Chlamydia trachomatis is the commonest curable sexually transmitted pathogen in the United Kingdom. Chlamydial infection is often asymptomatic and therefore underdiagnosed as there is no routine screening surveillance outside departments of genitourinary medicine. The true prevalence of chlamydial infection in the general population is currently unknown, but it is estimated to be as high as 10% in people under 20. Untreated carriers may present with complications of infection—salpingitis, possibly resulting in pelvic pain and tubal pregnancy or infertility in women and epidydimo-orchitis in men.1 Babies can acquire the infection at birth if their mother's cervix is infected2; this results in neonatal ophthalmia or pneumonitis, or both, and in nasopharyngeal and genital tract colonisation. The case we report raises the possibility that vertical transmission of vaginal chlamydial infection can remain asymptomatic for as long as six years.
Case report
A 6 year old girl was referred to an ophthalmologist because her eye was red and sticky and the condition had failed to respond to fucithalmic drops. The uniocular conjunctival injection, thickening, and follicle formation seen at examination suggested chlamydial infection. A swab from the eye was positive for C trachomatis by enzyme immunoassay testing (Syva Microtrak, Syva, CA) confirmed by direct immunofluorescence.3 The symptoms and signs resolved with topical tetracycline ointment.
The mode of transmission of infection was a source of concern. Three possibilities were considered: recent acquisition resulting from child sexual abuse, fomite contamination from another household member, and latent infection after vertical transmission.
The child's mother was seen at the genitourinary medicine clinic. She gave a clear history of recurring pelvic pain since age 16 and secondary infertility after the birth of the patient that had been cured by investigative tubal insufflation. Two months previously, she had been admitted to the surgical unit with abdominal pain and had undergone laparotomy, at which time bilateral pyosalpinges were noted. Her symptoms had settled with cephalosporin antimicrobial treatment. The only result related to chlamydial infection in the mother's hospital records was a negative endocervical enzyme immunoassay test undertaken in 1994.3 At the genitourinary medicine clinic the mother underwent full screening for sexually transmitted infection; all results were negative. The investigations included endocervical swabs for chlamydial testing by enzyme immunoassay, culture, and ligase chain reaction and urine for ligase chain reaction.
The mother's sexual partner for the past five years was also seen at the department of genitourinary medicine. He gave no history suggesting past or current chlamydial infection, and screening for sexually transmitted infection, including urine testing by ligase chain reaction, had negative results.
Because of the possibility of sexual abuse, the girl was examined at the child protection unit, but no physical stigmata of sexual abuse were noted. Vulval swabs were positive for C trachomatis by both ligase chain reaction and culture, and urine was positive for the organism by ligase chain reaction. At a subsequent formal interview by the child protection unit, the girl did not disclose anything to support the suspicion of abuse. Although her mother could not remember any early childhood problems with sticky eyes or recurrent chest infections, the general practitioner's records included two attendances for conjunctivitis when the girl was 4 months and 2 years old; on both occasions she was treated with chloromycetin ointment.
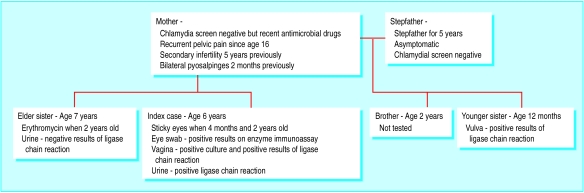
In view of the mother's medical history, the objective signs of tubal infection, and the lack of evidence to support sexual abuse as a mode of transmission, the possibility of vertical transmission was considered. It was felt appropriate to screen the patient's sisters, aged 7 years and aged 12 months, for chlamydial infection (see figure). A urine specimen from the elder sister was negative for chlamydia by ligase chain reaction, but a vulval swab from the younger sister was positive by ligase chain reaction. No other specimens were taken, and the vulval examination of the younger sister was normal. The records of the elder sister's general practitioner showed that when she was 2 years old she had had a course of erythromycin for a chest infection.
It was concluded that our patient's eye infection probably originated in autoinoculation from an asymptomatic genital tract infection and may have been acquired through vertical transmission at the time of birth or picked up later. All family members—including a 2 year old brother who was not screened—were treated systemically with single dose azithromycin at a dose appropriate for their age and weight.
Discussion
Chlamydial colonisation of the genital tract after vertical transmission was described first by Dunlop in 1966, and subsequently by other workers.2,4–6 It has been reported to persist for as long as three years. Chronic chlamydial eye infection, acquired at birth and persisting for many years, has also been described.7,8 In Mordhorst's series of 14 Danish patients with eye infections, one 9 year old girl was also found to have a vaginal chlamydial infection, but it is not clear whether sexual abuse had been excluded as a source of this genital tract infection.7
Although we could not prove that our patient's mother had a chlamydial infection, she had recently received antimicrobial treatment for directly visualised salpingitis and had a history of chronic pelvic pain and secondary infertility, all of which are recognised sequelae of chronic chlamydial infection.1 The results of chlamydial testing were negative in the elder sister. This could be because the mother acquired her infection between the births of this child and our patient, but is much more easily explained by the fact that the elder sister had had coincidental systemic antichlamydial treatment when she was 2 years old. The youngest sister too was found to have a chlamydial infection, also presumed to have been acquired as a result of vertical transmission.
The diagnosis would not have been made if the possibility of chlamydial infection had not been considered initially by the ophthalmologist and the appropriate swab taken for chlamydial testing. Dealing with a sexually transmitted infection in a non-genital site in a young child had to be dealt with sensitively and with considerable tact while maintaining openness about the possible routes of transmission so that the necessary investigations could be undertaken.
It was important to use as sensitive and specific a diagnostic test as possible for investigating this family. The availability of ligase chain reaction testing, with its enhanced sensitivity and suitability for testing urine specimens,9 was very helpful, particularly for the elder sister, who was very unwilling to have a genital examination and who might otherwise have required an anaesthetic so that adequate vaginal specimens could be obtained.
Prepubertal vaginal chlamydial infection is uncommon and has been associated with childhood sexual abuse.10 Any sexually transmitted infection in a child should alert the doctor to the possibilityof abuse. Appropriate measures should be taken to investigate that possibility, and all appropriate multidisciplinary workers should be involved. In our patient, the close cooperation of the general practitioner, social work department, and police enabled us to explore thoroughly the possibility of child sexual abuse, but there was no substantiating evidence.
We therefore conclude that the patient may have acquired her chlamydial infection at birth or picked it up later and that she developed a symptomatic ocular infection by activation of a latent ocular infection or by autoinoculation of the eye from her asymptomatic vaginal infection.
Figure.
Family cluster of Chlamydia trachomatis infection
Prepubertal chlamydial infection may indicate sexual abuse and requires sensitive multiagency management of the family
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Johnson AM, Grun L. Controlling genital chlamydial infection. BMJ. 1996;313:1160–1161. doi: 10.1136/bmj.313.7066.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schachter J, Grossman M, Sweet RL, Holt D, Jordan C, Bishop E. Prospective study of perinatal transmission of Chlamydia trachomatis. JAMA. 1986;255:3374–3377. [PubMed] [Google Scholar]
- 3.Thompson C, Jones R, Smith B, Brogan O, Smith IW, Carrington D. Evaluation of a microdot immunofluorescent antigen detection test for Chlamydia trachomatis. Gentiourinary Med. 1994;70:262–264. doi: 10.1136/sti.70.4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunlop EMC, Al-Hussaini MK, Freedman A, Garland JA, Harper IA, Jones BR. Infection by TRIC agent and other members of the Bedsonia group; with a note on Reiter's disease. III. Genital infection and disease of the eye. Trans Ophthal Soc UK. 1966;86:321–334. [PubMed] [Google Scholar]
- 5.Bell TA, Stamm WE, Wang SP, Kou CC, Holmes KK, Grayston JT. Chronic Chlamydia trachomatis infections in infants. JAMA. 1992;267:400–402. [PubMed] [Google Scholar]
- 6.Hammerschlag MR. Chlamydia trachomatis in children. Pediatr Ann. 1994;23:349–353. doi: 10.3928/0090-4481-19940701-08. [DOI] [PubMed] [Google Scholar]
- 7.Mordhorst CH, Wang SP, Grayston JT. Childhood trachoma in a nonendemic area. JAMA. 1978;239:1765–1771. doi: 10.1001/jama.239.17.1765. [DOI] [PubMed] [Google Scholar]
- 8.Stenberg K, Mardh P-A. Persistent neonatal chlamydial infection in a 6-year old girl. Lancet. 1986;ii:1278–1279. doi: 10.1016/s0140-6736(86)92702-9. [DOI] [PubMed] [Google Scholar]
- 9.Lee HH, Chernesky MA, Schachter J, Burczak JD, Andrews WW, Muldoon S. Diagnosis of Chlamydia trachomatis genitourinary infection in women by ligase chain reaction assay of urine. Lancet. 1995;345:213–216. doi: 10.1016/s0140-6736(95)90221-x. [DOI] [PubMed] [Google Scholar]
- 10.Ingram DL, Everett D, Lyna PR, White ST, Rockwell LA. Epidemiology of adult sexually transmitted disease agents in children being evaluated for sexual abuse. Pediatr Infect Dis J. 1992;11:945–950. doi: 10.1097/00006454-199211110-00008. [DOI] [PubMed] [Google Scholar]