The organisation of primary care services and their role as gatekeepers to more expensive specialist services have become key issues for policymakers, managers, and health professionals in many healthcare systems. The importance of primary care in delivering accessible, high quality services while constraining escalating costs is widely recognised.
In England the Labour government elected in 1997 made the formation of primary care groups and trusts the organisational centrepiece of its reforms to the NHS.1 Primary care groups, established throughout England in 1999, are expected to play a leading role in improving health, reducing inequalities, managing a unified budget for the health care of their registered populations, modernising services, improving quality, and integrating services through closer partnerships. Initially operating as subcommittees of health authorities, they bring together general practitioners, nurses, other health professionals, managers, and representatives of other service providers to manage local services. As they show their ability to manage their budgets and services, they take increased responsibility by becoming freestanding primary care trusts. In April 1999, 481 primary care groups were established in England; 17 of these became primary care trusts in April 2000, and many more are currently in the process of moving to trust status.
Summary points
The size of primary care organisations is only one of the factors that affect their performance: others include their policy priorities, functions, other organisational features, and the environment in which they operate
There is no evidence that increases in size of primary care groups and trusts beyond 100 000 patients will automatically generate substantial improvements in overall performance or economies of scale
Optimal size varies substantially for different functions of primary care groups and trusts
Organisational structures and organisational alliances can be used to achieve the different optimal sizes for different functions
One size will not suit all: bigger may be better for some functions and worse for others
The NHS white paper The New NHS suggested that primary care groups would typically serve populations of about 100 000,1 reflecting a policy of devolving responsibility and decision making to local communities. Although this recommended size did not seem to be based on a systematic review of evidence about optimal size, it probably reflected a mixture of experience (such as in relation to various models of commissioning) and consultation with managers and health professions involved in primary care.2 When primary care groups were established in 1999, they did indeed conform broadly with the policy, having average populations of about 100 000—though with a range from South West Shropshire's 43 618 patients, 29 general practitioners, and 8 practices to Brighton and Hove's 277 160 patients, 140 general practitioners and 53 practices. It has rapidly become apparent, however, that many health authorities and primary care groups consider a population of 100 000 to be too small, particularly for transition to trust status. Two thirds of trusts were considering mergers within their first six months,3 seemingly reflecting a widely held view that the optimum size was probably closer to 200 000 than 100 000. The national tracker survey of primary care groups and trusts reported that the average population size would increase to 183 000 if all the planned mergers go ahead.3 Primary care groups seem to have been caught up in the same “merger mania” that has been a feature of other parts of the healthcare systems of both Britain4,5 and the United States.6,7
We have recently completed a comprehensive review of the theoretical issues and empirical evidence which should inform decisions concerning the optimal size of primary care groups and trusts.8 We summarise the main conclusions below and discuss their implications for the advantages and disadvantages of mergers. While our conclusions are directed particularly at the issues faced by primary care organisations in England, they are relevant to all policymakers, managers, and health professionals facing decisions about the optimal size of healthcare organisations.
Methods
The main sources of empirical evidence relevant to optimal size of primary care organisations are the US literature on managed care organisations and the UK literature on the total purchasing pilot sites. We reviewed this evidence alongside more broadly based empirical and conceptual work on size and performance from the health services research, organisation theory, and industrial economics literatures (box B1).
Box 1.
: Sources of evidence on optimal size of primary care groups and trusts
- Search strategy
- Systematic search of bibliographic databases (see tables A and B on BMJ 's website for more details)
- Hand search of published and grey literature
- Direct approach to researchers working in the subject
- Theoretical literature
- Economic theory of firms, industrial organisations, and organisational change
- Empirical literature on size and performance
- US data—15 studies of managed care, primarily quantitative (multiple regression analysis, data envelopment analysis)
- UK data—15 studies, predominantly of total purchasing pilots, primarily qualitative; 3 quantitative simulations
Results of observational studies
The US and UK observational studies each have advantages and disadvantages. The US data permit more sophisticated statistical analysis, but there are considerable differences between US managed care organisations and English primary care groups and trusts in terms of their objectives, the extent of competition between them, the extent to which care is free at the point of use, and the healthcare labour markets in which they operate. Although the UK research has a more relevant institutional context, total purchasing pilot sites were limited to commissioning hospital and community health services, did not have unified budgets, and were not responsible for clinical governance. They did, however, have some ability to move resources between different areas of spending. With populations of about 30 000, they were also much smaller than primary care groups and trusts. Nevertheless, the evidence allows some conclusions to be drawn that are relevant to primary care groups and trusts (box B2). A description of the principal published studies is available on the BMJ 's website (tables C and D) and in our full report.8
Box 2.
: Empirical evidence on scale and performance of primary care organisations
- Evidence from US managed care organisations suggests that the per capita cost of providing care is minimised at population levels that are no larger, and possibly smaller, than the average size of primary care groups and trusts
- Evidence from UK total purchasing pilots suggests that managerial economies of scale are exhausted at population levels smaller than the current average size of primary care groups and trusts
- Evidence on the effect of size on bargaining power with providers is ambiguous: larger primary care groups and trusts may not be permitted to move their business to another provider
- Optimal population size for commissioning varies widely depending on the services being commissioned
- There is some evidence of economies of scale in pooling risks, but the marginal gains from pooling diminish rapidly with increasing population size: primary care groups and trusts of average size do not face substantial risks of bankruptcy
- There is no evidence that clinical governance activity benefits from economies of scale: larger organisations encounter increased problems in sustaining professional commitment and involvement in quality improvement activity
Putting size in context
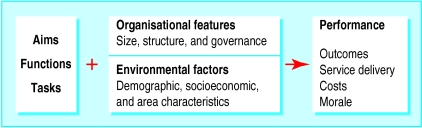
Consideration of the optimal size for primary care organisations needs to be set in a wider conceptual framework encompassing the roles they play in the NHS, other organisational features, the environment in which they work, and the various aspects of performance that are relevant (figure). Optimal size will depend on the aims, functions, and tasks of the organisation and may differ for different functions (health improvement, commissioning hospital and community services, providing primary care services, and influencing service quality).
Nor is size the only relevant feature. Performance will also be affected by the way that an organisation is governed, its management arrangements, its budgetary mechanisms, its implicit and explicit incentive schemes for teams and individuals, the ways it works with other organisations, the sociodemographic structure of the population it serves, and the characteristics of the area in which it operates. Organisational size is but one factor affecting the performance of an organisation.
This is illustrated by the risk pooling argument for large population size. Simulation studies using NHS data provide strong support for economies of scale in managing risks by pooling: the probability of substantial overspend or underspend per capita falls as the population covered increases.9–11 However, pooling is by no means the only method of managing risk. Primary care groups and trusts can be allowed to carry forward budget surpluses when demand is unexpectedly small and draw down the banked surplus when demand generates a deficit in a period. They can be permitted to insure—paying a premium from their budget each period and in return having the insurer cover their budget deficits in years when demand is high. The insurer could be the health authority, a group of primary care groups or trusts, or even private insurance companies. The fact that there are economies of scale in pooling risks does not imply that large size is the best method of managing expenditure risk.
A second illustration is commissioning. Given the differential incidence of different conditions in the population, the required total population to effectively commission for a service varies considerably,12,13 from about 50 000 or less for community nursing to over 1 000 000 for organ transplants. If the commissioning unit is the primary care organisation, such disparities imply difficult trade-offs in choosing the optimal size. But the commissioning unit can be smaller than a primary care group or trust if budgets are delegated to locality groups of practices within the group or trust. Or it can be larger than the primary care organisation if several such groups or trusts form a commissioning cooperative to purchase care for treatment of rarer conditions. The fact that large size may be best for some functions does not in itself imply that individual primary care organisations need to be responsible for large populations.
Size and other organisational features
The impact of population size on a primary care organisation's performance will depend on many other features of the organisation (box B3), including the extent to which services are directly provided or are commissioned from outside the organisation. The case for direct provision is often supported by the argument that it will ensure that the service provided better meets the organisation's specifications and quality criteria, because direct control of resources and employees gives greater control over work processes and outcomes. It is also often assumed that bringing services under a single organisational structure will enable service providers to work more closely together and to provide a better coordinated service to patients. However, evidence from US healthcare providers suggests that direct provision is not necessary to achieve these aims.14–18
Box 3.
: Effects of population size and organisational features on primary care organisations' performance
- Direct provision of services may improve control, but commissioning services provides increased flexibility and can achieve high levels of integration
- Larger primary care groups and trusts are likely to become more centralised and hierarchical with less professional engagement
- Partnerships and alliances around particular functions may have advantages over a single size for all functions
- Mergers often fail to deliver the anticipated benefits
- Positive outcomes of mergers require substantial investment in the management of change and may damage staff morale
Process costs and mergers
It is necessary to consider the process of increasing the size of primary care organisations through mergers. Evidence from the United States7and the NHS5,19 suggests that many mergers yield disappointing results and that any positive effects take a long time to appear. The anticipated benefits of mergers are largely in achieving economies of scale, particularly in terms of reduced management costs. The short to medium term costs lie in the additional management resource required to support the process, the damaging effect on staff morale, and the disruption to organisations caused by mergers. Mergers require careful preparation if anticipated benefits are to be realised and staff morale maintained.19,20
Discussion
Size is but one characteristic of primary care organisations, and optimal size will vary for different functions, with different organisational and governance structures, and in different environments. Despite the importance of the issue of organisational size, the evidence available from published research is limited both in quantity and relevance for primary care groups and trusts. However, four general conclusions that are relevant can be drawn from our review of the empirical and theoretical literature:
There is no evidence that increases in the population size of primary care groups or trusts beyond 100 000 will generate important cost savings or improvements in overall performance
Optimal size will vary substantially for different functions of primary care organisations
Organisational structures and organisational alliances can be used to achieve differing levels of aggregation for different functions
The important question is the optimal organisation of primary care groups and trusts, not just their size.
The issues facing primary care groups, health authorities, and the NHS Executive concerning mergers are immediate and pressing, and many primary care groups are already well advanced in preparations for the completion of mergers in April 2001. Many more potential mergers are still at the discussion stage and have not yet been finalised. The research evidence should cause managers and health professionals to consider whether mergers will deliver the anticipated benefits and at what costs.
All primary care organisations, regardless of population size, should look at ways of creating organisational structures and alliances for particular functions to deliver the benefits of larger size where these exist and of smaller size where this is beneficial. For those that remain relatively small (below 100 000), this may mean working in alliance with neighbouring groups or trusts for certain aspects of commissioning and strategic planning, particularly in developing partnership working with local authorities when strategic planning is likely to benefit from conterminous boundaries and populations. Even in their first year, most primary care groups were collaborating closely with their immediate neighbours in commissioning services, so much of the groundwork has already been done to establish collaborative commissioning based on larger populations. For larger primary care groups and trusts, obtaining the optimal mix of size and organisational features may mean creating devolved budgets and responsibilities for those functions that benefit from smaller organisational units. They will need to look to the formation of locality groups in areas such as primary care development and quality improvement through clinical governance.
Many primary care groups have been encouraged to merge by their health authorities,3 and there is anecdotal evidence that some health authorities have been applying considerable pressure. While this pressure is often rationalised by the anticipated benefits of a larger population, it also seems to reflect a lack of financial and managerial capacity at the level of health authorities and primary care groups and trusts. Health authorities have found themselves stretched in providing support and managing primary care groups. Smaller primary care groups have been constrained by the allocation of a management budget on a per capita basis (about £3 per head of population) and have seen mergers as the only way of increasing their managerial capacity. Both health authorities and primary care groups and trusts have found themselves drawing on the same limited pool of managers to staff a larger number of organisations.
These factors have fuelled the trend towards mergers, but they have little to do with the fundamental issue of whether mergers will deliver improved services at lower cost. Mergers in health care and other sectors of the economy are often a short term answer to a lack of resources to support the necessary managerial infrastructure and a shortage of skilled managers. Such justifications, though understandable given the pressures placed on health authorities and primary care organisations, are short sighted. The NHS Executive should look carefully at the constraints placed on the management budgets of primary care organisations and the shortage of managerial expertise to ensure that these do not become the major factors in decisions to merge.
Successful mergers require substantial investment in managerial capacity, careful attention to staff morale, and sufficient time to realise potential benefits. Many primary care groups have devoted considerable effort to securing the enthusiastic involvement of health professionals, and many felt that their successes in this area to be among their most important achievements during their first year.3 As these primary care groups merge with their neighbours, they will need to devote more time and resources to ensuring that the workforce remains motivated and that staff morale is sustained.
Supplementary Material
Figure.
Conceptual framework for considering optimal size of primary care organisations
Acknowledgments
We are grateful for comments from Brian Ferguson, Alan Maynard, Peter Smith, and Andy Street.
Footnotes
Funding: The authors are employed in the National Primary Care Research and Development Centre, which is funded by the Department of Health.
Competing interests: Nonedeclared.
Details of the literature search and its results appear on the BMJ's website
References
- 1.Secretary of State for Health. The new NHS: modern, dependable. London: Stationery Office; 1997. [Google Scholar]
- 2.Secretary of State for Health. Primary care: the future. Leeds: NHS Executive; 1996. [Google Scholar]
- 3.Wilkin D, Gillam S, Leese B, editors. National tracker survey of primary care groups and trusts: progress and challenges 1999/2000. Manchester: National Primary Care Research and Development Centre; 2000. [Google Scholar]
- 4.Garside P, Rice J. Merger mania. Health Serv J. 1994;104:22–24. [PubMed] [Google Scholar]
- 5.Goddard M, Ferguson B. Mergers in the NHS: made in heaven or marriages of convenience. London: Nuffield; 1997. [Google Scholar]
- 6.Shortell SM. The evolution of hospital systems: unfulfilled promises and self-fulfilling prophecies. Health Serv Res. 1998;45:177–214. doi: 10.1177/107755878804500202. [DOI] [PubMed] [Google Scholar]
- 7.Weill TP. Horizontal mergers in the United States: some practical realities. Health Serv Manage Res. 2000;13:137–151. doi: 10.1177/095148480001300301. [DOI] [PubMed] [Google Scholar]
- 8.Bojke C, Gravelle H, Wilkin D. Is bigger better for primary care groups and trusts? University of Manchester: National Primary Care Research and Development Centre; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crump BJ, Cubbon JE, Drummond MF, Hawkes RA, Marchment MD. Fundholding in general practice and financial risk. BMJ. 1991;302:1582–1584. doi: 10.1136/bmj.302.6792.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bachmann MO, Bevan G. Determining the size of total purchasing site to manage the financial risks of cost referrals: computer simulation model. BMJ. 1996;313:1054–1057. doi: 10.1136/bmj.313.7064.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin S, Rice N, Smith PC. Risk and the general practitioner budget holder. Soc Sci Med. 1998;47:1547–1554. doi: 10.1016/s0277-9536(98)00231-7. [DOI] [PubMed] [Google Scholar]
- 12.Killoran A, Griffiths J, Posnett J, Mays N. What can we learn from the total purchasing pilots about the management costs of primary care groups? A briefing paper for health authorities. London: King's Fund; 1998. . (National evaluation of total purchasing pilot projects working paper.) [Google Scholar]
- 13.Mays N, Dixon J. Purchaser plurality in UK health care. London: King's Fund; 1996. [Google Scholar]
- 14.Dynan L, Bazzoli G, Burns LR. Assessing the extent of integration achieved through physician-hospital arrangements. J Healthcare Manage. 1998;43:242–261. [PubMed] [Google Scholar]
- 15.Goldsmith JC. The illusive logic of integration. Healthcare Forum. 1994;37:26–31. [PubMed] [Google Scholar]
- 16.Kaluzny AD, Zuckerman HS, Ricketts TC, editors. Partners for the dance: forming strategic alliances in health care. Chicago: Health Administration Press; 1995. [Google Scholar]
- 17.Walston SS, Kimberly JR, Burns LR. Owned vertical integration and health care: promise and performance. Health Care Manage Rev. 1996;21:83–92. [PubMed] [Google Scholar]
- 18.Robinson JC, Casalino LP. Vertical integration and organizational networks in health care. Health Affair. 1996;15:7–22. doi: 10.1377/hlthaff.15.1.7. [DOI] [PubMed] [Google Scholar]
- 19.McClenahan J. Health care UK 1999/2000; the King's Fund review of health policy. London: King's Fund; 1999. Emerging problems with merger policy; pp. 94–97. [Google Scholar]
- 20.Garside P. Evidence based mergers? BMJ. 1999;318:345–346. doi: 10.1136/bmj.318.7180.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.