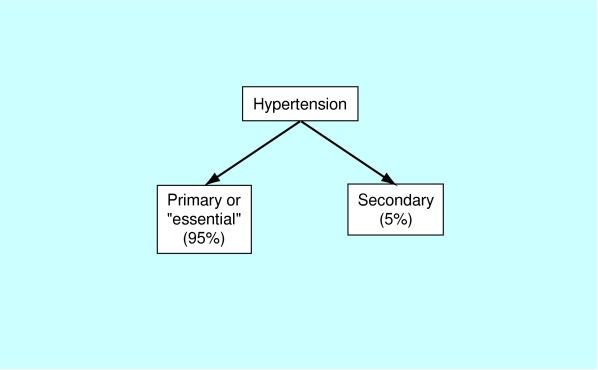
There is still much uncertainty about the pathophysiology of hypertension. A small number of patients (between 2% and 5%) have an underlying renal or adrenal disease as the cause for their raised blood pressure. In the remainder, however, no clear single identifiable cause is found and their condition is labelled “essential hypertension”. A number of physiological mechanisms are involved in the maintenance of normal blood pressure, and their derangement may play a part in the development of essential hypertension.
This article has been adapted from the newly published 4th edition of ABC of Hypertension. The book is available from the BMJ bookshop and at www.bmjbooks.com
It is probable that a great many interrelated factors contribute to the raised blood pressure in hypertensive patients, and their relative roles may differ between individuals. Among the factors that have been intensively studied are salt intake, obesity and insulin resistance, the renin-angiotensin system, and the sympathetic nervous system. In the past few years, other factors have been evaluated, including genetics, endothelial dysfunction (as manifested by changes in endothelin and nitric oxide), low birth weight and intrauterine nutrition, and neurovascular anomalies.
Physiological mechanisms involved in development of essential hypertensionCardiac outputPeripheral resistanceRenin-angiotensin-aldosterone systemAutonomic nervous systemOther factors:BradykininEndothelinEDRF (endothelial derived relaxing factor) or nitric oxideANP (atrial natriuretic peptide)Ouabain
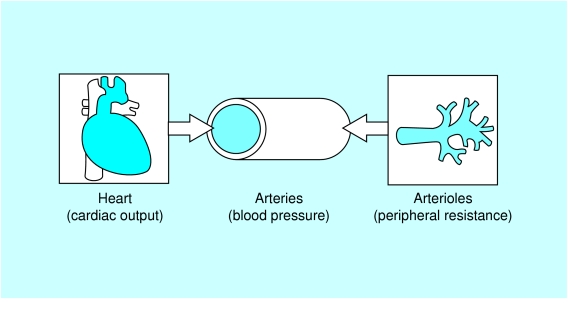
Cardiac output and peripheral resistance
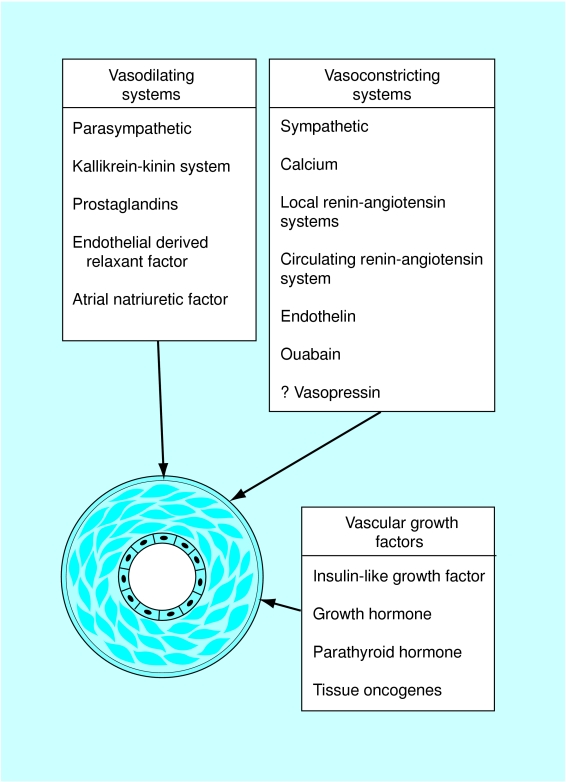
Maintenance of a normal blood pressure is dependent on the balance between the cardiac output and peripheral vascular resistance. Most patients with essential hypertension have a normal cardiac output but a raised peripheral resistance. Peripheral resistance is determined not by large arteries or the capillaries but by small arterioles, the walls of which contain smooth muscle cells. Contraction of smooth muscle cells is thought to be related to a rise in intracellular calcium concentration, which may explain the vasodilatory effect of drugs that block the calcium channels. Prolonged smooth muscle constriction is thought to induce structural changes with thickening of the arteriolar vessel walls possibly mediated by angiotensin, leading to an irreversible rise in peripheral resistance.
It has been postulated that in very early hypertension the peripheral resistance is not raised and the elevation of the blood pressure is caused by a raised cardiac output, which is related to sympathetic overactivity. The subsequent rise in peripheral arteriolar resistance might therefore develop in a compensatory manner to prevent the raised pressure being transmitted to the capillary bed where it would substantially affect cell homeostasis.
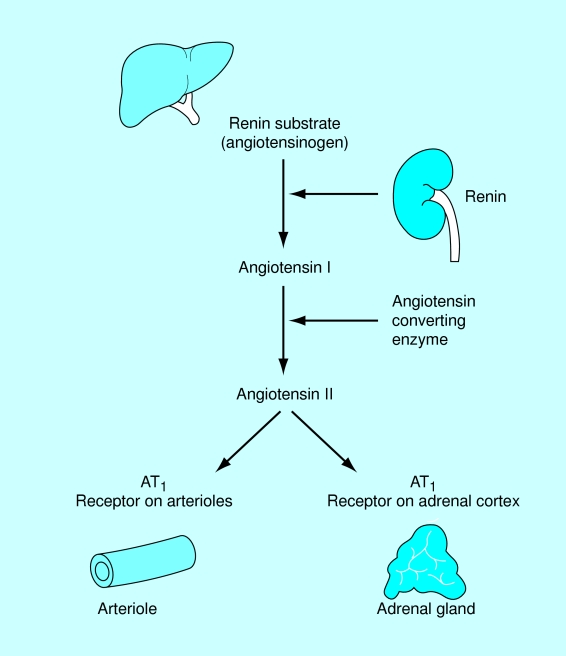
Renin-angiotensin system
The renin-angiotensin system may be the most important of the endocrine systems that affect the control of blood pressure. Renin is secreted from the juxtaglomerular apparatus of the kidney in response to glomerular underperfusion or a reduced salt intake. It is also released in response to stimulation from the sympathetic nervous system.
Renin is responsible for converting renin substrate (angiotensinogen) to angiotensin I, a physiologically inactive substance which is rapidly converted to angiotensin II in the lungs by angiotensin converting enzyme (ACE). Angiotensin II is a potent vasoconstrictor and thus causes a rise in blood pressure. In addition it stimulates the release of aldosterone from the zona glomerulosa of the adrenal gland, which results in a further rise in blood pressure related to sodium and water retention.
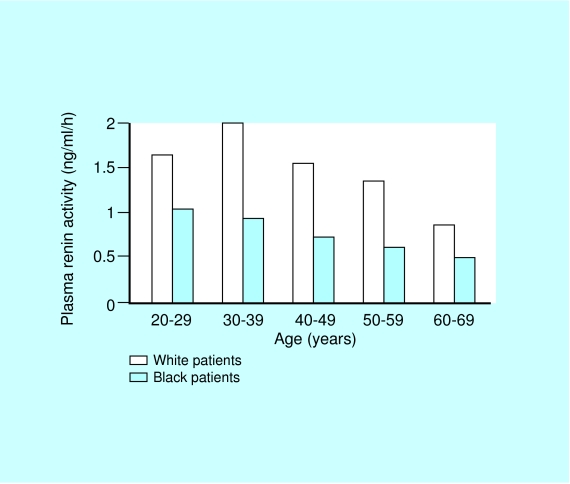
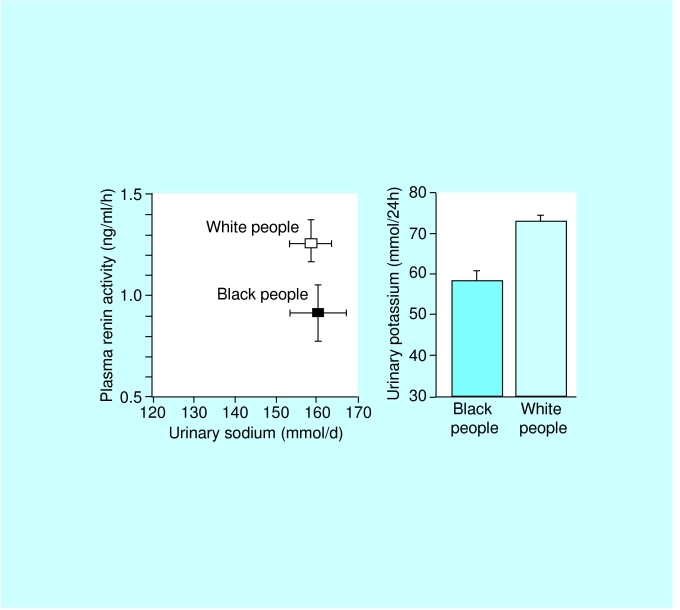
The circulating renin-angiotensin system is not thought to be directly responsible for the rise in blood pressure in essential hypertension. In particular, many hypertensive patients have low levels of renin and angiotensin II (especially elderly and black people), and drugs that block the renin-angiotensin system are not particularly effective.
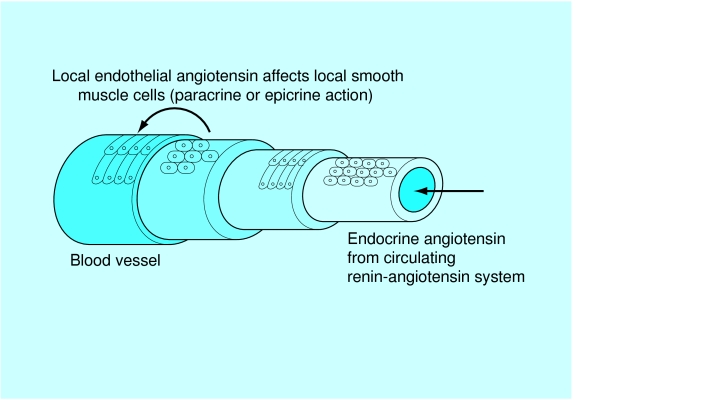
There is, however, increasing evidence that there are important non-circulating “local” renin-angiotensin epicrine or paracrine systems, which also control blood pressure. Local renin systems have been reported in the kidney, the heart, and the arterial tree. They may have important roles in regulating regional blood flow.
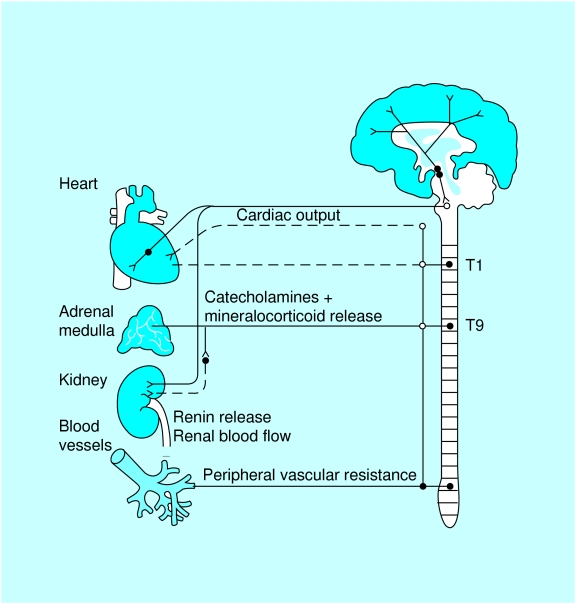
Autonomic nervous system
Sympathetic nervous system stimulation can cause both arteriolar constriction and arteriolar dilatation. Thus the autonomic nervous system has an important role in maintaining a normal blood pressure. It is also important in the mediation of short term changes in blood pressure in response to stress and physical exercise.
There is, however, little evidence to suggest that epinephrine (adrenaline) and norepinephrine (noradrenaline) have any clear role in the aetiology of hypertension. Nevertheless, their effects are important, not least because drugs that block the sympathetic nervous system do lower blood pressure and have a well established therapeutic role.
It is probable that hypertension is related to an interaction between the autonomic nervous system and the renin-angiotensin system, together with other factors, including sodium, circulating volume, and some of the more recently described hormones.
• Cross transplantation experiments with kidneys of hypertensive rats transferred to normotensives, and vice versa, strongly suggest that hypertension has its origins in the kidneys• Similarly human evidence from renal transplant recipients shows that they are more likely to develop hypertension if the donors' relatives are hypertensive• This essential hypertension may be due to a genetically inherited abnormality of sodium handling
Endothelial dysfunction
Vascular endothelial cells play a key role in cardiovascular regulation by producing a number of potent local vasoactive agents, including the vasodilator molecule nitric oxide and the vasoconstrictor peptide endothelin. Dysfunction of the endothelium has been implicated in human essential hypertension.
Modulation of endothelial function is an attractive therapeutic option in attempting to minimise some of the important complications of hypertension. Clinically effective antihypertensive therapy appears to restore impaired production of nitric oxide, but does not seem to restore the impaired endothelium dependent vascular relaxation or vascular response to endothelial agonists. This indicates that such endothelial dysfunction is primary and becomes irreversible once the hypertensive process has become established.
Vasoactive substances
Many other vasoactive systems and mechanisms affecting sodium transport and vascular tone are involved in the maintenance of a normal blood pressure. It is not clear, however, what part these play in the development of essential hypertension. Bradykinin is a potent vasodilator that is inactivated by angiotensin converting enzyme. Consequently, the ACE inhibitors may exert some of their effect by blocking bradykinin inactivation.
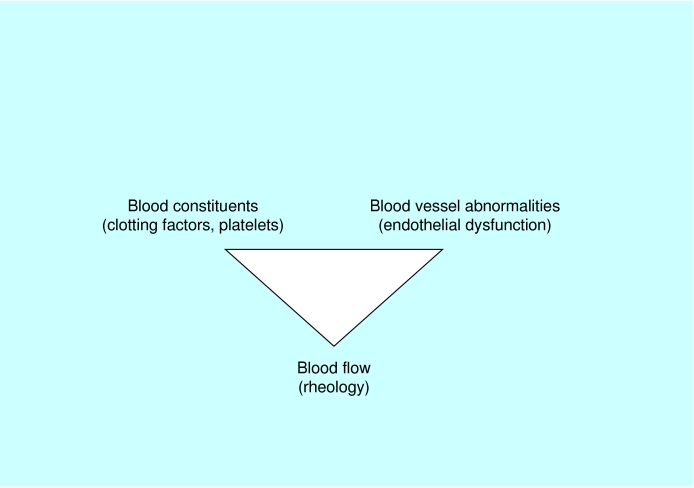
The thrombotic paradox of hypertension (the Birmingham paradox)Although the blood vessels are exposed to high pressures in hypertension, the main complications of hypertension (stroke and myocardial infarction) paradoxically are thrombotic rather than haemorrhagic.
Endothelin is a recently discovered, powerful, vascular, endothelial vasoconstrictor, which may produce a salt sensitive rise in blood pressure. It also activates local renin-angiotensin systems. Endothelial derived relaxant factor, now known to be nitric oxide, is produced by arterial and venous endothelium and diffuses through the vessel wall into the smooth muscle causing vasodilatation.
Atrial natriuretic peptide is a hormone secreted from the atria of the heart in response to increased blood volume. Its effect is to increase sodium and water excretion from the kidney as a sort of natural diuretic. A defect in this system may cause fluid retention and hypertension.
Sodium transport across vascular smooth muscle cell walls is also thought to influence blood pressure via its interrelation with calcium transport. Ouabain may be a naturally occurring steroid-like substance which is thought to interfere with cell sodium and calcium transport, giving rise to vasoconstriction.
Hypercoagulability
Patients with hypertension demonstrate abnormalities of vessel wall (endothelial dysfunction or damage), the blood constituents (abnormal levels of haemostatic factors, platelet activation, and fibrinolysis), and blood flow (rheology, viscosity, and flow reserve), suggesting that hypertension confers a prothrombotic or hypercoagulable state. These components appear to be related to target organ damage and long term prognosis, and some may be altered by antihypertensive treatment.
Insulin sensitivity
Epidemiologically there is a clustering of several risk factors, including obesity, hypertension, glucose intolerance, diabetes mellitus, and hyperlipidaemia. This has led to the suggestion that these represent a single syndrome (metabolic syndrome X or Reaven's syndrome), with a final common pathway to cause raised blood pressure and vascular damage. Indeed some hypertensive patients who are not obese display resistance to insulin. There are many objections to this hypothesis, but it may explain why the hazards of cardiovascular risk are synergistic or multiplicative rather than just additive.
Genetic factors
Although separate genes and genetic factors have been linked to the development of essential hypertension, multiple genes are most likely contribute to the development of the disorder in a particular individual. It is therefore extremely difficult to determine accurately the relative contributions of each of these genes. Nevertheless, hypertension is about twice as common in subjects who have one or two hypertensive parents, and many epidemiological studies suggest that genetic factors account for approximately 30% of the variation in blood pressure in various populations. This figure can be derived from comparisons of parents with their monozygotic and dizygotic twin children, as well as their other children, and with adopted children. Some familial concordance is, however, due to shared lifestyle (chiefly dietary) factors.
Examples of specific genetic mutations causing hypertension• Liddle's syndrome, a disorder associated with hypertension, low plasma renin and aldosterone levels, and hypokalaemia, all of which respond to amiloride, an inhibitor of the distal renal epithelial sodium channel• Glucocorticoid-remediable aldosteronism, a disorder mimicking Conn's syndrome, in which there is a chimeric gene formed from portions of the 11β-hydroxylase gene and the aldosterone synthase gene. This defect results in hyperaldosteronism, which is responsive to dexamethasone and has a high incidence of stroke• Congenital adrenal hyperplasia due to 11β-hydroxylase deficiency, a disorder that has been associated with 10 different mutations of the CYP11B1 gene• Syndrome of apparent mineralocorticoid excess, arising from mutations in the gene encoding the kidney enzyme 11α-hydroxysteroid dehydrogenase; the defective enzyme allows normal circulating concentrations of cortisol (which are much higher than those of aldosterone) to activate the mineralocorticoid receptors• Congenital adrenal hyperplasia due to 17α-hydroxylase deficiency, a disorder with hyporeninaemia hypoaldosteronism, absent secondary sexual characteristics, and hypokalaemia• Gordon's syndrome (pseudo-hypoaldosteronism): familial hypertension with hyperkalaemia, possibly related to the long arm of chromosome 17• Sporadic case reports of familial inheritance of phaeochromocytoma (multiple endocrine neoplasia, MEN-II syndrome), Cushing's syndrome, Conn's syndrome, renal artery stenosis due to fibromuscular dysplasiaOther associations• The angiotensinogen gene may be related to hypertension• The angiotensin converting enzyme gene may be related to left ventricular hypertrophy or hypertensive nephropathy• α-Adducin gene may be related to salt sensitive hypertension
Some specific genetic mutations can rarely cause hypertension. Experimental models of genetic hypertension have shown that the inherited tendency to hypertension resides primarily in the kidney. For example, animal and human studies show that a transplanted kidney from a hypertensive donor raises the blood pressure and increases the need for antihypertensive drugs in recipients coming from “normotensive” families. Conversely a kidney from a normotensive donor does not raise the blood pressure in the recipient.
Increased plasma levels of angiotensinogen, the protein substrate acted on by renin to generate angiotensin I, have also been reported in hypertensive subjects and in children of hypertensive parents.
Hypertension is rarely found in rural or “tribal” areas of Africa, but it is very common in African cities and in black populations in Britain and the United States. Whereas the rural/urban differences in Africa are clearly due to lifestyle and dietary factors, the finding that hypertension is commoner in black people compared with white people may have some genetic basis. There is some evidence from salt loading studies in medical students that black Americans are more susceptible to a given salt load than white Americans, and may be more sensitive to the beneficial effects of salt restriction.
Intrauterine influences
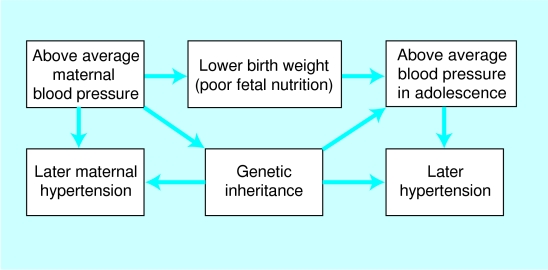
There is increasing evidence that fetal influences, particularly birth weight, may be a determinant of blood pressure in adult life. For example, babies who are small at birth are more likely to have higher blood pressure during adolescence and to be hypertensive as adults. Babies who are small for their age are also more likely to have metabolic abnormalities that have been associated with the later development of hypertension and cardiovascular disease, such as insulin resistance, diabetes mellitus, hyperlipidaemia, and abdominal obesity (the “Barker hypothesis”). Insulin resistance almost certainly contributes to the increased prevalence of coronary disease seen in adults of low birth weight.
It is possible, however, that genetic factors influence the Barker hypothesis. Mothers with above average blood pressure in pregnancy give birth to smaller babies who subsequently develop above average blood pressure themselves and eventually hypertension. It is entirely likely that the similarity of blood pressures in mother and child are genetic and, in a modern “healthy” society, unrelated to intrauterine undernutrition.
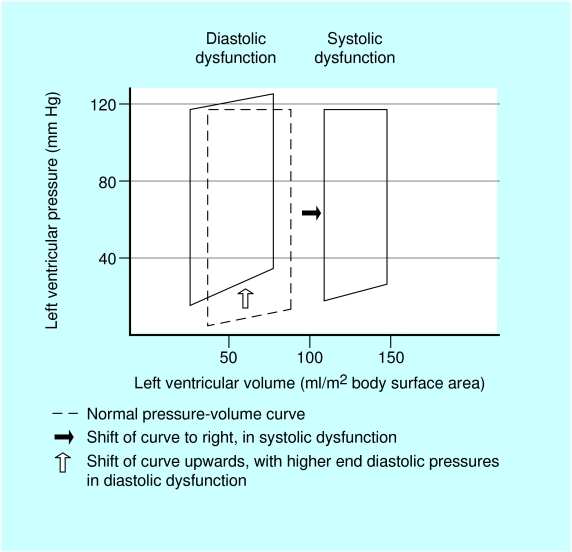
Diastolic dysfunction
In hypertensive left ventricular hypertrophy, the ventricle cannot relax normally in diastole. Thus, to produce the necessary increase in ventricular input, especially during exercise, there is an increase in left atrial pressure rather than the normal reduction in ventricular pressure, which produces a suction effect as described above. This can lead to an increase in pulmonary capillary pressure that is sufficient to induce pulmonary congestion. The rise in atrial pressure can also lead to atrial fibrillation, and in hypertrophied ventricles dependent on atrial systole the loss of atrial transport can result in a significant reduction in stroke volume and pulmonary oedema. Exercise induced subendocardial ischaemia can also produce an “exaggerated” impairment of diastolic relaxation of the hypertrophied myocardium.
Further reading
Barker DJP, Osmond C, Golding J, Kuh D, Wadsworth MEJ. Growth in utero, blood pressure in childhood and adult life and mortality from cardiovascular disease. BMJ 1989;298:564-7.
Dzau VJ. Circulating versus local renin-angiotensin system in cardiovascular homeostasis. Circulation 1988;77(suppl 1):I4-13.
Harrap SB. Hypertension: genes versus environment. Lancet 1994;344:169-71.
Hughes AD, Schachter M. Hypertension and blood vessels. Br Med Bull 1994;50:356-70.
Kurtz TW. Genetic models of hypertension. Lancet 1994;344:167-8.
Lip GYH, Li-Saw-Hee FL. Does hypertension confer a hypercoagulable state? J Hypertens 1998;16:913-6.
Mathias CJ. Role of sympathetic efferent nerves in blood pressure regulation and in hypertension. Hypertension 1991;18:22-30.
Sagnella G, Macgregor GA. Atrial natriuretic peptides. Q J Med 1990;77:1001-7.
Figure.
The relative frequency of primary and secondary hypertension
Figure.
The heart, arteries, and arterioles in hypertension
Figure.
Plasma renin in black and white hypertensive patients. Adapted from Freis ED, Materson BJ, Flamenbaum V. Comparison of propranolol or hydrochlorothiazide alone for treatment of hypertension. III. Evaluation of the renin-angiotensin system. Am J Med 1983;74:1029-41
Figure.
Local versus systemic renin-angiotensin systems
Figure.
Renin-angiotensin system and effects on blood pressure and aldosterone release
Figure.
The autonomic nervous system and its control of blood pressure. Reproduced with permission from Swales JD, Sever PS, Plart WS. Clinical atlas of hypertension. London: Gower Medical, 1991
Figure.
The control of peripheral arteriolar resistance. Reproduced with permission from Beevers DG, MacGregor GA. Hypertension in practice. 3rd ed. London: Martin Dunitz, 1999
Figure.
Virchow's triad and the prothrombotic state in hypertension
Figure.
Renin and electrolytes in black and white people. He J, Klag MJ, Appel LJ, Charleston J, Whelton PK. The renin-angiotensin system and blood pressure; differences between blacks and whites. Am J Hypertens 1999;12:555-62
Figure.
Possible mechanisms to explain why low birthweight babies are more likely to develop hypertension in later life
Figure.
Pressure-volume curves demonstrating diastolic/systolic dysfunction