Corresponding Author
Key words: cardiovascular diseases, health disparity, healthy lifestyle, smartphone, telemedicine
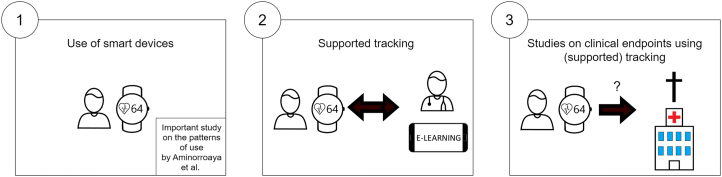
Smart devices such as smartphones and smartwatches are increasingly used for digital health solutions to manage diseases and track health goals.1 The expansion of digital health solutions and the number of vendors emerged particularly during the COVID-19 pandemic.2, 3, 4 Benefit of these solutions is often expected through increased health awareness, patient engagement, or early diagnosis and detection of disease deterioration. Presently there are no concrete guidelines from the American College of Cardiology, American Heart Association, or European Society of Cardiology on how to use, interpret or act on information from digital health solutions. Before adoption to routine clinical practice, 3 important steps should be made (see Figure 1): 1) general availability of digital health solutions for everybody; 2) supported and sustained use; and 3) evidence of its impact on clinical outcome and quality of life. The paper of Aminorroaya et al5 in this issue of JACC: Advances describes an important observation in view of the first step of general implementation of digital health solutions.
Figure 1.
Sequential Steps for a Successful Deployment of Digital Health Solutions
Step 1: patterns of use of digital health solutions
It is imperative to understand the uptake patterns of digital health solutions to enable the application of novel technologies in routine health care, because the current use patterns reveal the gaps and the readiness of the population to adopt these solutions. Aminorroaya et al5 performed a cross-sectional study using self-reported tracking of health-related goals using the Health Information National Trends Survey for 2017 to 2020. Health Information National Trends Survey is a long standing national project with extensive output for many years. The strength lies in the number of participants studied. The authors concluded that only 2 in 5 adults (∼40%) living in the United States with or at risk of cardiovascular disease used a digital health solution to track health goals. These health goals included optimizing body weight, increasing physical activity, and/or quitting smoking. Cardiovascular risk factors included hypertension, diabetes, obesity, and/or smoking. Importantly, Aminorroaya et al has studied the characteristics of the participants that used the solutions. Now we know that in this large study, participants with a younger age, female sex, Black race, higher educational attainment, and greater income more often used digital health solutions. This indicates that digital health solutions are not widely adopted throughout the community, with the consequent risk of undesired disparity in health care. To prevent disparities, digital health solutions should also be available and designed for groups that currently were related with minimal use, such as older people as well as those with lower educational attainment and income. In fact, these groups are at higher risk of cardiovascular disease. Interestingly, among those participants who already possess a device suitable for a digital health solution, an estimated 58% did not use their devices to track their cardiovascular health goals. Additional studies are needed to evaluate this group.
Step 2: supported tracking
Aminorroaya et al5 have helped provide important information that can then be used to drive implementation. For those sequential steps, however, additional questions remain to be answered. It must be clear how the digital health solutions are used. The intensity of use is important, and whether its use is successful. Evidence of efficacy of digital solutions is emerging6 and findings are consistent7,8; however, some authors have reported only modest impact.9 It must clear whether users receive bonuses or reminders to achieve goals. The use of the solutions over time have also to be clear. If a health goal is achieved, is there also a sustained benefit over the course of months to years? Tracking is often started enthusiastically, but staying motivated remains a challenge.10
It is useful to build in some form of support for the participants. There can be support via education, but preferably with coaching or even under medical supervision. Consequently, in case of suboptimal (or no) use of the digital health solutions, interventions can be proposed.11
Step 3: clinical endpoint studies
The last and most important step is to investigate digital health solutions for direct clinical benefit. This can be done, for example, by comparing the current gold standard of a treatment, added with an innovative digital health solution.12 Direct clinical benefit will unlock the true potential of digital health solutions.
In summary, now that uptake patterns are described by Aminorroaya et al,5 we can improve the development of digital health solutions for a more widespread adoption and test the direct clinical benefit of these solutions. Importantly, we should prevent that existing health disparities are further exacerbated. If all stakeholders are involved, such as patients, health care providers and insurance companies, it must be possible to increase the correct use of digital health solutions across the wide diversity of our population. In such way, we can truly move via inclusive digital health tracking to improve care, thereby unlocking its true potential.
Funding support and author disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Jensen M.T., Treskes R.W., Caiani E.G., et al. ESC Working Group on e-cardiology position paper: use of commercially available wearable technology for heart rate and activity tracking in primary and secondary cardiovascular prevention—in collaboration with the European Heart Rhythm Association, European Association of Preventive Cardiology, Association of Cardiovascular Nursing and Allied Professionals, Patient Forum, and the Digital Health Committee. Eur Heart J Digit Health. 2021;2:49–59. doi: 10.1093/ehjdh/ztab011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krishnaswami A., Beavers C., Dorsch M.P., et al. Gerotechnology for older adults with cardiovascular diseases: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76:2650–2670. doi: 10.1016/j.jacc.2020.09.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuuring M.J., Kauw D., Bouma B.J. COVID-19 pandemic: practical considerations on rapid initiation of remote care in chronic cardiac patients. Eur Heart J Digit Health. 2020;1:8–9. doi: 10.1093/ehjdh/ztaa007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barsom E.Z., Meijer H.A.W., Blom J., Schuuring M.J., Bemelman W.A., Schijven M.P. Emergency upscaling of video consultation during the COVID-19 pandemic: contrasting user experience with data insights from the electronic health record in a large academic hospital. Int J Med Inform. 2021;150 doi: 10.1016/j.ijmedinf.2021.104463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aminorroaya A., Dhingra L.S., Nargesi A.A., Oikonomou E.K., Krumholz H.M., Khera R. Use of smart devices to track cardiovascular health goals in the United States. JACC: Adv. 2023;2 doi: 10.1016/j.jacadv.2023.100544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piette J.D., List J., Rana G.K., Townsend W., Striplin D., Heisler M. Mobile health devices as tools for worldwide cardiovascular risk reduction and disease management. Circulation. 2015;132:2012–2027. doi: 10.1161/CIRCULATIONAHA.114.008723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kitsiou S., Paré G., Jaana M., Gerber B. Effectiveness of mHealth interventions for patients with diabetes: an overview of systematic reviews. PLoS One. 2017;12 doi: 10.1371/journal.pone.0173160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siopis G., Moschonis G., Eweka E., et al. Effectiveness, reach, uptake, and feasibility of digital health interventions for adults with hypertension: a systematic review and meta-analysis of randomised controlled trials. Lancet Digit Health. 2023;5:e144–e159. doi: 10.1016/S2589-7500(23)00002-X. [DOI] [PubMed] [Google Scholar]
- 9.Shariful Islam S.M., Farmer A.J., Bobrow K., et al. Mobile phone text-messaging interventions aimed to prevent cardiovascular diseases (Text2PreventCVD): systematic review and individual patient data meta-analysis. Open Heart. 2019;6 doi: 10.1136/openhrt-2019-001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasche P., Schlomann A., Mertens A. Who is still playing Pokémon go? A web-based survey. JMIR Serious Games. 2017;5 doi: 10.2196/games.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noah B., Keller M.S., Mosadeghi S., et al. Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials. Nature. 2018;1 doi: 10.1038/s41746-017-0002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koole M.A., Kauw D., Kooiman K.M., et al. An implantable loop recorder or smartphone based single-lead electrocardiogram to detect arrhythmia in adults with congenital heart disease? Front Cardiovasc Med. 2022;9 doi: 10.3389/fcvm.2022.1099014. [DOI] [PMC free article] [PubMed] [Google Scholar]