In many parts of the Western world there is a strong preference among gynaecologists to rely on surgical evacuation for the management of miscarriages in the first trimester. Why so many specialists have adopted surgery as the standard procedure seems determined by custom and habit and rooted in history rather than being an evidence based choice. During the first half of the 20th century the high rate of infections from retained products of conception with ensuing mortality from septicaemia—often complications from criminal attempts to terminate a pregnancy—resulted in the policy of immediate surgical evacuation whenever a diagnosis of inevitable abortion was made.1 Today these complications are rare, and their role in the justification of a universal tendency to perform surgery has therefore expired.2
Expectant management finds its main protagonists in general practice, where the process of spontaneous miscarriage is acknowledged more readily as being a well regulated natural process in human reproduction.
Relatively new is the medical approach to spontaneous miscarriages.3 The combination of the antiprogestogen mifepristone and the prostaglandin analogue misoprostol is being used successfully for the termination of pregnancies on a large scale. The use of these substances has also been tried in the management of spontaneous miscarriage.
Doctors and patients are confronted with a situation where opinions about the proper management of spontaneous miscarriage differ widely. That the available options are so diverse makes it even more complex. This paper aims to increase the awareness of various management options and explores the available evidence.
Summary points
Surgical evacuation is unnecessary after a complete miscarriage with retained products of conception and should be indicated by clinical rather than ultrasonographical criteria
Expectant management is used in general practice on a large scale and is more feasible than surgical evacuation
Medical management has no apparent benefits over expectant management, and it has side effects
Methods
We performed a search of Medline, Embase, the Cochrane Library, and PubMed to identify relevant literature, using spontaneous abortion and spontaneous miscarriage as primary search conditions for titles and abstracts. We carried out a crossover search from the obtained articles.
Studies from primary care
In 1989 the Dutch College of General Practitioners issued a practice guideline based on the expectant management of spontaneous miscarriage. A revised guideline, issued in 1997, confirmed expectant management as the strategy of first choice.4,5 Several observational studies from the United Kingdom, Canada, and the United States have also advocated expectant management by doctors as a feasible option.6–8 These studies showed that a major proportion of women with spontaneous miscarriages—a quarter in the United Kingdom and almost half in the North American studies—were managed successfully by doctors, either in the general practice or at home. Additionally, these studies showed that virtually all women under specialist care were bound to undergo surgical evacuation. Through an education programme focusing on both doctors and patients in Vancouver, British Columbia, surgical evacuations were reduced from 46% to 32%, and the incidence of complications even decreased during the study.9
These studies neither allow any conclusions about the differences between expectant and surgical management nor between the management in primary and secondary care, as it is likely that more serious cases were referred to hospital. They do, however, illustrate that expectant management is being practised widely in primary care, even in communities with a high rate of surgical intervention in the hospital environment.
Hospital based studies
Several hospital based randomised controlled trials comparing the various management options for spontaneous miscarriage are now available and provide more solid ground for management decisions. The table summarises the results of these trials.
Expectant management versus surgical evacuation
Nielsen and Hahlin published the first randomised study, which compared expectant management—during a period of three days—with surgical evacuation.10 They included women with inevitable and incomplete abortions with anterior-posterior diameters greater than 15 mm at ultrasonography. Success rates and complication rates were similar in both groups, as was the duration of vaginal bleeding, pain, sick leave, and packed cells volume after 3 and 14 days. Two more recent papers from this study showed no differences in psychological reactions and in subsequent fertility between both cohorts of women.11,12
Chipchase and James did a similar but smaller study among women with retained products of conception less than 50 mm on transvaginal ultrasonography after spontaneous miscarriages.13 They found no differences between expectant and surgical management in complication rates, duration of bleeding, pain, or sick leave.
Medical treatment versus surgical evacuation
De Jonge et al compared medical treatment (a single dose of the prostaglandin analogue misoprostol) with surgical evacuation.14 Women with inevitable miscarriages on clinical grounds were included. Several women were stabilised before randomisation: in each treatment arm about one third received blood transfusions. Medical treatment was considered successful if a complete miscarriage occurred within 12 hours. Only 3 of 23 patients (13%) were treated successfully with misoprostol compared with 26 of 27 patients (96%) allocated to surgery. Haemoglobin concentrations decreased significantly in women treated medically but were stable in those treated surgically. The study was discontinued after the present (interim) analysis. Patients entered in this study were apparently different from those in the other reports summarised in this paper. The fairly large uterine size (mean 13 weeks) and considerable proportion of women requiring blood transfusions before randomisation probably explain the high failure rate of medical treatment in this study.
Johnson et al compared medical treatment with surgical evacuation in women with miscarriages in the first trimester.15 Findings on ultrasonography were not specified, and included patients were a mixture of symptomatic women with non-vital pregnancies and incomplete or complete abortions. All patients were treated successfully in both treatment groups. In each group one major complication occurred: a laparotomy was done for a bleeding perforation after surgical evacuation, and a presumed ectopic pregnancy after medical treatment also resulted in a laparotomy, which did not confirm the diagnosis.
Hinshaw compared medical treatment with surgical evacuation in women with missed and incomplete abortions.16 An open study design was used: patients were either treated according to the randomised treatment allocation or according to their own preference. Pooled results were reported. Medical management comprised misoprostol in those with incomplete abortions, whereas those with missed abortions were treated with the antiprogestogen mifepristone, followed by misoprostol after a priming phase. In women with small uterine contents, no difference between medical treatment and surgery was found in the rate of complete evacuations. In those with larger uterine contents, the complete evacuation rate was significantly lower in medically treated women compared with those undergoing surgical evacuation. Overall, three haemorrhages greater than 500 ml occurred during medical treatment. In the surgically treated women three major complications also occurred: one perforation necessitating laparotomy with bowel resection and one cervical tear requiring suturing. The woman with the cervical tear developed sepsis and pelvic infection and was treated with high dose intravenous antibiotics. Chung et al compared medical management (misoprostol every four hours) with surgical evacuation in women with ultrasonographical evidence of retained products of conception greater than 5cm2 (transverse plane) or greater than 6cm2 (sagittal plane).17 Patients allocated misoprostol underwent a surgical evacuation the next day, whenever retained products of conception were still present (as was the case in 50% of patients). In the group allocated surgical removal, 2% required a second evacuation. There were significantly less short, medium, and long term complications in the women treated medically. Drug related gastrointestinal side effects occurred in up to 48% of these women.
Expectant management versus medical treatment
Nielsen et al were the first to explore the efficacy of expectant versus medical management in a randomised trial of women with spontaneous miscarriages in the first trimester.18 Women were either managed expectantly or received mifepristone followed by misoprostol 48 hours later. After five days, women with ultrasonographical evidence of retained products of conception greater than 15 mm underwent surgical evacuation. Success rates were similar in both groups, as were pain scores, vaginal bleeding, complications, and scores for patient satisfaction. Convalescence was 1.8 days longer after medical treatment.
Observational studies
Two observational hospital based studies are of special interest: a non-randomised study, performed by Cheung et al, provides detailed information about short term complications in a large series of patients.19 Women with complete abortions (n=297) were managed expectantly, whereas those showing retained products of conception on ultrasonography (n=470) were treated surgically. Treatment complications after surgery occurred in 6% of women: two cervical lacerations and four uterine perforations, for which two laparoscopies were done, whereas another patient needed an emergency hysterectomy for uncontrollable pelvic bleeding. Short term complications in those managed expectantly occurred in only 3% of women and were less severe, but the difference did not reach significance compared with those treated primarily by surgery.
In another observational study by Jurkovic et al, 221 asymptomatic women with a missed miscarriage diagnosed by ultrasonography were offered a choice between surgical evacuation or expectant management.20 Among 85 women (38%) opting for expectant management, 25% experienced a complete miscarriage whereas 17% needed surgical evacuation because of incomplete miscarriages. The remaining 59% requested surgical evacuation at some later stage, mostly for psychological reasons. The authors conclude that the success of expectant management is too low to justify its use in routine clinical practice.
Conclusion
Although miscarriage is the most common problem in pregnancy, the available evidence on its management is extremely limited. A considerable proportion of women with spontaneous miscarriages is being managed expectantly by doctors, even in communities where virtually all patients under secondary care are treated by surgical evacuation.
Surgical intervention in women with complete abortions is unnecessary and represents over treatment. Most studies in the table simply excluded these patients from further intervention. Even in women with ultrasonographical evidence of retained products of conception in the aftermath of a spontaneous miscarriage, immediate surgery is likely to be unnecessary in most cases, and medical treatment offers no advantages either. Arguably, clinical rather than ultrasonographical criteria should be used to indicate the necessity of surgical evacuation in these patients. In women with no history of passing any tissue, however, an empty uterine cavity on ultrasonography should raise suspicion of an ectopic pregnancy. In these women, measurements of serum human chorionic gonadotrophin concentrations together with repeated ultrasonography should lead the way in differentiating between a complete miscarriage and an ectopic pregnancy.21–23
In women still facing the process of spontaneous miscarriage there is strong evidence to suggest expectant management to be a realistic alternative to surgical evacuation, whereas medical treatment does not seem to offer any advantage. As mifepristone and misoprostol cause gastrointestinal side effects in up to 50% of patients and increase costs, these drugs probably deserve no place in the management of spontaneous miscarriage. Therefore, women with missed abortions or fetal death in the first trimester should be counselled accordingly and offered a choice between expectant and surgical management. This also seems true for women with evidence of non-vital pregnancies on ultrasonography before the onset of any clinical signs. Obviously, patients' preferences should play a key part in these management decisions, and more research is needed to elucidate the effect of these preferences on the acceptance of different treatment options. There seems, however, no point in denying a motivated well informed woman a fair chance to await the natural course of events whenever she prefers to do so. If surgical evacuation becomes necessary for medical or psychological reasons at some later stage, nothing is lost and at least then the reasons for surgical intervention are clear. Spontaneous miscarriage is a typical example of a condition where informed shared decision making should be put into practice thus replacing paternalism by partnership.24–26
Table.
Management of spontaneous miscarriage: randomised controlled trials
| Study | Type of patients | Retained products of conception* | Comparison (A v B) | Success of treatment (%)
|
P value | Complications (%) A v B | P value | |
|---|---|---|---|---|---|---|---|---|
| A | B | |||||||
| Nielsen and Hahlin10 | Inevitable and incomplete abortion | 15-50 mm | Expectant managment v surgery | 81/103 (79) | 52/52 (100) | >0.5 | 3 v 11 | >0.5 |
| Chipchase and James13 | Incomplete abortion | 5-25 mm | Expectant managment v surgery | 19/19 (100) | 16/16 (100) | >0.5 | 0.5 v 0.6 | >0.5 |
| De Jonge et al14 | Inevitable abortion | Uterine size <14 weeks | Medical treament v surgery | 3/23 (13) | 26/27 (96) | <0.05 | ? | — |
| Johnson et al15 | Missed and complete or incomplete abortion | ? | Medical treatment v surgery | 17/17 (100) | 12/12 (100) | >0.5 | 6 v 8 | >0.5 |
| Hinshaw16 | Missed and incomplete abortion | <24 mm and 24-77 mm | Medical treatment v surgery | 33/35 (94) and 54/64 (84) | 70/72 (98) and 96/97 (99) | >0.5 and <0.05 | 3 v 2 | >0.5 |
| Chung et al17 | Missed and incomplete abortion | >5 cm2 (transverse) or >6 cm2 (sagittal) | Medical treatment v surgery | 162/321 (50) | 308/314 (98) | <0.05 | 4 v 5 (short term) and 3 v 7 (medium and long term) | <0.05 and <0.05 |
| Nielsen et al18 | Missed and incomplete abortion | 15-50 mm | Expectant treatment v medical | 47/62 (76) | 49/60 (82) | >0.05 | 5 v 2 | >0.5 |
Determined by ultrasonography or other.
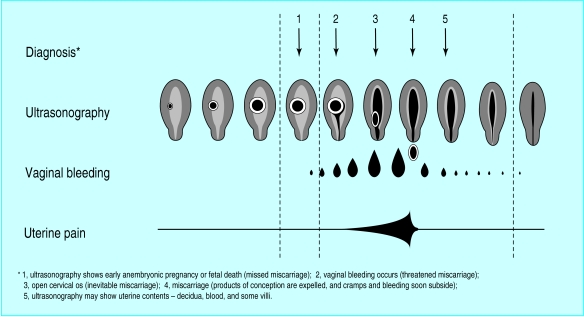
Figure.
Natural course of miscarriage, with opportunities for intervention
Figure.

Logo of the Miscarriage Association (www.miscarriageassociation.org.uk), an organisation offering support and information for women who have had a miscarriage
Editorial by Cahill
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Ballagh SA, Harris HA, Demasio K. Is curettage needed for uncomplicated incomplete spontaneous abortion? Am J Obstet Gynecol. 1998;179:1279–1282. doi: 10.1016/s0002-9378(98)70147-4. [DOI] [PubMed] [Google Scholar]
- 2.Report on confidential enquiries into maternal deaths in the United Kingdom 1994-1996. London: Stationery Office; 1998. Why mothers die. [DOI] [PubMed] [Google Scholar]
- 3.El-Refaey H, Hinshaw K, Hendhaw R, Smith N, Templeton A. Medical management of missed abortion and an embryonic pregnancy. BMJ. 1992;305:1399. doi: 10.1136/bmj.305.6866.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dutch Society of General Practitioners. Practice guideline (threatened) miscarriage [in Dutch] Huis Wetensch. 1989;32:138–143. [Google Scholar]
- 5.Flikweert S, Meijer LJ, De Haan M, Wiersma T. Dutch Society of General Practitioners. Practice guideline (threatened) miscarriage [in Dutch]. Huis Wetensch 1997.
- 6.Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315:32–34. doi: 10.1136/bmj.315.7099.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ambulatory Sentinel Practice Network. Spontaneous abortion in primary care. J Am Board Fam Pract. 1998;1:15–23. [PubMed] [Google Scholar]
- 8.Wiebe E, Janssen P. Management of spontaneous abortion in family practices and hospitals. Fam Med. 1998;30:293–296. [PubMed] [Google Scholar]
- 9.Wiebe E, Janssen P. Reducing surgery in management of spontaneous abortions. Family physicians can make a difference. Can Fam Physician. 1999;45:2364–2369. [PMC free article] [PubMed] [Google Scholar]
- 10.Nielsen S, Hahlin M. Expectant management of first-trimester spontaneous abortion. Lancet. 1995;345:84–86. doi: 10.1016/s0140-6736(95)90060-8. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen S, Hahlin M, Moller A, Granberg S. Bereavement, grieving and psychological morbidity after first trimester spontaneous abortion: comparing expectant management with surgical evacuation. Hum Reprod. 1996;11:1767–1770. doi: 10.1093/oxfordjournals.humrep.a019482. [DOI] [PubMed] [Google Scholar]
- 12.Blohm F, Hahlin M, Nielsen S, Milsom I. Fertility after a randomised trial of spontaneous abortion managed by surgical evacuation or expectant treatment. Lancet. 1997;349:995. doi: 10.1016/s0140-6736(97)24014-6. [DOI] [PubMed] [Google Scholar]
- 13.Chipchase J, James D. Randomised trial of expectant versus surgical management of spontaneous miscarriage. Br J Obstet Gynaecol. 1997;104:840–841. doi: 10.1111/j.1471-0528.1997.tb12030.x. [DOI] [PubMed] [Google Scholar]
- 14.De Jonge ETM, Makim JD, Manefeldt E, De Wet GH, Pattinson RC. Randomised clinical trial of medical evacuation and surgical curettage for incomplete miscarriage. BMJ. 1995;311:662. doi: 10.1136/bmj.311.7006.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson N, Priestnall M, Marsay T, Ballard P, Watters J. A randomised trial evaluating pain and bleeding after first trimester miscarriage treated surgically or medically. Eur J Obstet Gynecol Reprod Biol. 1997;72:213–215. doi: 10.1016/s0301-2115(96)02668-1. [DOI] [PubMed] [Google Scholar]
- 16.Hinshaw HKS. Medical management of miscarriage. In: Grudzinskas JG, O'Brien PMS, editors. Problems in early pregnancy. London: RCOG Press; 1997. pp. 284–295. [Google Scholar]
- 17.Chung TKH, Lee DTS, Cheung LP, Haines CJ, Chang AMZ. Spontaneous abortion: a randomized, controlled trial comparing surgical evacuation with conservative management using misoprostol. Fertil Steril. 1999;71:1054–1059. doi: 10.1016/s0015-0282(99)00128-4. [DOI] [PubMed] [Google Scholar]
- 18.Nielsen S, Hahlin M, Platz-Christensen J. Randomised trial comparing expectant with medical management for first trimester miscarriages. Br J Obstet Gynaecol. 1999;106:804–807. doi: 10.1111/j.1471-0528.1999.tb08401.x. [DOI] [PubMed] [Google Scholar]
- 19.Cheung LP, Sahota DS, Haines CJ, Chang AMZ. Spontaneous abortion: short term complications following either conservative or surgical management. Aust NZ J Obstet Gynaecol. 1998;38:61–64. doi: 10.1111/j.1479-828x.1998.tb02960.x. [DOI] [PubMed] [Google Scholar]
- 20.Jurkovic D, Ross JA, Nicolaides KH. Expectant management of missed miscarriage. Br J Obstet Gynaecol. 1998;105:670–671. doi: 10.1111/j.1471-0528.1998.tb10184.x. [DOI] [PubMed] [Google Scholar]
- 21.Ankum WM, Van der Veen F, Hamerlynck JVTH, Lammes FB. Transvaginal sonography and human chorionic gonadotrophin measurements in suspected ectopic pregnancy: a detailed analysis of a diagnostic approach. Hum Reprod. 1993;8:1307–1311. doi: 10.1093/oxfordjournals.humrep.a138247. [DOI] [PubMed] [Google Scholar]
- 22.Bannerjee S, Aslam N, Zosmer N, Woelfer B, Jurcovic D. The expectant management of women with early pregnancy of unknown location. Ultrasound Obstet Gynecol. 1999;14:231–236. doi: 10.1046/j.1469-0705.1999.14040231.x. [DOI] [PubMed] [Google Scholar]
- 23.Ankum WM. Diagnosing suspected ectopic pregnancy; HCG monitoring and transvaginal ultrasound lead the way. BMJ. 2000;321:1235–1236. doi: 10.1136/bmj.321.7271.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ. 1999;319:766–771. doi: 10.1136/bmj.319.7212.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ. 1999;319:780–782. doi: 10.1136/bmj.319.7212.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coulter A. Paternalism or partnership? BMJ. 1999;319:719–720. doi: 10.1136/bmj.319.7212.719. [DOI] [PMC free article] [PubMed] [Google Scholar]