In those who are severely immunosuppressed the treatment and prophylaxis of opportunistic infections remains important.
This article has been adapted from the forthcoming 5th edition of ABC of AIDS. The book will be available from the BMJ bookshop and at www.bmjbooks.com
Pneumocystis carinii pneumonia
Nowadays Pneumocystis carinii pneumonia most commonly occurs in those at risk of HIV infection who fail to take adequate prophylaxis or in those who are newly diagnosed with advanced disease, where it is frequently the presenting illness.
Clinical suspicion is aroused early in patients who are under regular medical supervision, leading to earlier diagnosis. Later diagnosis is asssociated with more severe disease and poorer treatment outcome. Techniques of diagnosis include sputum induction with nebulised saline; this obviates the need for bronchoscopy but the diagnostic sensitivity is lower. The use of lavage alone at bronchoscopy avoids transbronchial biopsy with its complications of haemorrhage and pneumothorax. Exercise oximetry and alternative imaging techniques with radiolabelled compounds are also being used in diagnosis. Monoclonal antibodies to pneumocystis proteins and sensitive DNA probes have been developed but have yet to reach the bedside. In the absence of a confirmatory test, a presumptive diagnosis may be made based on the clinical presentation and chest x ray appearances in a patient severely immunosuppressed and at risk.
Prophylaxis for Pneumocystis carinii pneumonia is essential after a first attack (secondary prophylaxis) but is also recommended for all patients once their CD4 cell counts falls below 200×106/l (primary prophylaxis). The risk of a first episode of infection below this CD4 count level in patients not on antiretroviral therapy is estimated to be 18% at 12 months for those who are asymptomatic, rising to 44% for those who have early symptomatic disease (eg oral candida, fever). Co-trimoxazole is the most effective agent. Although clinical trials have shown greater efficacy for co-trimoxazole compared to other regimens, there is a high rate of discontinuation due to side effects. Desensitisation regimens are used with the aim of reducing the rate of intolerance but there is uncertainty about their efficacy and which regimen is best.
Treatment of Pneumocystis carinii pneumonia
| Drug | Duration | Side effects | Comments |
|---|---|---|---|
| First choice | |||
| Co-trimoxazole (trimethoprim component 15-20 mg/kg per day PO/IV in divided doses) | 21 days | Nausea, vomiting, fever, rash, marrow suppression, raised transaminases | Intolerance common (25-50% of treated patients) |
| Alternative regimens | |||
| Severe disease | |||
| Pentamidine isethionate 4 mg/kg per day as slow intravenous infusion | 21 days | Hypotension, hyper- and hypoglycaemia, renal failure, marrow suppression, nausea, vomiting, cardiac arrest | 80% of patients will respond to treatment |
| Trimetrexate 45 mg/m2 IV and folinic acid 80 mg/m2 | 21 days | Marrow suppression, raised transaminases, rash, anaphylaxis | Should only be used as third or fourth line treatment |
| Mild to moderate disease | |||
| Clindamycin 600 mg 6 hourly PO/IV and primaquine 15 mg daily PO | 21 days | Diarrhoea, rash, nausea, vomiting, marrow suppression, methaemoglobinaemia, haemolysis | Clostridium difficile toxin associated diarrhoea is a frequent complication of clindamycin therapy |
| Trimethoprim 20 mg per kg/day PO/IV in 2-3 divided doses and dapsone 100 mg daily PO | 21 days | Rash, nausea, methaemoglobinaemia, marrow suppression | Alternative regimens should be used in patients with G6PD deficiency |
| Atovaquone suspension 750 mg twice daily | 21 days | Rash, raised transaminases, and neutropenia | Must be taken with food. Consider combination with IV pantamidine as resistance reported with monotherapy |
| Severe disease | |||
| Adjuvant high dose steroids (eg prednisolone 40-60 mg daily PO) | 5 days tapering over 14-21 days | Indicated in severe disease. Optimal dose not determined | |
PO=by mouth. IV=intravenously.
Toxoplasmosis
Cerebral toxoplasmosis is the commonest manifestation of toxoplasma infection. As toxoplasmosis is the most common cause of ring enhancing lesions on contrast CT brain scans a presumptive diagnosis is usually made and treatment started. The condition responds well if treatment is started early, and a combination of sulphadiazine and pyrimethamine is the treatment of choice. Side effects may prevent continued use of sulphadiazine, and clindamycin has been shown to be an effective alternative in controlled studies.
Corticosteroids are sometimes used in addition to first line treatment to reduce symptomatic cerebral oedema, but a clinical and radiological response seen after two weeks of treatment may be due solely to the corticosteroid effect rather than the antitoxoplasma treatment. A presumptive diagnosis of toxoplasma may therefore be made, although the underlying lesion may be due to something else, such as lymphoma or another infection. Relapse is common after treatment is stopped, and maintenance treatment is therefore necessary. In patients responding to antiretroviral therapy with sustained increases in CD4 count, discontinuation of prophylaxis is safe but there are limited current data to make definite recommendations.
Treatment of toxoplasmosis
First line
Sulphadiazine 4-6 g per day or clindamycin 600 mg × 4 per day
+
Pyrimethamine 50-100 mg per day
+
Folinic acid 15 mg per day
Alternatives
Clarithromycin 2 g per day or
Atovaquone 750 mg×4 per day PO+Pyrimethamine 50-100 mg per day PO.
Of patients with positive toxoplasma serology and a CD4 count of less than 100 × 106/l, approximately 1 in 3 will develop cerebral toxoplasmosis within 12 months without prophylaxis. Primary prophylaxis in patients with positive serology with a CD4 count of less than 200 × 106/l is therefore recommended. Co-trimoxazole or dapsone with pyrimethamine have been shown to reduce the incidence of toxoplasmosis compared to patients taking nebulised pentamidine for prophylaxis against Pneumocystis carinii pneumonia. Atovaquone with or without pyrimethamine may also be considered but this is based on more limited data. The macrolides clarithromycin and azithromycin might be anticipated to provide broad spectrum prophylaxis for toxoplasmosis, atypical mycobacterial and bacterial infections, but bacterial resistance might limit their use in this situation.
Patients with negative toxoplasma serology should be given advice how to avoid primary infection with toxoplasmosis. They should be advised not to eat raw or undercooked meat and avoid directly handling cats' faeces.
Cryptosporidiosis and other protozoa
In patients with less advanced HIV disease (CD4 counts >200 × 106/l) cryptosporidial infection usually causes a self limiting gastrointestinal illness and symptomatic treatment with antidiarroheal agents is all that may be needed. In those with more severe immunosuppression and persistent symptoms treatment is more difficult and reported successes with a variety of agents are still anecdotal. Symptoms and excretion of cysts may be intermittent. Responses have been described after treatment with a variety of agents, including spiramycin, erythromycin, diclazuril, letrazuril, hyperimmune bovine colostrum, paromamycin, azithromycin, and subcutaneous somatostatin.
Symptomatic treatment with antidiarroheal and antiemetic agents together with fluid, electrolyte, and nutritional support should be provided. Case reports suggest that immune reconstitution is likely to result in improvement and resolution of both symptoms and infection. Thus in the absence of an effective specific treatment against cryptosporidium, infected patients should be started on antiretroviral therapy to increase the CD4 count.
Patients at risk of infection should be advised to avoid possible exposure in water supplies particularly at times of documented outbreaks. Although unproven, measures that may be considered for patients with CD4 counts less than 200 × 106/l include using bottled water, point of use filters, or boiling water for more than one minute.
Diarrhoea often occurs in the absence of recognised pathogens in the stool, and metronidazole has relieved symptoms in some cases.
Viral infections
The treatment of opportunistic viral infections is summarised in the table. Prophylaxis is used after severe infection and in patients with increasing severity and frequency of recurrences. These recurrences can be a prelude to the chronic persistent mucocutaneous ulceration characteristic of AIDS.
Viral opportunistic infections
| Infection | Drug | Duration | Side effects | Comments |
|---|---|---|---|---|
| Herpes simplex | ||||
| Treatment | Acyclovir 200 mg 5 × a day orally or 10 mg/kg 8 hourly IV | 5-7 days | Duration may be extended in severe infections | |
| Prophylaxis | Acyclovir 200 mg 4 × a day or 400 mg 2 × day | Indefinite | ||
| Cytomegalovirus | ||||
| Treatment | Ganciclovir 5 mg/kg twice a day IV | 14-21 days | Neutropenia, anaemia | GCSF support may be required |
| Cidofovir 5 mg/kg IV once a week | 2 weeks | Nephrotoxicity: impaired creatine clearance, proteinuria, hypophosphataemia | Co-administer with probenecid and adequate hydration to reduce risk of nephrotoxicity | |
| Neutropenia | ||||
| Ocular toxicity | ||||
| Foscarnet 180 mg/kg daily | 14-21 days | Nephrotoxicity, hypomagnesaemia, hyper- and hypocalcaemia, hyper- and hypophosphataemia, hypokalaemia, nausea, vomiting, genital ulceration | Dose must be adjusted according to renal function | |
| Maintenance | Ganciclovir 3 mg daily orally | Until CD4 count > 100 × 106/l on HAART | As above | May be combined with intraoccular ganciclovir implants |
| Avoid in patients with diarrhoea | ||||
| Increases levels of didanosine | ||||
| Cidofovir 5 mg/kg once every 2 weeks | Until CD4 count > 100 × 106/l on HAART | As above | As above | |
| Alternative secondary prophylaxis regimens include daily intravenous foscarnet or ganciclovir, intravitreal injections of ganciclovir or foscarnet, and intraoccular ganciclovir implants | ||||
HAART=highly active antiretroviral therapy.
Fungal infections
Dermatophytic fungal infections respond well to imidazole creams. Oral candida is often asymptomatic in its early stages and may not require treatment. In more severe infections local treatment with frequent nystatin suspension, or pastilles, or amphotericin lozenges can be used. Systemic treatment with oral ketoconazole or fluconazole daily is required for more severe oropharyngeal and oesophageal candidiasis. Long term maintenance treatment may be required to prevent recurrences, and liver function tests should be monitored. Clinical resistance to treatment can occur and in the case of fluconazole may be related to emerging candida species that are less sensitive to fluconazole or to Candida albicans resistant strains. Intermittent therapy rather than maintenance may be a more appropriate strategy to reduce this risk but has yet to be assessed in a large controlled trial. Itraconazole solution has been found to be useful in cases of clinical resistance and this may be related to its topical action, better absorption, and greater spectrum of activity.
Vulvovaginal candidiasis can be a recurrent problem and should be treated either with topical agents (clotrimazole or miconazole pessaries and cream) or single high dose fluconazole.
Cryptococcal meningitis is treated with either fluconazole or amphotericin B with or without flucytosine. A large comparative study has shown that the overall mortality was similar in both treatment groups. However, there were more early deaths in the fluconazole group, and amphotericin sterilised the cerebrospinal fluid more rapidly but fluconazole was better tolerated. There was a 20% mortality and the factors predictive of death were an abnormal mental state, a cryptococcal antigen titre above 1024 and a white cell count below 0.02 × 109/l in the cerebrospinal fluid. Physicians will probably therefore prefer to treat patients with these poor prognostic markers with amphotericin rather than fluconazole. With a 20% mortality irrespective of what treatment is used it is clear that improvements in treatment are required.
Amphotericin B is still the mainstay of treatment of other systemic fungal infections. Itraconazole has shown to be effective in induction and maintenance treatment of disseminated histoplasmosis.
Fungal opportunistic infections
| Infection | Drug | Duration | Side effects | Comments |
|---|---|---|---|---|
| Candidiasis | ||||
| Local treatment | Nystatin oral suspension pastilles, miconazole oral gel, or amphotercin lozenges all 4-6 times a day | As required | Systemic therapy is commonly required | |
| Systemic treatment | Ketoconazole 200 mg a day (PO) | 1-2 weeks | Nausea (less if taken with food), abnormal liver function tests, hepatitis thrombocytopenia, rash | In patients who remain severely immunosuppressed, relapse is common and maintenance therapy is required |
| Fluconazole 50-200 mg a day (PO) | 1-2 weeks | Nausea, abnormal liver function tests | As above | |
| Itraconazole capsules or (PO) | 1-2 weeks | Nausea, abnormal liver function tests | ||
| Cryptococcosis | ||||
| Treatment | Amphotericin B 0.7-1.0 mg/kg/day (IV) ± flucytosine 75-100 mg/kg/day in 3-4 divided doses | Nausea, vomiting, rash, bone marrow suppression, renal impairment, hypocalcaemia | In patients who remain severely immunosuppressed, relapse is common and maintenance therapy is required | |
| Liposomal preparations of amphotericin reduce risk of nephrotoxicity | ||||
| or | ||||
| Fluconzaole 800 mg daily 1-3 days 600 mg daily thereafter (PO or IV) | As above | |||
Bacterial infections
Tuberculosis in HIV infection is treated in the standard way with isoniazid and rifampicin plus either pyrazinamide or ethambutol. Rifampicin is a potent enzyme inducer and increases the metabolism of drugs such as oral contraceptives, dapsone, fluconazole, ketoconazole, and anticonvulsants. Clinicans should also be aware of drug interactions between rifamycins (rifampicin and rifabutin) and antiretroviral drugs, particularly the protease inhibitors and the non-nucleoside reverse transcriptase inhibitors. Certain combinations of each are contraindicated or require dose adjustment to maintain therapeutic levels. Knowledge of these potential interactions is essential to avoid loss of clinical efficacy or increased risk of drug toxicity.
Although extrapulmonary disease is more common in HIV seropositive patients than in uninfected controls, the responses to treatment appear similar in the developed world if patients are compliant. Over the last few years there have been several outbreaks of tuberculosis with multiple drug resistance in the USA and Europe including the UK. Transmission of drug-resistant strains has occurred between patients and from patients to family members, healthcare workers, and prison guards. Mortality from drug resistant tuberculosis in this setting is high, around 70-90%. To reduce the risk of multiple drug resistant TB it is essential to ensure adherence to antituberculosis therapy by patients and for healthcare facilities to have in place procedures and facilities to reduce the risk of nosocomial transmission.
Disseminated infection with Mycobacterium avium complex causes considerable morbidity and mortality in the later stages of HIV infection (when CD4 counts are persistently below 50 × 106/l). Various combinations of drugs have been shown in uncontrolled studies to decrease mycobacteraemia and improve symptoms.
Treatment of Mycobacterium avium complex
Clarithromycin 1-2 g daily in divided doses
+
Ethambutol 15 mg/kg/day daily
+
Either Rifabutin 45-600 mg dailyRifampicin 45-600 mg dailyCiprofloxacin 500 mg twice dailyClofazimine 100 mg daily
3 or 4 drug regimens are recommended
Primary prophylaxis has been shown to significantly reduce the incidence of M avium complex bacteriaemia and should be considered in patients whose CD4 counts are less than 75 × 106/l. A variety of agents have been shown to be effective including rifabutin 300mg daily, clarithromycin 500 mg twice daily, or azithromycin 1200mg once weekly. Resistant strains can occur in those on clarithromycin and azithromycin prophylaxis who develop breakthrough bacteriaemia, and there is cross resistance. A combination of once weekly azithromycin and once daily rifabutin is probably the most effective prophylaxis regimen and may also provide additional prophylaxis against Pneumocystis carinii pneumonia.
Salmonella infections are treated with either co-trimoxazole or ciprofloxacin and campylobacter with ciprofloxacin. In salmonella infections relapses of enteritis or bacteraemia are common.
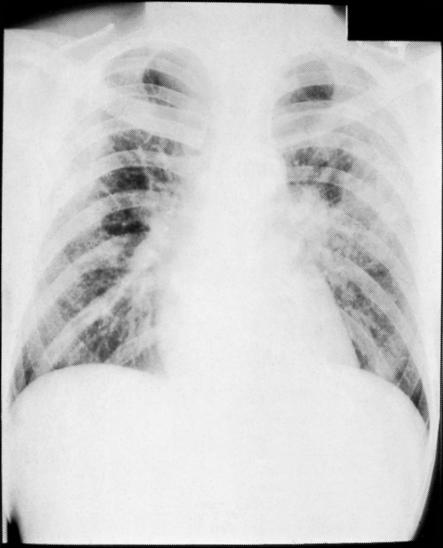
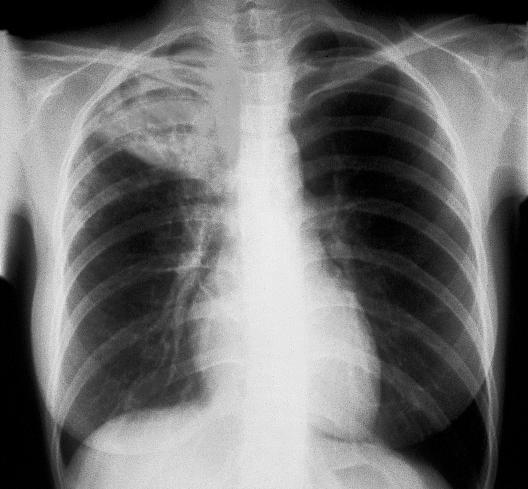
Figure.
Chest x ray appearance of Pneumocystis carinii pneumonia showing interstitial infiltrates
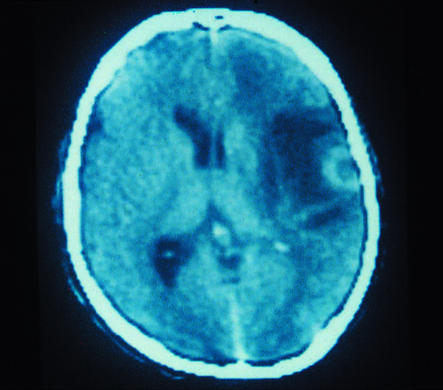
Figure.
CT scan showing ring enhancing lesions of cerebral toxoplasmosis surrounded by cerebral oedema (dark area)
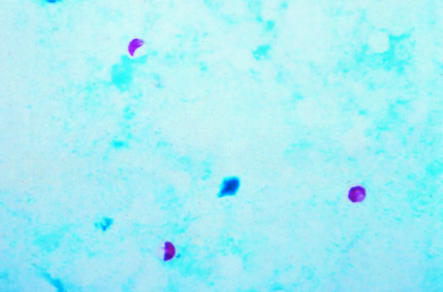
Figure.
Cryptosporidium
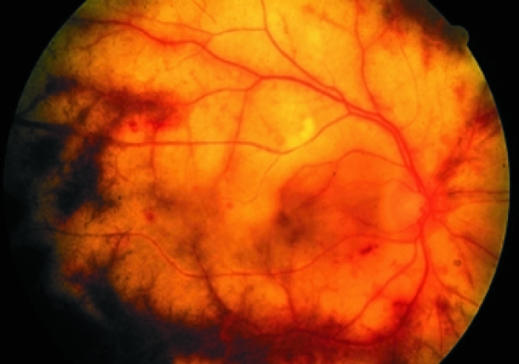
Figure.
Cytomegalovirus retinitis resulting from opportunistic infection of immunocompromised patient
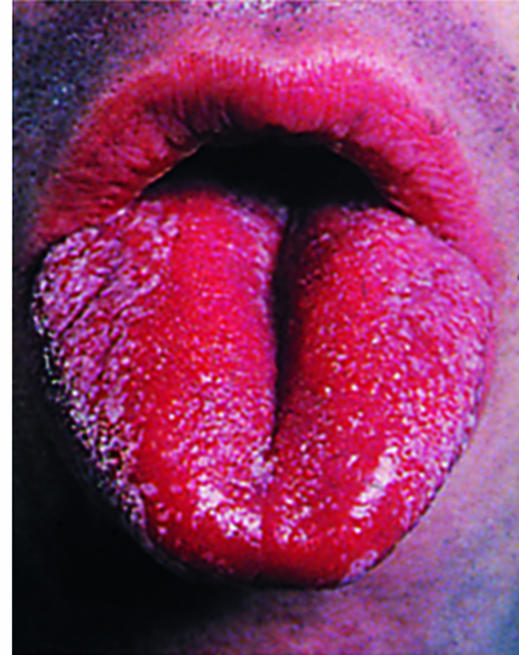
Figure.
Oral candidiasis
Figure.
SCOTT CAMAZINE/SPL
Chest x ray showing tuberculosis of the lung