ABSTRACT
Understanding the extent to which youth and families experienced COVID-related stress requires accounting for prior levels of stress and other associated factors. This is especially important for military families, which experience unique stressors and may be reluctant to seek outside help. In this prospective study, we examined the role of pre-pandemic family factors in predicting parent and youth stress during the COVID-19 pandemic. Participants were 234 families with at least one active-duty parent and a 3rd or 5th-grade child. Findings revealed that preexisting factors predicted youth and family COVID-related stress. Specifically, heightened pre-pandemic parental stress and youth internalizing symptoms were significant predictors of COVID-related stress. Implications for mental health professionals and other organizations supporting military parents and families during the COVID-19 pandemic as well as other times of upheaval are discussed.
KEYWORDS: COVID-19, parental stress, internalizing and externalizing symptoms, youth, military families
What is the public significance of this article?— This study shows that military families and their children experienced stress adjusting during the early months of the COVID-19 pandemic. According to parent reports, pre-pandemic parental stress and youth internalizing symptoms (i.e., symptoms of depression and anxiety) were associated with more stress during the pandemic. These findings can help mental health professionals supporting military families identify which families might be particularly at risk during the pandemic or other challenging times.
The onset of the COVID-19 pandemic greatly disrupted family life in the U.S. Closures, social distancing, and quarantine mandates restricted access to sources of support for parents and their children. Globally, numerous studies have highlighted that families experienced increased stress and negative mental health consequences during the pandemic (Ellis et al., 2020; Magson et al., 2020; Spinelli et al., 2020). School and workplace closures forced many parents to abruptly change their daily routines and restricted their access to previously available resources. Parents were tasked with managing their children’s health and educational needs while attending to their own health and occupational needs (Garbe et al., 2020; Patrick et al., 2020). In the early months of the pandemic, nearly half of all U.S. parents reported their stress levels were “high” (American Psychological Association, 2020), and over one-third of working parents reported struggling to manage childcare responsibilities (Pew Research Center, 2020). Rates of parental burnout increased significantly in most countries (Van Bakel et al., 2022), likely amplified by increased isolation and limited opportunities for respite through social interactions or leisure activity (Griffith, 2020).
Likewise, school closures and restrictions in extracurricular activities were associated with additional stressors for youth (Ellis et al., 2020; Magson et al., 2020). Youth reported increased conflict with parents and siblings (Evans et al., 2020) and greater isolation from peers and teachers (Rogers et al., 2021). Learning loss has also been documented, with younger students being the most affected (Donnelly & Patrinos, 2021). Furthermore, studies suggest a worsening trend for psychological adjustment among youth globally; rates of depression and anxiety doubled relative to pre-pandemic rates (Racine et al., 2021). Many youths also reported COVID-specific fears and worries related to themselves or a family member contracting the virus (Samji et al., 2022).
Military families and the COVID-19 pandemic
Although the impacts of COVID-19 were felt in all communities, its impact on military families has received little attention. There are more than 1.6 million youth in active-duty military families in the U.S. (U.S. Department of Defense, 2022). Military families are thought to be highly resilient, yet they face multiple, repeated stressors such as relocation and separations due to training and deployments, which can disrupt educational and employment experiences for family members (Blue Star Families, 2020a). In fact, research has found that frequent moves and parental deployments are stressful for military parents (Ruff & Keim, 2014) and associated with negative mental health and educational outcomes for military-connected youth (De Pedro et al., 2011) with the strongest associations occurring during middle childhood (Card et al., 2011). In addition, home-front parents may feel isolated or distressed with additional caregiving burdens when a military parent is deployed (Bradshaw et al., 2010; Lester et al., 2010). Frequent military-related moves can also limit opportunities to establish community ties and reduce access to extended family members who could help with various caregiving tasks. Military families have also been found to engage in less help-seeking behavior, in large part due to the stigma associated with help-seeking and pressure to demonstrate resiliency within military culture (Hall, 2011; Vogt, 2011).
During the pandemic, active-duty service members were considered “essential workers” required to work in field settings, which carried an increased risk of contracting the virus and may have exacerbated stress associated with balancing work and increased parenting demands (Khazan & Harris, 2020). Military families also experienced a “stop movement” order during the pandemic, which halted all movement among service members and their families. Thus, families awaiting relocation assignments faced uncertainty about the next steps, and service members returning from deployment or training experienced delays in returning to their families.
Pre-pandemic factors predicting adjustment to COVID-19
Preexisting vulnerabilities within families are likely to affect their adjustment to the pandemic (Prime et al., 2020), including preexisting levels of parenting stress as well as parental and youth mental health. Parenting stress, defined as a negative response resulting from a mismatch between parenting demands and resources available to meet those demands (Deater-Deckard, 1998), is a known risk factor for parental depression (Deater-Deckard, 1998; Song et al., 2022), the use of less effective parenting strategies (Coldwell et al., 2006), and increased child behavioral problems (Briggs-Gowan et al., 2001). These associations tend to be reciprocal in nature (Neece et al., 2012). For example, mothers with heightened levels of anxiety and depression tend to use more maladaptive parenting practices (England & Sim, 2009), which could add to overall levels of family stress and reduced youth well-being. In turn, youth with internalizing (e.g., anxiety, depression) and externalizing (e.g., defiance, aggression, hyperactivity) symptoms tend to place greater demands on parents’ time and energy, thereby increasing family levels of stress. Although these conditions are treatable, therapeutic services were likely more difficult to access during the pandemic. Likewise, although social support moderates youths’ experiences of stress and depression (Wang et al., 2014), if youth with preexisting mental health concerns had limited access to support from peers or adults, their symptoms may have been exacerbated (Fegert et al., 2020).
Few studies have explored pre-pandemic predictors of adjustment among general samples of parents and children. Westrupp et al. (2021) found preexisting parent and child psychological symptoms were predictive of worsened functioning and more strained relationships among both parents and children during the pandemic. Likewise, Van Loon et al. (2021) found that adolescents with higher levels of pre-pandemic stress reported more COVID-19 concerns about school, getting sick, and financial problems. Adolescents’ pre-pandemic internalizing problems were also associated with greater COVID-19 financial concerns. Studies have not yet addressed these questions with younger children whose COVID-19 concerns may have functioned differently given their development stage and potentially more limited understanding. Further, research is also needed examining the differences in COVID-related stress between youth with internalizing symptoms and those with externalizing symptoms, as children’s internalizing and externalizing symptoms may be differentially related to youth and family COVID-related stress.
Demographic factors
Demographic factors may also place some youth and families at increased risk of stress adjusting to the COVID-19 pandemic. During the pandemic, role strain appears to have disproportionately affected women in military families, including both service members and civilian spouses, with women reporting more negative impacts to their employment, their mental health, and their children’s mental health than men (Blue Star Families, 2020b). Single-parent families are also likely at greater risk due to one parent assuming all caregiving responsibilities in addition to attending to their own needs and job demands; these households might typically rely on external supports for respite, but pandemic-related closures might have restricted access to these supports, resulting in higher levels of stress (Ozbay et al., 2007). Similarly, families in which one parent is deployed or away for training may function similarly to single-parent households, posing an additional strain on the parent who is caregiving.
Current study
The goal of this prospective study of military families is to examine the degree to which pre-pandemic levels of parental stress and internalizing symptoms, and youth internalizing and externalizing symptoms predicted youth and family stress during the COVID-19 pandemic (i.e., “COVID-related stress”). We posited that parents’ reports of their own levels of pre-pandemic stress and internalizing symptoms, as well as their children’s internalizing and externalizing symptoms, would be positively associated with youth and family COVID-related stress levels. We expected to find these hypothesized associations even when controlling for the parent’s gender, marital and military status, rank, and whether a parent was deployed as well as child grade. By identifying risk factors predicting military families’ COVID-related stress, we hoped to gain information that could bolster efforts to support these families in the event of future national emergencies as well as during times of military-related upheaval such as the deployment of a parent or relocation.
Method
Participants
Participants were 234 parents enrolled in a longitudinal study examining school supports for active-duty military families. At the time of recruitment (Jan-Feb, 2019), all families had at least one active-duty parent and a 3rd (58.5%) or 5th (41.5%) grade student (i.e., target child) attending school in a civilian public school district located near a large U.S. military installation. We recruited families with 3rd and 5th-grade students into the larger study because past research suggests that children begin to reliably complete self-report measures at this age (Woolley et al., 2004). For the larger study from which these data are drawn, to maximize our potential sample, we recruited families with students in nonconsecutive elementary school grades in two consecutive years. The 2nd cohort was recruited in spring 2020 and therefore, is not included in this analysis. Among target children, 53.6% were female, and 46.4% were male. At the beginning of the COVID-19 pandemic, their average age was 10.8 years (SD = 1.1). Nearly one-fifth of families (18.7%) had a parent deployed at baseline (i.e., away for more than two weeks as part of his/her military work; the median length of current deployment was 12 or more months). Demographic characteristics of the parents are provided in Table 1.
Table 1.
Participant demographic characteristics (N = 234).
| Variable | % |
|---|---|
| Gender | |
| Female | 74.7% |
| Male | 25.3% |
| Military Status | |
| Active Duty | 30.8% |
| Civilian | 69.2% |
| Dual Military Family | 6.6% |
| Enlisted | 48.8% |
| Warrant or Commissioned Officer | 51.2% |
| Service Branch | |
| Army | 90.4% |
| Air Force | 7.6% |
| Navy | 1.0% |
| Marines | 0.5% |
| Coast Guard | 0.5% |
| Marital Status | |
| Married or living with a partner | 88.8% |
| Divorced | 7.1% |
| Separated | 2.5% |
| Single, never married | 1.5% |
| Race/Ethnicity | |
| White | 69.0% |
| Hispanic, Latinx, or Spanish origin | 18.5% |
| Black or African American | 17.4% |
| Asian | 9.8% |
| Pacific Islander | 3.3% |
| Native American | 1.1% |
| Another racial identity | 3.8% |
Procedures
Participating families were recruited through their public school district (see, Steggerda et al., 2022 for a detailed description of recruitment procedures). As part of the larger study, all participating parents were invited to complete online surveys in Spring 2019 (baseline) and Spring 2020 (follow-up) after schools had closed due to the COVID-19 pandemic. Baseline surveys were completed by 198 (78.0%) of the parents who originally consented. Follow-up surveys were completed by 184 parents (72.4%). Parents who completed one or both surveys were included for analysis (n = 234). Parents received a $20 gift card for each completed survey. All study procedures were approved by the Boston University Institutional Review Board.
Measures
Pre-pandemic family characteristics
Parental stress
Parents reported their baseline level of parental stress using the Parental Stress Items Scale (PSIS; Pearlin & Schooler, 1978). The PSIS consists of 7 items rated on a 4-point Likert scale (1 = “Not at All,” 4 = “Very Much”). Parents indicated how much they experienced each feeling (e.g., “frustrated,” “tense”) as a parent to the target child. The PSIS demonstrated good internal consistency reliability in this sample (α = .84).
Parent internalizing symptoms
Parents reported their pre-pandemic levels of internalizing symptoms using the anxiety and depression scales from the Patient-Reported Outcomes Measurement Information System (PROMIS; Pilkonis et al., 2011). The PROMIS depression and anxiety scales each have 8 items. Parents rated how often they experienced symptoms of depression (e.g., “I felt hopeless”) and anxiety (e.g., “I felt nervous”) over the past 7 days using a 5-point Likert scale (1 = “Never,” 5 = “Always”). Because the depression and anxiety scales were highly correlated (r = .75), we created an index of parent internalizing symptoms by averaging all 16 items from the two scales. The 16-item scale demonstrated excellent internal reliability in this sample (α = .94).
Youth internalizing and externalizing symptoms
Parents reported their child’s baseline internalizing and externalizing symptoms using the Behavior and Feelings Survey (BFS; Weisz et al., 2020). The internalizing and externalizing subscales of the BFS are designed to be used separately or as one measure; each subscale consists of 6 items. The parent indicated how much their child has had each “problem during the past week” on a 5-point Likert scale (0 = “Not a Problem,” 4 = “A Very Big Problem”). The internalizing subscale includes symptoms of depression (e.g., “feeling down or depressed”) and anxiety (“e.g., “worrying about bad things happening”). The externalizing subscale includes behavioral and conduct problems (e.g., “being rude or disrespectful to people,” “breaking rules at home or at school”). Given that youth internalizing and externalizing symptoms had a low correlation (r = .35) and in line with previous research that has examined associations between parenting and internalizing and externalizing symptoms separately (e.g., Joo & Lee, 2022; Vierhaus et al., 2013), the two subscales were analyzed separately. Both subscales had excellent internal reliability in this sample (internalizing α = .92; externalizing α = .92).
Stress adjusting during COVID-19
At follow-up, parents responded to two questions: (a) How stressful has it been for your child to adjust to changes associated with the COVID-19 outbreak? and (b) How stressful has it been for your family to adjust to changes associated with the COVID-19 outbreak? Responses were on a 5-point scale (1 = “Not at All Stressful” to 5 = “Extremely Stressful”).
Control variables
We included the parents’ gender identity, marital status (“married or living with a partner”/all other categories), whether the respondent was on active duty or a civilian, whether the active-duty parent was enlisted or an officer, whether there was a parent deployed at baseline, and child grade as control variables due to their possible associations with baseline family characteristics.
Data analysis
We first examined the frequency distributions for the two variables measuring youth and family stress in adjusting during the pandemic. Second, we examined the bivariate correlations among all study variables. Control variables that were significantly associated with at least one independent variable were retained. Finally, we conducted two-step hierarchical multiple regressions separately for each dependent variable. Regressions were conducted in Mplus using full information maximum likelihood (FIML) to handle missing data. Associations between the control and dependent variables were analyzed in Step 1. Then, the independent variables were added to the model in Step 2 to test the study hypotheses.
Results
The frequencies of parents’ responses to questions assessing youth and family stress during the pandemic are presented in Figure 1. While there was variation in child and family stress adjusting to the COVID-19 pandemic, very few parents expressed that their children (5.4%) and families (3.8%) had experienced changes associated with COVID-19 as “not at all stressful.” In fact, parents reported that adjusting was “somewhat stressful” (as indicated by a score of 3 out of 5) for 42.9% of youth and for 50.0% of families. In addition, adjusting during COVID-19 was reported as “very stressful” (4 out of 5) or “extremely stressful” (5 out of 5) for 22.9% of youth and 20.1% of families.
Figure 1.
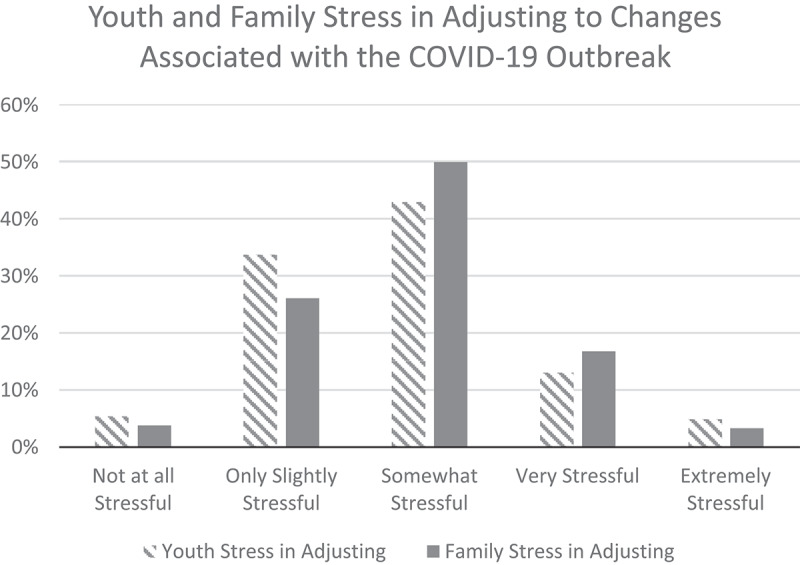
Youth and family stress in adjusting to changes associated with the COVID-19 outbreak.
Descriptive statistics for and correlations between pre-pandemic family functioning variables and parents’ reports of COVID-related stress are included in Table 2. All correlations were statistically significant in the expected direction. In examining associations between the control variables and baseline family characteristics, marital status was significantly associated with youth internalizing and externalizing symptoms (r = .174, p = .02; r = .163, p = .02, respectively) such that youth whose parents were married or living together were rated as having fewer symptoms. Further, having a deployed parent at baseline was positively associated with parent internalizing symptoms (r = .166, p = .02) such that the responding parent’s internalizing symptoms were worse if there was a deployed parent at that time. The respondent’s gender, whether they were on active duty, whether the active-duty parent was enlisted or an officer, and the child’s grade were not significantly correlated with any independent variables and therefore were removed from further analyses.
Table 2.
Descriptive statistics and correlations.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1. Parental Stress | 1.70 | 0.56 | |||||
| 2. Parent Internalizing | 1.59 | 0.60 | .54** | ||||
| 3. Youth Internalizing | 1.61 | 0.79 | .37** | .35** | |||
| 4. Youth Externalizing | 1.80 | 0.85 | .44** | .23** | .47** | ||
| 5. Youth COVID-Related Stress | 2.78 | 0.92 | .36** | .21* | .29** | .24** | |
| 6. Family COVID-Related Stress | 2.90 | 0.84 | .28** | .17* | .18* | .25** | .68** |
For parental stress, response options range from 1 to 4 with 4 indicating stronger agreement. For all other variables, response options range from 1 to 5. M and SD represent mean and standard deviation, respectively.
*p < .05, **p < .01.
Multiple regressions provided partial support for the hypothesis that parents’ reports of their child’s and family’s level of COVID-related stress would be associated with preexisting family characteristics (Table 3). Youth’s COVID-related stress was positively predicted by pre-pandemic parent reports of parental stress and youth internalizing symptoms. Neither parent internalizing symptoms nor youth externalizing symptoms predicted the youth’s levels of COVID-related stress. For family COVID-related stress, the only significant predictor was pre-pandemic parental stress, with parental stress predicting higher levels of family COVID-related stress.
Table 3.
Multiple regression models.
| Model 1: Youth COVID-Related Stress |
Model 2: Family COVID-Related Stress |
|||
|---|---|---|---|---|
| Variable | Step 1 | Step 2 | Step 1 | Step 2 |
| Parent Marital Status | −.514* | −.260 | −.376 | −.168 |
| Parent Deployed | .046 | −.120 | .204 | .102 |
| Parental Stress | .504** | .319* | ||
| Parent Internalizing | −.002 | .015 | ||
| Youth Internalizing | .197* | .053 | ||
| Youth Externalizing | .056 | .148 | ||
| R2 | .032 | .199** | .029 | .131* |
*p < .05, **p < .01.
Discussion
This study is among the first to examine stress experienced by military families during the COVID-19 pandemic. Given research suggesting that families, in general, faced significant challenges in the early months of the pandemic (Ellis et al., 2020) and that military-connected families face unique challenges (Blue Star Families, 2020a; De Pedro et al., 2011), we examined whether preexisting family stressors might predict adjustment to COVID-related disruptions. Results provided partial support for our hypotheses.
While military children and families can be highly resilient, our results suggest that most military children and families experienced at least moderate stress during this time. Parents in our sample most frequently reported that adjusting to the COVID-19 pandemic was “somewhat stressful” for both their child and family and rarely reported that adjusting was “not at all stressful.” Our initial bivariate analyses demonstrated that pre-pandemic parental stress, parent internalizing symptoms, youth internalizing symptoms, and youth externalizing symptoms were associated with parent reports of youth’s and families’ COVID-related stress. However, regression models indicated that only parental stress was associated with both youth and family COVID-related stress. This is the first known study to highlight pre-pandemic parental stress as an important risk factor for experiencing COVID-19 related stressors within military families. Our results also indicated pre-pandemic youth internalizing symptoms to be predictive of youth COVID-related stress within military families, supporting Van Loon et al.’s (2021) finding that civilian adolescents’ pre-pandemic internalizing problems were associated with greater COVID-19 concerns. Although prior studies have suggested that preexisting parental and youth psychopathology are predictive of worsened functioning during the pandemic (e.g., Westrupp et al., 2021), parent-reported youth externalizing symptoms and parent internalizing symptoms were not significant predictors of COVID-related stress within these military families. This may be partially attributed to covariance between these variables and parental stress. It is possible that in this circumstance, the demands of parenting a child with externalizing symptoms and/or the depleted parenting resources available to parents with internalizing systems are leading to parental stress (Deater-Deckard, 1998), which is in turn associated with COVID-related stress. Further research would allow for a deeper understanding of the reciprocal nature of parental stress and parent and child psychological symptoms in the context of the COVID-19 pandemic.
Limitations and implications for future research
This study has several limitations. First, we relied on parent reports of youth and family factors, which could reflect some bias in our assessment of child and family stress and functioning. For example, parents who report feeling stressed might be more likely to report that their children also experience higher levels of stress. Future research would benefit from the use of both parent and child reports of family functioning and stress. Parents also were asked about one particular child in their family. Parents likely experience different levels of parental stress with different children and would likely report different levels of internalizing and externalizing symptoms for each sibling. Parent reports of family COVID-related stress are likely influenced by these other family relationships; thus, these relationships should be considered in future research.
This study did not detect differences in the experiences of these military families based on the child’s grade. While the two-year difference may not have been sufficient to identify developmentally different experiences between the two groups, future research including a wider developmental window can address if and how youth development plays a role in COVID-19 stress. In addition, due to sample limitations, we were unable to conduct subgroup analyses to address questions about possible disparities across race or ethnicity in how military families responded to the COVID-19 pandemic (e.g., Karaca-Mandic et al., 2021).
Youth and family stress in adjusting during the pandemic were measured in Spring 2020, which was early in the pandemic and coincided with news of school closures and stay-at-home orders. This timing reflects a unique strength of the study: its examination of “early pandemic” functioning. Yet, it is possible that longer-term adjustment in these military families was differentially influenced by preexisting parent and youth characteristics, and that stress levels may change over time. Future studies should examine longer-term military family adjustment during the COVID-19 pandemic to determine whether levels of stress persist or change over time. In addition, the risk factors we explored were linked specifically with youth and family stress adjusting during the COVID-19 pandemic. Future research could examine how these factors relate to stress in adjusting during other transitions and challenging circumstances commonly faced by military families as well as protective factors that buffer children and families during challenging times.
Practice implications
While the COVID-19 pandemic created sudden changes and challenges across the world, military families experience times of upheaval frequently due to military life (e.g., parental separations during training and deployments, frequent moves). To mitigate the potential negative outcomes of these stressful times, mental health professionals and other organizations involved in supporting military parents and families (e.g., schools) should be aware of factors that can contribute to how these families adapt. Disruptions due to COVID-19 likely challenged many families regardless of preexisting vulnerabilities, but our results suggest military parents who were facing high levels of stress and children who were experiencing internalizing symptoms prior to the pandemic were at greater risk for COVID-related stress as pandemic-related changes unfolded. School psychologists and teachers can play an important role in supporting military-connected students and parents by monitoring their struggles and providing additional support, especially during times of stress. Likewise, greater awareness of the potential for parental stress and child internalizing problems to shape how military families responded to the pandemic could inform efforts to support these families when faced with other kinds of challenging and prolonged difficulties. Indeed, the results of this study could normalize the level of stress experienced by military families and counter the tendency to dismiss pandemic-related stressors that negatively affected civilian families (American Psychological Association, 2020). Reducing stigma and normalizing stress are important steps in promoting military families’ help-seeking behavior across contexts.
Acknowledgments
The authors would like to thank our school district and local partners, as well as the families who shared their experiences with us.
Funding Statement
The research reported here was supported by the Institute of Education Sciences, U.S. Department of Education, through Grant #R305A180142 to Boston University. The opinions expressed are those of the authors and do not represent views of the Institute or the U.S. Department of Education.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, ALD, upon reasonable request.
References
- American Psychological Association . (2020). Stress in the time of COVID-19, volume one. https://www.apa.org/news/press/releases/stress/2020/report
- Blue Star Families . (2020a). 2019 Military Family Lifestyle Comprehensive Report. https://bluestarfam.org/survey/
- Blue Star Families . (2020b). Resilience under stress study: Comprehensive report. https://bluestarfam.org/research/russ
- Bradshaw, C. P., Sudhinaraset, M., Mmari, K., & Blum, R. W. (2010). School transitions among military adolescents: A qualitative study of stress and coping. School Psychology Review, 39(1), 84–105. 10.1080/02796015.2010.12087792 [DOI] [Google Scholar]
- Briggs-Gowan, M. J., Carter, A. S., Moye Skuban, E., & McCue Horwitz, S. (2001). Prevalence of social-emotional and behavioral problems in a community sample of 1- and 2-year-old children. Journal of the American Academy of Child & Adolescent Psychiatry, 40(7), 811–819. 10.1097/00004583-200107000-00016 [DOI] [PubMed] [Google Scholar]
- Card, N. A., Bosch, L., Casper, D. M., Wiggs, C. B., Hawkins, S. A., Schlomer, G. L., & Borden, L. M. (2011). A meta-analytic review of internalizing, externalizing, and academic adjustment among children of deployed military service members. Journal of Family Psychology, 25(4), 508–520. 10.1037/a0024395 [DOI] [PubMed] [Google Scholar]
- Coldwell, J., Pike, A., & Dunn, J. (2006). Household chaos – Links with parenting and child behaviour. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 47(11), 1116–1122. 10.1111/j.1469-7610.2006.01655.x [DOI] [PubMed] [Google Scholar]
- De Pedro, K. M. T., Astor, R. A., Benbenishty, R., Estrada, J., Smith, G. R. D., & Esqueda, M. C. (2011). The children of military service members: Challenges, supports, and future educational research. Review of Educational Research, 81(4), 566–618. 10.3102/0034654311423537 [DOI] [Google Scholar]
- Deater-Deckard, K. (1998). Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice, 5(4), 314–332. 10.1111/j.1468-2850.1998.tb00152.x [DOI] [Google Scholar]
- Donnelly, R., & Patrinos, H. A. (2021). Learning loss during Covid-19: An early systematic review. Prospects, 51(4), 601–609. 10.1007/s11125-021-09582-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, W. E., Dumas, T. M., & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science, 52(3), 177. 10.1037/cbs0000215 [DOI] [Google Scholar]
- England, M. J., & Sim, L. J. (Eds.). (2009). Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. The National Academies Press. [PubMed] [Google Scholar]
- Evans, S., Mikocka-Walus, A., Klas, A., Olive, L., Sciberras, E., Karantzas, G., & Westrupp, E. M. (2020). From “it has stopped our lives” to “spending more time together has strengthened bonds”: The varied experiences of Australian families during COVID-19. Frontiers in Psychology, 11, 588667. 10.3389/fpsyg.2020.588667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert, J. M., Vitiello, B., Plener, P. L., & Clemens, V. (2020). Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14(1), 20. 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbe, A., Ogurlu, U., Logan, N., & Cook, P. (2020). COVID-19 and remote learning: Experiences of parents with children during the pandemic. American Journal of Qualitative Research, 4(3), 45–65. 10.29333/ajqr/8471 [DOI] [Google Scholar]
- Griffith, A. K. (2020). Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence, 1–7. 10.1007/s10896-020-00172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall, L. K. (2011). The importance of understanding military culture. Social Work in Health Care, 50(1), 4–18. 10.1080/00981389.2010.513914 [DOI] [PubMed] [Google Scholar]
- Joo, Y. S., & Lee, W. K. (2022). Impact of COVID-19-related stress on preschool children’s internalizing and externalizing problem behaviors: The indirect effect of mother’s depression and parenting behavior. Child Indicators Research, 15(6), 2093–2113. 10.1007/s12187-022-09946-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaca-Mandic, P., Georgiou, A., & Sen, S. (2021). Assessment to COVID-19 hospitalizations by race/ethnicity in 12 states. JAMA Internal Medicine, 181(1), 131–134. 10.1001/jamainternmed.2020.3857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazan, O., & Harris, A. (2020, September 3). What are parents supposed to do with their kids? The Atlantic. https://www.theatlantic.com/politics/archive/2020/09/limited-child-care-options-essential-workers/615931/
- Lester, P., Peterson, K., Reeves, J., Knauss, L., Glover, D., Mogil, C., Duan, N., Saltzman, W., Pynoos, R., Wilt, K., & Beardslee, W. (2010). The long war and parental combat deployment: Effects on military children and at-home spouses. Journal of the American Academy of Child & Adolescent Psychiatry, 49(4), 310–320. 10.1016/j.jaac.2010.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson, N. R., Freeman, J. Y. A., Rapee, R. M., Richardson, C. E., Oar, E. L., & Fardouly, J. (2020). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neece, C. L., Green, S. A., & Baker, B. L. (2012). Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities, 117(1), 48–66. 10.1352/1944-7558-117.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozbay, F., Johnson, D. C., Dimoulas, E., Morgan, C. A., Charney, D., & Southwick, S. (2007). Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry, 4(5), 35–40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2921311/ [PMC free article] [PubMed] [Google Scholar]
- Patrick, S. W., Henkhaus, L. E., Zickafoose, J. S., Lovell, K., Halvorson, A., Loch, S., Letterie, M., & Davis, M. M. (2020). Well-being of parents and children during the COVID-19 Pandemic: A national survey. Pediatrics, 146(4), e2020016824. 10.1542/peds.2020-016824 [DOI] [PubMed] [Google Scholar]
- Pearlin, L. I., & Schooler, C. (1978). The structure of coping. Journal of Health and Social Behavior, 19(1), 2–21. 10.2307/2136319 [DOI] [PubMed] [Google Scholar]
- Pew Research Center . (2020). Survey of U.S. adults conducted Oct. 13-19, 2020. https://www.pewresearch.org/fact-tank/2021/01/26/a-rising-share-of-working-parents-in-the-u-s-say-its-been-difficult-to-handle-child-care-during-the-pandemic/
- Pilkonis, P. A., Choi, S. W., Reise, S. P., Stover, A. M., Riley, W. T., & Cella, D., & on behalf of the PROMIS Cooperative Group . (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Racine, N., McAruthur, B. A., Cooke, J. E., Eircih, R., Zhu, J., & Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A Meta-analysis. JAMA Pediatrics, 175(11), 1142–1150. 10.1001/jamapediatrics.2021.2482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers, A. A., Ha, T., & Ockey, S. (2021). Adolescents’ perceived socio-emotional impact of COVID-19 and implications for mental health: Results from a U.S.-based mixed-methods study. Journal of Adolescent Health, 68(1), 43–52. 10.1016/j.jadohealth.2020.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruff, S. B., & Keim, M. A. (2014). Revolving doors: The impact of multiple school transitions on military children. The Professional Counselor, 4(2), 103–113. 10.15241/sbr.4.2.103 [DOI] [Google Scholar]
- Samji, H., Wu, J., Ladak, A., Vossen, C., Stewart, E., Dove, N., Long, D., & Snell, G. (2022). Review: Mental health impacts of the COVID-19 pandemic on children and youth – A systematic review. Child and Adolescent Mental Health, 27(2), 173–189. 10.1111/camh.12501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- song, S., Park, B., Lee, W. K., Park, N., & Kim, M. N. (2022). Examining the relationship between social support, parenting stress, and depression in South Korean single mothers. Journal of Child and Family Studies, 31(5), 1232–1245. 10.1007/s10826-021-02084-1 [DOI] [Google Scholar]
- Spinelli, M., Lionetti, F., Pastore, M., & Fasolo, M. (2020). Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Frontiers in Psychology, 11, 1713. 10.3389/fpsyg.2020.01713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steggerda, J. C., Cavell, T. A., Nicholson, J. H., Drew, A. L., Herrera, C., Gaffney, D., Slep, A. M. S., Lorber, M. F., & Spencer, R. (2022). Inventory of School Supports- Parent Report (ISS-PR): Development and preliminary validation with military connected-families. [Manuscript submitted for publication]. Department of Psychological Sciences, University of Arkansas. [Google Scholar]
- U.S. Department of Defense . (2022). Celebrating military children. https://www.defense.gov/Spotlights/Month-of-the-Military-Child/
- van Bakel, H., Bastiaansen, C., Hall, R., Schwabe, I., Verspeek, E., Gross, J. J., Brandt, J. A., Aguiar, J., Akgun, E., Arikan, G., Aunola, K., Bajgarová, Z., Beyers, W., Bílková, Z., Boujut, E., Chen, -B.-B., Dorard, G., Escobar, M. J., Furutani, K., … Roskam, I. (2022). Parental burnout across the globe during the COVID-19 pandemic. International Perspectives in Psychology: Research, Practice, Consultation, 11(3), 141–152. 10.1027/2157-3891/a000050 [DOI] [Google Scholar]
- van Loon, A. W. G., Creemers, H. E., Vogelaar, S., Miers, A. C., Saab, N., Westenberg, P. M., & Asscher, J. J. (2021). Prepandemic risk factors of COVID-19-related concerns in adolescents during the COVID-19 pandemic. Journal of Research on Adolescence, 31(3), 531–545. 10.1111/jora.12651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierhaus, M., Lohaus, A., Schmitz, A., & Schoppmeier, M. (2013). Relationships between maternal parenting stress and reports on children’s internalizing and externalizing problems: A cross-lagged structural equation model. Journal of Education and Developmental Psychology, 3(1), 39–50. 10.5539/jedp.v3n1p39 [DOI] [Google Scholar]
- Vogt, D. (2011). Mental health-related beliefs as a barrier to service use for military personnel and veterans: A review. Psychiatric Services, 62(2), 135–142. 10.1176/ps.62.2.pss6202_0135 [DOI] [PubMed] [Google Scholar]
- Wang, X., Cai, L., Qian, J., & Peng, J. (2014). Social support moderates stress effects on depression. International Journal of Mental Health Systems, 8(1), 41. 10.1186/1752-4458-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz, J. R., Vaugh-Coaxum, R. A., Evans, S. C., Thomassin, K., Hersh, J., Lee, E. H., Ng, M. Y., Lau, N., Raftery-Helmer, J. N., & Mair, P. (2020). Efficient monitoring of treatment response during youth psychotherapy: The behavior and feelings survey. Journal of Clinical Child & Adolescent Psychology, 49(6), 737–751. 10.1080/15374416.2018.1547973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westrupp, E. M., Bennett, C., Berkowitz, T., Youssef, G. J., Toumbourou, J. W., Tucker, R., Andrews, F. J., Evans, S., Teague, S. J., Karantzas, G. C., Melvin, G. M., Olsson, C., Macdonald, J. A., Greenwood, C. J., Mikocka-Walus, A., Hutchinson, D., Fuller-Tyszkiewicz, M., Stokes, M. A., Olive, L., & Sciberras, E. (2021). Child, parent, and family mental health and functioning in Australia during COVID-19: Comparison to pre-pandemic data. European Child & Adolescent Psychiatry. 10.1007/s00787-021-01861-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolley, M. E., Bowen, G. L., & Bowen, N. K. (2004). Cognitive pretesting and the developmental validity of child self-report instruments: Theory and applications. Research on Social Work Practice, 14(3), 191–200. 10.1177/1049731503257882 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, ALD, upon reasonable request.