Introduction
Infection with HIV causes a spectrum of clinical problems beginning at the time of seroconversion (primary HIV) and terminating with AIDS and death. It is now recognised that it may take 10 years or more for AIDS to develop after seroconversion. The Centers for Disease Control (CDC) in the USA developed the most widely used classification for HIV disease based on the presence of clinical symptoms and signs, the presence of certain conditions and investigative findings, the availability of HIV screening and the degree of immunosuppression as measured by the CD4 lymphocyte count. The infection is divided into four groups:
This article has been adapted from the forthcoming 5th edition of ABC of AIDS. The book will be available from the BMJ bookshop and at www.bmjbooks.com
Summary of CDC 1992 classification system for HIV disease
Group I Primary HIV
Group II Asymptomatic infection
Group III Persistent generalised lymphadenopathy
Group IV Symptomatic infection
Group IVA HIV wasting syndrome (AIDS) and constitutional disease
Group IVB HIV encephalopathy (AIDS) and neurological disease
Group IVC1 Major opportunistic infections specified as AIDS defining
Group IVC2 Minor opportunistic infections
Group IVD Cancers specified as AIDS defining
Group IVE Other conditions
Group I Primary HIV infection
Group II Asymptomatic phase
Group III Persistent generalised lymphadenopathy
Group IV Symptomatic infection
Group IV is subdivided into several subgroups and some of these (groups IVA, B, C1 and D) are AIDS defining conditions.
In 1992 the CDC included all HIV infected persons with CD4 lymphocyte counts of <200×106 cells/l as fulfilling an AIDS defining diagnosis. However, this additional classification is not widely used outside the USA.
A second classification also combines clinical and CD4 count information. Symptoms and clinical findings are graded in severity from A to C and CD4 counts as they fall from 1 to 3.
Group I Primary HIV infection
Primary HIV infection (PHI) is also called the seroconversion illness or acute HIV infection. It represents the stage of infection after the acquisition of the virus when antibodies are developing. Between 25% and 65% of people have been found to present with symptoms at the time of seroconversion. These can range from a mild, glandular fever-like illness to an encephalopathy. The severe symptoms are rare. The differential diagnosis of the mild seroconversion illness is protean and, without a high index of suspicion and a history indicating relevant risk behaviours or factors, the diagnosis may be missed.
Summary of CDC 1993 classification system for HIV disease
| CD4 lymphocyte count ×106/l | |||
|---|---|---|---|
|
(1)
|
(2)
|
(3)
|
|
| >500 | 200-499 | <199 | |
| (A) Asymptomatic including Groups I, II and III | A1 | A2 | A3 |
| (B) Symptomatic not A or C | B1 | B2 | B3 |
| (C) AIDS defining conditions | C1 | C2 | C3 |
The appropriate diagnostic tests for PHI, which should be carried out on serial blood samples, include tests for HIV antibodies and antigen. If these are negative and PHI is suspected, the definitive test is an HIV RNA polymerase chain reaction, which is the most sensitive test for the detection and quantification of the virus. Some of these assays are not routine and the interpretation of investigation results during PHI is difficult, therefore close consultation with colleagues in virology is strongly advised.
Clinical manifestations of primary HIV infection
| • Glandular fever-like illness | • Neurological symptoms |
| • Fever, malaise, diarrhoea, neuralgia | Meningitis |
| • Arthralgia, sore throat, headaches | Neuropathy |
| • Lymphadenopathy | Myelopathy |
| • Macular papular rash | Encephalopathy |
| • Ulceration | |
| Oropharynx | |
| Anogenital area | |
At the time of PHI there is sometimes a high rate of viral replication, leading to a transient rise in HIV viral load and concomitant immunosuppression due to a short lived fall in the CD4 count. This may result in manifestations of HIV disease which are normally seen later in the infection, for example oral candida. Diagnostic confusion as to the stage of HIV infection may arise, which can only be resolved by following up the patient for long enough to see the symptoms and signs resolve, HIV antibodies appear, the viral load fall and the CD4 count rise. Treatment should be directed at alleviating any symptoms, and there is considerable interest in the possible use of antiretroviral agents at this time because the virus may be more susceptible due to the relatively low numbers of virus particles which can replicate, the reduced ability of the predominantly non-syncytium inducing strains of virus to infect a wide variety of cell types and the enhanced immune response seen in PHI.
Such treatment may decrease long term damage to the immune system and delay or even prevent the development of AIDS. However, if not started within 12-18 months of PHI the theoretical advantage may be lost and, in any case, has to be balanced against the uncertain outcome, drug toxicity, adherence difficulties and the possibility of developing resistant virus, limiting future treatment options.
Differential diagnosis of glandular fever-like illness
| Condition | Test |
|---|---|
| Viral | |
| Infectious mononucleosis | Paul-Bunnell |
| Cytomegalovirus | Serology/culture |
| Rubella | Serology |
| Herpes simplex | HSV culture |
| Adenovirus | Serology |
| Hepatitis B/C | Serology |
| HIV | HIV, Ab, Ag, PCR |
| Protozoal | |
| Toxoplasmosis | Serology |
| Bacterial | |
| Syphilis | Serology |
| Streptococcal pharyngitis | Bacterial culture |
| Brucellosis | Serology |
| Neoplastic | |
| Lymphoma or leukaemia | Full blood count/diff |
| Lymph node biopsy | |
| Bone marrow | |
Group II Asymptomatic infection
After PHI, HIV antibodies continue to be detectable in the blood. The amount of virus in blood and lymphoid tissues falls to very low levels and the rate of HIV replication is slow although it does not cease. CD4 lymphocyte counts are within normal limits or generally above 350×106 cells/l. This phase may persist for 10 years or more. The role of antiretroviral therapy during asymptomatic infections is discussed in chapter 9. The decision to treat is made on the basis of the CD4 count and the viral load. The aim of therapy is to maintain immune function by suppressing viral replication to prevent further damage to the immune system. As for PHI treatment, the potential gain of therapy must be weighed against the potential risks and uncertainties.
Group III Persistent generalised lymphadenopathy
Persistent generalised lymphadenopathy may be a presenting feature of HIV infection in a person who is otherwise well. HIV related lymphadenopathy persists for at least three months, in at least two extra-inguinal sites and is not due to any other cause.
Common causes of generalised lymphadenopathy
| Condition | Test |
|---|---|
| Infections | |
| Bacterial | |
| Syphilis | Serological tests (Venereal Diseases Research Laboratory), Treponema pallidum haemagglutination and fluorescent antibody tests, brucellosis, serological tests |
| Viral | |
| Infectious mononucleosis | Paul-Bunnell |
| (Epstein-Barr virus) | |
| Cytomegalovirus | CMV cultures or antibodies |
| Hepatitis A | Serology |
| Hepatitis B | Serology |
| Rubella | Serology |
| Parasites | |
| Toxoplasmosis | Toxoplasma serology |
| Tumours | |
| Lymphomas | Full blood count, lymph node biopsy, CT or MRI scans etc |
| Leukaemias | |
| Others | |
| Miscellaneous | |
| Sarcoidosis | Clinical features, Kveim test |
Indications for lymph node biopsy
Constitutional symptoms
Painful nodes
Asymmetrical enlargement
Sudden increase in size
Hilar lymphadenopathy
A lymph node biopsy in HIV disease is not recommended as a routine procedure as the findings are non-specific and the presence of lymphadenopathy due to HIV alone does not worsen the prognosis. The indications for a biopsy are the same in HIV and non-HIV related conditions.
Constitutional symptoms in HIV infection
Weight loss >10% baseline
Fever lasting last least 1 month
Diarrhoea lasting at least 1 month
Group IV Symptomatic HIV infection before the development of AIDS
The progression of HIV infection is a result of a decline in immune competence that occurs due to increased replication of HIV from sites where it has been latent. The exact triggers for this reactivation are poorly understood. As the disease progresses, infected persons may suffer from constitutional symptoms, skin and mouth problems and haematological disorders, many of which are easy to treat or alleviate. A decrease in viral load in response to the introduction of antiretroviral therapy often corresponds to a complete or partial resolution of these symptoms.
Constitutional symptoms
Common constitutional symptoms associated with Group IVA HIV infection include malaise, fevers, night sweats, weight loss and diarrhoea. The exact criteria for diagnosing the AIDS defining HIV wasting syndrome are the combination of 10% weight loss from baseline and one of the other serious symptoms set out in the box. Many patients find these symptoms worrying and debilitating and they should be investigated to diagnose treatable causes other than HIV. Once other causes have been excluded, symptomatic treatment can include antipyretics, antidiarrhoeal agents and if all else fails, steroids.
Skin and mouth problems associated with HIV
Skin problems
| • Miscellaneous | • Bacterial |
| • Seborrhoeic dermatitis | Staphylococcal infection (impetigo) |
| • Fungal | Acneiform folliculitis |
| Tinea | • Viral |
| Cruris | Herpes simplex (types 1 and 2) |
| Pedis | Oral |
| Other | Genital |
| Candida | Perianal |
| Genital | Other |
| Perianal | Varicella zoster |
| Other | Human papillomavirus |
| • Pityriasis versicolor | Molluscum contagiosum |
| • Neoplastic | |
| Cervical dysplasia | |
Mouth problems
| • Hairy oral leucoplakia | • Ulceration |
| • Dental abscesses/caries | Bacterial |
| • Gingivitis | Herpetic |
| • Candidiasis | Aphthous |
Skin and mouth problems
Many skin problems occur in patients with HIV infection. These may represent exacerbations of previous skin disease, or a new problem. Identical skin conditions occur in HIV negative persons. However, in the immunocompromised, these common conditions may be more severe, persistent and difficult to treat. Many minor opportunistic infections (Group IVC2) manifest themselves on the skin and in the mouth. Seborrhoeic dermatitis is frequently seen and usually presents as a red scaly rash affecting the face, scalp and sometimes the whole body. This condition often responds well to 1% hydrocortisone and antifungal cream.
Other common dermatoses that respond to antifungal creams (eg, clotrimazole) include tinea cruris and pedis and candidiasis. Folliculitis often responds to 1% hydrocortisone and antifungal cream, impetigo to antibiotics and shingles to aciclovir, valaciclovir or famciclovir. Recurrent perianal or genital herpes may become more troublesome, with recurrences lasting longer and occurring more frequently; if this persists for more than 3 months it is considered an AIDS defining opportunistic infection (Group IVC1). Treatment with long term aciclovir, valaciclovir or famciclovir suppression is often required. Genital and perianal warts are common, difficult to treat and frequently recurrent, and high grade cervical dysplasia is seen more often in HIV infected women.
Mouth problems are also common, cause considerable distress and when severe may result in difficulty with eating and drinking. Oral candida can be managed with topical or systemic antifungals (eg nystatin, ketoconazole or fluconazole). If dysphagia develops, oesophageal candidiasis should be suspected and investigated. Oral hairy leucoplakia can be differentiated from oral candida by its characteristic distribution along the lateral borders of the tongue and the fact that it cannot be scraped off. Although unsightly, this condition which is due to Epstein-Barr virus reactivation is painless and temporary remission can be obtained with aciclovir, valaciclovir or famciclovir. Other oral conditions including dental abscesses, caries, gingivitis and oral ulceration (herpetic or bacterial) may occur. Mouth ulcers may be particularly difficult to treat and expert specialist assessment is recommended. Metronidazole, aciclovir, 0.2% chlorhexidine mouthwashes and analgesic sprays may all be effective depending on the cause and, in extreme cases, thalidomide has been used. Maintenance of good oral hygiene and dental care are important.
HIV and haematological problems
Lymphopenia with depression of the CD4 cell subset is a marker for HIV disease. Mild to moderate neutropenia and a normochromic, normocytic anaemia of unknown origin are often seen but usually have no adverse effect on HIV infected individuals. Severe anaemia or neutropenia should be investigated for other underlying causes. Thrombocytopenia is common in HIV disease and, only if persistent, causing bleeding and less than 20 × 109/l warrants treatment with antiretrovirals which is usually effective. Many therapies used to treat HIV may be toxic to bone marrow.
Risk of progression and the value of surrogate markers
One of the hardest problems confronting the physician dealing with an asymptomatic patient with HIV infection is predicting how soon that patient will progress to symptomatic disease or AIDS. This issue is important, first, in terms of counselling and secondly, to decide which patients may benefit from antiretroviral treatment or prophylaxis to prevent opportunistic infections.
Prognostic indicators in HIV infection
CD4 absolute lymphocyte count on percentage
At least two CD4 measurements needed before starting prophylaxis for opportunitic infectious antiretroviral therapy
the count can vary diurnally and seasonally
the count can be reduced by intercurrent infection
Viral load
At least two measures of viral load should be taken, using the same laboratory, to avoid interassay variation
Variables associated with rapid disease progression include a symptomatic PHI, older age at diagnosis and receiving a large inoculum of virus, for example via a contaminated transfusion from a donor with a high viral load. The effect of prophylaxis against opportunistic infections (eg, cotrimoxazole for pneumocystis and toxoplasmosis) has been to delay the onset of AIDS and to change the pattern of disease represented by the first AIDS defining illness. Antiretroviral treatment has independently been shown to increase survival before and after AIDS. Some infected individuals do not progress for many years and work is in progress to determine whether this is due to their genetic makeup, amount of viral inoculum, characteristics of the infective virus or their immune system.
Patients who may need close monitoring include individuals whose CD4 count falls below 350×106 cells/l, those with a rapidly declining CD4 count, those with a rising viral load and patients who are symptomatic as they may all be candidates for antiretroviral therapy. Patients who present with persistent constitutional symptoms, mouth or skin problems should be considered for antiretroviral therapy irrespective of CD4 count and viral load. These issues are discussed further in the chapters on treatment of infections and antiretroviral agents.
General management of HIV infected people
One of the most important aspects of dealing with any HIV infected person is confidentiality. Maintaining confidentiality might be complicated: for example the patient's family or friends may not know his or her diagnosis or sexual orientation; people at work (or school) may seek medical information (especially if the individual is having time off work); or the person may fear that information may inadvertently be given to third parties. Special precautions may be required, firstly to reassure the patient that confidentiality is protected and, secondly, to limit any unwarranted dissemination of confidential information.
General management of the HIV infected person
Protect confidentiality
Medical issues
Psychological support (patient, family and friends)
Avoidance of transmission
Other issues (dental treatment, insurance, work, or school, etc)
The routine medical management of these individuals is usually straightforward. They should be seen regularly, for example every three to six months. At each visit the patient's weight should be recorded and special attention given to mouth or skin problems and, if necessary, they should be referred to the appropriate specialist. Screening for STDs and hepatitis viruses should be offered if the individual is at risk and hepatitis A and B vaccines can be safely given. Repeating a full blood count and measuring the CD4 count and viral load every three to six months allows early detection of actual or imminent immune dysfunction. Patients should be advised to reattend if they develop any symptom, especially those suggestive of opportunistic infections or cancers, for example shortness of breath, cough, haemoptysis, pain or difficulty in swallowing, diarrhoea, weight loss, fevers, headaches, fitting, altered consciousness or purple spots on their skin. Other symptoms may indicate increased viral replication and the need to consider treatment.
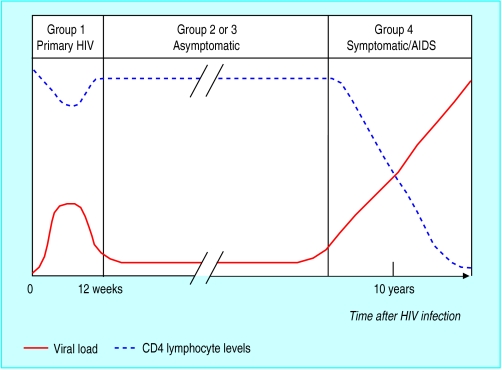
Figure.
Association between virological, immunological, and clinical events and time course of HIV infection
Figure.
Varicella zoster
Figure.
Hairy leucoplakia
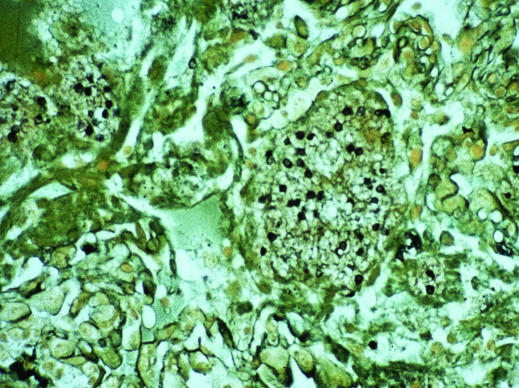
Figure.
WELLCOME LIBRARY
Pneumocystis carinii
Figure.
Oral candida