Corresponding Author

Key words: health care, hospitalization, primary care, telemedicine, telephone visit
Telemedicine is a rapidly evolving field that offers novel opportunities for the outpatient management of heart failure (HF). It involves the use of telecommunications technology such as phone or video consultations, remote monitoring devices, and mobile health applications to remotely assess, monitor, and manage HF patients. These tools have the potential to maintain clinical stability, prevent HF exacerbations, and reduce overall morbidity and mortality.1,2 During the COVID-19 pandemic, the rapid development and widespread implementation of telemedicine programs were crucial as a safe and effective means of delivering care to HF patients while minimizing their risk of exposure to the virus.3 Indeed, recent meta-analyses of randomized trials showed a consistent benefit of such programs in preventing hospitalizations and reducing mortality in HF patients.4,5 However, most trials evaluated large, hospital-based, cardiologist- and HF nurse-led telemedicine programs, with very few occurring in a primary care setting. Since primary care physicians (PCPs) are usually patients’ first point of medical contact when HF symptoms arise, data on the real-world use of telemedicine-delivered primary care for HF patients is needed.
In this issue of JACC: Advances, Casey et al6 provide an important report on downstream health care utilization of telemedicine (either telephone or video) visits compared to in-person office visits in a primary care setting. They analyzed 3,902 primary care visits with a primary diagnosis of HF from January to December 2022, of which 58.4% utilized telemedicine (44.9% telephone, 13.5% video), and 41.6% were in-person. After adjusting for a comprehensive list of confounders and compared to in-person visits, telephone visits were associated with more in-person follow-up visits (adjusted odds ratio [aOR]: 1.51; 95% CI: 1.08-2.21) but fewer emergency department visits (aOR: 0.73; 95% CI: 0.55-0.97). Compared to in-person visits, there was no significant difference in 7-day all-cause hospitalizations following a telephone or video visit, although video visits were associated with fewer HF hospitalizations (aOR: 0.41, 95% CI: 0.20-0.84). Interestingly, regardless of visit modality, visits with a patient’s personal PCP were associated with a lower risk of downstream emergency department and hospital utilization compared to visits with another doctor. The authors conclude that telemedicine appears to offer safe alternatives to in-person care for HF-related primary care and is a promising health care delivery strategy.
The authors are to be congratulated for their efforts to better understand the implications of the extensive incorporation of telemedicine into clinical practice. This study offers a real-world, post-COVID-19 pandemic-era description of the use of telemedicine by HF patients in the primary care setting. Specifically, it provides insight on patient preferences as well as the safety and effectiveness of telemedicine as a valuable tool for caring for HF patients in primary care. Importantly, however, as highlighted by the authors, while interpreting the results of this study, it is necessary to consider some biases that are associated with the study design itself.
A notable selection bias is evident, whereby a specific patient population of certain acuity may have opted for a particular visit modality.6 Despite multiple adjustments, this is a very difficult factor to account for. As an example, sicker patients may be inclined to present for an in-person visit rather than a video visit, which may explain the finding that video visits are associated with fewer HF hospitalizations. In this regard, the lack of randomization prevents us from drawing a definitive conclusion on the effectiveness of telemedicine-delivered primary care compared to in-person care for preventing HF hospitalizations. Nonetheless, it does provide valuable information from which one can conclude that when HF patients autonomously select their follow-up modality, the approach is generally safe, yields acceptable results, and does not lead to excessive downstream health care utilization. This also highlights that the timing and mode of delivery (in-person vs telemedicine) should be personalized based on patient risk and the available care delivery options.1 Moreover, aligning with patients’ preferences on which visit modality to use may enhance patient compliance and improve the patient-provider relationship.
Another critical point to consider is the limited generalizability of this study to other health care settings. Widespread adoption and utilization of telemedicine are greatly dependent on the target population, socioeconomic status, health care infrastructure, and technology available to both patients and health care providers. As an example, elderly HF patients may find it challenging to utilize the required devices because of limited technologic expertise, cognitive dysfunction, or compromised eyesight and hearing.7 Alternatively, low-income groups or ethnic minorities may have limited access to certain technology, which may explain their previously described lower utilization rate of telemedicine.8 Although the population analyzed by Casey et al6 showed broad socioeconomic and ethnic diversity, the context of already integrated telemedicine, as stated by the authors, may have influenced the results, which may not necessarily be applicable to settings with limited telemedicine adoption. Finally, health care systems and their regulations vary between and within countries, meaning that there is no “one size fits all” model. These observations should be taken into consideration if one intends to initiate a telemedicine program in primary care for HF patients, along with the likely need for training both patients and providers.9
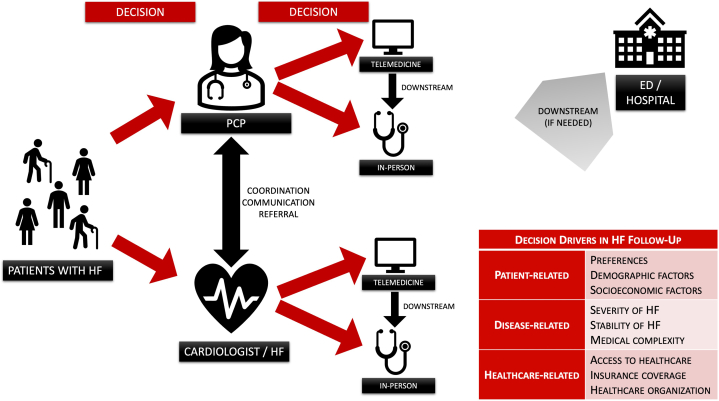
Despite these data reported by Casey et al,6 gaps of knowledge and uncertainties in the field of telemedicine-delivered primary care for HF patients remain. Firstly, there is a lack of robust randomized, controlled trial data in the primary care setting. To date, randomized, controlled trials and meta-analyses in this realm have mainly involved structured cardiologist or HF nurse-driven telemedicine programs rather than PCPs. Randomized trials evaluating clinical and economic outcomes between telemedicine-delivered vs in-person primary care and HF-specific structured telemedicine programs vs in-person HF specialist care are needed. Secondly, whether regular follow-up (telephone, video, or in-person) for HF patients is best provided by specialized HF teams, general cardiologists, or PCPs remains unclear, and this complex interaction demands attention. By overseeing patients’ multisystem comorbidities and their interaction with a HF diagnosis, PCPs may be better positioned to offer more holistic care. Further, owing to their longitudinal and long-term nature, PCPs have the benefit of establishing a solid provider-patient relationship that makes patients more likely to follow their advice, adhere to prescribed treatments, and seek timely medical attention when needed. Nonetheless, specialists’ care is equally as important as unique HF expertise is needed to identify HF progression that warrants referral for devices and advanced HF therapies. As such, the question of whether regular follow-up for HF patients is best provided by specialists or PCPs likely requires an intricate interplay of both, whereby effective communication between the PCP, the treating cardiologist or HF specialist, and the patient is paramount for shared decision-making and optimal patient care.10 Thirdly, customizing telemedicine initiatives to cater to the diverse needs of the individual patient, regardless of background, is crucial. Medical personnel and government health administrators ought to make a concerted effort to implement telemedicine programs that consider factors such as socioeconomic status, technological literacy, and cultural nuances to ensure equitable health care delivery. Lastly, decision drivers such as patient preferences and sociodemographic factors, medical complexity, and health care organization should be considered when formulating a follow-up plan for the individual HF patient. An ideal roadmap for the management of HF outpatients that incorporates telemedicine is proposed in Figure 1.
Figure 1.
Pathways and Decision Drivers in Outpatient Heart Failure Follow-Up
ED = emergency department; HF = heart failure; PCP = primary care physician.
In conclusion, telemedicine-delivered primary care models hold promise to revolutionize outpatient HF management. Such tools have the potential to maintain clinical stability, prevent HF exacerbations, and reduce overall morbidity and mortality. How to strategically integrate telemedicine into the continuum of traditional health care services is complex and warrants further study.
Funding support and author disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Heidenreich P.A., Bozkurt B., Aguilar D., et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American heart association Joint Committee on clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e263–e421. doi: 10.1016/j.jacc.2021.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Stevenson L.W., Ross H.J., Rathman L.D., Boehmer J.P. Remote monitoring for heart failure management at Home. J Am Coll Cardiol. 2023;81:2272–2291. doi: 10.1016/j.jacc.2023.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Tersalvi G., Winterton D., Cioffi G.M., et al. Telemedicine in heart failure during COVID-19: a Step into the Future. Front Cardiovasc Med. 2020;7 doi: 10.3389/fcvm.2020.612818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuan P.X., Chan W.K., Fern Ying D.K., et al. Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis. Lancet Digit Health. 2022;4:e676–e691. doi: 10.1016/S2589-7500(22)00124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholte N.T.B., Gürgöze M.T., Aydin D., et al. Telemonitoring for heart failure: a meta-analysis. Eur Heart J. 2023;44:2911–2926. doi: 10.1093/eurheartj/ehad280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casey S.D., Sax D.R., Mark D.G., et al. Similar rates of hospitalizations between telemedicine-delivered versus in-person primary care visits for chronic heart failure. JACC: Adv. 2024;3 [Google Scholar]
- 7.Tersalvi G., Gasperetti A., Schiavone M., et al. Acute heart failure in elderly patients: a review of invasive and non-invasive management. J Geriatr Cardiol. 2021;18:560–576. doi: 10.11909/j.issn.1671-5411.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hare A.J., Patel M.S., Volpp K., Adusumalli S. The Role of Behavioral economics in improving cardiovascular health Behaviors and outcomes. Curr Cardiol Rep. 2021;23:153. doi: 10.1007/s11886-021-01584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tersalvi G., Vicenzi M., Kirsch K., et al. Structured telephone support programs in chronic heart failure may be affected by a learning curve. J Cardiovasc Med. 2020;21:231–237. doi: 10.2459/JCM.0000000000000934. [DOI] [PubMed] [Google Scholar]
- 10.Morton G., Moore J. Systems of care for heart failure: bridging the divide between primary care and specialist services. Heart. 2023;109:1564–1570. doi: 10.1136/heartjnl-2022-321757. [DOI] [PubMed] [Google Scholar]