Abstract
Background
Patients with heart failure (HF) are a medically complex population with frequent hospitalizations. Downstream health care utilization following primary care delivered by telemedicine compared to in-person is unknown.
Objectives
The purpose of this study was to understand differences in return in-person visits, emergency department (ED) encounters, and hospitalizations following a telemedicine vs an in-person primary care visit for patients with HF seen for a HF-related complaint.
Methods
This was an observational study of all primary care visits for HF from January 1, 2022, to December 31, 2022, in an integrated health care delivery system. We compared 7-day in-person follow-up visits, ED visits, and hospitalizations (all-cause and HF-specific) by index visit type.
Results
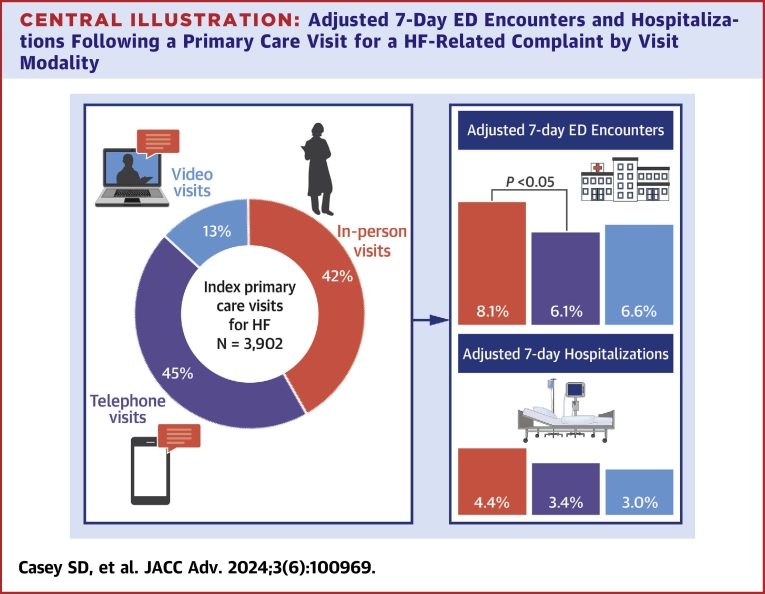
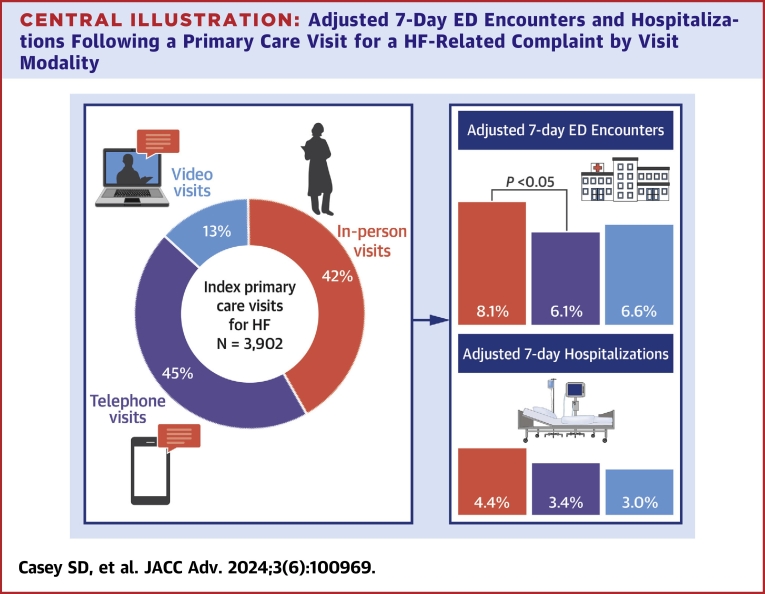
We included 3,902 primary care visits with a primary diagnosis of HF. Most visits utilized telephone or video visits (58.4% total; 44.9% telephone, 13.5% video). After adjustment, telephone visits were associated with more in-person follow-up visits (6.14% vs 4.20%; adjusted OR: 1.08-2.21; P < 0.05) but fewer ED visits (6.12% vs 8.07%; adjusted OR: 0.55-0.97; P < 0.05) compared to in-person visits. Most hospitalized patients (74%) had an admitting diagnosis of HF. There was no difference between 7-day all-cause hospitalization following telephone or video visits compared to in-person visits.
Conclusions
Most patients used telemedicine to address HF-specific primary care concerns. Telephone visits were associated with slightly higher short-term in-person primary care follow-up but lower ED utilization. Overall, downstream ED visits and hospitalizations were low. Telephone and video visits appear to offer safe alternatives to in-person care for HF-related primary care and are a promising health care delivery strategy
Key words: heart failure, primary care, telemedicine
Central Illustration
Patients with heart failure (HF) are a medically and socially complex population with high rates of hospitalization and mortality.1 Total annual health care costs attributed to HF are estimated to reach $70 billion by 2030, driven mainly by hospitalization costs.2,3 The clinical course of HF is marked by frequent exacerbations that prompt hospitalizations, and early primary care intervention for HF-related concerns is an opportunity to modify risk.
Accumulating evidence suggests that the SARS-CoV-2 pandemic disproportionately affects vulnerable populations including patients with HF.4, 5, 6 Telemedicine emerged during this period as a safe and convenient vehicle for health care delivery and persists in the post-pandemic period.7 Telemedicine-delivered primary care using telephone or video visits may improve outcomes by lowering barriers to access and offering a convenient option that may eliminate disincentives to seeking care.8,9 Video visits offer a face-to-face conversation that may better foster a physician-patient relationship but is associated with technical requirements and sociodemographic use disparities.10, 11, 12
The primary care setting is a cornerstone of outpatient HF management. However, telemedicine-delivered general primary care’s role in caring for patients with HF is incompletely understood, with most studies to date focusing instead on remote monitoring, nurse-led interventions, or postdischarge readmission prevention programs.13 While many of these studies show promise, the results are not generalizable to the routine primary care of patients with HF. Recently, work by Sammour et al14 found no increase in downstream emergency department (ED) visits or mortality following a transition from an in-person model to a telemedicine-based model for patients with HF in 2020, early in the SARS-CoV-2 pandemic. However, more ongoing evidence is needed to determine whether telemedicine is a safe and effective method of primary care delivery for this high-risk population.
The purpose of this study was to evaluate the safety and downstream acute care utilization of telephone or video visits compared to in-person office visits in a primary care setting. We analyzed automated electronic health record data from a large integrated delivery system 2 years after the beginning of the SARS-CoV-2 pandemic to compare telemedicine and in-person HF-related primary care for patients over a 1-year period. We investigated whether patients were more likely to require follow-up in-person office visits, ED visits, or hospitalizations (all-cause and hospitalizations due to HF) following a telemedicine vs an in-person visit. A secondary outcome examined downstream care utilization for patients whose primary care appointment was with their own personal primary care physician (PCP) compared to a physician unknown to them.
Methods
Study setting
In this cohort study, we examined primary care visits in the large, integrated health care delivery system of Kaiser Permanente Northern California, whose >4.5 million members represent the surrounding racial, ethnic, and socioeconomic diversity of northern California.15 The institutional review board of the Kaiser Foundation Research Institute approved the study protocol and materials and waived the requirement for written informed consent for participants because the study used deidentified data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines.16
All clinicians in the study setting have had access to video visit technology since 2014. Since 2016, patients who schedule a primary care appointment through the patient portal have been required to choose their visit type preference (in-person, video, or telephone visit). Patients can choose to see their own personal PCP. However, if their personal PCP is unavailable, they can elect to see another physician with availability at the time of appointment scheduling. After an initial SARS-CoV-2 pandemic emergency period during which telemedicine became the first line of contact between patients and primary care providers, in-person office visits returned to full availability for primary care appointments in April 2021, along with continued availability of telephone and video visit appointments. The scheduling availability and physicians available were comparable across visit types, with appointment availability generally within 3 days (often available the same day).
Study sample and measures
We identified index primary care visits with PCPs between January 1, 2022, and December 31, 2022, using the electronic health record and health system automated data sources. We included in-person office visits, video visits, and telephone visits with a HF-related diagnosis, including the following International Classification of Diseases-10th Revision diagnoses: I09.81, I11.0, I13.0, I13.2, I50.0, I50.1, I50.2, I50.3, I50.4, I50.8, and I50.9. We excluded visits from the study if the patient had any prior visit (outpatient, ED encounter, or hospitalization) within the previous 14 days to capture distinct care-seeking episodes. To measure short-term follow-up health care utilization outcomes, we extracted all in-person primary care office visits, ED visits, and hospitalizations that occurred within 7 days of the index encounter. We identified both all-cause hospitalizations and hospitalizations with an admitting diagnosis of HF using the same International Classification of Diseases Tenth Revision diagnoses as above.
Statistical analysis
We used multivariable logistic regression to examine the association between index visit type (in-person, video, or telephone visit) and outcomes, with a separate model for each outcome. All models were adjusted for patient age, sex, race/ethnicity, lower neighborhood socioeconomic status (at least 20% of households have household incomes below the federal poverty level or at least 25% of residents 25 years or older have less than a high school education in the Census block group), preferred language for health care, lower neighborhood internet access (no more than 80% of households have a residential fixed high-speed connection with at least 10 Mbps downstream and at least 1 Mbps upstream in the Census tract based on Federal Communications Commission data), driving distance from home to primary care facility, whether there is a fee for facility parking, whether the patient has a proxy for patient portal access, day the appointment was made (weekday vs weekend), visit day (Monday through Thursday vs Friday through Sunday), visit time (AM vs PM), number of days between appointment booking and visit, any mobile portal use in the prior 365 days, any video visits in the prior 365 days, whether the clinician was the patient’s own primary care clinician, any ED visit in the prior 365 days, any hospitalization in the prior 365 days, Elixhauser score, calendar month and medical center. Standard errors were adjusted for the repeated visits among patients by clustering observations by patient with a robust variance estimator. For easier interpretation, we calculated adjusted rates of each outcome by index visit type via marginal standardization by using Stata’s margins postestimation command.17
In the study setting, patients with an ejection fraction <50% are often enrolled in chronic disease management programs and receive routine care and frequent contact from multiple services. To examine the effects that these care exposures may have had on our results, we performed a sensitivity analysis, excluding patients with an ejection fraction <50% (Supplemental Table 1). All analyses were conducted using 2-sided tests for significance with P < 0.05 as the threshold for significance using Stata version 17.0 (STATA Corp).
Results
There were 3,902 primary care visits with a primary diagnosis of HF in our study corresponding to 3,320 patients (1.18 visits per patient) (Table 1). Of these, 81.6% were ≥65 years old, 56.1% were male, 15.3% were Asian, 11.4% were Black, 14.0% were Hispanic, and 56.8% were White. In total, 22.6% of patients lived in lower socioeconomic status neighborhoods. Most primary care visits were conducted using telephone or video (58.4% total; 44.9% telephone, 13.5% video), including those ≥65 years of age (58.0% total; 45.2% telephone, 12.8% video). There were more telephone and video visits than in-person visits among female patients (63% total; 47.6% telephone, 15.4% video) and black patients (64.9% total; 50.1% telephone, 14.8% video).
Table 1.
Baseline Characteristics of Patients With HF Who Had Primary Care Visits During the Study Period
| All (N = 3,902) | In-Person Office Visit (n = 1,625, 41.6%) | Telephone Visit (n = 1,751, 44.9%) | Video Visit (n = 526, 13.5%) | |
|---|---|---|---|---|
| Demographics | ||||
| Age group | ||||
| 18-44, y | 91 (2.3) | 30 (1.9) | 39 (2.2) | 22 (4.2) |
| 45-64, y | 626 (16) | 260 (16) | 271 (15.5) | 95 (18.1) |
| 65-74, y | 753 (19.3) | 300 (18.5) | 347 (19.8) | 106 (20.2) |
| >74, y | 2,432 (62.3) | 1,035 (63.7) | 1,094 (62.5) | 303 (57.6) |
| Sex | ||||
| Female | 1,711 (43.9) | 633 (39) | 814 (46.5) | 264 (50.2) |
| Race/ethnicity | ||||
| White | 2,216 (56.8) | 940 (57.9) | 1,006 (57.5) | 270 (51.3) |
| Black | 445 (11.4) | 156 (9.6) | 223 (12.7) | 66 (12.6) |
| Hispanic | 548 (14) | 237 (14.6) | 240 (13.7) | 71 (13.5) |
| Asian | 596 (15.3) | 244 (15) | 247 (14.1) | 105 (20) |
| Other | 97 (2.5) | 48 (3) | 35 (2) | 14 (2.7) |
| Neighborhood SES | ||||
| Low | 883 (22.6) | 370 (22.8) | 404 (23.1) | 109 (20.7) |
| Unknown | 167 (4.3) | 71 (4.4) | 76 (4.3) | 20 (3.8) |
| Neighborhood internet | ||||
| ≤80% | 1,306 (33.5) | 563 (34.7) | 582 (33.2) | 161 (30.6) |
| Unknown | 115 (3) | 50 (3.1) | 54 (3.1) | 11 (2.1) |
| Language | ||||
| English | 3,526 (90.4) | 1,435 (88.3) | 1,600 (91.4) | 491 (93.4) |
| Visit characteristics | ||||
| Visit with own PCP | 3,385 (86.8) | 1,438 (88.5) | 1,485 (84.8) | 462 (87.8) |
| Previous video visit use | 1,617 (41.4) | 554 (34.1) | 690 (39.4) | 373 (70.9) |
| Mobile app access | 2,081 (53.3) | 796 (49) | 924 (52.8) | 361 (68.6) |
| Travel time to facility | ||||
| ≤10 min | 1,538 (39.4) | 664 (40.9) | 664 (37.9) | 210 (39.9) |
| 10–20 min | 1,659 (42.5) | 682 (42) | 762 (43.5) | 215 (40.9) |
| >20 min | 686 (17.6) | 270 (16.6) | 319 (18.2) | 97 (18.4) |
| Unknown | 19 (0.5) | 9 (0.6) | 6 (0.3) | 4 (0.8) |
| Paid parking | ||||
| Yes | 374 (9.6) | 143 (8.8) | 176 (10.1) | 55 (10.5) |
| Health care proxy | ||||
| Yes | 265 (6.8) | 120 (7.4) | 102 (5.8) | 43 (8.2) |
| Days between booking and visit | ||||
| 0 d | 646 (16.6) | 191 (11.8) | 394 (22.5) | 61 (11.6) |
| 1 d | 489 (12.5) | 162 (10) | 262 (15) | 65 (12.4) |
| 2-7 d | 1,398 (35.8) | 500 (30.8) | 652 (37.2) | 246 (46.8) |
| Past medical/utilization history | ||||
| ≥1 ED visit in prior year | 2,462 (63.1) | 947 (58.3) | 1,167 (66.7) | 348 (66.2) |
| ≥1 Hospitalization in prior year | 1,464 (37.5) | 500 (30.8) | 718 (41) | 246 (46.8) |
| Elixhauser score | 11 (7-17) | 11 (7-16) | 10 (6-17) | 9 (3-17) |
Values are n (%) or median (IQR).
ED = emergency department; HF = heart failure; IQR = interquartile range; PCP = primary care physician; SES = socioeconomic status.
Approximately 30% of primary care visits occurred within 1 day of patient booking, although this rate was considerably higher for patients who booked telephone visits compared to office visits (37% vs 22%). Within 7 days following their initial primary care visit, 268 (6.9%) patients had an ED visit, and 143 (3.7%) were hospitalized. Among hospitalizations, 74% had an admitting diagnosis of HF. Patients seen by their personal PCP were less likely to have had a 7-day ED visit compared to patients who saw any other PCP (P = 0.021).
After adjustment, telephone visits were statistically significantly associated with more in-person primary care follow-up visits within 7 days (6.14% vs 4.20%; adjusted odds ratio [aOR]: 1.51; 95% CI: 1.08-2.21; P < 0.05) but fewer downstream ED visits within 7 days (6.12% vs 8.07%; aOR 0.73; 95% CI: 0.55-0.97; P < 0.05) compared to in-person visits (Table 2; Central Illustration). There was no statistically significant association between the likelihood of a 7-day all-cause hospitalization following a telephone or video visit compared to an in-person visit, although video visits were associated with fewer HF-specific hospitalizations (1.56% vs 3.64%; aOR: 0.41; 95% CI: 0.20-0.84; P < 0.05) than in-person visits. A sensitivity analysis that excluded patients with HFrEF was consistent with the results derived from the full cohort (Supplemental Table 1).
Table 2.
Short-Term Health Care Utilization Following Index Primary Care Visit Adjusted for Sociodemographic, Clinical, and Hospital Characteristics
| Visit Type | Adjusted % | OR | 95% CI | |
|---|---|---|---|---|
| 7-d PCP in-person visit | In-person | 4.20% | ||
| Telephone | 6.14% | 1.51 | 1.08-2.12 | |
| Video | 4.20% | 1.00 | 0.59-1.70 | |
| 7-d ED visit | In-person | 8.07% | ||
| Telephone | 6.12% | 0.73 | 0.55-0.97 | |
| Video | 6.56% | 0.79 | 0.51-1.22 | |
| 7-d hospitalization | In-person | 4.39% | ||
| Telephone | 3.38% | 0.75 | 0.51-1.11 | |
| Video | 2.95% | 0.65 | 0.36-1.17 | |
| 7-d HF-specific hospitalization | In-person | 3.64% | ||
| Telephone | 2.42% | 0.65 | 0.41-1.02 | |
| Video | 1.56% | 0.41 | 0.20-0.84 |
The full cohort of patients (N = 3,902) was included in the model for the 7-day PCP in-person visit. Nineteen patients with unknown travel times to their primary care facility were dropped from models for a 7-day ED visit, hospitalization, or HF-specific hospitalization, as these patients did not have a 7-day ED visit or hospitalization.
ED = emergency department; HF = heart failure; OR = odds ratio; PCP = primary care physician.
Central Illustration.
Adjusted 7-Day ED Encounters and Hospitalizations Following a Primary Care Visit for a HF-Related Complaint by Visit Modality
∗Indicates statistically significantly different compared to in-person visit comparison group. ED = emergency department; HF = heart failure.
Discussion
In this retrospective study of patients with a HF-related complaint in a large integrated health system late in the SARS-CoV-2 pandemic and early postpandemic time period, we found overall low rates of downstream ED and hospital utilization regardless of index visit type. We found telephone visits were associated with more downstream in-person office visits but fewer ED visits when compared to in-person office visits. Video visits were associated with fewer 7-day hospitalizations with an admitting diagnosis of HF compared to in-person visits. Lastly, visits with a patient’s personal PCP, regardless of visit modality, were associated with a lower risk of downstream ED and hospital utilization compared to visits with any other PCP. To our knowledge, this is the largest study of patients with HF comparing outcomes for telephone and video visits vs in-person primary care visits.
Patients more frequently utilized telephone or video visits (58.4%) than in-person care for evaluation of HF-related complaints during the study period, which included both the late pandemic and postpandemic time periods. A prepandemic study in our health system of more than 2 million primary care visits found that telephone or video delivered only 14% of all general primary care visits; thus, our current results indicate a marked change in care delivery.11 Increased barriers to in-person visits, fear of exposure to infection, and national telemedicine promotion may have contributed to this trend.18,19 Our study suggests that telemedicine is a viable adjunct to in-person care for patients with HF. Telemedicine may be especially effective for patients with HF by eliminating transportation and mobility barriers as well as facilitating prompt access to primary care. This is an important finding, given the projected rise in the global burden of HF.13,20
Telephone visits were associated with slightly lower downstream ED use compared to office visits and slightly higher rates of in-person follow-up, suggesting that they are likely safe and may be an effective way to triage or risk stratify patients who need in-person evaluation. Patients who booked telephone visits were more likely to be seen in 0 to 1 days, suggesting telephone visits may provide early access to manage more urgent needs. Telephone visits were also associated with fewer downstream ED visits, consistent with a previous study in our health system that included over 1 million primary care visits across all visit types.21 This finding may be due to effective triage practices by PCPs in identifying which patients would benefit from a face-to-face interaction following their index telephone visit. In contrast, our study noted that in-person and video visits prompted similar magnitudes of 7-day in-person follow-up visits, likely reflecting the benefits of face-to-face interactions. Potential advantages include the provision of clinically useful information and the establishment and maintenance of rapport.12,22, 23, 24 Taken together, our results suggest that telephone and video visits may be comparable alternatives to in-person HF primary care in preventing clinical deterioration requiring an ED visit or hospitalization.
We found no significant association between visit type and the risk of short-term hospitalization. Most hospitalized patients in our study (74%) had a primary admitting diagnosis of HF, suggesting an association between the index primary care encounter and HF symptoms requiring a higher level of care. We did find that patients who had a video visit had a lower risk of HF-hospitalization compared to those who had an in-person visit, suggesting that this telemedicine modality may be a safe alternative for managing symptoms of HF. Most (85%) of visits included in our study were with patients’ own PCPs, and more studies are needed to understand the effect of a known PCP compared to an unknown PCP on downstream health care utilization.25
Our results contrast with recent literature reports showing increased downstream health care utilization associated with telemedicine. Sammour et al14 recently found that a telemedicine-based model for HF specialty care was associated with higher mortality and intensive care unit admission at 90 days compared to in-person visits. Kalwani et al26 found that visits for newly diagnosed HF delivered by telemedicine were associated with an increased need for return primary care visits compared to visits that were conducted in-person. However, our results cannot be directly compared to these studies, as the patients included in our study were seen by general PCPs and not part of HF specialty care teams.
Study Limitations
While we collected a wide range of covariates, including demographic, technological, and geographical characteristics previously demonstrated to be associated with telemedicine use and outcomes, we are unable to adjust for all potential confounders, such as patients’ self-selection of visit type based on acuity or other factors. Due to the observational nature of our study, our results cannot be interpreted as causal. This study was conducted in a large integrated health care setting where video and telephone telemedicine were already widely available before the pandemic, and the findings may not directly generalize to other settings with less robust telemedicine infrastructures. We are unable to account for visit availability (in-person vs telephone vs video visit) at the time of booking, and we were only able to examine what visit type was ultimately scheduled. Health care utilization following the initial primary care visit was measured over a 7-day follow-up window but was not stratified by elapsed time from the index visit. It is not certain if these downstream visits were related to the initial chief complaint precipitating the index visit or if it was a new, unrelated health concern. However, the fact that 74% of associated hospitalizations had an admitting diagnosis of HF suggests that many ED visits and hospitalizations were likely related to worsening HF symptoms.
Conclusions
In this study of primary care visits for a HF-related concern, most primary care visits for patients with HF-related complaints during 2022 to 2023 were conducted via telemedicine. Overall, downstream ED utilization and hospitalization rates were low and relatively comparable across visit modalities. Telephone visits were followed by slightly higher follow-up office visits than patients who were originally seen in office visits. Video or telephone visits may be a viable ongoing method of primary care delivery for patients with HF in the post-SARS-CoV-2 pandemic era, although more studies are needed.
PERSPECTIVES.
COMPETENCY IN MEDICAL KNOWLEDGE: The safety and quality of telemedicine-delivered primary care to patients with HF are incompletely understood.
COMPETENCY IN PATIENT CARE: Patients with HF are a medically and socially complex population. Telemedicine may remove barriers to primary care in this population and improve care.
TRANSLATIONAL OUTLOOK 1: Telemedicine-delivered primary care is not associated with more downstream ED encounters or hospitalizations compared to in-person visits for HF patients seen for a HF-related complaint.
TRANSLATIONAL OUTLOOK 2: Telemedicine may offer a safe alternative to in-person care for HF-related concerns and is a promising health care delivery strategy.
Funding support and author disclosures
The project was supported by a grant (R01HS25189) from the Agency for Healthcare Research and Quality. Dr Casey has received funding from The Permanente Medical Group (TPMG) Delivery Science Fellowship Program and has nothing to disclose. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental table, please see the online version of this paper.
Supplementary data
References
- 1.Storrow A.B., Jenkins C.A., Self W.H., et al. The burden of acute heart failure on U.S. Emergency Departments. J Am Coll Cardiol HF. 2014;2(3):269–277. doi: 10.1016/j.jchf.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go A.S., Mozaffarian D., Roger V.L., et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidenreich P.A., Albert N.M., Allen L.A., et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zuin M., Rigatelli G., Bilato C. Excess of heart failure-related deaths during the 2020 COVID-19 pandemic in Unites States. Heart Lung. 2023;58:104–107. doi: 10.1016/j.hrtlng.2022.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reza N., DeFilippis E.M., Jessup M. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circ Heart Fail. 2020;13(5) doi: 10.1161/CIRCHEARTFAILURE.120.007219. [DOI] [PubMed] [Google Scholar]
- 6.Wu J., Mamas M.A., Mohamed M.O., et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107(2):113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 7.New HHS study shows 63-fold increase in medicare telehealth utilization during the pandemic. Centers for Medicare & Medicaid Services. https://www.cms.gov/newsroom/press-releases/new-hhs-study-shows-63-fold-increase-medicare-telehealth-utilization-during-pandemic
- 8.Ray K.N., Chari A.V., Engberg J., Bertolet M., Mehrotra A. Disparities in time spent seeking medical care in the United States. JAMA Intern Med. 2015;175(12):1983–1986. doi: 10.1001/jamainternmed.2015.4468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reed M.E., Huang J., Parikh R., et al. Patient-Provider video telemedicine integrated with clinical care: patient experiences. Ann Intern Med. 2019;171(3):222–224. doi: 10.7326/m18-3081. [DOI] [PubMed] [Google Scholar]
- 10.Eberly L.A., Kallan M.J., Julien H.M., et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed M.E., Huang J., Graetz I., et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.5873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang J.E., Lindenfeld Z., Albert S.L., et al. Telephone vs. video visits during COVID-19: safety-net provider perspectives. J Am Board Fam Med. 2021;34(6):1103–1114. doi: 10.3122/jabfm.2021.06.210186. [DOI] [PubMed] [Google Scholar]
- 13.Kirakalaprathapan A., Oremus M. Efficacy of telehealth in integrated chronic disease management for older, multimorbid adults with heart failure: a systematic review. Int J Med Inf. 2022;162 doi: 10.1016/j.ijmedinf.2022.104756. [DOI] [PubMed] [Google Scholar]
- 14.Sammour Y., Spertus J.A., Austin B.A., et al. Outpatient management of heart failure during the COVID-19 pandemic after adoption of a telehealth model. J Am Coll Cardiol HF. 2021;9(12):916–924. doi: 10.1016/j.jchf.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis A.C., Voelkel J.L., Remmers C.L., Adams J.L., McGlynn E.A. Comparing Kaiser Permanente members to the general population: implications for generalizability of research. Perm J. 2023;27(2):87–98. doi: 10.7812/TPP/22.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vandenbroucke J.P., von Elm E., Altman D.G., et al. Strengthening the reporting of observational studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10) doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. STATA J. 2012;12(2):308–331. [Google Scholar]
- 18.Ward K., Vagholkar S., Sakur F., Khatri N.N., Lau A.Y.S. Visit types in primary care with telehealth use during the COVID-19 pandemic: systematic review. JMIR Med Inform. 2022;10(11) doi: 10.2196/40469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorst S.L., Armitage C.J., Brownsell S., Hawley M.S. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: a systematic review. Ann Behav Med. 2014;48(3):323–336. doi: 10.1007/s12160-014-9607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Virani S.S., Alonso A., Aparicio H.J., et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 21.Reed M., Huang J., Graetz I., Muelly E., Millman A., Lee C. Treatment and follow-up care associated with patient-scheduled primary care telemedicine and in-person visits in a large integrated health system. JAMA Netw Open. 2021;4(11) doi: 10.1001/jamanetworkopen.2021.32793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hammersley V., Donaghy E., Parker R., et al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract. 2019;69(686):e595–e604. doi: 10.3399/bjgp19X704573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rush K.L., Howlett L., Munro A., Burton L. Videoconference compared to telephone in healthcare delivery: a systematic review. Int J Med Inf. 2018;118:44–53. doi: 10.1016/j.ijmedinf.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Donaghy E., Atherton H., Hammersley V., et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 2019;69(686):e586–e594. doi: 10.3399/bjgp19X704141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daniel H., Sulmasy L.S., Health, Public Policy Committee of the American College of Physicians Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. 2015;163(10):787–789. doi: 10.7326/M15-0498. [DOI] [PubMed] [Google Scholar]
- 26.Kalwani N.M., Koos H., Oesterle A., et al. Impact of telemedicine new patient visits on total visit utilization at an academic cardiovascular center: an instrumental variable analysis. Circulation. 2022;146(Suppl_1) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.