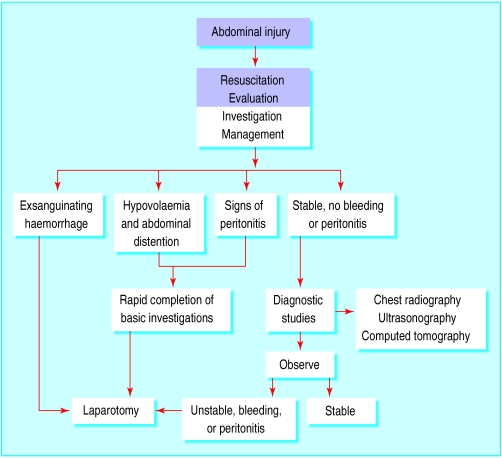
The liver is the most commonly injured solid intra-abdominal organ, but injuries to the pancreas are fairly rare. The primary goal in the treatment of severe abdominal injuries is to preserve life, and management is divided into four sequential phases: resuscitation, evaluation, initial management, and definitive treatment.
Liver trauma
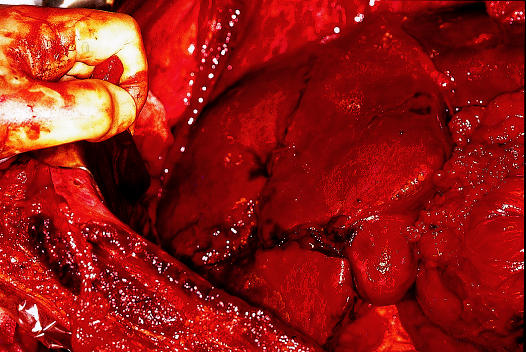
Liver trauma constitutes a broad spectrum of injuries. The magnitude of the injury, the management requirements, and the complexity of the surgical repair are determined by the extent, anatomical location, and mechanism of injury. Blunt liver trauma is usually due to road traffic accidents, assaults, or falls from heights, and results in deceleration injuries with lacerations of liver tissue from shearing stresses. High velocity projectiles, close range shotgun injuries, and crushing blunt trauma cause fragmentation of the hepatic parenchyma with laceration of vessels and massive intraperitoneal haemorrhage. Penetrating injuries such as stab or gunshot wounds cause bleeding without much devitalisation of the liver parenchyma.
Resuscitation
Resuscitation follows standard advanced trauma life support principles: maintenance of a clear airway, urgent fluid resuscitation, ventilatory and circulatory support, and control of bleeding. Effective venous access should be obtained and volume replacement started immediately. The patient's blood is grouped and crossmatched, and blood samples should be sent for urgent analysis of haemoglobin concentration, white cell count, blood gas pressures, and urea, creatinine, and electrolyte concentrations. Patients should also have a nasogastric tube and urinary catheter inserted.
Clinical features of serious liver injury
Hypovolaemic shock:
Hypotension
Tachycardia
Decreased urine output
Low central venous pressure
Abdominal distension
Criteria for non-operative management of liver injuries
Haemodynamically stable after resuscitation
No persistent or increasing abdominal pain or tenderness
No other peritoneal injuries that require laparotomy
< 4 units of blood transfusion required
Haemoperitoneum <500 ml on computed tomography
Simple hepatic parenchymal laceration or intrahepatic haematoma on computed tomography
A liver injury should be suspected in patients with evidence of blunt trauma or knife or gunshot wounds to the right upper quadrant or epigastrium. Occasionally physical signs may be minimal, and gunshot entry and exit wounds can be deceptively distant from the liver. Diagnosis may be difficult in patients who are not fully conscious or have head or spinal cord injuries. The insidious onset of shock in a multiply injured or unconscious patient can easily be missed.
Evaluation
The most important decision after initial resuscitation is whether urgent surgery is needed. Patients who respond to fluid resuscitation and remain stable can be observed closely, investigated, and re-evaluated. Patients who remain shocked after 3 litres of intravenous fluid usually have continued bleeding and require urgent laparotomy. Surgery should not be delayed to obtain the results of special investigations.
Indications for laparotomy
Stab or gunshot wounds that have penetrated the abdomen
Signs of peritonitis
Unexplained shock
Evisceration
Uncontrolled haemorrhage
Clinical deterioration during observation
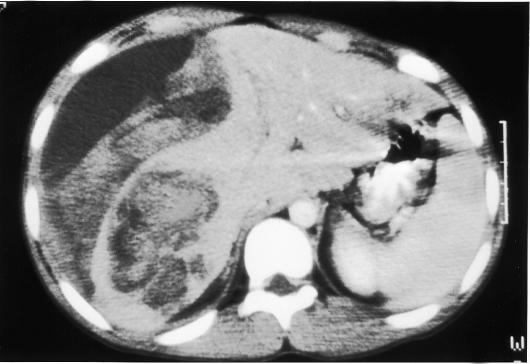
Computed tomography of the abdomen is useful in haemodynamically stable patients suspected of having a major liver injury. Patients with large intrahepatic haematomas or limited capsular tears who have small volumes of blood in the peritoneal cavity can be treated non-operatively. They must, however, be observed carefully and have repeated physical examination.
Surgical management
Most liver injuries are simple and can be treated relatively easily. Complex lesions need to be diagnosed early and may require major surgery by an experienced hepatobiliary surgeon.
The priorities of surgery are to stop haemorrhage, remove dead or devitalised liver tissue, and ligate or repair damaged blood vessels and bile ducts.
Operative approach
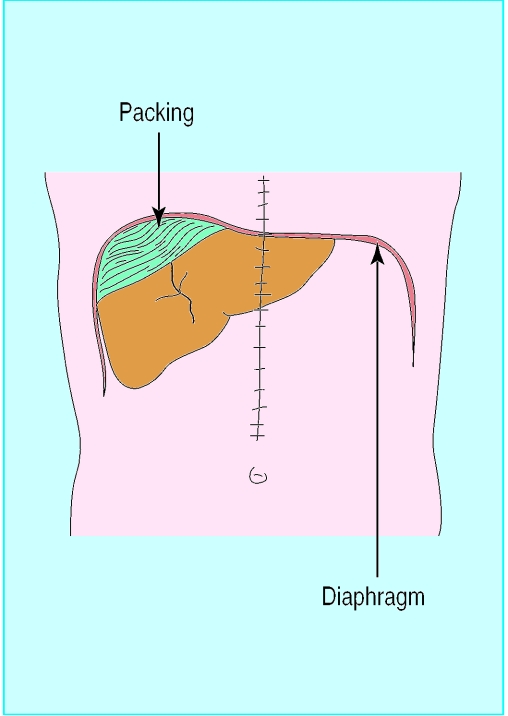
Patients should be prepared from the sternal notch to the pubis so that the incision can be extended into the chest if more proximal control of the vena cava or aorta is needed. A midline incision is used, and the first step is to remove blood and clots and control active bleeding from liver lacerations by packing. Care should be taken to avoid sustained periods of hypotension, and it is important to restore the patient's circulating blood volume during surgery. Any perforations in the bowel should be rapidly sutured to minimise contamination.
Most liver injuries have stopped bleeding spontaneously by the time of surgery. These wounds do not require suturing but should be drained to prevent bile collections. Liver bleeding can usually be stopped by compressing the liver with abdominal packs while experienced surgical and anaesthetic help is summoned.
If visibility is obscured by continued bleeding, the hepatic artery and portal vein should be temporarily clamped with a vascular clamp to allow accurate identification of the site of bleeding. If bleeding cannot be stopped the area should be packed; absorbable gauze mesh can be wrapped around an injured lobe and sutured to maintain pressure and tamponade bleeding. The abdomen is then closed without drainage and the packing removed under general anaesthesia two to three days later. Packing is also used if a coagulopathy develops or to allow the patient to be transferred to a tertiary referral unit for definitive management.
Patients with blunt injuries associated with substantial amounts of parenchymal destruction may require resectional debridement. Rarely, a severe crushing injury necessitates a formal hepatic lobectomy. The most difficult problems are lacerations of the vena cava and major hepatic veins behind the liver because temporary clamping of the inflow vessels does not slow blood loss from hepatic veins. Advanced operative techniques including total hepatic vascular isolation by clamping the portal vein and the vena cava above and below the liver or lobectomy may be required.
Postoperative complications
Rebleeding from the injury, bile leaks, ischaemic segments of liver, and infected fluid collections are the main postoperative complications associated with liver trauma. Angiography (with selective embolisation) is useful if recurrent arterial bleeding or haemobilia occur. Computed tomography is used to define intra-abdominal collections, which are best drained by ultrasound guided needle aspiration or a percutaneous catheter. Subhepatic sepsis develops in about a fifth of cases and is usually related to bile leaks, ischaemic tissue, undrained collections, or bowel injury. The site of bile leaks is best identified by endoscopic retrograde cholangiopancreatography and treated by endoscopic sphincterotomy or stenting, or both.
Prognosis
The overall mortality after liver injury is 10-15% and depends largely on the type of injury and the extent of injury to other organs. Only 1% of penetrating civilian wounds are lethal, whereas the mortality after blunt trauma exceeds 20%. The mortality after blunt hepatic injury is 10% when only the liver is injured. If three major organs are injured, however, mortality approaches 70%. Bleeding causes more than half of the deaths.
Pancreatic trauma
Injuries to the pancreas are uncommon and account for 1-4% of severe abdominal injuries. Most pancreatic injuries occur in young men. Blunt trauma to the pancreas and duodenum usually results from road traffic accidents, when an unrestrained driver is thrown on to the steering wheel. Handlebars may inflict similar injuries to motorcyclists or children on bicycles. Deceleration injury during blunt trauma to the epigastrium may transect the neck of the pancreas over the vertebral bodies. The deep location of the pancreas means that considerable force is needed to cause an injury, and patients often have damage to surrounding organs, including the liver, spleen, stomach, duodenum, and colon. Penetrating injuries may also damage the portal vein or inferior vena cava.
Diagnosis
Blunt trauma to the pancreas may be clinically occult and parenchymal and duct injury may not be recognised during initial evaluation or even surgery. A high index of suspicion is therefore necessary in patients with severe upper abdominal injuries. Abdominal radiographs may show retroperitoneal air and a ruptured duodenum. Serum amylase activity is a poor indicator. It can be normal in patients with severe pancreatic damage and increased in patients with no demonstrable injury to the pancreas. Contrast enhanced computed tomography is the best investigation. Features of pancreatic injury include pancreatic oedema or swelling and fluid collections within or behind the peritoneum or in the lesser peritoneal sac. Endoscopic retrograde cholangiopancreatography can be use to assess the integrity of the main ducts in stable patients.
Intraoperative evaluation
Pancreatic injury is usually diagnosed at laparotomy. The injury may be obvious in patients with a major fracture of the body or neck of the pancreas or associated duodenal injury. Other clues to pancreatic injury are retroperitoneal bile staining, fat necrosis, peripancreatic oedema, or subcapsular haematoma. The pancreas should be fully mobilised and exposed to rule out a duct injury. Failure to detect a major injury to the pancreatic duct is an important cause of postoperative morbidity.
Further reading
Feliciano DV, Lewis CA. Hepatic trauma. In: Pitt H, Carr-Locke DL, Ferrucci R, eds. Hepatobiliary and pancreatic disease. Boston: Little, Brown, 1994:107-24
Pachter HL, Hofsetter SR. The current status of nonoperative management of adult blunt hepatic injuries. Am J Surg 1995;169:442-54.
Krige JEJ, Bornman PC, Beningfield SJ, Funnell I. Pancreatic trauma. In: Pitt H, Carr-Locke DL, Ferrucci R, eds. Hepatobiliary and pancreatic disease. Boston: Little, Brown, 1994:421-36
Haemodynamically stable patients with minor injuries of the body or tail of the pancreas who have no visible damage to the duct can be managed by external drainage of the injury site with soft silastic drains. Major injuries of the body and tail of the pancreas that affect the duct should be treated by distal pancreatectomy. Patients with injuries to the head of the pancreas without devitalisation of pancreatic tissue can be managed by external drainage provided that any associated duodenal injury is amenable to simple repair.
Complications associated with pancreatic trauma
Intra-abdominal abscess
Wound infection
Pancreatic fistula
Pseudocyst
Pancreatic abscess or ascites
Acute or chronic pancreatitis
Pancreatoduodenectomy as a primary procedure is restricted to stabilised patients with disruption of the ampulla of Vater or major devitalising injuries of the pancreatic head and duodenum. Injuries of this severity occur after blunt trauma or gunshot wounds but are uncommon with stab wounds.
Complications
Pancreatic fistulas are the most common complication and generally close spontaneously. However, if a serious duct injury is present, a chronic fistula may develop and require surgical intervention. Pseudocysts that follow pancreatic injury are usually the result of inadequate drainage of pancreatic injury or failure to recognise a major ductal injury. They can be treated by percutaneous drainage guided by ultrasonography or computed tomography if the pancreatic injury was minor. However, patients who have major duct injury may require internal drainage or pancreatic resection.
Figure.
Management of major abdominal trauma
Figure.
Stellate fracture of right lobe of liver
Figure.
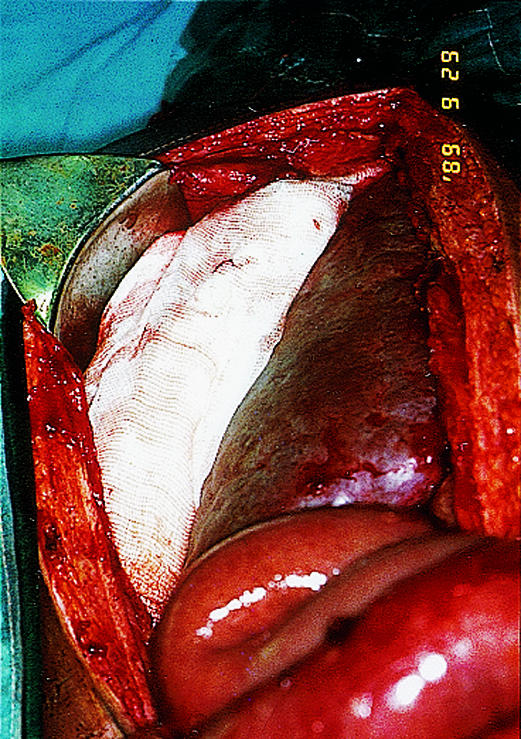
Packing of bleeding liver
Figure.
Large intrahepatic haematoma in patient with blunt trauma
Figure.
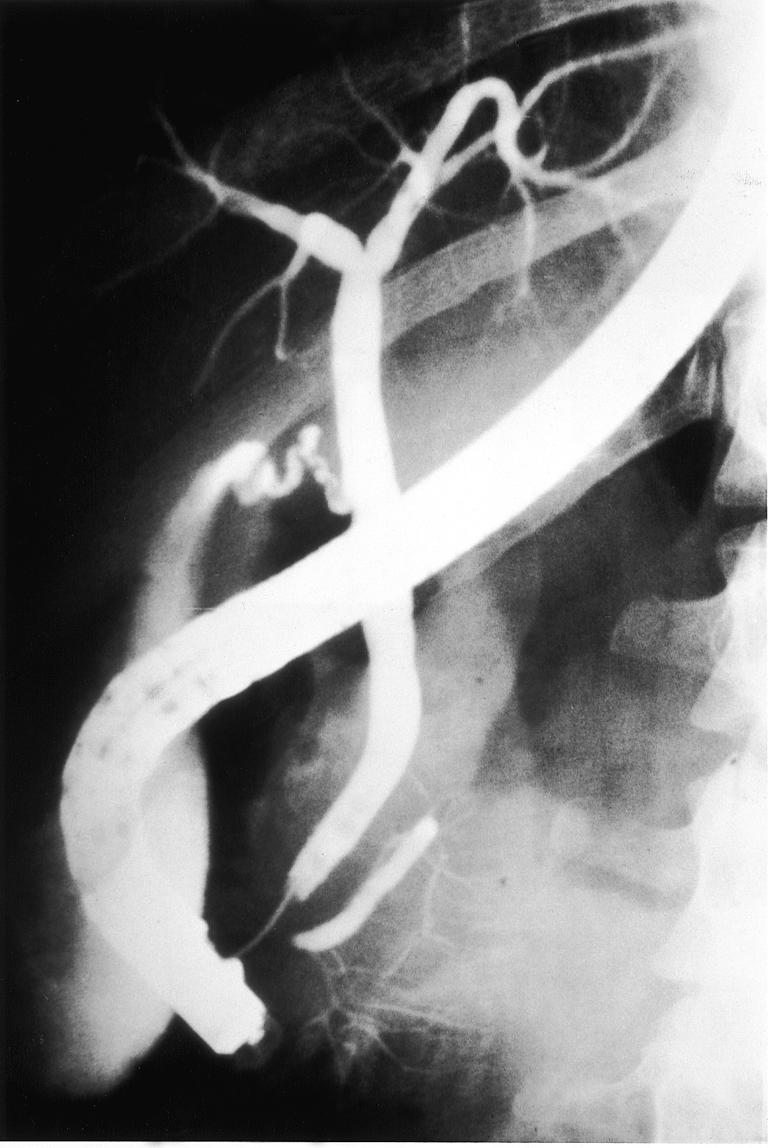
Endoscopic retrograde cholangiopancreatograph showing injury to pancreatic duct with obstruction in the pancreatic neck
Figure.
Pancreatic leak caused by a gunshot wound. The bullet is also visible
Footnotes
J E J Krige is associate professor of surgery, Groote Schuur Hospital, Cape Town, South Africa.
I J Beckingham, consultant hepatobiliary and laparoscopic surgeon, department of surgery, Queen's Medical Centre, Nottingham (Ian.Beckingham@nottingham.ac.uk). The series will be published as a book later this year.