Background
Six billion people lack access to safe, timely, and affordable cardiac surgical care when needed. Nevertheless, cardiovascular diseases are the leading cause of morbidity and mortality, and an estimated one-third of this burden will require surgical or interventional care.1 This is exacerbated by the epidemiological transition away from communicable diseases and toward noncommunicable diseases: Ischemic heart disease affects younger populations in low- and middle-income countries (LMICs) compared to high-income countries (HICs), at ages when adults are their families’ primary caregivers and greatly contribute to their countries’ socioeconomic growth. Rheumatic heart disease is a disease of poverty affecting 30 to 40 million people worldwide, a number anticipated to only be the tip of the iceberg.1 Congenital heart disease is the most common major congenital anomaly with a relatively stable incidence worldwide, affecting 1 in every 100 live births.1 LMICs are estimated to reach over 2 billion children by 2050, projecting enormous burdens of congenital and rheumatic heart disease. In addition, neglected diseases among the world’s poorest populations, such as endomyocardial fibrosis and Chagas cardiomyopathy, present unique cardiac surgical challenges that remain poorly understood.
Access to cardiac surgery requires accessibility, capacity, quality, affordability, and acceptability. A lack of political prioritization, government spending on health care, and misconceptions regarding cardiac surgical care delivery have impeded global cardiac surgery scale-up. The cardiac surgical workforce, including nonsurgical members of heart teams, remains a notable rate-limiting factor: Qualified, multidisciplinary human resources for health care are indispensable to ensuring access and optimizing patient outcomes. Nevertheless, the long training pathways and diversity of heart teams severely limit cardiovascular care delivery worldwide and prevent rapid scaling of the global workforce.
Over 100 countries and territories lack cardiac surgeons
Although the majority of the world lives in LMICs, most surgeons practice in HICs.2 HICs have approximately 7.15 cardiac surgeons per million population compared to 0.04 in low-income countries. Similarly, there are 9.51 pediatric cardiac surgeons per million pediatric population in HICs compared to 0.07 in low-income countries. It remains unclear how many—or rather how few—nonsurgical cardiovascular health care professionals exist and where they are distributed, including (interventional) cardiologists, cardiac anesthesiologists, cardiac intensivists, perfusionists, technicians, and other health workers.
Further challenges exist. Women remain underrepresented in the surgical workforce. In the United States, 6% of cardiothoracic surgeons are women, whereas in Canada, 11% of cardiovascular surgeons are women.3 Representation in the global cardiac surgical workforce remains unknown; however, a review of the Cardiothoracic Surgery Network database suggests only 3.7% (5/135) of cardiac surgeons in sub-Saharan Africa are women. Women from minoritized populations are particularly underrepresented in HICs, whereas social, cultural, and other factors disproportionately prevent women from entering, remaining, and progressing in the LMIC workforce. Meanwhile, continued medical education, research capacity and support, and career progression opportunities are variable across and within countries. Countries with fewer surgeons, especially those with only 1 surgeon, cannot afford to temporarily lose their workforce, whereas online professional training and capacity-building-oriented visiting teams remain scarce. Lastly, rural and remote regions and island states face unique challenges due to low population densities and insufficient tertiary care capacity, requiring collaborations to develop regional centers and efficient referral networks.4
Regional perspectives
Here, we provide a brief overview of access to cardiac surgery through different regional perspectives and experiences, recognizing the need for greater nuance and understanding of issues at the country level.
The Asia-Pacific primarily struggles with vast geographical distances and sparse population densities. Currently, there is only 1 local cardiac surgeon for 12 million people across the region.4 Asia-Pacific island states have the world’s largest relative rheumatic heart disease burden, whereas other cardiovascular pathologies and risk factors, such as ischemic heart disease and diabetes, are rapidly rising.4 Traditionally, Asia-Pacific nations have collaborated to facilitate health care delivery, with recent political commitments to strengthen access to surgical health care through National Surgical, Obstetric, and Anesthesia Plans supported by the World Health Organization’s Western Pacific Regional Office and surgeons’ presence in governments.
Central and South America have high public insurance coverage although large private health care sectors are commonplace. There is great economic, cultural, and political variability between countries, whereas income inequality is consistently high (Gini index >40). Although there is a larger population in Central and South America than in North America (650 vs 370 million people), North America has 5.4 times as many cardiac surgeons (3,997 vs 747).2 In 2019, the Latin American Association of Cardiac and Endovascular Surgery was established to unite surgeons across Latin America and provide an accessible platform for professional development through educational videos, research collaborations, and capacity-building meetings. The association has partnered with other regional professional societies to facilitate exchange programs and continued medical education.
The Middle East and North Africa share linguistic, religious, and cultural heritage and possess several centers of excellence. Countries in the region are common training hubs (eg, Morocco and Egypt) although pathways remain ill-defined. In various countries, no dedicated training programs culminating in accreditation exist; rather, they commonly involve a “Masters in Surgery,” which is more research-oriented than clinically oriented. Several countries have been faced with conflict-induced political instability with direct effects on the funding, infrastructure, and accessibility of health care. For example, in Yemen, local cardiac surgical capacity is largely halted due to ongoing conflict and lack of supplies entering the country.
North America is faced with a concurrent relative abundance of capacity1 and disparities in access to care, whether due to financial (United States) or geographical barriers (Canada). Simultaneously, disparities exist because of structural barriers, systemic racism, and unconscious biases. In Europe, smaller health systems exist which minimize geographical barriers apart from the Nordic Countries, whereas universal health coverage models provide financial risk protection. However, the cultural and linguistic diversity, differential acceptance of and health care provision for immigrant populations, and political trends impose potential barriers to care that may trickle down on the workforce. Several countries (eg, Belgium, France, Germany) are common destinations for surgeons from LMICs to train and return home. Nevertheless, pathways to enter training are not always clear and transparent, limiting a clear pipeline to foster the global workforce.
South, Southeast, and East Asia are home to over half of the world’s population but only 19.4% of cardiac surgeons.2 Several centers in China and India perform the highest annual cardiac surgical volumes in the world.1 On the other end of the spectrum is the complete lack of local capacity: Bhutan, Brunei, Laos, and Timor-Leste have no local surgeons, whereas elsewhere, the capacity is incredibly low (eg, in Cambodia, 1 cardiac surgeon for 17 million people, and in Myanmar, 1 for 54 million).2
Sub-Saharan Africa has the lowest workforce density with 0.12 cardiac surgeons per million people.2 Few local training programs exist: Senior surgeons have commonly trained outside Africa, whereas younger surgeons have often trained in accredited programs in Northern Africa, South Africa, Ghana, or Kenya, with variable support. For example, surgeons training abroad in South Africa as “supernumary registrars” are often not paid and require their own or external funding. Without external support, the debt incurred by the end of training forces many to seek jobs in HICs to compensate, further exacerbating that many do not return home.
Way forward
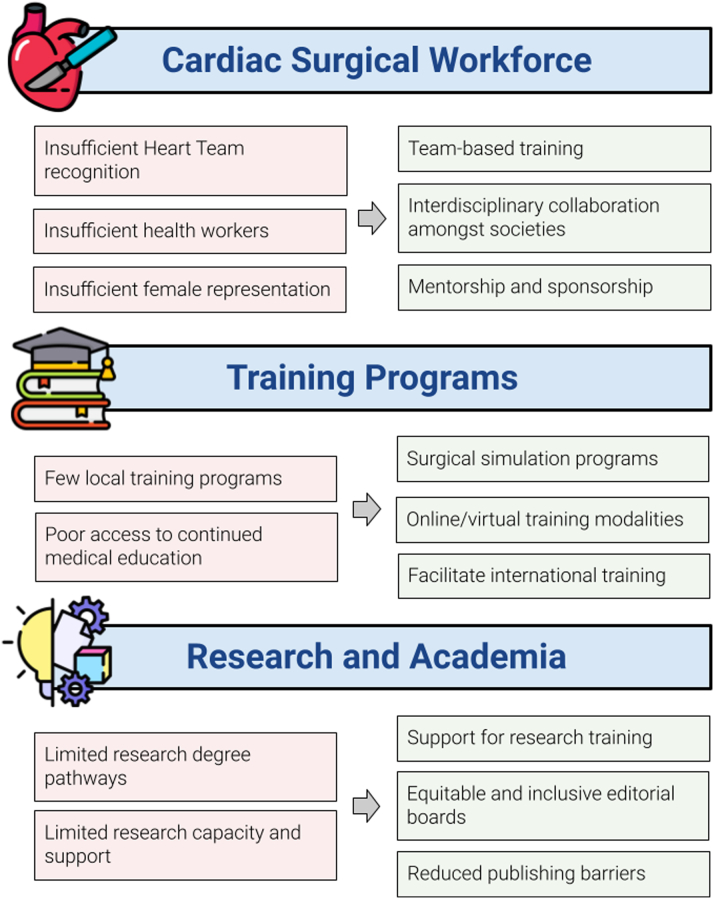
Scaling the global workforce requires attention in 3 common areas: education, research, and funding (Figure 1).
Figure 1.
Challenges and Solutions to Expanding the Global Cardiac Surgical Care Workforce
Scaling the cardiac surgical workforce, including nonsurgical members of the cardiovascular care continuum, requires careful attention for education, research, and funding. Challenges (red boxes) exist across the workforce spectrum, which may be partially addressed through the proposed solutions (green boxes). Solutions include a recognition of all health care professionals involved in the management of cardiac surgical conditions; increased and improved training pathways and modalities for cardiac surgeons and nonsurgeons; diversity, equity, and inclusion across cardiac surgery; research infrastructure and support; and more sustainable partnerships and financing.
Education
Cardiac surgery requires the expertise of multiple health care professionals. The “heart team” notion was created to facilitate clinical decision-making amid the burgeoning volume of interventional and surgical options and increasing patient complexity.5 It has since become the standard of care with Class I recommendations in the most recent coronary and valvular disease guidelines. Increasing access to cardiac surgery not only requires a cardiac surgeon but also anesthesiologists, cardiologists, intensivists, perfusionists, biomedical engineers, nutritionists, physiotherapists, and pharmacists. A heart team approach can be promoted through educational initiatives that are team-based as opposed to individual-based. The shortage of other team members must be taken as seriously as shortage of cardiac surgeons. Similar to surgeons, there is a stark disparity in the distribution of anesthesia providers and a limited understanding of how many are specialized in cardiac care. Steps should be taken to ensure heart team members learn to function as a team early on, ideally within the context where they work or will be working. In addition, particular efforts should be made to address structural barriers and (un)conscious biases in training and practice and to facilitate mentorship and sponsorship structures to enhance diversity, equity, and inclusion within the growing workforce.
Simulation training has emerged as a key component of training in HICs and LMICs.6 Low- and medium-fidelity simulators provide opportunities to develop more advanced skills in resource-limited settings where cardiac surgical training programs are still in their infancy. Innovations such as the GlobalSurgBox were designed to provide trainees with a user-friendly and low-cost means to gain surgical skills even with limited access to operating room settings. Moreover, the pandemic has emphasized the importance of simulation and virtual learning as traveling electives, fellowships, and educational initiatives have been halted.7 The technology platform Proximie combines artificial intelligence and higher-fidelity simulation to facilitate knowledge dissemination, connecting surgeons globally to operate or follow operations in real time via a shared virtual reality platform. Similarly, while online learning has evolved out of necessity due to COVID-19, its power to democratize knowledge and foster support networks between training programs cannot be overlooked and should be maintained far beyond the pandemic.8
Research and data
Global disparities in access to cardiac surgery remain insufficiently understood. More comprehensive data are required to define the most pressing gaps and understand how to best target advocacy efforts. Currently, there is no comprehensive global registry that tracks the number of cardiac centers, surgeons, caseloads, or outcomes, largely hindered by costs, political interests, and logistical challenges. If not globally, regional efforts should be encouraged to prioritize collecting population health data on the global cardiac surgical disease burden, (un)met need, and care capacity. This would inform policy plans, such as National Surgical, Obstetric, and Anesthesia Plans, and facilitate political prioritization. This may further inform cost-effective programs that facilitate earlier intervention and better outcomes. For example, congenital and rheumatic heart disease screening can be integrated into already existing robust primary health systems.
Programs must not only excel at patient care and facilitate education but also be supported to engage in research. Only a small proportion of peer-reviewed research is contributed by LMICs due to language and financial barriers, fewer regional journals, and insufficient research capacity and support. Although global cardiac surgery sessions now exist at all major conferences, professional societies and journals overwhelmingly comprise HIC representatives and are largely focused on smaller-scale efforts.9 Equitable representation in societies and journals’ editorial boards should be the norm, rather than the exception. Policies to detect and discourage “parachute” research (LMIC-based research without local authors) should be enforced by journals, such as involving local authors when conducting global surgical research. Finally, scholarships and grant funding should be allocated to support research degree (eg, MSc, PhD) tracks to enable more surgeons and trainees to pursue their academic ambitions.
Funding
Current funding structures, which rely greatly on foreign aid, philanthropy, and private sector funding, are unsustainable. Governmental funding is commonly earmarked, resulting in politicized spending on short-term initiatives that may not meet the needs of the local population or benefit population health at large. Donations, while not always earmarked, have a track record of poor fiscal returns, unsustainability, and insufficient auditing resulting in wasted resources. Instead, social finance may be pursued, which leverages governmental, nongovernmental, or private capital with the stipulation that certain social and/or economic goals are met. Given that existing financing is, at best, inconsistent and, at worst, wasteful, innovative financing instruments to scale cardiac surgical capacity must be explored.
Conclusions
Cardiovascular diseases are the leading cause of morbidity and mortality, yet political prioritization and awareness to expand the cardiac surgical workforce remain limited. Clear ways forward exist to foster and strengthen heart teams across countries with considerable socioeconomic returns on investment; failing to move forward means that millions of people will continue to die from preventable and treatable cardiac surgical conditions year after year.
Funding support and author disclosures
Dr Vervoort is supported by the Canadian Institutes of Health Research (CIHR) Vanier Canada Graduate Scholarship. All other authors have no disclosures. No funding received.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Vervoort D., Swain J.D., Pezzella A.T., Kpodonu J. Cardiac surgery in low- and middle-income countries: a state-of-the-art review. Ann Thorac Surg. 2021;111(4):1394–1400. doi: 10.1016/j.athoracsur.2020.05.181. [DOI] [PubMed] [Google Scholar]
- 2.Vervoort D., Meuris B., Meyns B., Verbrugghe P. Global cardiac surgery: access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 2020;159:987–996.e6. doi: 10.1016/j.jtcvs.2019.04.039. [DOI] [PubMed] [Google Scholar]
- 3.Gao S.W., Forcillo J., Watkins A.C., et al. 60 Years after the first woman cardiac surgeon: we still need more women in cardiac surgery. CJC Open. 2021;3:S89–S94. doi: 10.1016/j.cjco.2021.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vervoort D., Vinck E.E., Tiwari K.K., Tapaua N. Cardiac surgery and small island states: a bridge too far? Ann Thorac Surg. 2021;111(3):931–936. doi: 10.1016/j.athoracsur.2020.05.150. [DOI] [PubMed] [Google Scholar]
- 5.Holmes D.R., Jr., Rich J.B., Zoghbi W.A., Mack M.J. The heart team of cardiovascular care. J Am Coll Cardiol. 2013;61:903–907. doi: 10.1016/j.jacc.2012.08.1034. [DOI] [PubMed] [Google Scholar]
- 6.Lin Y., Han J.J., Kelly J.J., Gergen A.K., Downs E. Development of a modular and equitable surgical simulator. Global Health: Science and Practice 2022. https://www.ghspjournal.org/content/early/2022/06/03/GHSP-D-21-00744 [DOI] [PMC free article] [PubMed]
- 7.Vervoort D., Dearani J.A., Starnes V.A., Thourani V.H., Nguyen T.C. Brave new world: virtual conferencing and surgical education in the COVID-19 era. J Thorac Cardiovasc Surg. 2021;161(3):748–752. doi: 10.1016/j.jtcvs.2020.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das T.M., Kaur G., Nematollahi S., et al. Medical education in the digital era—a new paradigm for acquiring knowledge and building communities. JACC Adv. 2022;1:100031. [Google Scholar]
- 9.Guetter C.R., Vervoort D., Luc J.G.Y., Ouzounian M. Female and country representation on editorial boards of cardiothoracic surgery journals. Semin Thorac Cardiovasc Surg. Published online August 26, 2021 doi: 10.1053/j.semtcvs.2021.08.015. [DOI] [PubMed] [Google Scholar]