Contrast agents are widely used in imaging, but until recently they had little place in ultrasonography. This has changed with the introduction of microbubbles—small (typically 3 μm in diameter) gas filled bubbles that are usually injected intravenously. Injecting a gas into the circulation may seem potentially hazardous, but extensive clinical experience has shown that the tiny volume of air or gas given (under 200 μl) is not dangerous, and the safety of microbubbles compares well to that of conventional agents in radiography and magnetic resonance imaging.1 Although microbubbles were originally designed simply to improve conventional ultrasound scanning, recent discoveries have opened up powerful emerging applications. This article describes some of these applications in radiology and cardiology and discusses the potential of microbubbles for therapy.
Methods
We prepared this review from contributions from researchers with special knowledge of the use of microbubbles in radiology, cardiology, and treatment. We combined our personal experience in research over several years with a review of recent literature on the subject.
How microbubbles work
Microbubbles work by resonating in an ultrasound beam, rapidly contracting and expanding in response to the pressure changes of the sound wave. By a fortunate coincidence, they vibrate particularly strongly at the high frequencies used for diagnostic ultrasound imaging. This makes them several thousand times more reflective than normal body tissues. In this way they enhance both grey scale images and flow mediated Doppler signals. As well as being useful in itself, the resonance that microbubbles produce has several special properties that can be exploited to improve diagnoses. Just as with a musical instrument, multiple harmonic signals—or overtones—are produced. Ultrasound scanners can be tuned to “listen” to these harmonics, producing strong preferential imaging of the microbubbles in an image. The selective excitation produced can also destroy microbubbles relatively easily, an effect that can be useful both in imaging and in emerging therapeutic applications.
Microbubbles in general radiology
Microbubbles increase the intensity of Doppler signals from blood for several minutes after their injection, and this effect can be prolonged by infusing them.2 They can thus rescue or improve an undiagnostic Doppler examination by raising the intensity of weak signals to a detectable level. For example, they can improve detection of flow in the intracranial arteries by transcranial Doppler in adults, where the skull greatly attenuates the ultrasound signal.3 Another use is in detecting flow in smaller vessels, such as in the circulation of malignant tumours.4
Anticipated developments
Robust methods for detecting and measuring microcirculatory flow, allowing quantification of regional ischaemia in the myocardium and other organs
Routine use of microbubbles to enhance imaging of the liver parenchyma, improving accuracy of ultrasonographic assessment and staging of cancer
Development of microbubbles as tools for delivery of gene therapy and other treatments to specific sites
Microbubble based methods of non-invasive clot lysis
Microbubbles can also be administered into body cavities, allowing simple functional tests to be performed. For example, vesicoureteric reflux in children can be revealed by injecting them into the bladder cavity and scanning the kidneys and ureters (fig 1). Fallopian tube patency can be confirmed by detecting an enhanced signal after instilling microbubbles into the uterine cavity. Several studies have confirmed that these techniques show high sensitivity and specificity compared with the established methods of x ray micturating cystourethrography and salpingography (both of which involve ionising radiation) and could replace them in some situations.5,6
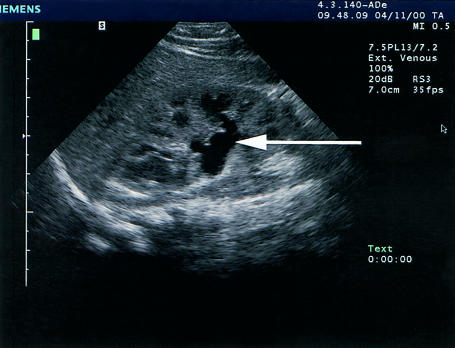
Figure 1.
Use of microbubbles to demonstrate vesicoureteric reflux. Top figure shows left kidney with a slightly dilated renal pelvis (arrow). Bottom figure shows the same area after microbubbles have been instilled into the bladder. Bright echoes, representing microbubbles can now be seen in the renal pelvis (arrow), indicating vesicoureteric reflux, which was confirmed on x ray micturating cystourethrogram. (Images courtesy of Dr Thomas Albrecht, Benjamin Franklin University, Berlin, Germany)
Specific diagnostic applications
Imaging the liver
This is perhaps the most promising clinical application of microbubbles in radiology at present. Some, but not all, microbubbles are taken up by the liver and spleen. The precise mechanism is unclear, but the reticuloendothelial system is probably involved. This liver phase lasts about 30 minutes with the licensed agent Levovist7 and several hours with some new agents in clinical trials.8 During this phase the liver is particularly well seen with microbubble-specific imaging modes such as harmonic imaging. The main practical importance is that many focal liver lesions, particularly metastases and hepatocellular carcinoma, appear as defects, and their visibility is greatly increased with microbubbles (fig 2).9
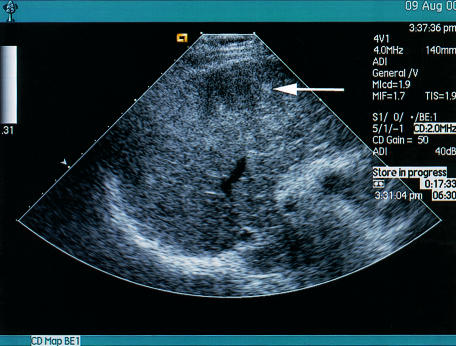
Figure 2.
Effect of liver-specific microbubbles on the visualisation of a hepatocellular carcinoma complicating chronic hepatitis B infection. Top figure shows the liver is heterogeneous with an ill defined lesion (arrow). Bottom figure shows the presence of liver-specific microbubbles (Levovist) administered 5 minutes earlier. A defect is clearly seen in the central right lobe of the liver, with several additional defects thought to represent additional satellite foci of hepatocellular carcinoma
Early evidence from several studies suggests that this can substantially increase the sensitivity of ultrasound to metastatic disease.9–12 It seems particularly useful in detecting small lesions (under 1 cm diameter), for which all imaging methods lack sensitivity. A recently completed multicentre study showed an increased sensitivity to liver metastases from 71% to 88%, and the mean size of the smallest lesions detected decreased by 50% to under 1 cm.13 It therefore seems likely that the sensitivity of ultrasound to liver metastases, and possibly to hepatocellular carcinoma, could be substantially increased. This mode of scanning has limitations, however, including the transience of the effect and the difficulty of accessing the whole of the liver. The advent of new, more durable, liver-specific agents currently in clinical trials will probably address at least the former concern.
Microbubbles may also increase specificity in liver imaging since some lesions can be characterised by their enhancement patterns. For example, haemangiomas, common benign tumours that can mimic more aggressive pathology, show a characteristic globular or peripheral pattern of enhancement with centripetal fill-in, and their identification with ultrasound may avoid the need for further tests to characterise them.14 Another study has shown that late uptake of microbubbles is characteristic of many benign lesions.15
An analysis of the initial vascular enhancement produced by microbubbles can also give much useful information. Changes in intensity (or loudness) of a spectral Doppler signal are proportional to microbubble concentration. Thus, if a hepatic vein is scanned after a bolus injection of microbubbles, analysis of the changes in Doppler intensity with time gives much useful information. Early enhancement is seen in cirrhosis and malignancy because of vascular shunting and arterialisation of the liver's blood supply.16,17 This simple technique may be particularly useful for distinguishing between different types of diffuse liver disease and diagnosing cirrhosis, for which traditional imaging findings are notoriously unhelpful so that biopsy is often required. Research is under way to study whether early enhancement of the ultrasound signal is also characteristic of “micrometastases” in colon cancer before they are detectable by conventional methods.
Imaging the heart
Microbubbles can enhance Doppler flow signals in cardiac ultrasonography, and this can be useful in several situations, such as detecting valvular stenoses.18 Of greater impact has been their role in improving delineation of the endocardial border. Microbubble contrast agents highlight the left ventricular cavity and make the blood-tissue boundary much clearer, which helps in assessing regional abnormalities in wall motion, estimating ejection fraction, and detecting left ventricular thrombus. Evaluating left ventricular function is key to the management of many cardiac conditions, and this procedure forms about 60% of the workload of an adult echocardiography department. Good endocardial definition is critical to this evaluation, and any improvement in definition is especially useful for the 10-20% of patients with technically difficult studies using standard techniques.19 Some contrast agents have been shown to convert 74% of non-diagnostic images into diagnostic studies by improving endocardial visualisation.20 They can assist in thrombus detection when imaging is difficult, which may be crucial in deciding whether to start anticoagulant treatment.
Good endocardial definition is particularly critical when echocardiography is performed under physiological or pharmacological stress (“stress echocardiography”), and the use of contrast agents in this situation has been particularly valuable. In about 35% of stress echocardiographic studies some segments of the endocardium are poorly seen, and contrast agents can render most of these interpretable. Overall, such agents improve diagnostic reliability and accuracy and reduce interobserver variability.20 Many centres perform at least 60% of their studies with the aid of contrast agents.
Emerging roles for microbubbles in cardiology include assessing myocardial perfusion. For this, an understanding of the fragility of microbubbles in an ultrasound beam is crucial. Until recently, detecting blood flow required intermittent imaging because of extensive destruction of microbubbles when continuous scanning was used.21 Now, however, contrast-specific technologies that use low acoustic power, and hence disrupt microbubbles less, allow real time imaging of perfusion. This allows information about wall motion and myocardial perfusion to be obtained simultaneously (fig 3), offering great potential for diagnosing acute myocardial infarction, determining the area of myocardium at risk, and assessing the success of thrombolysis. Microvascular integrity, and therefore myocardial perfusion, is essential for functional recovery of affected segments of heart muscle, and myocardial contrast echocardiography can accurately predict this.22 Real time perfusion imaging in stress echocardiography may offer a potent tool for assessing both resting and inducible ischaemia. The method can be extended further by applying intermittent high power pulses to destroy most of the microbubbles in a scan plane and then watching refilling: the rate at which this occurs is a measure of microcirculatory flow speed.23
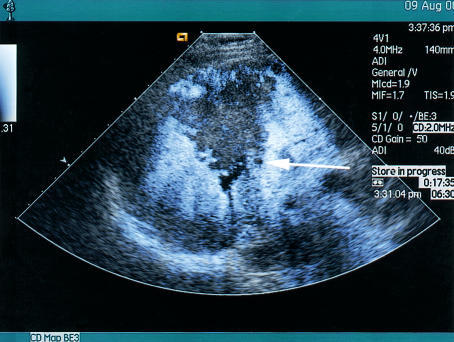
Figure 3.
Echocardiographic image of the left ventricle using real time imaging of perfusion and an intravenous microbubble as contrast agent. The contrast agent fills the ventricular cavity, clearly delineating the endocardial border, and gives colour enhancement in the myocardium, showing perfusion of the apex and septum (arrows)
Treatment with microbubbles
The use of microbubbles in treatments may eventually be even more important than their diagnostic uses.24 Microbubbles can aid drug delivery in themselves (by acting as “cavitation nuclei”) and as agents to carry drugs for site-specific treatment. Their most exciting application is in the emerging area of gene therapy, where delivery of genetic material to a chosen site is difficult.25
Ultrasound can potentiate drug delivery by creating transient non-lethal perforations in cell membranes to aid ingress of large molecules and particles into the cells (“sonoporating”). In general this requires high acoustic power, substantially beyond that permitted for imaging, but the power needed is greatly reduced when microbubbles are present. This is because microbubbles lower the amount of energy necessary for cavitation, the process in which extreme oscillations induced by ultrasound pulses lead to microbubble collapse.26–28 The potential of this in gene therapy has already been shown.29 Cavitation of microbubbles in capillary beds also increases capillary permeability, which improves local access of the released therapeutic agent.30
Microbubbles as drug delivery vehicles
Microbubbles can be formulated to carry therapeutic agents. Some albumin based microbubbles and those with shells of charged lipids take up genetic material directly.24,27 Bespoke microbubbles can also be constructed (fig 4). Hydrophilic compounds can be encased within lipid membranes or polymeric shells that stabilise the microbubbles. The circulation of these loaded microbubbles can be followed with ultrasound, and when they reach the target area they can be disrupted, releasing their therapeutic payload to the surrounding tissue (fig 5). A recent study showed that transfection of a reporter gene in a mouse heart model was increased 10-fold using microbubbles loaded with an adenovirus gene vector.28
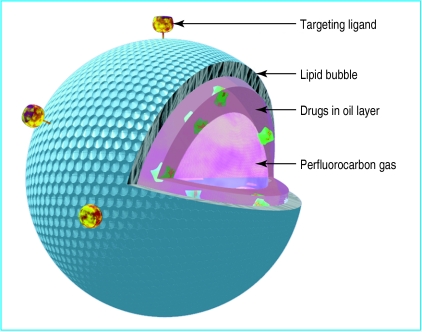
Figure 4.
Diagram of a microbubble constructed for drug delivery. Gas-filled microspheres may be designed so that their interior is loaded with drug and gas. A stabilising material, here a lipid, surrounds the perfluorocarbon bubble. Drugs may be incorporated by themselves or, if insoluble in water, in an oil layer. The microsphere may be targeted to specific tissue by incorporating protein ligands on the surface
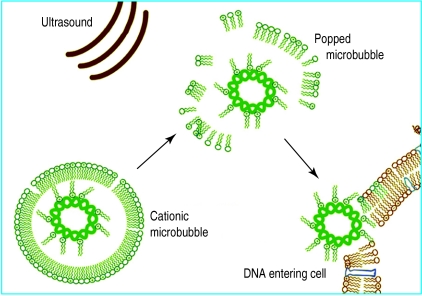
Figure 5.
Gene delivery using ultrasound and microbubbles. The presence of gas in the gene-filled microbubble allows ultrasound energy to “pop” the bubble. An energetic wave is then created which allows the genetic material to enter surrounding cells
Delivery to a specific site can be aided by incorporating ligands into the membrane of the microbubbles that target receptors on cell membranes. For example, incorporation of a surface ligand that binds to the GPIIB/IIIA receptors on activated platelets allows microbubbles to bind to a thrombus and deliver thrombolytic agents.30
Internet resources on microbubbles
Burns PN, Becher H. Handbook of Contrast Echocardiography. Frankfurt: Springer Verlag, 2000. (Textbook of contrast imaging, mainly of cardiographic interest) Free download on http://www.sunnybrook.utoronto.ca/EchoHandbook/)
http://contrastultrasound.com Images, resources and links of general interest. (Supported by ATL/Phillips)
http://www.ultrasoundinsider.com/ Comprehensive list of links of general interest in ultrasound, with many microbubble-related links.
Acknowledgments
We thank Ms Terri New for producing figures 4 and 5, Dr Thomas Albrecht for providing figure 1, and Dr David Blomley for many helpful comments on the manuscript.
Footnotes
Competing interests: MJKB is supported by Schering AG, Berlin, and ECU is president and CEO of ImaRx Therapeutics, Tucson AZ. Both companies are involved in microbubble technology. In addition, MJKB and DOC have received reimbursement for attending symposia and fees for speaking, organising education and research support, and consulting from several companies involved in microbubble technology.
References
- 1.Nanda NC, Carstensen C. Echo-enhancing agents: safety. In: Nanda NC, Schlief R, Goldberg BB, editors. Advances in echo imaging using contrast enhancers. Dordrecht: Kluwer; 1997. pp. 115–131. [Google Scholar]
- 2.Albrecht T, Urbank A, Mahler M, Bauer A, Dore CJ, Blomley MJ, et al. Prolongation and optimization of Doppler enhancement with a microbubble US contrast agent by using continuous infusion: preliminary experience. Radiology. 1998;207:339–347. doi: 10.1148/radiology.207.2.9577478. [DOI] [PubMed] [Google Scholar]
- 3.Ries F, Honisch C, Lambertz M, Schlief R. A transpulmonary contrast medium enhances the transcranial Doppler signal in humans. Stroke. 1993;24:1903–1909. doi: 10.1161/01.str.24.12.1903. [DOI] [PubMed] [Google Scholar]
- 4.Cosgrove D. Why do we need contrast agents for ultrasound? Clin Radiol. 1996;51(suppl 1):1–4. [PubMed] [Google Scholar]
- 5.Darge K, Troeger J, Duetting T, Zieger B, Rohrschneider W, Moehring K, et al. Reflux in young patients: comparison of voiding US of the bladder and retrovesical space with echo enhancement versus voiding cystourethrography for diagnosis. Radiology. 1999;210:201–207. doi: 10.1148/radiology.210.1.r99ja40201. [DOI] [PubMed] [Google Scholar]
- 6.Strandell A, Bourne T, Bergh C, Granberg S, Asztely M, Thorburn J. The assessment of endometrial pathology and tubal patency: a comparison between the use of ultrasonography and X-ray hysterosalpingography for the investigation of infertility patients. Ultrasound Obstet Gynecol. 1999;14:200–204. doi: 10.1046/j.1469-0705.1999.14030200.x. [DOI] [PubMed] [Google Scholar]
- 7.Blomley MJ, Albrecht T, Cosgrove DO, Eckersley RJ, Butler-Barnes J, Jayaram V, et al. Stimulated acoustic emission to image a late liver and spleen-specific phase of Levovist in normal volunteers and patients with and without liver disease. Ultrasound Med Biol. 1999;25:1341–1352. doi: 10.1016/s0301-5629(99)00081-2. [DOI] [PubMed] [Google Scholar]
- 8.Forsberg F, Goldberg BB, Liu JB, Merton DA, Rawool NM, Shi WT. Tissue-specific US contrast agent for evaluation of hepatic and splenic parenchyma. Radiology. 1999;210:125–132. doi: 10.1148/radiology.210.1.r99ja11125. [DOI] [PubMed] [Google Scholar]
- 9.Harvey CJ, Blomley MJ, Eckersley RJ, Heckemann RA, Butler-Barnes J, Cosgrove DO. Pulse-inversion mode imaging of liver specific microbubbles: improved detection of subcentimetre metastases. Lancet. 2000;355:807–808. doi: 10.1016/S0140-6736(99)04545-6. [DOI] [PubMed] [Google Scholar]
- 10.Blomley MJ, Albrecht T, Cosgrove DO, Patel N, Jayaram V, Butler-Barnes J, et al. Improved imaging of liver metastases with stimulated acoustic emission in the late phase of enhancement with the US contrast agent SH U 508A: early experience. Radiology. 1999;210:409–416. doi: 10.1148/radiology.210.2.r99fe47409. [DOI] [PubMed] [Google Scholar]
- 11.Harvey CJ, Blomley MJK, Eckersley RJ, Heckemann RA, Butler-Barnes J, Cosgrove DO. Improved detection of hepatic malignancies using pulse inversion mode of the ultrasound contrast agent Levovist (SH U 508A): early experience. Radiology (in press). [DOI] [PubMed]
- 12.Albrecht T, Hoffmann CW, Schmitz SA, Schettler S, Overberg A, Germer CT, et al. Phase inversion sonography during the liver-specific phase of Levovist: improved detection of liver metastases. AJR Am J Roentgenol (in press). [DOI] [PubMed]
- 13.Blomley MJK, Albrecht T, Wilson SR, Burns PN, Lafortune M, Leen E, et al. Improved detection of metastatic liver lesions using pulse inversion harmonic imaging with Levovist: a multicenter study [abstract] Radiology. 1999;213(P):1685. [Google Scholar]
- 14.Kim TK, Choi BI, Han JK, Hong HS, Park SH, Moon SG. Hepatic tumors: contrast agent-enhancement patterns with pulse-inversion harmonic US. Radiology. 2000;216:411–417. doi: 10.1148/radiology.216.2.r00jl21411. [DOI] [PubMed] [Google Scholar]
- 15.Blomley MJK, Sidhu PS, Cosgrove DO, Albrecht T, Harvey CJ, Heckemann RA, et al. Do different types of liver lesion differ in their uptake of the microbubble SHU508 in its late liver phase: early experience. Radiology (in press). [DOI] [PubMed]
- 16.Albrecht T, Blomley MJK, Cosgrove DO. Non-invasive diagnosis of hepatic cirrhosis by transit time analysis of an ultrasound contrast agent. Lancet. 1999;353:1579–1583. doi: 10.1016/S0140-6736(98)06373-9. [DOI] [PubMed] [Google Scholar]
- 17.Blomley MJ, Albrecht T, Cosgrove DO, Jayaram V, Eckersley RJ, Patel N, et al. Liver vascular transit time analyzed with dynamic hepatic venography with bolus injections of an US contrast agent: early experience in seven patients with metastases. Radiology. 1998;209:862–866. doi: 10.1148/radiology.209.3.9844688. [DOI] [PubMed] [Google Scholar]
- 18.Mulvagh SL, DeMaria AN, Feinstein SB, Burns PN, Kaul S, Miller JG, et al. Contrast echocardiography: current and future applications. J Am Soc Echocardiogr. 2000;13:331–342. doi: 10.1067/mje.2000.105462. [DOI] [PubMed] [Google Scholar]
- 19.Cohen JL, Cheirif J, Segar DS, Gillam LD, Gottdiener JS, Hausnerova E, et al. Improved left ventricular endocardial border delineation and opacification with OPTISON (FS069), a new echocardiographic contrast agent. Results of a phase III multicentre trial. J Am Coll Cardiol. 1998;32:746–752. doi: 10.1016/s0735-1097(98)00311-8. [DOI] [PubMed] [Google Scholar]
- 20.Cheng S-C, Dy TC, Feinstein SB. Contrast echocardiography: review and future directions. Am J Cardiol. 1998;81(12A):41–8G. doi: 10.1016/s0002-9149(98)00053-8. [DOI] [PubMed] [Google Scholar]
- 21.Cwajg J, Xie F, O'Leary E, Kricsfeld D, Dittrich H, Porter TR. Detection of angiographically significant coronary artery disease with accelerated intermittent imaging after intravenous administration of ultrasound contrast material. Am Heart J. 2000;139:675–683. doi: 10.1016/s0002-8703(00)90047-4. [DOI] [PubMed] [Google Scholar]
- 22.Czitrom D, Karila-Cohen D, Brochet E, Juliard JM, Faraggi M, Aumont M-C, et al. Acute assessment of microvascular perfusion patterns by myocardial contrast echocardiography during myocardial infarction: relation to timing and extent of functional recovery. Heart. 1999;81:12–16. doi: 10.1136/hrt.81.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burns PN, Becher H. Handbook of contrast echocardiography. Frankfurt: Springer Verlag; 2000. Method for quantitative analysis; pp. 154–169. [Google Scholar]
- 24.Miller MW. Gene transfection and drug delivery. Ultrasound Med Biol. 2000;26(suppl 1):S59–S62. doi: 10.1016/s0301-5629(00)00166-6. [DOI] [PubMed] [Google Scholar]
- 25.Russell SJ. Science, medicine, and the future: gene therapy. BMJ. 1997;315:1289–1292. doi: 10.1136/bmj.315.7118.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Apfel RE, Holland CK. Gauging the likelihood of cavitation from short-pulse, low-duty cycle diagnostic ultrasound. Ultrasound Med Biol. 1991;17:179–185. doi: 10.1016/0301-5629(91)90125-g. [DOI] [PubMed] [Google Scholar]
- 27.Porter TR, Iverson PL, Li S, Xia F. Interaction of diagnostic ultrasound with synthetic oligonucleotide-labeled perfluorocarbon-exposed sonicated dextrose albumin microbubbles. J Ultrason Med. 1996;15:577–584. doi: 10.7863/jum.1996.15.8.577. [DOI] [PubMed] [Google Scholar]
- 28.Shohet RV, Chen S, Zhou Y-T, Wang Z, Meidell RS, Unger RH, et al. Echocardiographic destruction of albumin microbubbles directs gene delivery to the myocardium. Circulation. 2000;101:2554–2556. doi: 10.1161/01.cir.101.22.2554. [DOI] [PubMed] [Google Scholar]
- 29.Price RJ, Skyba DM, Kaul S, Skalak TC. Delivery of colloidal particles and red blood cells to tissue through microvessel ruptures created by targeted microbubble destruction with ultrasound. Circulation. 1998;98:1264–1267. doi: 10.1161/01.cir.98.13.1264. [DOI] [PubMed] [Google Scholar]
- 30.Wu Y, Unger EC, McCreery TP, Sweitzer RH, Shen D, Wu G, et al. Binding and lysing of blood clots using MRX-408. Invest Radiol. 1998;33:880–885. doi: 10.1097/00004424-199812000-00006. [DOI] [PubMed] [Google Scholar]