening experiences enhances a Combat Veteran’s sense of purpose in life or desire to live.
This study also confirms that TBIs have long-lasting physical and psychological impacts. The Committee on Accelerating Progress in Traumatic Brain Injury Research and Care indicates that TBIs do “not have a place to reside” in the U.S health care system and TBIs should not be viewed as a one-time event, but rather managed as a condition (National Academies of Sciences and Medicine, 2022). Healthcare providers “need a comprehensive set of ‘bio-psycho-socio-ecological’ lenses to truly see a TBI in all its dimensions, and care and concern over time – not just in terms of a bounded episode” (National Academies of Sciences and Medicine, 2022, p. xii). It is clear from our study that a holistic approach must be taken to identify or diagnose the TBI, educate Combat Veterans and their families about TBIs and their effects, and offer rehabilitation. Consider the relief any patient feels when they find out that their invisible symptoms have a name, it is validating. Once someone is diagnosed, a care plan is created, and they can take steps to heal or adjust to a new normal. When TBIs are not diagnosed, patients and families can struggle, attaching their own names to the symptoms, “I thought I was just a crazy person” (personal communication, 2022). One study participant explained, “The Veteran has to figure out how to cope with a brain injury and if they cannot cope, they commit suicide.” Recognition and care for these invisible injuries may be lifesaving.
Clinical and policy implications
Study findings revealed two concrete ways to assist Army Combat Veterans at high risk for suicide. First, all Combat Veterans with a history of being in or near a blast need to be systematically identified and offered a comprehensive TBI evaluation (biological, physical, social, and ecological). The literature provides strong evidence that blast-waves cause concussion injuries, so health care providers can make confident diagnoses in the post-deployment period (Cernak, 2017). A comprehensive evaluation of the Combat Veteran’s symptoms may help to convince the Soldier, their family, and health care providers that the TBI symptoms are real and deserving of treatment. Further, a TBI diagnosis may relieve some of the burden associated with living with a TBI because a diagnosis may prompt health care providers to educate the Combat Veteran and their family members about their injury and offer continuous follow-up care to address their potential long-term care needs.
Second, all Army Combat Veterans who have a combat-related TBI must be given a Purple Heart to officially recognize their combat injury and sacrifice. According to Army Human Resources command, “the Purple Heart differs from all other decorations in that an individual is not ‘recommended’ for the decoration; rather he or she is entitled to it upon meeting specific criteria” (Army Human Resources Command, 2019).
We considered several explanations for why Combat Veterans in this study did not receive Purple Heart medals, including having sufficient self-efficacy. As described by the study participants, subjective decision-making by Army leaders and the updated policy requiring medical documentation from the deployment (Army Human Resources Command, 2019) makes it difficult for many Combat Veterans to receive the Purple Heart. So, self-efficacy, for example, cannot get around policy. Thus, the current Purple Heart policy should be reviewed for potential changes.
Limitations
There are several limitations to note. First, Covid-19 restrictions on Army posts and the Ukraine crisis negatively impacted study recruitment efforts. For example, typical recruitment opportunities, such as unit formations, in-person meetings, and social gatherings were not available because they were either limited to service members or canceled due to the Covid-19 pandemic. The Ukraine crisis caused unexpected overseas troop mobilizations which also hindered recruitment efforts. Second, in line with other military suicide studies, women and people of color are under-represented in this study, despite efforts to recruit a diverse sample utilizing a diverse group of gatekeepers. There was specific hesitation among women and service members of color to participate, thus readers must take caution in generalizing the study findings to these populations and future studies must find ways to include them. The authors surmise that in-person recruitment and relationship building would help to gain trust within these populations. Third, the sample size was small, which is not ideal for regression analyses, however, the sample size met the power requirement for the analyses (Faul et al., 2009). Replication in larger samples would be beneficial to increase the confidence in the generalizability of the quantitative results. Fourth, the psychological co-morbidities of participants were not identified, so we were not able to control for those potential confounders. Finally, the study relied upon self-reported data (e.g., number of combat-related blast exposures) and was cross-sectional, which only captures the respondents’ perspectives at one point in time.
Conclusion
This study highlights the importance of examining suicide risk in Army Combat Veterans with a TBI and adds Purple Heart status as an important variable to consider in Combat Veteran studies. This study also described the values, beliefs, and meaning of the Purple Heart medal among Post-9/11 Combat Veterans. Future studies should evaluate suicide risk in Army Combat Veterans over time to look for predictive variables unique to having a TBI, and to understand when and how to effectively intervene to prevent suicide. It is important to determine if suicide risk decreases after Army Combat Veterans with a TBI are evaluated, diagnosed, treated, and given a Purple Heart medal. This could be a systematic preventive intervention for Combat Veterans with a TBI. Lastly, public education efforts are necessary to enhance everyone’s understanding of the connections between combat-related TBIs and suicide risk. In the words of a Combat Veteran, “maybe, the more this gets talked about and the more people will be reading these articles going ‘hey that happened to me, too,’ and they get diagnosed with a TBI, and they get a Purple Heart … maybe they’ll go get checked up on and get help if they need it.”
Acknowledgments
We thank James Schreiber, PhD (Duquesne University) for providing statistical oversight throughout the study and Dr. Joane T. Moceri (University of Portland) for her consultation. We also extend our gratitude to the Army Combat Veterans who courageously shared their stories with us.
Funding Statement
This work was in part supported by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. (W81XWH-16-2-0004). Opinions, interpretations, conclusions, and recommendations are those of the author and are not necessarily endorsed by the MSRC or the Department of Defense.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
- Allan, N. P., Gros, D. F., Lancaster, C. L., Saulnier, K. G., & Stecker, T. (2019). Heterogeneity in short‐term suicidal ideation trajectories: Predictors of and projections to suicidal behavior. Suicide and Life-Threatening Behavior, 49(3), 826–837. 10.1111/sltb.12480 [DOI] [PubMed] [Google Scholar]
- Anestis, M. D., & Bryan, C. J. (2013). Means and capacity for suicidal behavior: A comparison of the ratio of suicide attempts and deaths by suicide in the US military and general population [Article]. Journal of Affective Disorders, 148(1), 42–47. 10.1016/j.jad.2012.11.045 [DOI] [PubMed] [Google Scholar]
- Anestis, M. D., Khazem, L. R., Mohn, R. S., & Green, B. A. (2015). Testing the main hypotheses of the interpersonal-psychological theory of suicidal behavior in a large diverse sample of United States military personnel. Compr Psychiatry, 60, 78–85. 10.1016/j.comppsych.2015.03.006 [DOI] [PubMed] [Google Scholar]
- Army Human Resources Command . (2019). Purple Heart. https://www.hrc.army.mil/content/Purple%20Heart
- Brenner, L. A., Homaifar, B. Y., Adler, L. E., Wolfman, J. H., & Kemp, J. (2009). Suicidality and veterans with a history of traumatic brain injury: Precipitating events, protective factors, and prevention strategies. Rehabilitation Psychology, 54(4), 390–397. 10.1037/a0017802 [DOI] [PubMed] [Google Scholar]
- Bryan, C., & Anestis, M. (2011). Reexperiencing symptoms and the interpersonal-psychological theory of suicidal behavior among deployed service members evaluated for traumatic brain injury. Journal of Clinical Psychology, 67(9), 856–865. 10.1002/jclp.20808 [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., Clemans, T. A., & Hernandez, A. M. (2012). Perceived burdensomeness, fearlessness of death, and suicidality among deployed military personnel. Personality and Individual Differences, 52(3), 374–379. 10.1016/j.paid.2011.10.045 [DOI] [Google Scholar]
- Bryan, C. J., & Cukrowicz, K. C. (2011). Associations between types of combat violence and the acquired capability for suicide [Article]. Suicide & Life-Threatening Behavior, 41(2), 126–136. 10.1111/j.1943-278X.2011.00023.x [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., Cukrowicz, K. C., West, C. L., & Morrow, C. E. (2010). Combat experience and the acquired capability for suicide [Article]. Journal of Clinical Psychology, 66(10), 1044–1056. 10.1002/jclp.20703 [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., Hernandez, A. M., Allison, S., & Clemans, T. (2013). Combat exposure and suicide risk in two samples of military personnel [Article]. Journal Of Clinical Psychology, 69(1), 64–77. 10.1002/jclp.21932 [DOI] [PubMed] [Google Scholar]
- Bullman, T., Schneiderman, A., & Bossarte, R. (2018). Suicide risk by unit component among Veterans who served in Iraq or Afghanistan. Archives of Suicide Research, 22(1), 1–10. 10.1080/13811118.2017.1304308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterworth, S. E., Green, B. A., & Anestis, M. D. (2017). The association between specific combat experiences and aspects of the Interpersonal Theory of Suicide. Comprehensive Psychiatry, 78, 9–18. 10.1016/j.comppsych.2017.06.003 [DOI] [PubMed] [Google Scholar]
- Cerel, J., Van de Venne, J. G., Moore, M. M., Maple, M. J., Flaherty, C., & Brown, M. M. (2015). Veteran exposure to suicide: Prevalence and correlates. Journal of Affective Disorders, 179, 82–87. 10.1016/j.jad.2015.03.017 [DOI] [PubMed] [Google Scholar]
- Cernak, I. (2017). Understanding blast-induced neurotrauma: How far have we come? Concussion, 2(3), CNC42. 10.2217/cnc-2017-0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell, J. W., & Plano Clark, V. L. (2018). Designing and conducting mixed methods research (3rd ed.). Sage. [Google Scholar]
- Department of Defense . (2012, September 18). DoD policy guidance for management of mild traumatic brain injury/concussion in the deployed setting (Policy No. 6490.11).
- Faul, F., Erdfelder, E., Buchner, A., & Lang, A. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Fonda, J. R., Fredman, L., Brogly, S. B., McGlinchey, R. E., Milberg, W. P., & Gradus, J. L. (2017). Traumatic brain injury and attempted suicide among Veterans of the wars in Iraq and Afghanistan. American Journal of Epidemiology, 186(2), 220–226. 10.1093/aje/kwx044 [DOI] [PubMed] [Google Scholar]
- Giacomo, C. (2019, November 1). Suicide has been deadlier than combat for the military. The New York Times. https://www.nytimes.com/2019/11/01/opinion/military-suicides.html
- Gutierrez, P. M., Pease, J., Matarazzo, B. B., Monteith, L. L., Hernandez, T., & Osman, A. (2016). Evaluating the psychometric properties of the Interpersonal Needs Questionnaire and the acquired capability for Suicide Scale in military veterans. Psychological Assessment, 28(12), 1684–1694. 10.1037/pas0000310 [DOI] [PubMed] [Google Scholar]
- Holloway, I., & Galvin, K. (2017). Qualitative research in nursing. John Wiley & Sons Incorporated. [Google Scholar]
- Houtsma, C., Khazem, L. R., Green, B. A., & Anestis, J. C. (2017). Isolating effects of moral injury and low post-deployment support within the U.S. military [Article]. Psychiatry Research, 247, 194–199. 10.1016/j.psychres.2016.11.031 [DOI] [PubMed] [Google Scholar]
- Joiner, T. E. (2005). Why people die by suicide. Harvard University Press. [Google Scholar]
- Kimbrell, T., Pyne, J. M., Kunik, M. E., Magruder, K. M., Petersen, N. J., Yu, H. J., Hudson, T. J., Schulz, P. E., & Qureshi, S. U. (2011). The impact of Purple Heart commendation and PTSD on mortality rates in older veterans. Depression and Anxiety, 28(12), 1086–1090. 10.1002/da.20850 [DOI] [PubMed] [Google Scholar]
- Leininger, M., & McFarland, M. R. (2006). Culture care diversity and universality: A worldwide nursing theory (2nd ed.). Jones and Bartlett. [Google Scholar]
- Martin, R. L., Assavedo, B. L., Bryan, A. O., Green, B. A., Capron, D. W., Rudd, M. D., Bryan, C. J., & Anestis, M. D. (2020). The relationship between post-battle experiences and thwarted belongingness and perceived burdensomeness in three United States military samples. Archives of Suicide Research, 24(sup1), 156–172. 10.1080/13811118.2018.1527266 [DOI] [PubMed] [Google Scholar]
- Martin, R. L., Houtsma, C., Bryan, A. O., Bryan, C. J., Green, B. A., & Anestis, M. D. (2017). The impact of aggression on the relationship between betrayal and belongingness among US military personnel. Military Psychology, 29(4), 271–282. 10.1037/mil0000160 [DOI] [Google Scholar]
- Military Health System . (2020, July 17). DoD numbers for TBI worldwide. https://health.mil/About-MHS/OASDHA/Defense-Health-Agency/Research-and-Development/Traumatic-Brain-Injury-Center-of-Excellence/DoD-TBI-Worldwide-Numbers
- Miller, T. C., & Zwerdling, D. (2010). Soldiers with brain trauma denied Purple Hearts, adding insult to injury. ProPublica. https://www.propublica.org/article/soldiers-with-brain-trauma-denied-purple-hearts-adding-insult-to-injury [Google Scholar]
- Moceri-Brooks, J., Garand, L., Sekula, L. K., & Joiner, T. (2023). Exploring the use of the Interpersonal Needs Questionnaire to examine suicidal thoughts and behaviors among Post-9/11 U.S. Combat Veterans: An integrative review. Military Psychology, 1–13. 10.1080/08995605.2023.2178223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteith, L. L., Schneider, A. L., Holliday, R., & Bahraini, N. H. (2021). Assessing institutional betrayal among female veterans who experienced military sexual trauma: A rasch analysis of the Institutional Betrayal Questionnaire.2. Journal of Interpersonal Violence, 36(23–24), 10861–10883. 10.1177/0886260520983959 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences and Medicine . (2022). Traumatic brain injury: A roadmap for accelerating progress. The National Academies Press. 10.17226/25394 [DOI] [PubMed] [Google Scholar]
- Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The suicidal behaviors questionnaire-revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. 10.1177/107319110100800409 [DOI] [PubMed] [Google Scholar]
- ProPublica . (2012). Lost to history: Missing war records complicate benefit claims by Iraq, Afghanistan Veterans. https://www.propublica.org/article/lost-to-history-missing-war-records-complicate-benefit-claims-by-veterans
- Smith, C. P. (2017). First, do no harm: Institutional betrayal and trust in health care organizations. Journal of Multidisciplinary Healthcare, 10, 133–144. 10.2147/JMDH.S125885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick, B. G., & Fidell, L. S. (2001). Using multivariate statistics. Allyn and Bacon. [Google Scholar]
- Tanielian, T., & Jaycox, L. (2008). Invisible wounds of war. RAND Corporation. [Google Scholar]
- Van Orden, K. A., Cukrowicz, K. C., Witte, T. K., & Joiner, T. E. (2012). Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychology Assessment, 24(1), 197–215. 10.1037/a0025358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Suicide Prevention, House of Representatives . (2019). https://www.c-span.org/video/?460184-1/veteran-suicide-prevention
- von Steinbüchel, N., Wilson, L., Gibbons, H., Hawthorne, G., Höfer, S., Schmidt, S., Bullinger, M., Maas, A., Neugebauer, E., Powell, J., von Wild, K., Zitnay, G., Bakx, W., Christensen, A., Koskinen, S., Sarajuuri, J., Formisano, R., Sasse, N., & Truelle, J. (2010). Quality of life after brain injury (QOLIBRI): Scale development and metric properties. Journal of Neurotrauma, 27(7), 1167–1185. 10.1089/neu.2009.1076 [DOI] [PubMed] [Google Scholar]
- Zwerdling, D., & Miller, T. C. (2010, September 9). Purple hearts elusive for traumatic brain injuries. NPR. https://www.npr.org/2010/09/09/129606127/purple-hearts-elusive-for-traumatic-brain-injuries [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.