Abstract
Background: Mobile technology is increasingly prevalent in healthcare, serving various purposes, including remote health monitoring and patient self-management, which could prove beneficial to early hospital discharges. Aims: This study investigates the transitional care program experience facilitating early discharges in a pediatric setting through the use of an easy-to-use mobile medical device (TytoCare™, TytoCare Ltd., Natanya, Israel). Outcomes: This study aims to assess the effectiveness of telehomecare in achieving complete resolution of diseases without readmission, compare the length of stay between intervention and standard care groups, and gather user and professional experiences. Methods: A randomized open-label, controlled pilot study enrolled 102 children, randomly assigned to the telehomecare (TELE) group (n = 51, adopting early hospital discharge with continued home monitoring) or the standard-of-care (STAND) group (n = 51). Primary outcomes include complete disease resolution without readmission. Secondary objectives include recording a shorter length of stay in the intervention group. Surveys on user and professional experiences were conducted. A group of 51 children declining telemedicine services (NO-TELE) was also included. Results: In the TELE group, 100% of children achieved complete disease resolution without readmission, with a median duration of stay of 4 days, significantly shorter than the 7 days in the STAND group (p = 0.01). The telemedicine system demonstrated efficient performance and high satisfaction levels. The NO-TELE group showed no significant differences in demographics or digital technology competence. Perceived benefits of telemedicine included time and cost savings, reduced hospital stays, and technology utility and usability. Conclusions: This study demonstrates that user-friendly mobile medical devices effectively facilitate early hospital discharges in a pediatric setting. These devices serve as a bridge between home and hospital, optimizing care pathways.
Keywords: user-friendly mobile, medical devices, early hospital discharges, pediatrics, children
1. Introduction
The utilization of digital health in pediatric care offers an opportunity to leverage technology for connecting patients and families with expert healthcare providers, mitigating costs and risks associated with hospital-based care [1]. Connected health, encompassing telecare, telemedicine, telehealth, m-Health, e-Health, and digital health services, has experienced substantial growth in pediatrics, addressing healthcare access disparities and overcoming social and geographic barriers [2,3].
As the shift toward home-based care supported by technology continues, patients and family caregivers need to understand and assume greater responsibilities for this new care model [4,5].
Recently, innovative “hospital at home” (HaH) initiatives have been developed to connect home-based care with hospital services, utilizing Technology-Enabled Care (TEC) for improved patient care and self-management. Kanagala et al. [6] reported that HaH care can result in lower median length of stay and readmission rates, offering a flexible model adaptable to varying demand situations with better clinical outcomes. Beyond economic considerations, early hospital discharge is crucial for optimizing care, especially in pediatric settings. The “European Association for Children in Hospital Charter” emphasizes the necessity of hospital admission only when essential, advocating for the prompt discharge of hospitalized children to ensure their psychophysical well-being [7].
Mobile technology is increasingly prevalent in healthcare [8,9], serving various purposes, including remote health monitoring and patient self-management, which could prove beneficial for early hospital discharges with significant psychosocial and economic impacts.
A user-friendly device refers to a device that is easy and intuitive to use, designed to accommodate the needs of a diverse range of users, including those with limited abilities or technological skills. A user-friendly mobile device, the TytoCare™ system, functions as both an otoscope and stethoscope [10,11,12]. Enabling remote examinations of ears, throat, skin, heart, and lungs, it supports the transmission of examination data from caregivers or healthcare professionals to physicians, overcoming obstacles to telemedicine integration.
Although limited, existing data on user-friendly mobile device use in pediatrics show promise. Wagner et al. [13] demonstrated concordance between measurements from remote physical examinations with a mobile medical device and in-person examinations in children older than 2 years. McDaniel et al. [14] highlighted superior sound and image quality compared to stand-alone devices, reducing diagnostic limitations. Notario et al. [15] demonstrated the feasibility and positive reception of in-home telehealth mobile devices, leading to reduced hospitalizations compared to usual care.
This study aims to explore the experience of a transitional care program using a user-friendly mobile medical device (TytoCare™, TytoCare Ltd., Natanya, Israel) to facilitate early hospital discharges in a pediatric environment. User and physician experience surveys will contribute valuable insights, furthering our understanding of the role of mobile medical devices as enablers in the perspective of HaH healthcare in pediatrics.
2. Methods
2.1. Study Design and Randomization
Before the start of a study, researchers should develop a detailed randomization protocol outlining the procedures for assigning participants to different treatment groups.
This study employed a single-center, two-group, randomized, open-label design with parallel arms conducted at Buzzi Children’s Hospital, situated in the metropolitan area of Milan, Italy. The experimental group involved early discharge with telehomecare (TELE), while the standard care (STAND) group received in-person physical care until the completion of hospitalization.
All patients/caregivers admitted from November 2022 to July 2023 who met the eligibility criteria were offered participation in the project. Those who agreed to engage in telemedicine were enrolled and subjected to randomization.
Informed consent was obtained and the allocation sequence, which was generated using a randomization procedure, assigned the participants to different groups. The randomization was executed in a 1:1 ratio (TELE/STAND) through a computer-generated number determinant. A physician who was unrelated to the process created a registration form to document it. Treatment allocation remained unblinded to both subjects and physicians.
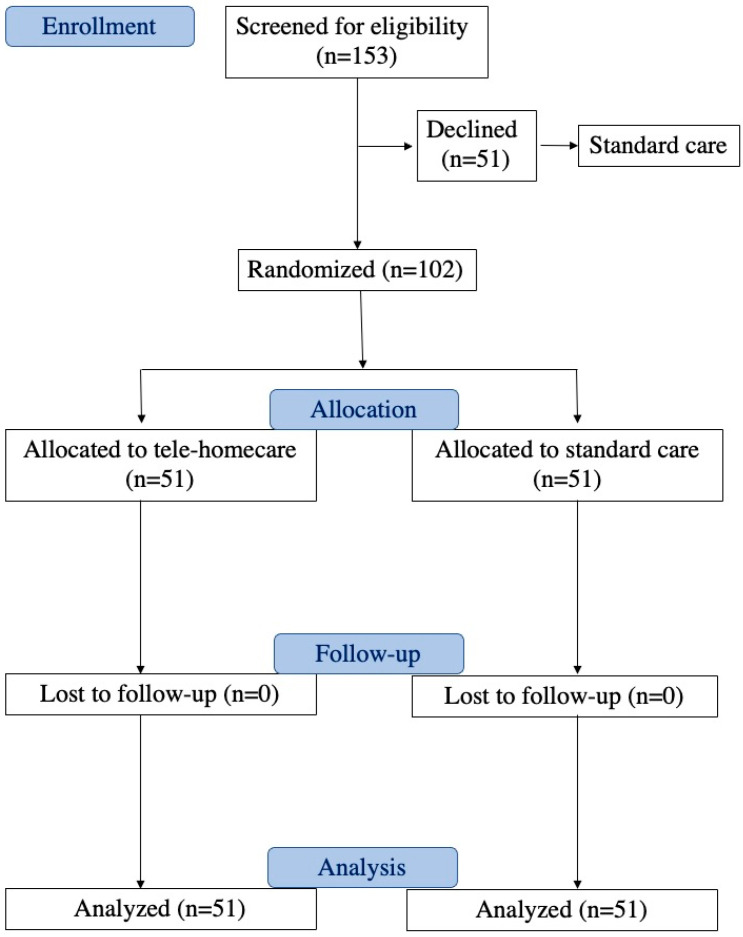
Children declining participation in the telemedicine project continued with standard treatment. The study process adhered to the Consolidated Standards of Reporting Trials guidelines, as illustrated in Figure 1. The protocol was registered in the Clinical Trials Registry clinicaltrials.gov (NCT06171763) (accessed on 20 December 2023).
Figure 1.
Flow diagram depicting the progression through the phases of the randomized trial involving two groups (telehomecare and standard care).
Periodic review of documentation and verification of data integrity were scheduled during the study.
2.2. Participants
Participants in the present study were consecutively enrolled at the Buzzi Children’s Hospital (Milano, Italy) in the Pediatric Unit, Pediatric Surgery Unit, and Palliative Care Unit, and dyads of the hospitalized patient and family caregiver were recruited.
Inclusion criteria:
Age of enrolled subjects: 0–18 years.
Gender of patients (males and females).
Patient status: hospitalized at the completion of treatment.
Stability in vital signs (heart rate, respiratory rate, oxygen saturation).
Stability/improvement/resolution in biochemical tests.
No fever.
Consent/Assent: participants must be willing and provide appropriate consent or assent based on their age.
Proximity to domicile: living within a maximum 45 min distance from the facility.
Adequate home environment
Language proficiency: adequate proficiency in the Italian language.
Possession of a compatible device.
Exclusion criteria:
Refusal to participate in the program.
Instability in vital signs.
Presence of fever.
Deteriorating results in biochemical tests.
Living more than 45 min away from the facility.
Inadequate home facilities.
Language barrier.
Lack of possession of a compatible device.
Not having a device with an operating system capable of supporting the Tytocare app 7.0.0.433.
Parental consent was obtained from all participants or their responsible guardians after a thorough explanation of the study’s purpose. The study was conducted in accordance with the Declaration of Helsinki guidelines and approved by the Ethics Committee Milano Area 1 (Protocol number n. 0033846, date 3 August 2022). A medical team of 14 professionals were trained in the use of the TytocareTM device and voluntarily agreed to participate in the project.
2.3. Intervention
The telehomecare intervention entails an early hospital discharge with ongoing home monitoring utilizing a user-friendly mobile device (TytoCare™). Additionally, an in-person clinical reassessment was conducted 72 h after discharge to evaluate intervention outcomes.
Patient instructions were developed and shared to facilitate access to and download of medical reports, promoting patient engagement and empowerment in managing their healthcare.
2.3.1. Experimental Group: Telehomecare
For patients/caregivers allocated to the TELE group, healthcare personnel trained in TytoCare™ system usage provided instructions before discharge. Subsequently, each patient received a device for use until the scheduled post-discharge clinical assessment. A parent or caregiver was invited to participate for each pediatric patient.
Every 24 h, remote synchronous teleconsultation assessed the patient, with the physician using the TytoCare™ device for a comprehensive routine procedure, including medical history and physical examination. Data collection sheets were completed during the tele-visit.
At the 72 h post-discharge mark, an in-person clinical assessment was scheduled to evaluate outcomes. Specifically, the visit evaluated the complete resolution of the disease state through a post-discharge objective examination.
TytoCare™ is a registered medical device compliant with European Medical Device Directive 93/42/EEC. The certificate of conformity and technical datasheet are provided in Supplementary Material S1.
The TytoCare™ System served as the remote physical examination tool. This device enabled patients to conduct examinations and transmit audio, video, or image data to medical professionals located remotely; the TytoCare™ Device establishes a connection with an application on the patient’s mobile device to facilitate the communication of examination data and enable online meetings with clinicians. TytoCare™ is a modular, all-in-one device that encompasses functions such as a stethoscope, otoscope, tongue depressor, and thermometer:
-
-
Stethoscope: Frequency range of 20–3500 Hz, heart rate range of 30–250 BPM, dimensions of 40 × 39 mm, and a weight of 0.06 kg.
-
-
Otoscope: Image resolution of 640 × 480 (VGA), weight of 0.02 kg, and an adaptable speculum for children (3 mm).
-
-
Tongue Depressor: For children (60 mm), weight of 0.011 kg.
-
-
Thermometer: Detection range of 34.4–42.2 °C; accuracy of 0.2 °C for the temperature range 38–41 °C, with a precision of 0.2 degrees Celsius within the range of 38 to 41 degrees Celsius and a precision of 0.3 degrees Celsius outside this range (compliant with ASTM E1965-98 [16] and ISO 80601-2-56 [17]).
2.3.2. Non-Intervention Group: Standard Care
Patients in the STAND group remained hospitalized for ongoing treatment. Every 24 h, in-person assessments by medical staff included a traditional physical examination utilizing standard equipment such as a digital thermometer, conventional stethoscope, and otoscope. The same data collection sheet was completed during these assessments. After 72 h of hospital observation, an in-person clinical examination was conducted to evaluate outcomes, specifically assessing the complete resolution of the disease state through a post-discharge objective examination.
Additionally, a group of 51 children declining telemedicine service (NO-TELE) was included in the study to record the reasons for refusal.
2.4. Outcomes
Considering in-person visits as the standard care procedure, the primary objective is to achieve concordance with complete resolution of the disease through in-person physical care without readmission to the hospital, expecting non-readmission in a minimum of 90% of cases. Secondary objectives include recording a lower length of stay in the interventional group. User and professional experience surveys were conducted to evaluate the level of acceptance and satisfaction with the telehomecare model.
2.5. Sample Size
A sample size of 50 in each randomized group achieves 80% power to detect a non-inferiority margin difference between group proportions of −0.0800. The reference group proportion is 0.9800, and the interventional group proportion is assumed to be 0.9000 under the null hypothesis of inferiority. The power was computed for the case when the standard treatment group proportion is 0.9889. The test statistic used is the one-sided Score test (Farrington and Manning). The significance level targeted for the test was 0.0500, and the achieved significance level by this design is 0.0465.
2.6. User and Physician Survey Questions
After randomization, in both the TELE and STAND groups, a user survey was distributed (see Table 1). The survey consisted of self-administered questions categorized into five sections, covering the following topics:
Sociodemographic information about the children and parents.
Employment details of parents who work.
Distance between home and the hospital.
Parents’ knowledge, attitudes, and technological skills in utilizing technologies, digital communication systems, and telehealth services [18,19,20].
Table 1.
Telehomecare and standard care user survey.
| Question | Telehomecare | Standard Care | No-Telemedicine |
|---|---|---|---|
| Demographic and socioeconomic characteristics of the children and parents | |||
| Who is completing the questionnaire? | |||
| Mother | 84.31% | 94.12% | 86.27% |
| Father | 15.69% | 5.88% | 11.76% |
| Other | 0% | 0% | 1.96% |
| What is the age of the individual completing the questionnaire? | 35.70 ± 10.79 | 35.93 ± 7.81 | 38.08 ± 8.47 |
| What is the nationality of the individual completing the questionnaire? | |||
| Italian/Foreign | 72.6%/27.4% | 70.59%/29.41% | 82.35/17.65% |
| Does the patient have siblings? | |||
| Yes (1/more than 1) | 52% | 53.33% | 54.9% |
| (38%/14%) | (30.0%/16.67%) | (37.25%/17.4%) | |
| No | 48% | 53.33% | 45.1% |
| What is the parental educational background of the individual answering the questionnaire? | |||
| Middle school | 12.0% | 10.0% | 7.84% |
| High school | 46.0% | 40.0% | 52.94% |
| College and/or postgraduate | 42.0% | 50% | 39.21% |
| Employment characteristics of the working parents | |||
| Is the mother currently employed? | |||
| Yes, employed-full-time/part-time/independent contractor | 72.5% | 76.47% | 78.43% |
| No, not seeking work/unemployed and seeking work | 27.45% | 23.53% | 21.57% |
| Is the father currently employed? | |||
| Yes, employed-full-time/part-time/independent contractor | 97.877% | 100% | 96.08% |
| No, not seeking work/unemployed and seeking work | 2.13% | 0% | 3.92 |
| Distance from residence to hospital | |||
| How far is the hospital from your home (in kilometers)? | 26.25 ± 10.40 | 24.65 ± 16.65 | 25.81 ± 10.79 |
| What mode of transportation would you use to reach the hospital? | |||
| Public transport/Private vehicle | 16.33%/83.67% | 19.57%/80.43% | 8.7%/92.30% |
| Parental proficiency, mindset, and ability in utilizing technology, digital communication systems and telehealth services | |||
| How frequently do you: | |||
| Require assitance with reading medical documentation | |||
|
25.49%/33.33% | 16.67%/23.33% | 11.76%/21.57% |
|
29.41% | 46.67% | 45.10% |
|
9.8%/1.96% | 13.33%/0% | 19.61%/1.96 |
| Experience challenges in comprehending health status because of reading limitations | |||
|
27.45%/37.25% | 16.67%/30% | 17.65%/21.57% |
|
27.45% | 43.33% | 50.98% |
|
4%/0% | 6.67%/3.33% | 9.80% |
| Encounter difficulties in comprehending health-related information | |||
|
39.22%/37.25% | 23.33%/33.33% | 25.49%/37.25% |
|
19.61% | 40.0% | 29.41% |
|
3.92%/0% | 0%/3.33% | 7.84% |
| Feel confident in filling out medical consent forms | |||
|
20.0%/16.0% | 10.0%/6.67% | 11.76%/21.57% |
|
20% | 30% | 45.10% |
|
36%/8% | 30%/23.33% | 19.6%/1.96% |
| Do you have internet access at your home? | |||
| Yes/No | 94.12%/5.88% | 93.33%/6.67% | 89.90%/10.20% |
| How frequently do you utilize your home internet connection? | |||
| Every day | 100% | 100% | 97.56% |
| One/two times a week | 0% | 0% | 2.44% |
| Occasionally | 0% | 0% | 0% |
| What do you primarily use your smartphone for? | |||
| Phone calls | 94.11% | 94.12% | 94.11% |
| Messages | 92.16% | 902% | 88.23% |
| Shopping | 72.55% | 82.36 | 68.62% |
| Banking | 76.47% | 74.5% | 64.71% |
| Sending emails | 90.20% | 86.28 | 74.51% |
| Learning | 52.94% | 54.90% | 47.06% |
| Social network use | 72.55% | 58.8% | 66.66% |
| Entertainment (games/movies) | 62.74% | 62.74% | 49.01% |
| Checking health status | 39.21% | 43.14 | 68.63% |
| How would you rate your proficiency in using digital technologies? | |||
| Excellent/Good | 82.35% | 82.35% | 78% |
| Moderate | 17.65% | 17.65% | 20% |
| Inadequate | 0% | 0% | 2% |
| Utilization of applications or online platforms for: | |||
|
80.97% | 80.39% | 84.31% |
|
80.39% | 80.39% | 78.43% |
|
82.35% | 82.35% | 70.58% |
|
80.39% | 80.39% | 68.63% |
|
74.51% | 74.50% | 82.35% |
|
74.51% | 74.50% | 74.51% |
|
0.04% | 0.04% | 0.02% |
| I possess the ability to locate valuable health-related content online | |||
| Fully agree/Agree/Tend to agree | 96.08% | 96% | 98% |
| Disapprove | 3.92% | 4% | 2% |
| I am proficient in assessing health-related information obtained from the internet | |||
| Fully agree/Agree/Tend to agree | 82.35% | 90% | 86% |
| Disapprove | 17.65% | 10% | 14% |
| I am comfortable utilizing health-related information sourced from the internet. | |||
| Fully agree/Agree/Tend to agree | 86.27% | 90% | 80% |
| Disapprove | 13.73% | 10% | 20% |
| I began utilizing the internet to seek health-related information only following the onset of the COVID-19 pandemic | |||
| Fully agree/Agree/Tend to agree | 52% | 41% | 46% |
| Disapprove | 48% | 59% | 54% |
| Tele-visit | |||
| Did you know the definition of “Tele-visit” prior to today? | |||
| Yes | 45.10% | 20% | 50.98% |
| No | 54.90% | 78% | 47.06% |
| I thought it was something different | 0% | 2% | 1.96% |
| Have you ever used a telemedicine service in the past? | |||
| Yes/No | 13.73%/86.27% | 8.33%/91.67% | 6%/94% |
| If Yes, regarding your previous experiences with telemedicine, what is your level of satisfaction? | |||
| Very satisfied/Satisfied/Partially satisfied | 100% | 96% | 95.45% |
| Not at all satisfied | 0% | 4% | 4.55% |
Additionally, a survey on the perceived disadvantages and advantages of using the telemedicine option was recorded (see Table 2) [18,19,20].
Table 2.
Disadvantages and advantages of using telemedicine option.
| Question | Telehomecare | Standard Care |
|---|---|---|
| Disadvantages and limits | ||
| Because I believe that you don’t establish a personal relationship with the doctor | ||
| Fully agree/Agree/Tend to agree | 82.0% | 85.59% |
| Disapprove | 18.0% | 14.41% |
| Because I believe that it is not possible to ask the doctor all the questions | ||
| Fully agree/Agree/Tend to agree | 75.51% | 82.14% |
| Disapprove | 24.49% | 17.86% |
| The proposed technological tools are too difficult to use | ||
| Fully agree/Agree/Tend to agree | 78.43% | 77.78% |
| Disapprove | 21.57% | 22.22% |
| I think a tele-visit is NOT as reliable as a real visit | ||
| Fully agree/Agree/Tend to agree | 86.27% | 92.86% |
| Disapprove | 13.73% | 7.14% |
| I think I might have connection problems | ||
| Fully agree/Agree/Tend to agree | 66.7% | 50% |
| Disapprove | 33.3% | 50% |
| I’m not familiar enough with technology in general | ||
| Fully agree/Agree/Tend to agree | 68.63% | 60.71% |
| Disapprove | 31.37% | 39.29% |
| I would still need someone’s help during the visit (for connection, to hold the baby, etc.) and it’s not guaranteed that they will be available | ||
| Fully agree/Agree/Tend to agree | 68.63% | 67.86% |
| Disapprove | 31.37% | 32.14% |
| I fear there may be privacy issues | ||
| Fully agree/Agree/Tend to agree | 54.9% | 64.29% |
| Disapprove | 45.10% | 35.71% |
| Main reason why you decided to make yourself available to adopt the telemedicine service for your child’s discharge | ||
| It will save me time | ||
| Fully agree/Agree/Tend to agree | 90.0% | 85.11% |
| Disapprove | 10.0% | 14.89% |
| It will save me money (travel, permits, etc.) | ||
| Fully agree/Agree/Tend to agree | 87.76% | 85.11% |
| Disapprove | 12.24% | 14.89% |
| Because I could no longer care for the child in hospital (due to work, caring for other children, etc.) | ||
| Fully agree/Agree/Tend to agree | 66.7% | 89.36% |
| Disapprove | 33.33% | 10.64% |
| Because I think the child is better at home anyway | ||
| Fully agree/Agree/Tend to agree | 90.0% | 93.75% |
| Disapprove | 10% | 6.25% |
| Because I think this type of technology is now safe and useful | ||
| Fully agree/Agree/Tend to agree | 98.0% | 97.87% |
| Disapprove | 2.0% | 2.13% |
| Because I trust the doctors who proposed it to me | ||
| Fully agree/Agree/Tend to agree | 96.08% | 96.3% |
| Disapprove | 3.92% | 3.7% |
| Because I like experimenting with new technologies | ||
| Fully agree/Agree/Tend to agree | 96.08% | 88.4% |
| Disapprove | 3.92% | 11.54% |
| Because I didn’t want to say no to the ward doctors | ||
| Fully agree/Agree/Tend to agree | 43.14% | 40.74% |
| Disapprove | 56.86% | 59.26% |
| Because thanks to an active collaboration with the doctor, I am able to take care of my baby even at home | ||
| Fully agree/Agree/Tend to agree | 98.04% | 96.3% |
| Disapprove | 1.96% | 3.70% |
Exclusively within the TELE group, supplementary data were gathered post-intervention to assess user satisfaction and the perceived level of care utilizing the Tytocare device (see Table 3).
Table 3.
Satisfaction survey in using telemedicine in telehomecare group.
| Questions | Telehomecare |
|---|---|
| The information received upon discharge was clear regarding: | |
| Operation of Tytocare device | |
| No, not at all | 2.13% |
| Yes, but not as clear | 6.38% |
| Yes/Yes how much | 91.49% |
| Who would have contacted her | |
| No, not at all | 2.13% |
| Yes, but not as clear | 6.38% |
| Yes/Yes how much | 91.49% |
| When he would contact her | |
| No, not at all | 2.13% |
| Yes, but not as clear | 0% |
| Yes/Yes how much | 97.87% |
| How Tytocare should have been used | |
| No, not at all | 4.26% |
| Yes, but not as clear | 8.51% |
| Yes/Yes how much | 91.49% |
| How he should have followed the therapy | |
| No, not at all | 8.51% |
| Yes, but not as clear | 4.26% |
| Yes/Yes how much | 87.24% |
| What to do if the child gets worse | |
| No, not at all | 8.89% |
| Yes, but not as clear | 4.44% |
| Yes/Yes how much | 86.66% |
| Who to contact in case of need | |
| No, not at all | 2.17% |
| Yes, but not as clear | 8.70% |
| Yes/Yes how much | 89.13% |
| Satisfaction in using telemedicine | |
| How satisfied are you overall with the telehomecare you received? | |
| No, not at all | 0% |
| Yes/Yes how much | 100% |
| During telehomecare the doctors who treated the child were very scrupulous and caring | |
| Fully agree/Agree/Tend to agree | 96% |
| Disapprove | 4% |
| The doctor made me feel safe while continuing the therapy at home with tele-visits | |
| Fully agree/Agree/Tend to agree | 100% |
| Disapprove | 0% |
| The doctor made the experience during the tele-visits pleasant | |
| Fully agree/Agree/Tend to agree | 97.92% |
| Disapprove | 2.08% |
| I felt comfortable communicating with the professional using the telemedicine system | |
| Fully agree/Agree/Tend to agree | 97.87% |
| Disapprove | 2.13% |
| I was able to describe my child’s health condition during televisit | |
| Fully agree/Agree/Tend to agree | 97.87% |
| Disapprove | 2.13% |
| I managed to collect and share the required parameters with the doctor | |
| Fully agree/Agree/Tend to agree | 100% |
| Disapprove | 0% |
| I followed all the instructions I was given on what to do once I got home | |
| Fully agree/Agree/Tend to agree | 100% |
| Disapprove | 0% |
| I had no technical problems during the tele-visit (e.g., connection, hearing, seeing) | |
| Fully agree/Agree/Tend to agree | 100% |
| Disapprove | 0% |
| How do you rate the telemedicine experience? | |
| Poor/Fair | 0% |
| Good/very good | 100% |
| In light of your experience with Tytocare, if you were asked to use the Tytocare telemedicine device in the future, do you think you would still be willing to evaluate its use? | |
| No/More no that yes | 6.25% |
| Yes/More yes that no | 93.75% |
In the TELE and STAND groups, the surveys were handed out immediately after randomization and then collected at the 72 h point during in-person clinical assessment.
Within the group of patients who declined the telemedicine service, a self-administered survey was recorded to identify factors that might have impeded their engagement and utilization of the proposed technological tools (see Table 4).
Table 4.
Survey on reasons for rejecting the telemedicine option among non-telemedicine users.
| Question | No Telemedicine |
|---|---|
| Main reason why you decided NOT to make yourself available to adopt the Tytocare device for your child’s discharge | |
| Because I believe that you don’t establish a personal relationship with the doctor | |
| Fully agree/Agree/Tend to agree | 95.45% |
| Disapprove | 4.55% |
| Because I believe that it is not possible to ask the medical doctor all the questions | |
| Fully agree/Agree/Tend to agree | 93.18% |
| Disapprove | 6.82% |
| The proposed technological tools are too difficult to use | |
| Fully agree/Agree/Tend to agree | 84.09% |
| Disapprove | 15.91% |
| I think a tele-visit is NOT as reliable as a real visit | |
| Fully agree/Agree/Tend to agree | 97.73% |
| Disapprove | 2.27% |
| I think I might have connection problems | |
| Fully agree/Agree/Tend to agree | 68.18% |
| Disapprove | 31.82% |
| I’m not familiar enough with technology in general | |
| Fully agree/Agree/Tend to agree | 62.22% |
| Disapprove | 37.78% |
| I would still need someone’s help during the visit (for connection, to hold the baby, etc.) and it’s not guaranteed that they will be available | |
| Fully agree/Agree/Tend to agree | 69.57% |
| Disapprove | 30.43% |
| I fear there may be privacy issues | |
| Fully agree/Agree/Tend to agree | 68.89% |
| Disapprove | 31.11% |
| Because I don’t trust technologies | |
| Fully agree/Agree/Tend to agree | 65.22% |
| Disapprove | 34.78% |
| I think that only in hospital does my son receive the best care | |
| Fully agree/Agree/Tend to agree | 97.83% |
| Disapprove | 2.17% |
| Parent’s willingness to use the device in the future | |
| No/More no that yes | 59.18% |
| Yes/More yes that no | 40.82% |
In all patients, a self-administered survey on the satisfaction level of the hospitalization experience was also recorded (see Table 5).
Table 5.
Patient satisfaction level of the hospitalization experience [9] in telehomecare, standard care and no-telemedicine groups.
| Question | Telehomecare | Standard Care | No Telemedicine |
|---|---|---|---|
| The doctors who treated the child were very thorough and caring | |||
| Fully agree/Agree/Tend to agree | 96% | 100% | 100% |
| Disapprove | 4% | 0% | 0% |
| The doctors attending to the child were exceptionally meticulous and compassionate | |||
| Fully agree/Agree/Tend to agree | 100% | 100% | 100% |
| Disapprove | 0% | 0% | 0% |
| The parent believes that the child can only receive the best care in a hospital | |||
| Fully agree/Agree/Tend to agree | Not considered | 53.33% | 50.98% |
| Disapprove | 46.67% | 49.02% | |
| At times, the doctor treating the child did not pay attention to what the child or the caregiver was attempting to communicate | |||
| Fully agree/Agree/Tend to agree | 32% | 40%% | 50.98% |
| Disapprove | 68% | 60%% | 49.02% |
| The parent believes that the doctor was not as competent as they should have been. | |||
| Fully agree/Agree/Tend to agree | 90% | 100% | 90% |
| Disapprove | 10% | 0% | 10% |
| The parent is satisfied with the care received | |||
| No | 0% | 0% | 0% |
| Yes | 100% | 100% | 100% |
| Would you recommend this department to other patients? | |||
| No/More no that yes | 0% | 0% | 0% |
| Yes/More yes that no | 100% | 100% | 100% |
| Would you still choose this department for treatment? | |||
| No/More no that yes | 0% | 0% | 0% |
| Yes/More yes that no | 100% | 100% | 100% |
| How would you rate the care you received? | |||
| Poor/Fair | 0% | 0% | 0% |
| Good/very good | 100% | 100% | 100% |
A physician experience survey was also self-administered at the conclusion of the study and was taken into consideration for this study’s purpose (see Table 6).
Table 6.
Physician survey.
| Questions | Response % |
|---|---|
| How satisfied are you overall with the Tytocare process with patients? | |
|
0% |
|
3.85% |
|
21.15% |
|
75% |
| How many adults were present during the televisit? | |
|
65.22% |
|
34.78% |
| How well were the parents able to follow all the instructions provided for home care? | |
|
0% |
|
5.77% |
|
9.62% |
|
84.62% |
| Did the parents adhere to the agreed-upon time for the televisit?” | |
|
0% |
|
1.92% |
|
11.54% |
|
86.54% |
| Were there any technical problems during the tele-visit? | |
|
42.31% |
|
15.38% |
|
21.15% |
|
21.15% |
| How successful was the parent in collecting and sharing the required information and parameters? | |
|
1.92% |
|
3.85% |
|
23.08% |
|
71.15% |
| How comfortable did you feel communicating with your parent using the telemedicine system? | |
|
0% |
|
23.08% |
|
76.92% |
3. Data Analysis
Quantitative data were summarized using either mean and standard deviation (SD) or median and interquartile range (IQR), based on the data distribution assessed using the Shapiro–Wilk test. To test differences between groups, a Student t test or the one-way ANOVA were used. The significance was set at p-value less than 0.05. All data analyses were performed using Stata software version 16.1 (StataCorp, College Station, TX, USA).
4. Results
As reported in Figure 1, during the consecutive enrollment period, the project was presented to 153 hospitalized patients (86 males, 67 females, mean age 3.37 ± 4.0 years).
Among them, 102 patients accepted the telemedicine solution and were subsequently randomized, while the remaining 51 patients declined the telemedicine option.
4.1. Randomized Telehomecare and Standard Care Groups
A total of 102 children (59 males and 43 females, mean age of 3.36 ± 3.98 years), affected by respiratory diseases (56.9%) (bronchiolitis, pneumonia, asthma, upper airways disorders), abdominal pathologies (17.6%) (gastroenteritis, colitis, appendicitis, stones) and other pathologies (21.5%) (osteomyelitis, uro-genital and other infections, endocrine problems, burns) accepted the telemedicine service.
These patients were randomly assigned to the TELE group (n = 51) or the STAND group (n = 51), as illustrated in Figure 1.
4.1.1. Clinical Outcomes
In a comparable manner to the STAND group, a total of 51/51 (100%) children included in the TELE arm reached complete resolution of disease during the telemedicine intervention, without readmission to the hospital.
An adequate transmission of clinical parameters with mobile devices was obtained in all children. No significant technical problems occurred during telemonitoring (Table 3).
With home telemonitoring, the median length of hospital stay was 4 days (IQR 3–8) in the interventional group, significantly shorter than 7 days (IQR 5–9) in the STAND group (p = 0.01).
4.1.2. User Survey Results in Randomized Groups
All enrolled participants successfully completed the survey. Table 1 illustrates the survey questionnaire along with the corresponding responses.
The TELE and STAND groups exhibited no significant difference in terms of sociodemographic characteristics, as well as the parents’ proficiency in utilizing technologies, digital communication systems, and telehealth services.
In both groups, in most cases, the survey was completed by the mother (TELE: 84.32%, STAND: 94.12%) who had a regular job (TELE: 72.5%, STAND: 76.47%).
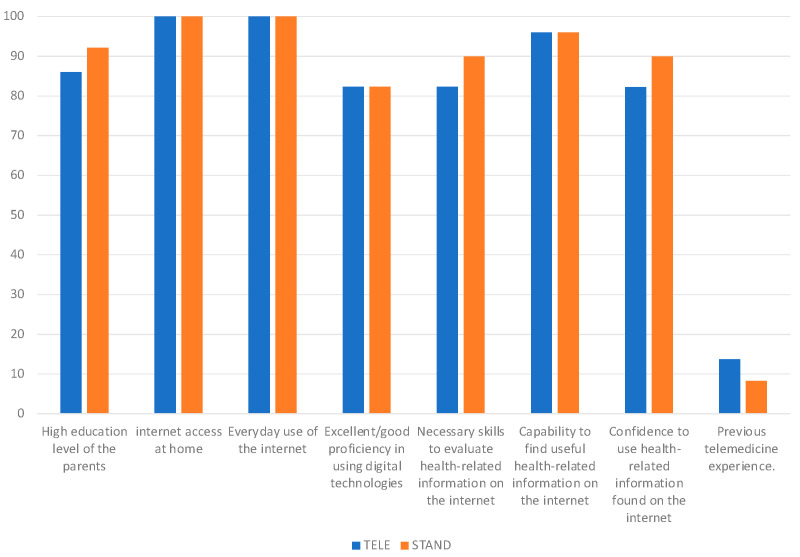
Respondents generally had a high level of education (TELE: 86.0%, STAND: 92.16%) and demonstrated excellent or good competence in using digital technologies (82.35%). Internet access at home was usually used every day (100%). Only 13.73% of cases in TELE and 8.33% in STAND had previous telemedicine experience.
In Figure 2, the main knowledge, attitudes and skills of the parents in using technologies, digital communication systems and telehealth services are shown.
Figure 2.
Parents’ knowledge, attitudes, and technological skills in utilizing technologies, digital communication systems, and telehealth services.
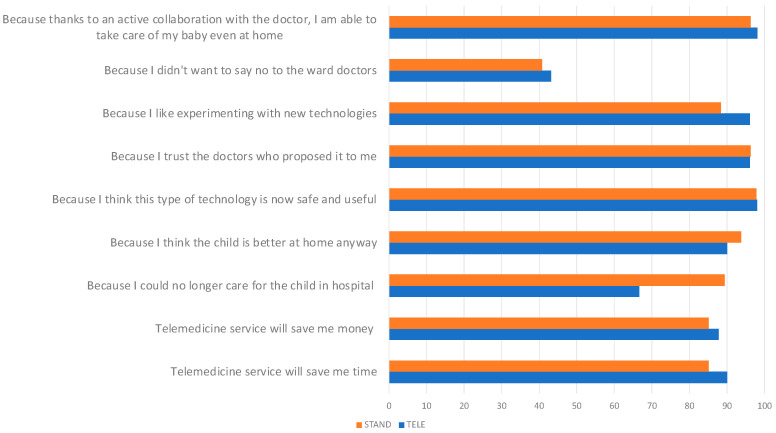
In Table 2, the disadvantages and advantages of using telemedicine options are reported. In both groups, the main possible limitation of telemedicine is the lack of personal contact with doctors, and in more than 80% of cases, a tele-visit was not considered as reliable as a real visit.
As reported in Figure 3, the main motivations for using telemedicine included time (90%) and money in travel and permits (87.76%), relevance to stay at home (90%), technology safety and utility (98%), significant trust in the professionalism of the service providers (96.9%).
Figure 3.
Motivations for using telemedicine.
In Table 3, the satisfaction survey for the TELE group in using the telemedicine option is presented. The TELE users were very satisfied or satisfied in all areas on training in using, including operational steps (91.49%), contact (91.49%), therapeutic indications (87.24%), support (89.13%).
All respondents reported satisfaction with the telemedicine experience (100%); no dissatisfaction was expressed (0%). In the 97.87% of cases, parents are able to correctly describe the child’s health information, sharing the parameters without technical problems (100%). Additionally, 93.75% of the respondents stated they would repeat the telemedicine experience.
4.2. No-Telemedicine Group
A total of fifty-one patients (27 males and 24 females), affected by respiratory diseases 64.7%, abdominal pathologies 13.7% and other disorders 21.6%, with a mean age of 3.47 ± 4.04 years, comprised the NO-TELE group.
There is no statistically significant difference in demographic data and types of diseases between the group that declined the telemedicine option and the groups that accepted the telemedicine solution. All patients achieved full recovery from the disease during their hospitalization.
Table 1 and Table 3 present the survey questionnaire along with the corresponding responses of patients in the NO-TELE group.
Upon comparison with the group that embraced the telemedicine option, no significant differences were observed in terms of age and demographic features. The majority demonstrated excellent or good competence in using digital technologies (78%) and reported regular daily Internet use at home (97.56%).
The primary reasons for declining the telemedicine option included the inability to establish a personal relationship with the medical doctor (95.45%) and the incapacity to ask the medical doctor questions directly (93.18%). Respondents expressed concerns about the reliability of tele-consultations compared to in-person visits (97.73%) and showed a preference for traditional hospitals as the optimal care structure (97.83%). Worries about privacy issues (68.89%), difficulties in using technology (84.09%), and potential technical problems (68.18%) were also cited as limiting factors. Despite the current refusal of the telemedicine option, 40.82% of cases did not rule out the possibility of using the service in the future.
4.3. Patient Satisfaction Level of the Hospitalization Experience
In Table 4, the survey results on the hospitalization experience in all groups are presented. In all, the level of patient satisfaction is high, with no significant differences observed between the groups.
4.4. Physician Survey Results
As reported in Table 6, 96.15% of physicians expressed satisfaction with the adopted system. During tele-visits, no or limited technical problems, immediately resolved (temporary audio problems), were detected in 78.85% of cases; in the remaining 21.15%, temporary connection problems were recorded. Comfortable communication (100%) and useful data sharing with parents (94.23%) were reported, with no issues in following-up instructions (94.24%) and with adequate adherence to the agreed-upon time (98.08%).
5. Discussion
Our study underscores the utility of user-friendly mobile medical devices, exemplified by the TytoCare™ system, in effectively reducing hospital stays while achieving optimal clinical outcomes comparable to standard care. The system showed proficient performance in transmitting clinical information during telehealth visits, earning high levels of satisfaction from both patients and physicians. These mobile medical devices serve as a valuable bridge between home and hospital, optimizing care pathways.
Hospitalization can be an inherently stressful experience for children, impacting behavioral and emotional responses with potential implications for health and developmental outcomes [21]. Hospitalized children may undergo a disconnection from their familiar family surroundings and recreational activities, navigating an environment where they encounter unfamiliar and invasive medical procedures [22]. These alterations can be perceived as traumatic events, eliciting stress responses. In certain instances, susceptibility to stress, clinical conditions, and care-related characteristics may contribute to the onset of Pediatric Medical Traumatic Stress, resulting in enduring negative psychological effects [23,24]. The risks associated with these stressors are particularly pronounced in cases of chronic illnesses, conditions involving frequent or prolonged hospitalizations, or in the presence of psychosocial vulnerability [25]. Furthermore, the hospitalization of a child is a stressful event for parents as well [24]. Parents often grapple with anxiety and depression during the hospitalization period, especially in families with children facing chronic pathologies [26,27], leading to significant implications for the child’s health and behavioral outcomes [24,26,27].
Improving the hospital discharge process as highlighted by the “European Association for Children in Hospital Charter” [7] is crucial in pediatric care, aligning with the imperative to discharge children promptly for their psychophysical well-being [28]. Telemedicine, as a bridge between home and hospital, emerges as a promising tool, though the literature on its role in early hospital discharge is limited [29,30]. Vesterby et al. [29] reported that telemedicine support shortens length of stay after fast-track hip replacement in adults. Minguez Clemente et al. [31] demonstrated that follow-up through a telemedicine program after early discharge from hospitalization is equally effective as conventional home follow-up in patients with chronic obstructive pulmonary disease. Our study contributes valuable insights by demonstrating a significant reduction in hospital stays through the use of a mobile medical device in a pediatric setting. This suggests that a telemedicine approach allows for quicker discharges without compromising clinical safety or physical outcomes, thereby enhancing the quality of children’s care.
Ensuring timely discharge and preventing readmissions are crucial indicators of effective integration between hospital and community services [32]. The use of a user-friendly mobile medical device not only led to a reduction in hospital stays but also ensured satisfactory clinical outcomes without instances of readmission, supporting the effectiveness of home telecare. This highlights the role of mobile remote presence devices as integrative tools for remote patient monitoring, supporting the evolution of family-centered care [30]. A hybrid “home–hospital” model could be seen as a prospective approach in pediatric care for “vulnerable” children, including those with chronic illnesses and medical fragility.
These populations, which have a high priority for health services and technological support systems, could greatly benefit from this approach to address their multiple health needs [8].
Our study participants expressed satisfaction with TytoCareTM, even if they were initially unfamiliar with the concept. The positive experiences reported, coupled with a willingness to recommend the service, emphasize the potential of these technologies in healthcare. Trust in professional service emerged as a crucial factor influencing user satisfaction and perceived care levels, underscoring the need for integrating technological innovation into medical training, as emphasized by Chastonay et al. [33].
Perceived benefits of telemedicine, including time and cost savings, reduced hospital stays, and technology utility and usability, align with the evolving landscape of healthcare delivery. While limitations were reported by some individuals opting against telemedicine, our findings overall support the positive impact of mobile medical devices in pediatric care, fostering patient satisfaction and efficient healthcare delivery. The telemedicine option leads to a lack of personal contact with one’s medical doctor during telemedicine services. These results confirm that some disadvantages of telehealth include limitations with performing comprehensive physical examinations with impersonal interactions with physicians [3].
Telemedicine must deal with many legal and regulatory obstacles [9]. Even though our users expressed limited privacy concerns, regulatory frameworks for telemedicine are insufficient, often lacking clarity [3]. The ethical responsibilities, conflict of interest considerations, and obligations to protect personal health information are the same for practicing telemedicine as they are for practicing in-person medicine; thus, regulatory, legal, and ethical considerations of telemedicine should be taken into account. However, at this time, particularly concerning healthcare and medical practice, uniform regulations at the European level are absent [3]. The wide range of norms and regulations governing practice and privacy contributes to confusion for providers involved in telemedicine practice [3].
According to the literature [34], we recorded high levels of physician satisfaction utilizing telemedicine. Telemedicine utilizing mobile devices can serve as an additional tool to facilitate a broader and more enduring adoption of telemedicine [34].
To fully harness the potential of telemedicine and remove the obstacles to its utilization, future research and initiatives are imperative. These should focus on enhancing the long-term satisfaction in using telemedicine and the cost-effectiveness of telemedicine services, ensuring unrestricted access to the internet, and establishing specific guidelines concerning data protection safety, informed consent, and professional liability [8].
6. Study Limitations
As a pilot study, this research was limited by the small sample size with various diseases at admission; thus, further studies with a larger number of patients are mandatory to confirm the positive role of user-friendly mobile medical devices in early hospital discharges, investigating potential variations among age groups (neonates, infants, children, and adolescents) and types of disease.
We present a randomized study to explore a transitional care program utilizing a user-friendly mobile medical device. Randomization alone did not completely remove the potential for systematic differences between treatment groups in this study. Enthusiasm for a new treatment may lead to improved outcomes being observed in this patient group, irrespective of the actual treatment efficacy. Thus, a blinded or masked trial can help limit bias. However, in some cases, such as in our protocol, the nature of the treatments under investigation makes blinding difficult. Therefore, to mitigate bias related to the open-label design, we applied a meticulous study design and randomization to patients/caregivers who agreed to participate in telemedicine. All steps of the protocol and randomization have been planned and recorded to ensure transparency at every stage, thereby facilitating reproducibility. Additionally, standardized eligibility criteria were applied before randomization.
Additionally, in order to better evaluate user acceptance, additional aspects of user and physician satisfaction should be explored further, also considering that the final timeline of the project and the availability of users and professionals to participate can certainly impact the reported satisfaction levels. The long-term use of the system will help us better understand the factors that most significantly influence the level of satisfaction and adaptability of this technological approach into existing processes, workflows, and practices.
Finally, the viability of the telemedicine service needs to be assessed in relation to cost–benefit considerations, considering both direct and indirect costs for patients, families, organizations, and the healthcare system [3,27,34,35]. While this project is currently in the exploratory phase, economic evaluation has not yet been incorporated but is planned as a future objective. Specifically, we will evaluate the sustainability of the telemedicine approach, taking into consideration the value that it can generate in social, economic–administrative, and environmental contexts, while considering both the professional/hospital context and that of the user.
7. Conclusions
In conclusion, our study supports the idea that user-friendly mobile medical devices may provide a valuable tool for facilitating early hospital discharges in a pediatric setting. This approach not only maintains a high level of care but also effectively reduces the length of stay, enhancing the quality of children’s care. The integration of mobile medical devices represents a significant advancement in clinical tools to facilitate family-centered care for children, aligning with the vision of HaH healthcare and the concept of a virtual public hospital in pediatrics.
Acknowledgments
The authors thank (1) Valentina Frezzotti for study participation; (2) Multimed S.r.l for supporting this project; (3) Nicola Bladen for English revision of the manuscript.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/children11060683/s1: Supplementary Material S1: Certificate of conformity and technical datasheet of TytoCare™.
Author Contributions
G.Z.: conceptualization, methodology, writing—original draft, writing—review and editing, supervision; M.M.: conceptualization, methodology, writing—original draft, writing—review and editing, supervision; L.F. (Laura Fiori): data collection, investigations, writing—original draft, writing—review; P.E.: data collection, investigations, writing—original draft, writing—review; F.D.: data collection, investigations, writing—original draft, writing—review; C.Z.: data collection, investigations, writing—original draft, writing—review; L.F. (Laura Folgori): data collection, investigations, writing—original draft, writing—review; A.M.: data collection, investigations, writing—original draft, writing—review; D.B.: formal statistical analysis, writing—original draft, writing—review; C.G.: methodology, investigations, writing—original draft, writing—review; M.P.: methodology, investigations, writing—original draft, writing—review; L.M.: methodology, investigations, writing—original draft, writing—review; G.I.: methodology, formal statistical analysis, writing—original draft, writing—review; D.D.: data collection, investigations, writing—original draft, writing—review; V.F.: data collection, investigations, writing—original draft, writing—review; P.C.: data collection, investigations, writing—original draft, writing—review, E.Z.: data collection, writing—original draft, writing—review, writing—review; G.P.: data collection, writing—original draft, writing—review, writing—review; V.C.: conceptualization, methodology, writing—original draft, writing—review, writing—review and editing, supervision. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Parental consent was obtained from all participants or their responsible guardians after explaining the nature of the study, which was conducted following the guidelines of the Declaration of Helsinki and approved by the Ethics Committee Milano Area 1 (Protocol number n. 0033846, date 3 August 2022). A medical team of 14 professionals were trained in the use of the Tytocare™ device and voluntarily agreed to participate in the project.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Project performed within the MUSA—Multilayered Urban Sustainability Action—project, funded by the European Union—NextGenerationEU, under the National Recovery and Resilience Plan (NRRP, project code ECS00000037) Mission 4 Component 2 Investment Line 1.5: Strengthening of research structures and creation of R&D “innovation ecosystems”, set up of “territorial leaders in R&D” and with the extraordinary research support of Fondazione Romeo and Enrica Invernizzi (Milan, Italy).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bird M., Li L., Ouellette C., Hopkins K., McGillion M.H., Carter N. Use of Synchronous Digital Health Technologies for the Care of Children with Special Health Care Needs and Their Families: Scoping Review. JMIR Pediatr. Parent. 2019;2:e15106. doi: 10.2196/15106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor K. How Digital Technology Is Transforming Health and Social Care. Deloitte; London, UK: 2015. Connected health. [Google Scholar]
- 3.Gajarawala S.N., Pelkowski J.N. Telehealth Benefits and Barriers. J. Nurse Pract. 2021;17:218–221. doi: 10.1016/j.nurpra.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barbosa W., Zhou K., Waddell E., Myers T., Dorsey E.R. Improving Access to Care: Telemedicine Across Medical Domains. Annu. Rev. Public Health. 2021;42:463–481. doi: 10.1146/annurev-publhealth-090519-093711. [DOI] [PubMed] [Google Scholar]
- 5.Haleem A., Javaid M., Singh R.P., Suman R. Medical 4.0 technologies for healthcare: Features, capabilities, and applications. Internet Things Cyber-Physical Syst. 2022;2:12–30. doi: 10.1016/j.iotcps.2022.04.001. [DOI] [Google Scholar]
- 6.Kanagala S.G., Gupta V., Kumawat S., Anamika F., McGillen B., Jain R. Hospital at home: Emergence of a high-value model of care delivery. Egypt. J. Intern. Med. 2023;35:21. doi: 10.1186/s43162-023-00206-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGillion M., Yost J., Turner A., Bender D., Scott T., Carroll S., Ritvo P., Peter E., Lamy A., Furze G., et al. Technology-Enabled Remote Monitoring and Self-Management—Vision for Patient Empowerment Following Cardiac and Vascular Surgery: User Testing and Randomized Controlled Trial Protocol. JMIR Res. Protoc. 2016;5:e149. doi: 10.2196/resprot.5763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zuccotti G., Calcaterra V., Foppiani A. Present and future of telemedicine for pediatric care: An Italian regional experience. Ital. J. Pediatr. 2023;49:10. doi: 10.1186/s13052-023-01408-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mannarino S., Calcaterra V., Fini G., Foppiani A., Sanzo A., Pisarra M., Infante G., Marsilio M., Raso I., Santacesaria S., et al. A pediatric telecardiology system that facilitates integration between hospital-based services and community-based primary care. Int. J. Med Inform. 2024;181:105298. doi: 10.1016/j.ijmedinf.2023.105298. [DOI] [PubMed] [Google Scholar]
- 10.Fabbrizio A., Fucarino A., Cantoia M., De Giorgio A., Garrido N.D., Iuliano E., Reis V.M., Sausa M., Vilaça-Alves J., Zimatore G., et al. Smart Devices for Health and Wellness Applied to Tele-Exercise: An Overview of New Trends and Technologies Such as IoT and AI. Healthcare. 2023;11:1805. doi: 10.3390/healthcare11121805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haskel O., Itelman E., Zilber E., Barkai G., Segal G. Remote Auscultation of Heart and Lungs as an Acceptable Alternative to Legacy Measures in Quarantined COVID-19 Patients—Prospective Evaluation of 250 Examinations. Sensors. 2022;22:3165. doi: 10.3390/s22093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagner R., Lima T.C., da Silva M.R.T., Rabha A.C.P., Ricieri M.C., Fachi M.M., Afonso R.C., Motta F.A. Assessment of Pediatric Telemedicine Using Remote Physical Examinations with a Mobile Medical Device: A Nonrandomized Controlled Trial. JAMA Netw. Open. 2023;6:e2252570. doi: 10.1001/jamanetworkopen.2022.52570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDaniel N.L., Novicoff W., Gunnell B., Gordon D.C. Comparison of a Novel Handheld Telehealth Device with Stand-Alone Examination Tools in a Clinic Setting. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2019;25:1225–1230. doi: 10.1089/tmj.2018.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Notario P.M., Gentile E., Amidon M., Angst D., Lefaiver C., Webster K. Home-Based Telemedicine for Children with Medical Complexity. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2019;25:1123–1132. doi: 10.1089/tmj.2018.0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. [(accessed on 19 May 2024)]. Available online: http://www.aal-europe.eu/wp-content/uploads/2020/02/vINCI-Call-2017-DIGITAL-SKILLS-QUESTIONNAIRE-END-USERS.pdf.
- 16.Standard Specification for Infrared Thermometers for Intermittent Determination of Patient Temperature. ASTM; West Conshohocken, PA, USA: 2023. [(accessed on 22 May 2024)]. Available online: https://www.astm.org/e1965-98r23.html. [Google Scholar]
- 17.Medical Electrical Equipment—Part 2-56: Particular Requirements for Basic Safety and Essential Performance of Clinical Thermometers for Body Temperature Measurement. ISO; Geneva, Switzerland: 2017. [(accessed on 22 May 2024)]. Available online: https://www.iso.org/standard/75005.html. [Google Scholar]
- 18.Vuorikari R., Kluzer S., Punie Y. DigComp 2.2: The Digital Competence Framework for Citizens—With New Examples of Knowledge, Skills, and Attitudes, EUR 31006 EN. Publications Office of the European Union; Luxembourg: 2022. [DOI] [Google Scholar]
- 19.Bravo G., Del Giudice P., Poletto M., Battistella C., Conte A., De Odorico A., Lesa L., Menegazzi G., Brusaferro S. Validazione Della Versione Italiana del Questionario di Alfabetizzazione Sanitaria Digitale (IT-eHEALS). Bollettino Epidemiologico Nazionale. 2018. [(accessed on 20 February 2019)]. Available online: https://www.epicentro.iss.it/ben/2018/luglio-agosto/2.
- 20.Bonn M. The effects of hospitalisation on children: A review. Curationis. 1994;17:20–24. doi: 10.4102/curationis.v17i2.1384. [DOI] [PubMed] [Google Scholar]
- 21.Gomes G.L.L., Fernandes M.d.G.M., da Nóbrega M.M.L. Hospitalization anxiety in children: Conceptual analysis. Ansiedade da hospitalização em crianças: Análise conceitual. Rev. Bras. Enferm. 2016;69:940–945. doi: 10.1590/0034-7167-2015-0116. [DOI] [PubMed] [Google Scholar]
- 22.Al Jowf G.I., Ahmed Z.T., An N., Reijnders R.A., Ambrosino E., Rutten B.P.F., de Nijs L., Eijssen L.M.T. A Public Health Perspective of Post-Traumatic Stress Disorder. Int. J. Environ. Res. Public Health. 2022;19:6474. doi: 10.3390/ijerph19116474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Commodari E. Children staying in hospital: A research on psychological stress of caregivers. Ital. J. Pediatr. 2010;36:40–49. doi: 10.1186/1824-7288-36-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oh D.L., Jerman P., Marques S.S., Koita K., Boparai S.K.P., Harris N.B., Bucci M. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18:83. doi: 10.1186/s12887-018-1037-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coyne I. Children’s Experiences of Hospitalization. J. Child Health Care. 2006;10:326–336. doi: 10.1177/1367493506067884. [DOI] [PubMed] [Google Scholar]
- 26.Brazil K., Krueger P. Patterns of family adaptation to childhood asthma. J. Pediatr. Nurs. 2002;17:167–173. doi: 10.1053/jpdn.2002.124110. [DOI] [PubMed] [Google Scholar]
- 27.Joint Improvement Team Scotland Delayed Discharge. [(accessed on 14 March 2015)]. Available online: https://www.alliance-scotland.org.uk/blog/resources/joint-improvement-team-legacy-report/
- 28.Vesterby M.S., Pedersen P.U., Laursen M., Mikkelsen S., Larsen J., Søballe K., Jørgensen L.B. Telemedicine support shortens length of stay after fast-track hip replacement. Acta Orthop. 2017;88:41–47. doi: 10.1080/17453674.2016.1256939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franck L.S., O’Brien K. The evolution of family-centered care: From supporting parent-delivered interventions to a model of family integrated care. Birth Defects Res. 2019;111:1044–1059. doi: 10.1002/bdr2.1521. [DOI] [PubMed] [Google Scholar]
- 30.Clemente P.M., Pascual-Carrasco M., Hernandez C.M., de Molina R.M., Arvelo L.A., Cadavid B., Lopez F., Sanchez-Madariaga R., Sam A., Alonso A.T., et al. Follow-up with Telemedicine in Early Discharge for COPD Exacerbations: Randomized Clinical Trial (TELEMEDCOPD-Trial) COPD. 2021;18:62–69. doi: 10.1080/15412555.2020.1857717. [DOI] [PubMed] [Google Scholar]
- 31.Kokorelias K.M., Gignac M.A.M., Naglie G., Cameron J.I. Towards a universal model of family centered care: A scoping review. BMC Heal. Serv. Res. 2019;19:564. doi: 10.1186/s12913-019-4394-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coffey A., Leahy-Warren P., Savage E., Hegarty J., Cornally N., Day M.R., Sahm L., O’connor K., O’doherty J., Liew A., et al. Interventions to Promote Early Discharge and Avoid Inappropriate Hospital (Re)Admission: A Systematic Review. Int. J. Environ. Res. Public Health. 2019;16:2457. doi: 10.3390/ijerph16142457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Han E.-R., Yeo S., Kim M.-J., Lee Y.-H., Park K.-H., Roh H. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: An integrative review. BMC Med Educ. 2019;19:460. doi: 10.1186/s12909-019-1891-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoff T., Lee D.-R.D. Physician Satisfaction with Telehealth: A Systematic Review and Agenda for Future Research. Qual. Manag. Heal. Care. 2022;31:160–169. doi: 10.1097/qmh.0000000000000359. [DOI] [PubMed] [Google Scholar]
- 35.Bell-Aldeghi R., Gibrat B., Rapp T., Chauvin P., Le Guern M., Billaudeau N., Ould-Kaci K., Sevilla-Dedieu C. Determinants of the Cost-Effectiveness of Telemedicine: Systematic Screening and Quantitative Analysis of the Literature. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2023;29:1078–1087. doi: 10.1089/tmj.2022.0161. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.