Abstract
The ring finger protein 213 gene (RNF213) is involved in several vascular diseases, both intracranial and systemic ones. Some variants are common in the Asian population and are reported as a risk factor for moyamoya disease, intracranial stenosis and intracranial aneurysms. Among intracranial vascular diseases, both moyamoya disease and intracranial artery dissection are more prevalent in the Asian population. We performed a systematic review of the literature, aiming to assess the rate of RNF213 variants in patients with spontaneous intracranial dissections. Four papers were identified, providing data on 53 patients with intracranial artery dissection. The rate of RNF213 variants is 10/53 (18.9%) and it increases to 10/29 (34.5%), excluding patients with vertebral artery dissection. All patients had the RNF213 p.Arg4810Lys variant. RNF213 variants seems to be involved in intracranial dissections in Asian cohorts. The small number of patients, the inclusion of only patients of Asian descent and the small but non-negligible coexistence with moyamoya disease familiarity might be limiting factors, requiring further studies to confirm these preliminary findings and the embryological interpretation.
Keywords: RNF213, moyamoya disease, intracranial artery dissection, magnetic resonance angiography, intracranial stenosis, atherosclerosis
1. Introduction
The ring finger protein 213 gene (RNF213; NM_001256071.2) encodes a 590 kDa protein containing a RING finger domain with E3 ubiquitin–protein ligase activity and two regions of ATPase-associated domains. RNF213 is related to angiogenesis and vascular inflammation in experiments in vitro and in vivo, but its exact physiologic functions remain unknown [1]. Its role as a vasculopathy–susceptibility locus was demonstrated in 2011 in a cohort of Japanese families with moyamoya disease, investigated through genome-wide linkage analysis, identifying heterozygosity for RNF213 p.Arg4810Lys (c.14429G>A, rs112735431) polymorphism as significantly associated with the disease [2]. Moyamoya disease is an intracranial, non-atherosclerotic, non-inflammatory steno-occlusive progressive disease, characterized by the development of compensatory collateral networks, which give the disease its name [3]. After this first demonstration, a genome-wide association study analysis in Japanese patients with moyamoya disease found that 95% and 73% of familial and non-familial patients, respectively, had the RNF213 p.Arg4810Lys variant, providing an odds ratio of 190.8 for having moyamoya disease [4]. The same association was documented in Korean and Chinese cohorts of moyamoya patients [5,6] with a lower allele frequency for the RNF213 p.Arg4810Lys variant in Chinese patients compared to Japanese and Korean patients, and another variant also being present in Chinese patients (RNF213 p.Ala5021Val) as a susceptibility factor for the development of moyamoya disease [7]. In large cohorts, the RNF213 (c.14576G>A) mutation was reported in 69.9–85.4% of cases of moyamoya disease [8,9,10]. In non-Asian patients, and particularly in Caucasian patients, the RNF213 p.Arg4810Lys variant is extremely rare, and several different pathogenetic variants of RNF213 have been identified [7] with a lower odds ratio (2.24) [11], showing a strong association with moyamoya disease only in familial cases [7].
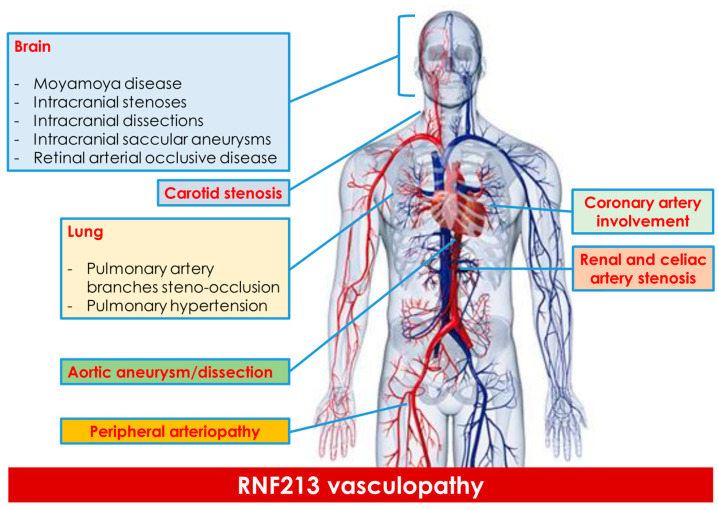
Additionally, the RNF213 c.14576G>A variant has been implicated in other vascular diseases. The first description was of the pulmonary (peripheral pulmonary artery stenosis with pulmonary hypertension) and coronary arteries [12], which are sometimes associated with moyamoya disease [11,13], particularly in carriers of the homozygous mutation of RNF213, p.Arg4810Lys. In the following years, the concept of RNF213-associated vasculopathy was developed [14]. It has been suggested that heterozygous R4810K variant causes classical moyamoya disease, but the same variant is associated with moyamoya disease and systemic vascular disease when present in the homozygous state, in a gene dosage-dependent manner [11]. Homozygous patients showed a diffuse narrowing of the aorta and iliofemoral arteries, together with stenosis of renal, celiac or peripheral pulmonary arteries, with or without moyamoya disease [15]. However, heterozygous patients were mostly asymptomatic or had isolated moyamoya disease. This association suggests a high penetrance of systemic vasculopathy in homozygous patients and a low penetrance of moyamoya disease in heterozygous patients.
Returning to the intracranial arteries, in East Asian patients, the RNF213 (c.14576G>A) variant is implicated in 21–23.2% of intracranial internal carotid artery stenosis (ICS) cases, but not in vertebral artery stenosis [9,16]. This variant is notably prevalent among East Asians without intracranial disease, with allele frequencies of 2.8% in Japanese patients, 2.5% in Korean patients and 1.1% in Chinese patients, while it is rarely found in Western Caucasians [9,17]. The reported Minor Allele Frequency9 (MAF) for RNF213 is 0.0012 and it significantly increases the risk of having moyamoya disease in Japanese, Korean and Chinese patients Interestingly, the frequency of RNF213 (c.14576G>A) in Japanese patients with cerebral aneurysms (CAN) is lower than in those with ICS and is similar to that in control subjects without vascular lesions, ranging from 0 to 2.1% [18]. Moreover, RNF213 variants (p.Arg2438Cys and p.Ala2826Thr) have been identified in French–Canadian patients with intracranial aneurysms. However, few studies have explored the relationship between intracranial aneurysms and RNF213, failing to clarify the site, morphology (saccular, fusiform or dissected) and clinical characteristics of these aneurysms [19]. The etiology of intracranial aneurysms varies based on the site of origin within the intracranial vessels, exhibiting different frequencies in men and women, as well as varying rupture rates. Therefore, assessing these aneurysms requires a nuanced approach considering their diverse origins and characteristics [20,21]. Figure 1 summarizes the main sites of arterial diseases associated with RNF213 variants.
Figure 1.
The main sites of systemic vasculopathy described in RNF213 variants are summarized.
Intracranial artery dissection is a rare neurovascular condition whose genetic underpinnings are less understood compared to extracranial artery dissection [22,23]. Most research involves patients from Asia, with 95% of studies involving more than 40 patients and 61% of studies including 20 to 39 patients focusing on this population [24,25,26,27,28]. Among adults, a higher incidence of intracranial artery dissection is observed in Asian men, a trend not seen in non-Asian populations. The average age at diagnosis is 50.4 years (ranging from 47 to 61 years) [22], with older patients being more likely to present with subarachnoid hemorrhage. The differences in the prevalence and characteristics of intracranial artery dissections between ethnic groups, as well as the higher frequency in children compared to adults, indicate potential genetic risk factors. However, the genetic basis for intracranial artery dissections remains largely unexplored. In this systematic review, we aimed to assess the prevalence of RNF213 variants in intracranial artery dissection in Asian population, as both issues are more prevalent in Asian than in non-Asian people.
2. Materials and Methods
A systematic review of the published papers reporting RNF213 variations in patients with acute spontaneous intracranial artery dissection was performed, following the Meta-Analyses and Systematic Reviews of Observational Studies (MOOSE) group guidelines [29]. We searched PubMed and EMBASE databases for studies addressing RNF213 status in spontaneous intracranial artery dissection without lower time limits until 28 February 2024. We used the following keywords for PubMed: “((RNF213) OR (ring finger protein 213))” AND “(intracranial artery dissection)”. We excluded patients with moyamoya disease and traumatic or iatrogenic intracranial artery dissection. In addition, we applied forward and backward citation tracking to improve the results. All studies presenting original data about the topic of the review were included. We limited the selection to English studies and excluded case reports and studies on nonhuman subjects. Abstracts presented at relevant scientific meetings were excluded because of the lack of relevant information. We avoided including duplicated datasets. Two investigators (MZ, RP) independently screened the papers retrieved in the literature search according to the previously detailed criteria. The NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [30] was used to evaluate each eligible publication. The following information was extracted: authors, year of publication, country, number of patients and main demographic and diagnostic features, RNF213 variants and the rate of their identification. In the case of missing values, we tried to derive them whenever possible [30]. Disagreements between the two reviewers were addressed and resolved by consensus.
3. Results
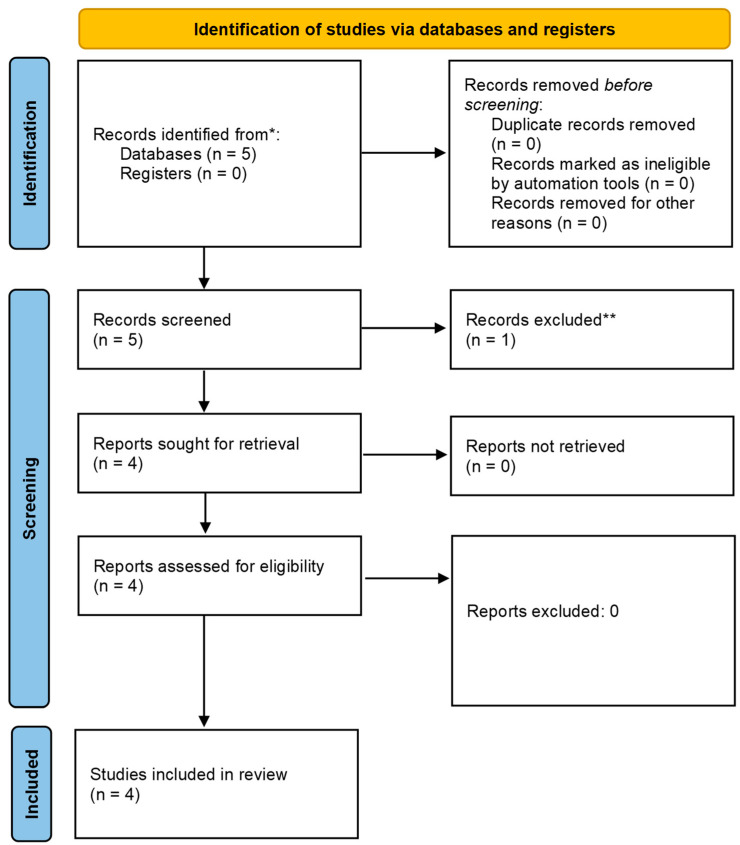
The systematic review of the available literature was performed in accordance with the Section 2. The selection of the studies is summarized in the PRISMA diagram [31] (Figure 2).
Figure 2.
PRISMA diagram [31]. ** The excluded paper [32] included both symptomatic and asymptomatic patients with intracranial artery diseases and relies on a single MRI technique to diagnose the subtype of the disease, and this is not reliable for intracranial artery dissections. Moreover, details on RNF213 polymorphisms were not provided.
A total number of four studies were retrieved and analyzed. The citation tracking did not find any other published report about the topic of the review. The results of the data extraction are summarized in Table 1.
Table 1.
Data of the included studies on RNF213 testing in intracranial artery dissection.
| Reference | Country | Intracranial Artery Dissection Patients (N) | Sex | Age (Years) (Mean ± SD) | Dissected Artery | Diagnostic Technique (N) | Genetic Testing | RNF213 Variants (N/%) | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Kim JS 2018 [33] | Korea | 24 cases vs. 24 age and sex matched controls | 8 males (33.3%) | 41.8 ± 10.2 | 21 MCA, 2 ICA, 1 PCA | MRA (n = 21), CTA (n = 3), DSA (n = 13), HRMRA (n = 21). | Blood samples for major SNIPs of RNF213 in East Asian patients [2] (p.D4013N, p.P4608S, p.R4810K, p.R4853K, p.D4836N and p.E4950D) amplifying and sequencing three exons (44, 60 and 62) |
8 (33.3) in cases vs. 1 (4.2) in controls All had heterozygous p.R4810K (c.14576G>A) variant |
11 had ischemic stroke, 7 had TIA, 3 had headache, and 3 pts were asymptomatic |
| Tashiro R et al., 2019 [34] | Japan | 24 patients with intracranial VA dissection, 62 patients with moyamoya disease and 48 healthy controls | NR | NR | Intracranial VA | MRA and BPAS-MRI were used to diagnose intracranial VA dissection [35] |
Saliva sample for RNF213 c.14576G>A polymorphism |
69.0% (40/58) in the moyamoya disease group, 0% (0/24) in the intracranial VAD group and 4.2% (2/48) in the healthy control group |
|
| Shinya Y 2020 [36] | Japan | 1 | Woman | 63 | MCA | MRA DSA |
Blood sample | p.Arg4810Lys (rs112735431) variant | Subarachnoid hemorrhage with left MCA dissection resulting in an irregular shape and fusiform dilation of the left M2 MCA wall. Progression to moyamoya disease pattern |
| Kim YJ 2016 [37] | Korea | 4/81 patients had MCA dissection | NR | NR | MCA | MRA HR-MRI [38] |
Blood samples for major SNIPs of RNF213 in East Asian patients [2] (p.D4013N, p.P4608S, p.R4810K, p.R4853K, p.D4836N and p.E4950D) amplifying and sequencing three exons (44, 60 and 62) |
Only the heterozygote of p.R4810K was more frequent in the non-atherosclerosis group than the atherosclerosis group (62.5% [10/16] versus 26.7% [4/15], respectively; p = 0.045). |
81 patients < 60 years old with isolated MCA steno-occlusion: 45 (56.6%) in the atherosclerosis and 36 (44.4%) in the nonatherosclerosis Group. 28/36 (77.8%) in non-atherosclerosis group had suspected moyamoya disease |
SNIPs: single-nucleotide polymorphisms; MCA: middle cerebral artery; ICA: internal carotid artery; PCA: posterior cerebral artery; SD: standard deviation; TIA: transient ischemic attack; MRA: Magnetic Resonance Angiography; CTA: Computed Tomography Angiography; HRMRA: high-resolution MRA; VA: vertebral artery.
The rate of RNF213 variants in intracranial artery dissection is reported as 10/53 (18.9%) and increases to 10/29 (34.5%) when excluding patients with VA dissection. All patients had the RNF213 p.Arg4810Lys variant.
4. Discussion
The RNF213 gene plays a significant role in the ethnic disparity observed in the localization of cerebral vascular diseases. Initially recognized as a susceptibility gene for moyamoya disease [39], RNF213 variants are now linked to a broader spectrum of vascular conditions beyond moyamoya [40], including intracranial atherosclerosis. This association underscores the gene’s involvement in various non-moyamoya vascular diseases, further highlighting its significance in understanding the genetic underpinnings of cerebral vascular disorders [11,16,33,37]. In addition, the RNF213 R4810K variant is associated with smaller intracranial arteries, suggesting impaired vasculogenesis [41,42]. Hongo et al. showed that the outer diameter of the MCA was smaller in R4810K carriers [41]. Moreover, negative remodeling, investigated with high-resolution MRI, involves all the intracranial arteries; the stenotic MCA segments are measured in patients with this variant [42], predisposing the smaller intracranial arteries to hemodynamic compromise. The exact role and mechanisms of RNF213-related vascular impairment are not well known and whether RNF213 mutations induce a loss-of-function or gain-of-function allele status is controversial. Missense mutations might disrupt gene transcription and protein function to a certain extent, causing the pathological dysregulation of substrate ubiquitination due to changes in the functional domain [43,44]. Among the studies suggesting the role of RNF213 in vascular wall construction [2], a functional study on the RNF213 p.Arg4810Lys variant proposed that mutations in the founder are a risk factor for moyamoya disease through reduced angiogenic activity [45,46] and induced mitotic abnormalities [47]. A study on animal models found a link to a variety of artery-wall developments, showing thinning of the intima and media layers after ligation of the common carotid artery in RNF213-knockout mice [48], thinning in vascular walls and increased Mmp9 expression [49] or enhanced post-ischemic angiogenesis [50]. Moreover, RNF213 was associated with inflammatory responses and angiogenesis [45,51]. All these studies show an association between RNF213 and vascular remodeling processes, even the formation of an aneurysm after anastomotic surgery [52].
Several intracranial artery diseases are more prevalent in Asian than non-Asian populations: not only moyamoya disease, but also atheromasic stenosis and intracranial artery dissections. In non-Asians, intracranial dissections account for <10% of all dissections [53], whereas, in Asians, intracranial artery dissections are more common than extracranial artery dissections [15,54]. Genetic variation may partially explain these differences, and RNF213, which is highly prevalent in Asian populations, might be one of the candidate genes to be investigated. In the small cohort described by Kim et al. [33], of the twenty-four patients with intracranial artery dissection, eight (33.3%) had an RNF213 variant. All patients had the same heterozygous p.R4810K (c.14576G>A) variant, with a significantly higher prevalence (p = 0.023) in patients with intracranial artery dissection compared to controls. Interestingly, after adjusting for hypertension and RNF213 polymorphism, both hypertension (adjusted odds ratio [OR], 10.185; 95% confidence interval [CI], 1.066 to 97.305; p = 0.04) and the presence of the RNF213 variant (adjusted OR, 14.247; 95% CI, 1.563 to 129.841; p = 0.018) were independently associated with intracranial artery dissection. In the control group, eight patients with extracranial ICA dissection were included and none had RNF213 variants. Notably, one of the patients with intracranial artery dissection and the RNF213 variant had a family history of moyamoya disease.
In addition, Kim et al. [36] investigated the relationship between MCA steno-occlusion and RNF213 variants, finding that one of their four patients with intracranial MCA dissection harbored the c.14576G>A variant, but only a minority of the enrolled patients underwent genetic testing: 31 patients, 16/36 (44.4%), in the non-atherosclerosis group and 15/45 (33.3%) in the atherosclerosis group. Thirteen cases were heterozygous for RNF213 variants. RNF213 heterozygotes were more frequent in the non-atherosclerosis than in the atherosclerosis group. It is interesting to note that the diagnostic criteria for moyamoya disease were primarily developed for children and it is not completely known if they might be applied in the same way to adults. In fact, adult-onset moyamoya disease can present with unilateral MCA steno-occlusion [26], progressing over years to bilateral moyamoya disease [55,56]. In addition, a focal MCA stenosis without the sufficient development of moyamoya collaterals at the early stages of adult-onset moyamoya disease has been described [57], and even the initial involvement of the mid-portion of M1 MCA [58]. Shinya et al. [36] reported a case of a patient with an MCA dissection and the RNF213 p.Arg4810Lys, which progressed to involve ICA with a moyamoya disease-like angiogenesis over six years. This case might help to consider some non-atherosclerotic intracranial diseases as a continuum or overlapping entities. The RNF213 p.Arg4810Lys variant could be a common susceptibility factor. It was found in about 80% of moyamoya disease patients in Asia [59], in non-cardioembolic cerebral infarction in the Japanese population [59], in about 2% of the general population in East Asian people as a stroke-related genetic factor [2,4,60,61] and, finally, in several systemic vascular diseases, such as coronary stenosis, pulmonary hypertension and intracranial artery stenosis [11,12,15,61,62,63,64,65].
Tashiro R et al. [34] considered only patients with intracranial VA dissection in comparison with patients with moyamoya disease, using the fragility of the vessels as their mean trait. The authors found the RNF213 c.14576G>A variant in 69.0% (40/58) of the moyamoya disease group, 0% (0/24) of the intracranial VA dissection group and 4.2% (2/48) of the healthy control group. These differences were significant in the adjusted multivariate analysis. In a cohort of patients with intracranial atherosclerosis, Shinya et al. [16] did not find patients with atherosclerotic lesions in the posterior circulation harboring the RNF c.14576G>A variant, suggesting that there is no relationship between this gene and vascular lesions in the posterior circulation.
From an embryological standpoint, there is a theory that views moyamoya disease through the lens of neurocristopathy, suggesting that it primarily affects arteries derived from the neural crest rather than those of mesodermal origin. From this perspective, the RNF213 gene variants are not only observed in moyamoya disease patients but also in those with anterior circulation atherosclerosis rather than posterior circulation [16,33,38]. However, delineating between anterior and posterior circulation can be challenging, as highlighted by Komiyama et al. [66]. Komiyama proposed that moyamoya disease represents a progressive arteriopathy of the primitive ICA, with its pathogenesis being influenced by genetic factors. Notably, he emphasized that the distal cortical branches of the primitive ICA, vertebral artery, basilar artery and external carotid artery remain unaffected, while steno-occlusive changes primarily occur near the bifurcation of the cranial and caudal divisions of the primitive ICA [66]. The existing data regarding the absence of RNF213 variants in posterior circulation atherosclerosis are insufficient to draw conclusive conclusions, especially considering that some arteries in the posterior circulation derive from the neural crest. Komiyama et al. [66] outlined the embryological distribution of neural crest cells, which extends to the territory of the primitive ICA and divides into cranial and caudal divisions at the origin of the posterior communicating artery [67]. The cranial division includes the distal ICA, anterior and middle cerebral arteries and the anterior choroidal artery, while the caudal division comprises the posterior communicating artery, the P1 segment of the posterior cerebral artery, the distal basilar artery and other arteries [68]. During early embryogenesis, significant vascular transformations occur, including the shift of the telencephalic branch of the primitive anterior choroidal artery to the caudal division of the primitive ICA, eventually forming the P2-4 segments of the posterior cerebral artery [67,68,69]. This process results in the dispersion of neural crest cells to various arterial structures, contributing to the formation of the arterial circle of Willis and its branches. The exact embryological border between the primitive internal carotid system and the vertebro-basilar system remains variable. It has been suggested that RNF213, a susceptibility gene for moyamoya disease, may primarily affect derivatives of the primitive ICA among intracranial vessels. However, it is important to note that RNF213 has not been implicated in congenital ICA and MCA anomalies in a Japanese case series. Nevertheless, there have been reports of individuals with RNF213 gene mutations presenting with ruptured MCA peripheral multiple aneurysms associated with twig-like MCA [70].
The hypothesis emerging from these observations is that RNF213 variants may be associated with intracranial artery dissection, potentially increasing the vulnerability of intracranial arteries to dissection. This aligns with the broader role of RNF213 polymorphisms as non-specific markers that increase the vulnerability to intracranial arterial diseases, possibly acting as one of multiple predisposing factors [39]. This hypothesis may partially explain the higher prevalence and risk of intracranial arterial diseases, including intracranial atherosclerosis and artery dissections, in Asian populations [71], where RNF213 variants are more prevalent among East Asians than Caucasians [38]. However, the strength of this association is generally low, and the various limitations outlined in individual studies may affect the final conclusions. One limitation of the general interpretation of the causative role of RNF213 variants in intracranial and systemic arteriopathies lies in the structural properties of this gene. Indeed, RNF213 has a very long open reading frame, encoding a huge protein (length greater than 5000 aminoacyds). Due to these properties, and particularly the length of the gene, rare variants or mutations that affect the protein coding capacity might be expected at a higher rate. This issue should lead to caution in the interpretation of the role of variants of unknown significance.
A final observation might be raised about the association of RNF213 variants with intracranial and systemic vascular disease, including intracranial dissection, moyamoya disease, intracranial aneurisms and visceral stenoses (i.e., renal artery stenosis) and the independent role of arterial hypertension as risk factor for intracranial dissection. This pattern could resemble the known focal form of fibromuscular disease [72], where intracranial involvement apart from aneurysms is rare but has been reported.
5. Conclusions
RNF213 is a gene involved in vascular wall remodeling and documented as a susceptibility marker in several intracranial and systemic vascular diseases, particularly in Asian populations. It might also be involved in intracranial artery dissection and the actual rate ranges from 18.9% to 34.5%, depending on the inclusion or exclusion of VA dissections. All patients had the RNF213 p.Arg4810Lys variant. The small number of patients, the inclusion of only patients of Asian descent and the small but non-negligible coexistence with moyamoya disease familiarity might be limiting factors, requiring further studies to confirm these preliminary findings and the embryological interpretation.
Author Contributions
Conceptualization, M.Z. and R.P.; methodology, M.Z. and R.P.; literature search and screening: M.Z., I.G., F.A., M.N. and C.M.; writing—original draft preparation, M.Z. and R.P.; writing—review and editing, M.Z., I.G., F.A., M.N., C.M., S.D., G.D.C., L.B., C.P., M.S.S., A.P., F.V. and R.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Koizumi A., Kobayashi H., Hitomi T., Harada K.H., Habu T., Youssefian S. A new horizon of moyamoya disease and associated health risks explored through RNF213. Environ. Health Prev. Med. 2016;21:55–70. doi: 10.1007/s12199-015-0498-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu W., Morito D., Takashima S., Mineharu Y., Kobayashi H., Hitomi T., Hashikata H., Matsuura N., Yamazaki S., Toyoda A., et al. Identification of RNF213 as a susceptibility gene for moyamoya disease and its possible role in vascular development. PLoS ONE. 2011;6:e22542. doi: 10.1371/journal.pone.0022542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hashimoto N., Tominaga T., Miyamoto S., Nagata I., Houkin K., Suzuki N., Takagi Y., Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis. Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis) Neurol. Med. Chir. 2012;52:245–266. doi: 10.2176/nmc.52.245. [DOI] [PubMed] [Google Scholar]
- 4.Kamada F., Aoki Y., Narisawa A., Abe Y., Komatsuzaki S., Kikuchi A., Kanno J., Niihori T., Ono M., Ishii N., et al. A genome-wide association study identifies RNF213 as the first Moyamoya disease gene. J. Hum. Genet. 2011;56:34–40. doi: 10.1038/jhg.2010.132. [DOI] [PubMed] [Google Scholar]
- 5.Lin J., Sheng W. RNF213 variant diversity predisposes distinct populations to dissimilar cerebrovascular diseases. BioMed Res. Int. 2018;2018:6359174. doi: 10.1155/2018/6359174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun X.S., Wen J., Li J.X., Lai R., Wang Y.-F., Liu H.-J., Sheng W.-L. The association between the ring finger protein 213 (RNF213) polymorphisms and moyamoya disease susceptibility: A meta-analysis based on case-control studies. Mol. Genet. Genom. 2016;291:1193–1203. doi: 10.1007/s00438-016-1172-5. [DOI] [PubMed] [Google Scholar]
- 7.Guey S., Kraemer M., Hervé D., Ludwig T., Kossorotoff M., Bergametti F., Schwitalla J.C., Choi S., Broseus L., Callebaut I., et al. Rare RNF213 variants in the C-terminal region encompassing the RING-finger domain are associated with moyamoya angiopathy in Caucasians. Eur. J. Hum. Genet. 2017;25:995–1003. doi: 10.1038/ejhg.2017.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyawaki S., Imai H., Shimizu M., Yagi S., Ono H., Mukasa A., Nakatomi H., Shimizu T., Saito N. Genetic variant RNF213 c.14576G>A in various phenotypes of intracranial major artery stenosis/occlusion. Stroke. 2013;44:2894–2897. doi: 10.1161/STROKEAHA.113.002477. [DOI] [PubMed] [Google Scholar]
- 9.Liao X., Deng J., Dai W., Zhang T., Yan J. Rare variants of RNF213 and moyamoya/non-moyamoya intracranial artery stenosis/occlusion disease risk: A meta-analysis and systematic review. Environ. Health Prev. Med. 2017;22:75. doi: 10.1186/s12199-017-0680-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishisaka E., Watanabe A., Murai Y., Shirokane K., Matano F., Tsukiyama A., Baba E., Nakagawa S., Tamaki T., Mizunari T., et al. Role of RNF213 polymorphism in defining quasi-moyamoya disease and definitive moyamoya disease. Neurosurg. Focus. 2021;51:E2. doi: 10.3171/2021.5.FOCUS21182. [DOI] [PubMed] [Google Scholar]
- 11.Fukushima H., Takenouchi T., Kosaki K. Homozygosity for moyamoya disease risk allele leads to moyamoya disease with extracranial systemic and pulmonary vasculopathy. Am. J. Med. Genet. A. 2016;170:2453–2456. doi: 10.1002/ajmg.a.37829. [DOI] [PubMed] [Google Scholar]
- 12.Bang O.Y., Chung J.W., Kim D.H., Won H.H., Yeon J.Y., Ki C.S., Shin H.J., Kim J.S., Hong S.C., Kim D.K., et al. Moyamoya Disease and Spectrums of RNF213 Vasculopathy. Transl. Stroke Res. 2020;11:580–589. doi: 10.1007/s12975-019-00743-6. [DOI] [PubMed] [Google Scholar]
- 13.Suzuki H., Kataoka M., Hiraide T., Aimi Y., Yamada Y., Katsumata Y., Chiba T., Kanekura K., Isobe S., Sato Y., et al. Genomic comparison with supercentenarians identifies RNF213 as a risk gene for pulmonary arterial hypertension. Circ. Genom. Precis. Med. 2018;11:e002317. doi: 10.1161/CIRCGEN.118.002317. [DOI] [PubMed] [Google Scholar]
- 14.Hiraide T., Suzuki H., Momoi M., Shinya Y., Fukuda K., Kosaki K., Kataoka M. RNF213-Associated Vascular Disease: A Concept Unifying Various Vasculopathies. Life. 2022;12:555. doi: 10.3390/life12040555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang S.A., Song J.S., Park T.K., Yang J.H., Kwon W.C., Kim S.R., Kim S.R., Kim S.M., Cha J., Jang S.Y., et al. Nonsyndromic peripheral pulmonary artery stenosis is associated with homozygosity of RNF213 p.Arg4810Lys regardless of cooccurrence of moyamoya disease. Chest. 2018;153:404–413. doi: 10.1016/j.chest.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 16.Shinya Y., Miyawaki S., Imai H., Hongo H., Ono H., Takenobu A., Nakatomi H., Teraoka A., Saito N. Genetic Analysis of Ring Finger Protein 213 (RNF213) c.14576G>A in Intracranial Atherosclerosis of the Anterior and Posterior Circulations. J. Stroke Cerebrovasc. Dis. 2017;26:2638–2644. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.043. [DOI] [PubMed] [Google Scholar]
- 17.Wang X., Wang Y., Nie F., Li Q., Zhang K., Liu M., Yang L., Zhang Q., Liu S., Zeng F., et al. Association of Genetic Variants with Moyamoya Disease in 13,000 Individuals: A Meta-Analysis. Stroke. 2020;51:1647–1655. doi: 10.1161/STROKEAHA.120.029527. [DOI] [PubMed] [Google Scholar]
- 18.Zhou S., Ambalavanan A., Rochefort D., Xie P., Bourassa C.V., Hince P., Dionne-Laporte A., Spiegelman D., Gan-Or Z., Mirarchi C., et al. RNF213 Is Associated with Intracranial Aneurysms in the French-Canadian Population. Am. J. Hum. Genet. 2016;99:1072–1085. doi: 10.1016/j.ajhg.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyawaki S., Imai H., Takayanagi S., Mukasa A., Nakatomi H., Saito N. Identification of a genetic variant common to moyamoya disease and intracranial major artery stenosis/occlusion. Stroke. 2012;43:3371–3374. doi: 10.1161/STROKEAHA.112.663864. [DOI] [PubMed] [Google Scholar]
- 20.UCAS Japan Investigators The Natural Course of Unruptured Cerebral Aneurysms in a Japanese Cohort. N. Engl. J. Med. 2012;366:2474–2482. doi: 10.1056/NEJMoa1113260. [DOI] [PubMed] [Google Scholar]
- 21.Zheng J., Zhang J. Neoplastic cerebral aneurysm from metastatic tumor: A systematic review of clinical and treatment characteristics. Clin. Neurol. Neurosurg. 2015;128:107–111. doi: 10.1016/j.clineuro.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 22.Debette S., Compter A., Labeyrie M.A., Uyttenboogaart M., Metso T.M., Majersik J.J., Goeggel-Simonetti B., Engelter S.T., Pezzini A., Bijlenga P., et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015;14:640–654. doi: 10.1016/S1474-4422(15)00009-5. [DOI] [PubMed] [Google Scholar]
- 23.Traenka C., Kloss M., Strom T., Lyrer P., Brandt T., Bonati L.H., Grond-Ginsbach C., Engelter S. Rare genetic variants in patients with cervical artery dissection. Eur. Stroke J. 2019;4:355–362. doi: 10.1177/2396987319861869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwak J.H., Choi J.W., Park H.J., Chae E.Y., Park E.S., Lee D.H., Suh D.C. Cerebral artery dissection: Spectrum of clinical presentations related to angiographic findings. Neurointervention. 2011;6:78–83. doi: 10.5469/neuroint.2011.6.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang Y.C., Chen Y.F., Wang Y.H., Tu Y.K., Jeng J.S., Liu H.M. Cervicocranial arterial dissection: Experience of 73 patients in a single center. Surg. Neurol. 2009;72((Suppl. S2)):S20–S27. doi: 10.1016/j.surneu.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Kim B.M., Kim S.H., Kim D.I., Shin Y.S., Suh S.H., Kim D.J., Park S.I., Park K.Y., Ahn S.S. Outcomes and prognostic factors of intracranial unruptured vertebrobasilar artery dissection. Neurology. 2011;76:1735–1741. doi: 10.1212/WNL.0b013e31821a7d94. [DOI] [PubMed] [Google Scholar]
- 27.Nakajima S., Tsukahara T., Minematsu K. A study of vertebrobasilar artery dissection with subarachnoid hemorrhage. Acta Neurochir. Suppl. 2010;107:45–49. doi: 10.1007/978-3-211-99373-6_7. [DOI] [PubMed] [Google Scholar]
- 28.Yamaura A., Ono J., Hirai S. Clinical picture of intracranial non-traumatic dissecting aneurysm. Neuropathology. 2000;20:85–90. doi: 10.1046/j.1440-1789.2000.00276.x. [DOI] [PubMed] [Google Scholar]
- 29.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 30.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim H.J., Choi E.H., Chung J.W., Kim J.H., Kim Y.S., Seo W.K., Kim G.M., Bang O.Y. Luminal and Wall Changes in Intracranial Arterial Lesions for Predicting Stroke Occurrence. Stroke. 2020;51:2495–2504. doi: 10.1161/STROKEAHA.120.030012. [DOI] [PubMed] [Google Scholar]
- 33.Kim J.S., Lee H.B., Kwon H.S. RNF213 Polymorphism in Intracranial Artery Dissection. J. Stroke. 2018;20:404–406. doi: 10.5853/jos.2018.02075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tashiro R., Fujimura M., Sakata H., Endo H., Tomata Y., Sato-Maeda M., Niizuma K., Tominaga T. Genetic analysis of ring finger protein 213 (RNF213) c.14576G>A polymorphism in patients with vertebral artery dissection: A comparative study with moyamoya disease. Neurol Res. 2019;41:811–816. doi: 10.1080/01616412.2019.1615726. [DOI] [PubMed] [Google Scholar]
- 35.Itabashi R., Mori E., Furui E., Sato S., Yazawa Y., Kawata K., Fujiwara S. A dilated surface appearance on basiparallel anatomic scanning-magnetic resonance imaging is a useful tool for the diagnosis of spontaneous vertebral artery dissection in lateral medullary infarction. J. Stroke Cerebrovasc. Dis. 2014;23:805–810. doi: 10.1016/j.jstrokecerebrovasdis.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 36.Shinya Y., Miyawaki S., Nakatomi H., Shin M., Teraoka A., Saito N. Hemorrhagic Onset Intracranial Artery Dissection of Middle Cerebral Artery Followed by Progressive Arterial Stenosis with Genetic Variant RNF213 p.Arg4810Lys (rs112735431) World Neurosurg. 2020;141:192–195. doi: 10.1016/j.wneu.2020.04.241. [DOI] [PubMed] [Google Scholar]
- 37.Kim Y.J., Lee J.K., Ahn S.H., Kim B.J., Kang D.W., Kim J.S., Kwon S.U. Nonatherosclerotic isolated middle cerebral artery disease may be early manifestation of moyamoya disease. Stroke. 2016;47:2229–2235. doi: 10.1161/STROKEAHA.116.012751. [DOI] [PubMed] [Google Scholar]
- 38.Kwak H.S., Hwang S.B., Chung G.H., Jeong S.K. High-resolution magnetic resonance imaging of symptomatic middle cerebral artery dissection. J. Stroke Cerebrovasc. Dis. 2014;23:550–553. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 39.Fujimura M., Sonobe S., Nishijima Y., Niizuma K., Sakata H., Kure S., Tominaga T. Genetics and biomarkers of moyamoya disease: Significance of RNF213 as a susceptibility gene. J. Stroke. 2014;16:65–72. doi: 10.5853/jos.2014.16.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bang O.Y., Fujimura M., Kim S.K. The pathophysiology of moyamoya disease: An update. J. Stroke. 2016;18:12–20. doi: 10.5853/jos.2015.01760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hongo H., Miyawaki S., Imai H., Shinya Y., Ono H., Mori H., Nakatomi H., Kunimatsu A., Saito N. Smaller outer diameter of atherosclerotic middle cerebral artery associated with RNF213 c.14576G>A variant (rs112735431) Surg. Neurol Int. 2017;8:104. doi: 10.4103/sni.sni_59_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi E.H., Lee H., Chung J.W., Seo W.K., Kim G.M., Ki C.S., Kim Y.C., Bang O.Y. Ring Finger Protein 213 Variant and Plaque Characteristics, Vascular Remodeling, and Hemodynamics in Patients with Intracranial Atherosclerotic Stroke: A High-Resolution Magnetic Resonance Imaging and Hemodynamic Study. J. Am. Heart Assoc. 2019;8:e011996. doi: 10.1161/JAHA.119.011996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahel J., Lehner A., Vogel A., Schleiffer A., Meinhart A., Haselbach D., Clausen T. Moyamoya disease factor RNF213 is a giant E3 ligase with a dynein-like core and a distinct ubiquitin-transfer mechanism. eLife. 2020;9:e56185. doi: 10.7554/eLife.56185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ye F., Niu X., Liang F., Dai Y., Liang J., Li J., Wu X., Zheng H., Qi T., Sheng W. RNF213 loss-of-function promotes pathological angiogenesis in moyamoya disease via the Hippo pathway. Brain. 2023;146:4674–4689. doi: 10.1093/brain/awad225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hitomi T., Habu T., Kobayashi H., Okuda H., Harada K.H., Osafune K., Taura D., Sone M., Asaka I., Ameku T., et al. Downregulation of Securin by the variant RNF213 R4810K (rs112735431, G>A) reduces angiogenic activity of induced pluripotent stem cell-derived vascular endothelial cells from moyamoya patients. Biochem. Biophys. Res. Commun. 2013;438:13–19. doi: 10.1016/j.bbrc.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 46.Kobayashi H., Matsuda Y., Hitomi T., Okuda H., Shioi H., Matsuda T., Imai H., Sone M., Taura D., Harada K.H., et al. Biochemical and Functional Characterization of RNF213 (Mysterin) R4810K, a Susceptibility Mutation of Moyamoya Disease, in Angiogenesis In Vitro and In Vivo. J. Am. Heart Assoc. 2015;4:4. doi: 10.1161/JAHA.115.002146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hitomi T., Habu T., Kobayashi H., Okuda H., Harada K.H., Osafune K., Taura D., Sone M., Asaka I., Ameku T., et al. The moyamoya disease susceptibility variant RNF213 R4810K (rs112735431) induces genomic instability by mitotic abnormality. Biochem. Biophys. Res. Commun. 2013;439:419–426. doi: 10.1016/j.bbrc.2013.08.067. [DOI] [PubMed] [Google Scholar]
- 48.Sonobe S., Fujimura M., Niizuma K., Nishijima Y., Ito A., Shimizu H., Kikuchi A., Arai-Ichinoi N., Kure S., Tominaga T. Temporal profile of the vascular anatomy evaluated by 9.4-T magnetic resonance angiography and histopathological analysis in mice lacking RNF213: A susceptibility gene for moyamoya disease. Brain Res. 2014;1552:64–71. doi: 10.1016/j.brainres.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 49.Sonobe S., Fujimura M., Niizuma K., Fujimura T., Furudate S., Nishijima Y., Kure S., Tominaga T. Increased vascular MMP-9 in mice lacking RNF213: Moyamoya disease susceptibility gene. Neuroreport. 2014;25:1442–1446. doi: 10.1097/WNR.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 50.Ito A., Fujimura M., Niizuma K., Kanoke A., Sakata H., Morita-Fujimura Y., Kikuchi A., Kure S., Tominaga T. Enhanced post-ischemic angiogenesis in mice lacking RNF213; a susceptibility gene for moyamoya disease. Brain Res. 2015;1594:310–320. doi: 10.1016/j.brainres.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 51.Ohkubo K., Sakai Y., Inoue H., Akamine S., Ishizaki Y., Matsushita Y., Sanefuji M., Torisu H., Ihara K., Sardiello M., et al. Moyamoya disease susceptibility gene RNF213 links inflammatory and angiogenic signals in endothelial cells. Sci. Rep. 2015;5:13191. doi: 10.1038/srep13191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fukushima Y., Miyawaki S., Inoue T., Shimizu S., Yoshikawa G., Imai H., Saito N., Tsutsumi K. Repeated de novo aneurysm formation after anastomotic surgery: Potential risk of genetic variant RNF213 c.14576G>A. Surg. Neurol. Int. 2015;6:41. doi: 10.4103/2152-7806.153709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guillon B., Lévy C., Bousser M.G. Internal carotid artery dissection: An update. J. Neurol. Sci. 1998;153:146–158. doi: 10.1016/S0022-510X(97)00287-6. [DOI] [PubMed] [Google Scholar]
- 54.Kwon J.Y., Kim N.Y., Suh D.C., Kang D.W., Kwon S.U., Kim J.S. Intracranial and extracranial arterial dissection presenting with ischemic stroke: Lesion location and stroke mechanism. J. Neurol. Sci. 2015;358:371–376. doi: 10.1016/j.jns.2015.09.368. [DOI] [PubMed] [Google Scholar]
- 55.Kelly M.E., Bell-Stephens T.E., Marks M.P., Do H.M., Steinberg G.K. Progression of unilateral moyamoya disease: A clinical series. Cerebrovasc. Dis. 2006;22:109–115. doi: 10.1159/000093238. [DOI] [PubMed] [Google Scholar]
- 56.Lee S.C., Jeon J.S., Kim J.E., Chung Y.S., Ahn J.H., Cho W.S., Son Y.J., Bang J.S., Kang H.S., Oh C.W. Contralateral progression and its risk factor in surgically treated unilateral adult moyamoya disease with a review of pertinent literature. Acta Neurochir. 2014;156:103–111. doi: 10.1007/s00701-013-1921-8. [DOI] [PubMed] [Google Scholar]
- 57.Kuroda S., Ishikawa T., Houkin K., Nanba R., Hokari M., Iwasaki Y. Incidence and clinical features of disease progression in adult moyamoya disease. Stroke. 2005;36:2148–2153. doi: 10.1161/01.STR.0000182256.32489.99. [DOI] [PubMed] [Google Scholar]
- 58.Goyal M.S., Hallemeier C.L., Zipfel G.J., Rich K.M., Grubb R.L., Jr., Chicoine M.R., Moran C.J., Cross D.T., III, Dacey R.G., Jr., Derdeyn C.P., et al. Clinical features and outcome in North American adults with idiopathic basal arterial occlusive disease without moyamoya collaterals. Neurosurgery. 2010;67:278–285. doi: 10.1227/01.NEU.0000371977.55753.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Akamatsu Y., Fujimura M., Uenohara H., Shimizu H., Tominaga T. Development of moyamoya disease in pregnancy and puerperium: Case report. Neurol. Med. Chir. 2014;54:824–826. doi: 10.2176/nmc.cr.2014-0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miyatake S., Miyake N., Touho H., Nishimura-Tadaki A., Kondo Y., Okada I., Tsurusaki Y., Doi H., Sakai H., Saitsu H., et al. Homozygous c.14576G>A variant of RNF213 predicts early-onset and severe form of moyamoya disease. Neurology. 2012;78:803–810. doi: 10.1212/WNL.0b013e318249f71f. [DOI] [PubMed] [Google Scholar]
- 61.Kamimura T., Okazaki S., Morimoto T., Kobayashi H., Harada K., Tomita T., Higashiyama A., Yoshimoto T., Takahashi J.C., Nakagawara J., et al. Prevalence of RNF213 p.R4810K Variant in Early-Onset Stroke with Intracranial Arterial Stenosis. Stroke J. Cereb. Circ. 2019;50:1561–1563. doi: 10.1161/STROKEAHA.118.024712. [DOI] [PubMed] [Google Scholar]
- 62.Morimoto T., Mineharu Y., Ono K., Nakatochi M., Ichihara S., Kabata R., Takagi Y., Cao Y., Zhao L., Kobayashi H., et al. Significant association of RNF213 p.R4810K, a moyamoya susceptibility variant, with coronary artery disease. PLoS ONE. 2017;12:e0175649. doi: 10.1371/journal.pone.0175649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kobayashi H., Kabata R., Kinoshita H., Morimoto T., Ono K., Takeda M., Choi J., Okuda H., Liu W., Harada K.H., et al. Rare variants in RNF213, a susceptibility gene for moyamoya disease, are found in patients with pulmonary hypertension and aggravate hypoxia-induced pulmonary hypertension in mice. Pulm. Circ. 2018;8:2045894018778155. doi: 10.1177/2045894018778155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koizumi A., Kobayashi H., Liu W., Fujii Y., Senevirathna S.T.M.L.D., Nanayakkara S., Okuda H., Hitomi T., Harada K.H., Takenaka K., et al. P.R4810K, a polymorphism of RNF213, the susceptibility gene for moyamoya disease, is associated with blood pressure. Environ. Health Prev. Med. 2013;18:121–129. doi: 10.1007/s12199-012-0299-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu S., Liu M., Li Q., Liu X., Wang Y., Mambiya M., Zhang K., Yang L., Zhang Q., Shang M., et al. Association of single nucleotide polymorphisms of MTHFR, TCN2, RNF213 with susceptibility to hypertension and blood pressure. Biosci. Rep. 2019;39:BSR20191454. doi: 10.1042/BSR20191454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Komiyama M. Moyamoya disease is a progressive arteriopathy of the primitive internal carotid artery. Interv. Neuroradiol. 2003;9:39–45. doi: 10.1177/159101990300900105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Padget D.H. The development of the cranial arteries in the human embryo. Contrib. Embryol. 1948;32:205–261. [Google Scholar]
- 68.Lasjaunias P., Berenstein A., ter Brugge K.G. Clinical Vascular Anatomy and Variations. 2nd ed. Springer; Berlin/Heidelberg, Germany: 2001. Intradural arteries. Surgical neuroangiography I; pp. 479–629. [Google Scholar]
- 69.Puelles L., Harrisom M., Paxinos G., Watson C. A developmental ontology for the mammalian brain based on the prosomeric model. Trends Neurosci. 2013;36:570–578. doi: 10.1016/j.tins.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 70.Fukuyama R., Yamamura K., Murata H., Miyatake S., Matsumoto N., Abe H. Ruptured aneurysm of an aplastic or twig-like middle cerebral artery with ring finger protein 213 mutation: A case report. No Shinkei Geka Neurol. Surg. 2020;48:533–540. doi: 10.11477/mf.1436204224. [DOI] [PubMed] [Google Scholar]
- 71.Yang W.J., Wong K.S., Chen X.Y. Intracranial atherosclerosis: From microscopy to high-resolution magnetic resonance imaging. J. Stroke. 2017;19:249–260. doi: 10.5853/jos.2016.01956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gornik H.L., Persu A., Adlam D., Aparicio L.S., Azizi M., Boulanger M., Bruno R.M., De Leeuw P., Fendrikova-Mahlay N., Froehlich J., et al. First international consensus on the diagnosis and management of fibromuscular dysplasia. J. Hypertens. 2019;37:229–252. doi: 10.1097/HJH.0000000000002019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.