Abstract
Background
Children living in food insecure households have poorer mental health outcomes compared with their food-secure peers; however, the relationship between the severity of food insecurity and diagnosed mental health conditions in young children remains unknown. This study examined the association between household food insecurity and reported diagnosed mental health conditions among children aged 5–11 years in Canada.
Methods
This study included 16 216 children aged 5–11 years living in Canada, from the 2019 Canadian Health Survey on Children and Youth. We measured household food insecurity using the Household Food Security Survey Module. We measured diagnosed mental health conditions by parent/caregiver report of health professional-diagnosed anxiety, depression, autism spectrum disorder or attention-deficit/hyperactive disorder. We developed a multivariable logistic regression model to assess the association between severities of food insecurity and mental health, controlling for potentially confounding variables.
Results
17.0% of children lived in households reporting some level of food insecurity (5.4% marginal, 8.0% moderate and 3.6% severe). The prevalence of at least one diagnosed mental health condition in the same population was 10.9%. After adjusting for sociodemographic characteristics, children from marginal, moderate and severe food insecure households had a 1.39 (95% CI 0.99 to 1.97), 1.46 (95% CI 1.13 to 1.89) and 1.67 (95% CI 1.18 to 2.35) increased odds of having a diagnosed mental health condition, respectively.
Conclusion
Household food insecurity is associated with an increased presence of diagnosed mental health conditions in children aged 5–11 years. This study adds to the body of research showing that social and economic inequities, including household food insecurity, negatively impact the health of children.
Keywords: mental health, epidemiology, nutrition & dietetics, paediatrics, public health, food insecurity
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study analysed a large sample that was representative of the broader Canada population of children aged 5–11, so results are generalisable across this population.
This study was able to control for a variety of sociodemographic, family and economic variables, including parent/caregiver mental health, which reduces the risk of confounding by another variable.
This study relies on parent/caregiver reports of household food insecurity and child mental health, which may not reflect true levels of food insecurity and mental health diagnoses.
This is a cross-sectional study and is, therefore, unable to determine whether household food insecurity causes increased mental health diagnoses among children.
Background
The prevalence of mental health conditions in children and youth is estimated at about one in five in Canada.1 Prior to COVID-19, previous studies showed an increasing trends in the prevalence of some mental health conditions and developmental disorders, particularly attention-deficit/hyperactive disorder (ADHD) in boys, and in the perceived need for professional help over the past 30 years.2 Likewise, data from a nationally representative sample in Canada showed an increased prevalence of poor/fair mental health, anxiety and depression disorders, and increased mental health services since 2011.3 Since 2020, emerging evidence indicates the COVID-19 pandemic likely exacerbated mental health issues in children and youth.4
Longitudinal research has found that mental health conditions in adolescence can have adverse health impacts in later life, such as lower self-reported general health and an increased likelihood of suicide in adulthood.5 6 In addition to direct harms to individuals, there is a burden of mental illness on families and communities, including societal and economic costs.7 To reduce the immediate and long-term impacts associated with these conditions, understanding key risk factors and preventing mental health conditions at an earlier age is a priority for public health.
A key social determinant of health is food insecurity. Broadly defined, food insecurity is the inability or uncertainty about being able to acquire or consume an adequate diet quality or sufficient quantity of food in socially acceptable ways.8 In Canada, food insecurity is measured and monitored as a household’s financial ability to access adequate food and encompasses a range of experiences from worrying about running out of food before there is money to buy more, to compromising on the quality or quantity of food due to lack of money, to not eating for whole days due to lack of money to buy food. The prevalence of household food insecurity in Canada is high, particularly among households with children.9 It is estimated that 1 in 4, or 1.8 million, children under the age of 18 in Canada lived in food insecure households in 2022.9 10 Food insecurity in Canada is linked to compromised diets in children,11 which negatively impacts child growth and development.12 Beyond diet, exposure to adverse childhood experiences can trigger stress responses, which impact brain development and increase the risk of poor mental health through adulthood.13
Despite the high prevalence of food insecurity among children in Canada, there is limited Canadian research on the impacts of food insecurity on the mental health of young children. In longitudinal research, food insecurity in early childhood has been linked to psychosocial problems, depression and suicide in subsequent years.14 15 A recent cross-sectional study showed greater mental healthcare use among children living in food insecure households in Ontario.16 Another recent cross-sectional study using population survey data shows poorer mental health among food insecure Canadian children and adolescents.17 However, this study classifies children as food insecure solely based on the child-referenced items in the household food insecurity questionnaire, which arguably misclassifies many children living in food insecure households (as indicated by an affirmative response to at least one adult-referenced item) as ‘food secure’. Research from the USA has shown families of individuals with autism spectrum disorder (ASD) or ADHD experience higher levels of food insecurity due to multiple social and biological mechanisms.18 19 For example, parents of children with ASD spend more money in out-of-pocket healthcare expenses than those without ASD, impacting household finances.20 No previous Canadian research has used a population-representative sample of young children to examine the relationship between severities of household food insecurity and diagnosed mental health conditions while controlling for key confounding factors such as parent mental health.
We drew on the latest national population health survey of Canadian children, the 2019 Canadian Health Survey on Children and Youth (CHSCY),21 to examine the association between household food insecurity and parent/caregiver reports of health professional-diagnosed mental health conditions in children between the ages of 5 and 11 years while controlling for key factors of socioeconomic and family well-being. This study builds on prior knowledge by examining a younger age group, multiple levels of household food insecurity and the association with specific mental health conditions and developmental disorders. Given the personal, economic and social burden of mental illness in Canada and its increase in children and youth since the COVID-19 pandemic,4 it is crucial to understand early intervention points that could be targeted through public health policies to help mitigate future burdens.
Methods
Study participants
We examined Canadian children 5–11 years, whose parent or caregiver responded to the 2019 CHSCY. The CHSCY is a national health survey run by Statistics Canada that represents 98% of Canada’s children and youth aged 1–17 years as of 31 January 2019, who lived in private dwellings across Canada’s 10 provinces and 3 territories.21 The survey sampling frame excluded children living on First Nation reserves, other Indigenous settlements, foster homes or children and youth who were institutionalised. Statistics Canada stratified the CHSCY population sample by subprovincial geographic strata and age group (1–4 years, 5–11 years and 12–17 years). Participants completed the survey predominantly online (70.0%) while 26.4% completed it by phone with an interviewer; the remaining 3.6% completed the survey in both modalities.22 For children younger than 12 years, the person most knowledgeable (PMK) of the sampled child completed the survey. PMKs were the birth parent for 97% of participants. This paper refers to a child’s PMK as their ‘parent/caregiver’. Parents/caregivers reported on multiple measures of their child’s health and well-being. The response rate for children 5–11 years was 57.8%. To ensure national representation of the population in the survey sample, Statistics Canada provides weighted and bootstrapping values to conduct analyses. A total of 16 694 children aged 5–11 participated in CHSCY. We excluded children from our study sample if they were missing any exposure or outcome data used in the study, leaving a final analytical sample of 16 216 children.
Exposure: household food insecurity
The main exposure was the severity of household food insecurity, measured using the validated 18-question Household Food Security Survey Module (HFSSM).23 Questions on the HFSSM measured a gradient of experiences related to food insecurity over the previous 12 months, from worrying about food running out to not eating for a whole day due to lack of money to buy more food.21 We used established definitions to categorise children as food secure, marginally food insecure, moderately food insecure or severely food insecure based on the number of affirmative answers on the HFSSM.24 Food secure indicates no difficulty with income-related food access, marginally food insecure is defined as exactly one indication of difficulty with income-related food access (eg, worried food would run out), moderately food insecure indicates compromise in the quality and/or the quantity of food consumed and lastly, severely food insecure indicates reduced food intake and disrupted eating patterns.24 In sensitivity analyses, we used a dichotomised exposure of food secure or food insecure (marginal, moderate or severe).
Outcome: diagnosed mental health conditions
The primary outcome of this study was parent/caregiver report of a mental health condition that is expected to last or has already lasted 6 months or more and was diagnosed by a health professional. We categorised children as having any diagnosed mental health condition if their parent/caregiver responded affirmatively to at least one of four questions related to the following long-term conditions: (1) ‘An anxiety disorder, such as a phobia or obsessive–compulsive disorder or a panic disorder’; (2) ‘A mood disorder such as depression, bipolar disorder, mania or dysthymia’; (3) ‘Attention deficit disorder or attention deficit hyperactivity disorder, also known as ADD or ADHD’ or (4) ‘Autism spectrum disorder, also known as autism, autistic disorder, Asperger’s disorder or pervasive developmental disorder’. We also analysed three secondary outcomes. We assessed the associations between food insecurity and autism spectrum disorder and ADHD as two separate outcomes. We assessed anxiety disorder and mood disorder grouped together because small sample sizes of children with these outcomes precluded analysing them separately. As a sensitivity analysis, we combined the three levels of food insecurity together to create a dichotomous exposure variable and analysed its association with the primary outcome: having any of the four mental health outcomes.
Covariates
We identified several potential confounding variables a priori in the existing literature based on their established association with household food insecurity or child health outcomes.9 14 25–30 Covariates included sex at birth (male, female), age (years), highest parental educational attainment (high school or less, college/trades, bachelor’s or more), parent/caregiver-reported household income adjusted for household size, parent/caregiver self-perceived mental health (excellent/very good, good, fair/poor), race and ethnic origin (white/non-racialized, black, East Asian, Indigenous, Latin American, other/multiple, South Asian, Southeast Asian/Filipino and West Asian/Arab), immigration status (non-immigrant, immigrant/non-permanent resident) and parent divorce/separation (yes, no).
Statistical analysis
We calculated the weighted prevalence of mental health conditions and sociodemographic characteristics across food security categories and performed χ2 tests for categorical variables and ANOVA for continuous variables to assess statistically significant differences between covariate groups.
We created bivariate logistic regression models to estimate the unadjusted associations between each covariate and the mental health conditions. We created multivariable logistic regression models to estimate the association between food insecurity and mental health conditions, adjusting for age, sex, household income divided by the square root of the number of household members to adjust for household size,31 highest level of parental educational attainment, parent self-perceived mental health, race or ethnic origin and Indigenous identity, child immigration status and parent/caregiver divorce or separation.
To account for the complex survey design, in all analyses, we used PROC SURVEY commands in SAS with bootstrap weights and bootstrap replications (n=1000) provided by Statistics Canada. We assessed collinearity using variance inflation factors and none exceeded a value of 2, indicating no significant collinearity. We conducted a sensitivity analysis with food security collapsed into two categories: food secure versus not food secure. We conducted all analyses by using SAS Enterprise Guide (V.8.2).
Patient and public involvement
This study uses secondary data from a survey previously conducted by Statistics Canada. All participant identifiers had been removed from the data so it was not possible to involve participants in the development of the research question, outcome measures, study design, conduct of the study or dissemination of the results.
Results
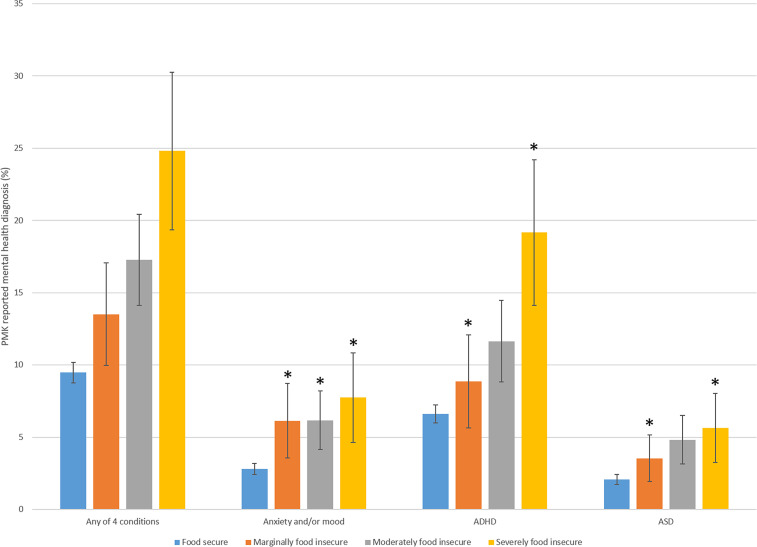
The total sample of Canadian children between the ages of 5 and 11 years included in this study was 16 216. The prevalence of household food insecurity in our sample was 17.0%; 5.4% were marginally food insecure, 8.0% were moderately food insecure and 3.6% were severely food insecure. The prevalence of any parent/caregiver-reported diagnosed mental health condition in our sample was 10.9% (8.4% reported a single condition, 2.5% reported two or more conditions); 2.5% had ASD, 7.6% had ADHD, 3.4% had anxiety or depression (figure 1).
Figure 1.
Prevalence of diagnosed mental health conditions in children 5–11, by food security status; Canada, 2019. *Interpret estimate with caution due to a coefficient of variation greater than 15%. ADHD, attention-deficit/hyperactive disorder; ASD, autism spectrum disorder; PMK, person most knowledgeable.
There were significant differences in most sociodemographic characteristics across food insecurity categories (table 1). Children in households with higher levels of food insecurity tended to have lower household income, lower levels of parent education, were more likely to identify as black or Indigenous, were more likely to be born in Canada, were more likely to have a parent/caregiver with fair or poor mental health and were more likely to have experienced parent/caregiver divorce or separation (table 1). There were no significant differences in age or sex.
Table 1.
Characteristics of study population of children age 5–11, by food security status; Canada, 2019
| Characteristics | Total | Food secure | Marginally food insecure | Moderately food insecure | Severely food insecure | P value for differences across groups |
| Age (mean years) | 8.0 | 8.0 | 7.9 | 8.0 | 8.2 | 0.0883 |
| Sex | ||||||
| Female | 48.7 | 48.6 | 53.4 | 47.0 | 49.5 | 0.2253 |
| Male | 51.3 | 51.4 | 46.6 | 53.0 | 50.5 | 0.2253 |
| Household income adjusted for household size (mean dollars) | 52 786 | 57 781 | 31 365 | 28 355 | 23 969 | <0.0001 |
| Highest parental education | ||||||
| High school or less | 13.6 | 10.7 | 22.8 | 28.6 | 33.1 | <0.0001 |
| College/trades | 38.3 | 36.6 | 42.8 | 48.0 | 49.5 | <0.0001 |
| Bachelor’s or more | 48.2 | 52.8 | 34.3 | 23.4 | 17.4 | <0.0001 |
| Race and ethnic origin | ||||||
| Black | 5.6 | 4.7 | 8.4 | 10.9 | 8.3 | <0.0001 |
| East Asian | 4.7 | 5.2 | 3.1 | 2.9 | 0.6 | <0.0001 |
| Indigenous | 5.1 | 3.9 | 10.5 | 9.3 | 15.8 | <0.0001 |
| Latin American | 1.1 | 1.0 | 2.6 | 2.1 | 0.8 | <0.0001 |
| Other/multiple | 2.1 | 1.9 | 4.2 | 3.3 | 1.8 | <0.0001 |
| South Asian | 7.1 | 7.6 | 6.4 | 4.8 | 1.5 | <0.0001 |
| Southeast Asian/Filipino | 4.1 | 3.8 | 7.9 | 6.4 | 2.0 | <0.0001 |
| West Asian/Arab | 3.2 | 3.2 | 3.8 | 2.8 | 4.0 | <0.0001 |
| White/non-racialised | 66.8 | 68.7 | 53.2 | 57.4 | 65.2 | <0.0001 |
| Child immigration status | ||||||
| Immigrant/non-perm resident | 9.0 | 8.8 | 15.0 | 8.0 | 4.9 | <0.0001 |
| Not immigrant/non-perm resident | 91.0 | 91.2 | 85.0 | 92.0 | 95.1 | <0.0001 |
| Experience parental separation | ||||||
| Experienced separation/divorce | 18.8 | 15.9 | 25.6 | 32.1 | 46.2 | <0.0001 |
| Never experienced separation/divorce | 81.2 | 84.1 | 74.4 | 67.9 | 53.8 | <0.0001 |
| PMK mental health | ||||||
| Excellent/very good | 71.6 | 74.6 | 66.7 | 56.9 | 40.7 | <0.0001 |
| Good | 22.8 | 21.2 | 26.3 | 32.9 | 33.1 | <0.0001 |
| Fair/poor | 5.6 | 4.2 | 7.0 | 10.2 | 26.3 | <0.0001 |
PMK, person most knowledgeable.
Figure 1 shows the prevalence of health professional-diagnosed mental health conditions by household food insecurity status. The survey-weighted percentage of children aged 5–11 with a mental health diagnosis was 9.5% in food secure households, 13.5% in marginally, 17.3% in moderately and 24.8% in severely food insecure households.
In the unadjusted model of our primary outcome, household food insecurity was dose-dependently associated with increased odds of having a mental health condition (table 2). After adjusting for confounding factors, the effect sizes and the dose-dependent relationship were diminished, yet a significant association remained for children living in moderately and severely food insecure households, who had a 1.46 (95% CI 1.13 to 1.89) and 1.67 (95% CI 1.18 to 2.35) higher risk of having any diagnosed mental health condition, respectively, compared with children living in food secure households (table 2).
Table 2.
Unadjusted and adjusted logistic regression models of the association between household food insecurity status and any diagnosed mental health condition
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Household food security | ||
| Food secure | REF | REF |
| Marginally food insecure | 1.49 (1.08 to 2.06) | 1.39 (0.99 to 1.97) |
| Moderately food insecure | 1.99 (1.58 to 2.52) | 1.46 (1.13 to 1.89) |
| Severely food insecure | 3.15 (2.32 to 4.27) | 1.67 (1.18 to 2.35) |
| Age (years) | 1.24 (1.20 to 1.29) | 1.25 (1.21 to 1.30) |
| Sex | ||
| Female | REF | REF |
| Male | 2.44 (2.08 to 2.87) | 2.70 (2.29 to 3.19) |
| Household income (adjusted for household size, per CAD$10000) | 0.96 (0.94 to 0.98) | 0.99 (0.97 to 1.01) |
| Highest level parent education | ||
| High school or less | REF | REF |
| College/trades | 0.80 (0.65 to 0.98) | 0.97 (0.78 to 1.19) |
| University or more | 0.49 (0.40 to 0.60) | 0.80 (0.63 to 1.01) |
| Parent’s mental health status | ||
| Excellent/very good | REF | REF |
| Good | 2.33 (1.96 to 2.77) | 1.95 (1.63 to 2.34) |
| Fair/poor | 4.34 (3.45 to 5.46) | 3.60 (2.80 to 4.63) |
| Race and ethnic origin | ||
| White/non-racialised | REF | REF |
| Black | 0.79 (0.57 to 1.09) | 0.83 (0.58 to 1.18) |
| East Asian | 0.58 (0.39 to 0.86) | 0.78 (0.51 to 1.18) |
| Indigenous | 1.58 (1.20 to 2.10) | 1.11 (0.83 to 1.48) |
| Latin American | 0.56 (0.25 to 1.24) | 0.67 (0.30 to 1.51) |
| Other/multiple | 0.74 (0.42 to 1.28) | 0.67 (0.38 to 1.20) |
| South Asian | 0.29 (0.19 to 0.43) | 0.42 (0.28 to 0.65) |
| Southeast Asian/Filipino | 0.53 (0.33 to 0.85) | 0.68 (0.41 to 1.14) |
| West Asian/Arab | 0.35 (0.17 to 0.71) | 0.46 (0.21 to 1.02) |
| Immigration status | ||
| Non-immigrant | REF | REF |
| Immigrant/non-permanent resident | 0.35 (0.24 to 0.52) | 0.47 (0.31 to 0.72) |
| Divorce/separation | ||
| No | REF | REF |
| Yes | 2.26 (1.90 to 2.68) | 1.47 (1.22 to 1.77) |
Regarding the secondary outcomes, in the unadjusted analysis of mood and/or anxiety disorders, each level of food insecurity was associated with over twice the odds of a mood and/or anxiety disorder. However, adjusting for confounding factors attenuated each association, especially the association with severe food insecurity, which was no longer statistically significant (table 3). In the analysis of ADHD, adjusting for confounding factors also attenuated the associations between each level of food insecurity and diagnosed ADHD, although in this case, only participants with severe food insecurity remained significantly more likely to have ADHD (table 4). Similar to the other outcomes, the analysis of ASD showed that adjusting for confounding factors attenuated the associations between each level of food insecurity and diagnosed ASD, although in this case, the moderately food insecure group was the only one that remained statistically significant after covariate adjustment (table 5).
Table 3.
Unadjusted and adjusted logistic regression models of the association between household food insecurity status and a diagnosed mood or anxiety disorder
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Household food security | ||
| Food secure | REF | REF |
| Marginally food insecure | 2.27 (1.40 to 3.67) | 2.18 (1.33 to 3.60) |
| Moderately food insecure | 2.29 (1.56 to 3.35) | 1.73 (1.15 to 2.59) |
| Severely food insecure | 2.92 (1.84 to 4.63) | 1.48 (0.90 to 2.43) |
| Age (years) | 1.30 (1.21 to 1.39) | 1.30 (1.21 to 1.39) |
| Sex | ||
| Female | REF | REF |
| Male | 1.52 (1.17 to 1.97) | 1.60 (1.22 to 2.09) |
| Household income (adjusted for household size, per CAD$10000) | 0.97 (0.94 to 1.00) | 1.00 (0.97 to 1.03) |
| Highest level parent education | ||
| High school or less | REF | REF |
| College/trades | 1.09 (0.76 to 1.57) | 1.39 (0.93 to 2.06) |
| University or more | 0.64 (0.44 to 0.93) | 1.14 (0.75 to 1.75) |
| Parent’s mental health status | ||
| Excellent/very good | REF | REF |
| Good | 3.45 (2.58 to 4.61) | 2.86 (2.12 to 3.87) |
| Fair/poor | 6.03 (4.25 to 8.56) | 4.85 (3.37 to 7.00) |
| Race and ethnic origin | ||
| White/non-racialised | REF | REF |
| Black | 0.52 (0.25 to 1.06) | 0.55 (0.26 to 1.15) |
| East Asian | 0.58 (0.30 to 1.14) | 0.78 (0.39 to 1.56) |
| Indigenous | 1.67 (1.06 to 2.64) | 1.17 (0.74 to 1.86) |
| Latin American | 0.66 (0.07 to 5.88) | 0.74 (0.08 to 6.52) |
| Other/multiple | 1.03 (0.34 to 3.10) | 0.96 (0.33 to 2.81) |
| South Asian | 0.26 (0.09 to 0.72) | 0.38 (0.13 to 1.09) |
| Southeast Asian/Filipino | 0.28 (0.11 to 0.71) | 0.36 (0.14 to 0.91) |
| West Asian/Arab | 0.20 (0.05 to 0.75) | 0.28 (0.07 to 1.04) |
| Immigration status | ||
| Non-immigrant | REF | REF |
| Immigrant/non-permanent resident | 0.39 (0.20 to 0.75) | 0.64 (0.32 to 1.27) |
| Divorce/separation | ||
| No | REF | REF |
| Yes | 2.13 (1.62 to 2.80) | 1.27 (0.93 to 1.72) |
Table 4.
Unadjusted and adjusted logistic regression models of the association between household food insecurity status and diagnosed attention deficit hyperactivity disorder
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Household food security | ||
| Food secure | REF | REF |
| Marginally food insecure | 1.37 (0.89 to 2.11) | 1.23 (0.79 to 1.93) |
| Moderately food insecure | 1.86 (1.39 to 2.51) | 1.30 (0.95 to 1.78) |
| Severely food insecure | 3.35 (2.38 to 4.73) | 1.64 (1.12 to 2.39) |
| Age (years) | 1.30 (1.24 to 1.35) | 1.30 (1.25 to 1.37) |
| Sex | ||
| Female | REF | REF |
| Male | 2.67 (2.18 to 3.29) | 2.98 (2.41 to 3.68) |
| Household income (adjusted for household size, per CAD$10000) | 0.94 (0.92 to 0.97) | 0.97 (0.95 to 1.00) |
| Highest level parent education | ||
| High school or less | REF | REF |
| College/trades | 0.70 (0.55 to 0.88) | 0.84 (0.66 to 1.08) |
| University or more | 0.40 (0.31 to 0.51) | 0.67 (0.51 to 0.90) |
| Parent’s mental health status | ||
| Excellent/very good | REF | REF |
| Good | 2.16 (1.76 to 2.66) | 1.71 (1.38 to 2.12) |
| Fair/poor | 3.70 (2.80 to 4.91) | 2.85 (2.09 to 3.88) |
| Race and ethnic origin | ||
| White/non-racialised | REF | REF |
| Black | 0.67 (0.43 to 1.03) | 0.66 (0.42 to 1.03) |
| East Asian | 0.44 (0.25 to 0.78) | 0.60 (0.33 to 1.09) |
| Indigenous | 1.64 (1.18 to 2.27) | 1.10 (0.79 to 1.56) |
| Latin American | 0.34 (0.11 to 1.01) | 0.41 (0.14 to 1.23) |
| Other/multiple | 0.46 (0.20 to 1.04) | 0.41 (0.18 to 0.94) |
| South Asian | 0.15 (0.09 to 0.27) | 0.22 (0.12 to 0.39) |
| Southeast Asian/Filipino | 0.34 (0.16 to 0.70) | 0.43 (0.20 to 0.93) |
| West Asian/Arab | 0.42 (0.18 to 0.96) | 0.53 (0.21 to 1.33) |
| Immigration status | ||
| Non-immigrant | REF | REF |
| Immigrant/non-permanent resident | 0.34 (0.20 to 0.57) | 0.51 (0.29 to 0.89) |
| Divorce/separation | ||
| No | REF | REF |
| Yes | 2.62 (2.15 to 3.19) | 1.62 (1.31 to 2.00) |
Table 5.
Unadjusted and adjusted logistic regression models of the association between household food insecurity status and diagnosed autism spectrum disorder
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Household food security | ||
| Food secure | REF | REF |
| Marginally food insecure | 1.73 (1.04 to 2.87) | 1.53 (0.90 to 2.59) |
| Moderately food insecure | 2.37 (1.59 to 3.55) | 1.74 (1.14 to 2.64) |
| Severely food insecure | 2.80 (1.72 to 4.57) | 1.70 (0.98 to 2.94) |
| Age (years) | 0.97 (0.91 to 1.04) | 0.97 (0.91 to 1.04) |
| Sex | ||
| Female | REF | REF |
| Male | 4.07 (2.80 to 5.90) | 4.13 (2.85 to 6.01) |
| Household income (adjusted for household size, per CAD$10000) | 0.95 (0.90 to 1.00) | 0.98 (0.93 to 1.03) |
| Highest level parent education | ||
| High school or less | REF | REF |
| College/trades | 0.85 (0.57 to 1.27) | 1.01 (0.67 to 1.53) |
| University or more | 0.61 (0.40 to 0.92) | 0.90 (0.57 to 1.41) |
| Parent’s mental health status | ||
| Excellent/very good | REF | REF |
| Good | 1.87 (1.34 to 2.63) | 1.69 (1.21 to 2.38) |
| Fair/poor | 4.35 (2.97 to 6.36) | 3.77 (2.51 to 5.64) |
| Race and ethnic origin | ||
| White/non-racialised | REF | REF |
| Black | 1.27 (0.75 to 2.16) | 1.29 (0.71 to 2.35) |
| East Asian | 1.04 (0.58 to 1.87) | 1.28 (0.69 to 2.35) |
| Indigenous | 1.29 (0.71 to 2.34) | 0.96 (0.53 to 1.73) |
| Latin American | 0.53 (0.01 to 31.5) | 0.59 (0.01 to 35.1) |
| Other/multiple | 2.06 (0.95 to 4.49) | 1.74 (0.77 to 3.90) |
| South Asian | 0.67 (0.38 to 1.18) | 0.92 (0.49 to 1.72) |
| Southeast Asian/Filipino | 1.43 (0.70 to 2.94) | 1.59 (0.73 to 3.46) |
| West Asian/Arab | 0.31 (0.03 to 2.92) | 0.40 (0.04 to 3.76) |
| Immigration status | ||
| Non-immigrant | REF | REF |
| Immigrant/non-permanent resident | 0.50 (0.19 to 1.33) | 0.57 (0.19 to 1.65) |
| Divorce/separation | ||
| No | REF | REF |
| Yes | 1.34 (0.97 to 1.85) | 0.99 (0.69 to 1.41) |
Sensitivity analysis using two levels of food security, food secure and food insecure showed associations similar to those between moderate household food insecurity and any of the four diagnosed mental health conditions, with children in food insecure households having almost 50% higher odds of having a mental health condition after adjusting for confounders (online supplemental table 1).
bmjopen-2023-081538supp001.pdf (114.6KB, pdf)
Discussion
This study examined the association between household food insecurity and diagnosed mental health conditions among children aged 5–11 years using a nationally representative sample of children in Canada. We found that children living in food insecure households were more likely to have a diagnosed mental health condition, including anxiety or mood disorders, ASD and ADHD, and this held true after adjustment for sociodemographic and parent/caregiver characteristics. Household food insecurity was dose-dependently associated with a child’s likelihood of having a diagnosed mental health condition, speaking to the importance of examining food insecurity by severity when possible. After adjusting for important confounders including income and parent/caregiver mental health, children in severely food insecure households were 67% more likely to have a diagnosed mental health condition compared with children in food secure households.
Previous studies found increased odds of negative mental health outcomes among children and youth living in households experiencing food insecurity. Anderson et al identified associations between household food security and healthcare visits for a mental disorder among Canadian children aged 1–17.16 This study showed an increasing prevalence of mental health service use with increasing household food insecurity severity, similar to our study. Men et al identified relationships between household food security and mental health among Canadian youth aged 12–24.32 Similar to our findings among children 5–11 years, they showed a dose–response relationship between severity of household food insecurity and mental health, where the odds of presence of diagnosed mental health conditions increased as the severity of household food insecurity increased among adolescents and adults.32 Sharifi et al also used CHSCY to examine the relationship between food insecurity and mental health among 1–17 years, with similar findings to our study. Our findings expand on the results of Sharifi et al by using household food insecurity as the exposure, which is a more sensitive measure of a child’s experience of food insecurity, by testing the dose relationship using four levels of food security and by disaggregating developmental disorders ASD and ADHD.17
Household food insecurity can impact a child’s mental health through a number of mechanisms.14 Children from severely food insecure households face reduced quality, quantity and frequency of meals which may directly impact behavioural difficulties and mental health conditions.33 An indirect pathway may be through parental well-being where parents and caregivers experiencing food insecurity may reduce sensitive and responsive parenting from the chronic financial and emotional stress of acquiring food, which can negatively impact the child’s overall mental health.33 This suggests that even if children are not themselves experiencing disrupted eating or hunger, the uncertainty around food affordability and food availability in the family is enough to precipitate mental health conditions.
Our findings also suggest that there is an association with specific mental health conditions, which is aligned with previous research. One US study of children 6–12 years showed that food insecurity, dichotomised into two levels, was significantly associated with ADHD.18 There may also be temporal differences in exposure to food insecurity and the likelihood of developing a mood/anxiety disorder compared with a neurodevelopmental disorder. Macronutrient deficiencies affecting neurotransmitters and neuropsychiatric regulation in the early years may have effects on brain development and subsequent mental health problems.34 Additionally, psychosocial and environmental effects including parental stress may contribute to the association between food insecurity and child mental health.34
One major strength of this study was examining the dose–response relationship of household food insecurity with parent/caregiver-reported diagnosed mental health conditions. Additionally, this is one of the few studies in the literature that analyses mental health specifically among young children between 5 and 11 years in Canada. The survey used for these analyses, CHSCY, is sampled and weighted to be representative of the child population in Canada. Additionally, food insecurity was captured using the HFSSM, which is well validated as the primary measurement tool of household food insecurity in Canada. Given the breadth of data collected in the CHSCY, we were also able to control for multiple sociodemographic, family and economic factors in our analysis, including parent/caregiver mental health, which is an important confounder of the relationship between food security and child mental health.
Certain limitations should be considered when interpreting the results. The study used a cross-sectional design and is, therefore, unable to determine causality or to detangle the potential bidirectional relationship between food insecurity and child mental health. For instance, poor child mental health may worsen a family’s food insecurity by depleting scarce financial and time resources. Additionally, while parents/guardians are better positioned than younger children to provide accurate reporting of child health and household measures, the reliance on parental reports of both household food insecurity and health professional-diagnosed mental health conditions introduces a risk of information biases such as recall and social desirability biases. Further, parental reports have been shown to underestimate children’s experience of food insecurity, compared with child reports.35 To whatever degree this bias was present in our study, it would underestimate food insecurity and likely bias our results towards the null. It is also important to note some limitations of the CHSCY survey. Although the CHSCY data provide nationally representative data, the 2019 response rate to this survey cycle was only 57.8% for children 5–11 years and 51.8% overall.22 This may introduce some selection bias in the population surveyed, although the impact on our findings, if any, is unclear given the correcting use of bootstrap weights and replicates and existing evidence that response rates on health surveys are not related to non-response bias or data representativeness.36
Conclusion
This study found that Canadian children aged 5–11 who live in food insecure households are more likely to have been diagnosed with a mental health condition than children in food secure households. Compounded by the increases in child mental health conditions and rising food insecurity rates, both food insecurity and mental health are public health priorities. This study supports the need to implement policies that are focused on creating sustainable systems to alleviate the burden of food insecurity on mental health.
Supplementary Material
Footnotes
Contributors: JT, SO, SN and SC contributed to conceptualising and designing the study and preparing the manuscript draft. JT conducted the statistical analysis. SC validated the analysis and provided project oversight. JT, SO and SC contributed to developing and refining the methods and interpreting the results. JT, SO, SN, DH and SC reviewed the manuscript for intellectual content and approved the final version for publication. SC is the author acting as guarantor and is responsible for the conduct of the study and the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. The Canadian Health Survey on Children and Youth data are deidentified participant data, available on successful application to Statistics Canada’s Research Data Centre programme: https://www.statcan.gc.ca/eng/rdc/index.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the Ethics Review Board of Public Health Ontario (approval number: 2022-003.03). Participants gave informed consent to participate in the Canadian Health Survey on Children and Youth before taking part.
References
- 1. Mental Health Commission of Canada . Children and Youth. Ottawa, ON: Health Canada, 2017. Available: https://mentalhealthcommission.ca/what-we-do/children-and-youth/ [Google Scholar]
- 2. Comeau J, Georgiades K, Duncan L, et al. Changes in the prevalence of child and youth mental disorders and perceived need for professional help between 1983 and 2014: evidence from the Ontario child health study. Can J Psychiatry 2019;64:256–64. 10.1177/0706743719830035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wiens K, Bhattarai A, Pedram P, et al. A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. Epidemiol Psychiatr Sci 2020;29:e115. 10.1017/S2045796020000281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Madigan S, Racine N, Vaillancourt T, et al. Changes in depression and anxiety among children and adolescents from before to during the COVID-19 pandemic: A systematic review and meta-analysis. JAMA Pediatr 2023;177:567–81. 10.1001/jamapediatrics.2023.0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnson D, Dupuis G, Piche J, et al. Adult mental health outcomes of adolescent depression: A systematic review. Depress Anxiety 2018;35:700–16. 10.1002/da.22777 [DOI] [PubMed] [Google Scholar]
- 6. Kessler RC, Avenevoli S, Costello EJ, et al. Prevalence, persistence, and Sociodemographic correlates of DSM-IV disorders in the National Comorbidity survey replication adolescent supplement. Arch Gen Psychiatry 2012;69:372–80. 10.1001/archgenpsychiatry.2011.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ahmad S, Briante C, Khan M, et al. The Life and Economic Impact of Major Mental Illnesses in Canada. Ottawa, Ontario: Canadian Electronic Library, 2015. [Google Scholar]
- 8. Government of Canada . Household food insecurity in Canada: Overview, Available: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview.html
- 9. Tarasuk VLT, Fafard St-Germain AA. Household Food Insecurity in Canada, 2021. Toronto: Research to identify policy options to reduce food insecurity (PROOF), 2022. Available: https://proof.utoronto.ca/wp-content/uploads/2023/11/Household-Food-Insecurity-in-Canada-2022-PROOF.pdf [Google Scholar]
- 10. Statistics Canada . Table 13-10-0835-01 Food Insecurity by Selected Demographic Characteristics. Ottawa, ON, 2023. Available: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310083501 [Google Scholar]
- 11. Hutchinson J, Tarasuk V. The relationship between diet quality and the severity of household food insecurity in Canada. Public Health Nutr 2022;25:1013–26. 10.1017/S1368980021004031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Owen L, Corfe B. The role of diet and nutrition on mental health and wellbeing. Proc Nutr Soc 2017;76:425–6. 10.1017/S0029665117001057 [DOI] [PubMed] [Google Scholar]
- 13. Merrick MT, Ports KA, Ford DC, et al. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl 2017;69:10–9. 10.1016/j.chiabu.2017.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Melchior M, Chastang J-F, Falissard B, et al. Food insecurity and children’s mental health: A prospective birth cohort study. PLOS ONE 2012;7:e52615. 10.1371/journal.pone.0052615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Paquin V, Muckle G, Bolanis D, et al. Longitudinal Trajectories of food insecurity in childhood and their associations with mental health and functioning in adolescence. JAMA Netw Open 2021;4:e2140085. 10.1001/jamanetworkopen.2021.40085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anderson KK, Clemens KK, Le B, et al. Household food insecurity and health service use for mental and substance use disorders among children and adolescents in Ontario, Canada. CMAJ 2023;195:E948–55. 10.1503/cmaj.230332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sharifi V, Dimitropoulos G, Williams JVA, et al. Food insecurity is associated with poor mental health in Canadian children and adolescents. Can J Psychiatry 2024;69:296–8. 10.1177/07067437231225938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hatsu IE, Eiterman L, Stern M, et al. Household food insecurity is associated with symptoms of emotional dysregulation in children with attention deficit hyperactivity disorder: the MADDY study. Nutrients 2022;14:1306. 10.3390/nu14061306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Karpur A, Vasudevan V, Lello A, et al. Food insecurity in the households of children with autism spectrum disorders and intellectual disabilities in the United States: analysis of the National survey of children’s health data 2016–2018. Autism 2021;25:2400–11. 10.1177/13623613211019159 [DOI] [PubMed] [Google Scholar]
- 20. Rogge N, Janssen J. The economic costs of autism spectrum disorder: A literature review. J Autism Dev Disord 2019;49:2873–900. 10.1007/s10803-019-04014-z [DOI] [PubMed] [Google Scholar]
- 21. Statistics Canada . Canadian Health Survey on Children and Youth (CHSCY), 2019. Available: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5233
- 22. Statistics Canada . 2019 Canadian Health Survey on Children and Youth (CHSCY): User Guide. 2020. [Google Scholar]
- 23. Government of Canada . The Household Food Security Survey Module (HFSSM), 2023. Available: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview/household-food-security-survey-module-hfssm-health-nutrition-surveys-health-canada.html
- 24. Government of Canada . Determining food security status, 2020. Available: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview/determining-food-security-status-food-nutrition-surveillance-health-canada.html
- 25. Fernández CR, Yomogida M, Aratani Y, et al. Dual food and energy hardship and associated child behavior problems. Acad Pediatr 2018;18:889–96. 10.1016/j.acap.2018.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu R, Urquia ML, Tarasuk V. The prevalence and predictors of household food insecurity among adolescents in Canada. Can J Public Health 2023;114:453–63. 10.17269/s41997-022-00737-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McIntyre L, Wu X, Kwok C, et al. The pervasive effect of youth self-report of hunger on depression over 6 years of follow up. Soc Psychiatry Psychiatr Epidemiol 2017;52:537–47. 10.1007/s00127-017-1361-5 [DOI] [PubMed] [Google Scholar]
- 28. McLaughlin KA, Green JG, Alegría M, et al. Food insecurity and mental disorders in a national sample of U.S. J Am Acad Child Adolesc Psychiatry 2012;51:1293–303. 10.1016/j.jaac.2012.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. PROOF . Food Insecurity and Mental Health, 2018. Available: https://proof.utoronto.ca/resource/food-insecurity-and-mental-health/
- 30. Tarasuk V, Fafard St-Germain A-A, Mitchell A. Geographic and socio-demographic predictors of household food insecurity in Canada, 2011–12. BMC Public Health 2019;19:12. 10.1186/s12889-018-6344-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Statistics Canada . Adjusted total income of private household, 2016. Available: https://www23.statcan.gc.ca/imdb/p3Var.pl?Function=DEC&Id=252278
- 32. Men F, Elgar FJ, Tarasuk V. Food insecurity is associated with mental health problems among Canadian youth. J Epidemiol Community Health 2021;75:741–8. 10.1136/jech-2020-216149 [DOI] [PubMed] [Google Scholar]
- 33. Ashiabi GS, O’Neal KK. A framework for understanding the association between food insecurity and children’s developmental outcomes. Child Dev Perspectives 2008;2:71–7. 10.1111/j.1750-8606.2008.00049.x [DOI] [Google Scholar]
- 34. Cain KS, Meyer SC, Cummer E, et al. Association of food insecurity with mental health outcomes in parents and children. Acad Pediatr 2022;22:1105–14. 10.1016/j.acap.2022.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bernard R, Hammarlund R, Bouquet M, et al. Parent and child reports of food insecurity and mental health: divergent perspectives. Ochsner J 2018;18:318–25. 10.31486/toj.18.0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lee S, Brown ER, Grant D, et al. Exploring Nonresponse bias in a health survey using neighborhood characteristics. Am J Public Health 2009;99:1811–7. 10.2105/AJPH.2008.154161 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-081538supp001.pdf (114.6KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. The Canadian Health Survey on Children and Youth data are deidentified participant data, available on successful application to Statistics Canada’s Research Data Centre programme: https://www.statcan.gc.ca/eng/rdc/index.