Epidemiology of HIV-1 and HIV-2 infections in developing countries
The epidemiology and burden of HIV in the developing world are discussed earlier (see chapter 1). Two distinct viruses, HIV types 1 and 2 (HIV-1/HIV-2), cause AIDS. HIV-1 is responsible for the great majority of infections globally, HIV-2 being very rare outside of West Africa. Individual cases of HIV-2 infection have been described in other parts of Africa, Europe, the Americas, and Asia (India), but most people with HIV-2 infection have some epidemiological link to West Africa.
This article has been adapted from the forthcoming 5th edition of ABC of AIDS. The book will be available from the BMJ bookshop and at www.bmjbooks.com
The routes of transmission of HIV-1 and HIV-2 (as described in chapter 1) are the same worldwide, but the relative importance of different modes of transmission differs according to region. In most developing countries, heterosexual transmission is the dominant mode of spread, and mother to child transmission of HIV is much more common than in industrialised countries. Homosexual transmission is rare in Africa, but is more common in South East Asia and central and south America. Transmission associated with injecting drug use is particularly frequent in parts of south and South East Asia and central and south America. Acquisition of infection from contaminated blood remains a problem, especially in parts of sub-Saharan Africa and south Asia; in some countries commercial blood donation acts to amplify the spread of transfusion-transmitted HIV infection, both to the recipients of blood as well as to donors who may become infected through exposure to unsterile equipment. Women and children are at especially high risk for transfusion transmitted HIV infection, the former because of the high incidence of anaemia and haemorrhage associated with pregnancy and childbirth, and the latter because of malarial anaemia.
The transmission of HIV-2 infection is less efficient than that of HIV-1; this applies particularly to mother to child transmission, with only about 1% of HIV-2 infected mothers passing the infection on to their offspring. By comparison, up to 42% of HIV-1 infected mothers pass the infection to their children by all routes (intrauterine, puerperal, and breast milk). Sexual transmission of HIV-2 is also less efficient, especially before the development of end-stage immune deficiency. Postnatal transmission of HIV-1 by breast milk is more important than previously believed and approximately doubles the risk of mother to child transmission.
Clinical aspects of HIV disease in developing countries
As in industrialised countries, the spectrum of clinical manifestations associated with HIV infection is wide—ranging, as the CD4 count falls, from an asymptomatic state, through symptomatic disease, to fatal illness characterised by opportunistic infections, malignancies, neurological disease, and wasting. Initial acquisition of HIV infection (“acute HIV infection” or “seroconversion illness”) may be complicated by a syndrome resembling infectious mononucleosis, or a wide range of other manifestations, as described in chapter 4. However, since this syndrome is not specific, it is rarely recognised, even when clinically apparent.
Early manifestations of HIV disease
Common early symptoms and signs are weight loss, fever, night sweats, and diarrhoea. Skin disorders are frequent early manifestations, especially varicella zoster, fungal infections, and pruriginous dermatitis, an itchy rash consisting initially of papules, which become shallow ulcers due to scratching and finally heal leaving pigmented macules.
Tuberculosis
Tuberculosis is unquestionably the most important opportunistic infection complicating HIV infection in developing countries, and may present at any stage in the course of immunodeficiency. In early HIV disease, pulmonary tuberculosis is similar to that found in HIV-negative people. In advanced immunodeficiency, tuberculosis is often disseminated and multibacillary in nature. Nocardiosis, while much less common, is a differential diagnosis in some areas.
Bacterial septicaemia
An inadequately recognised manifestation of HIV disease in developing countries has been bacterial septicaemia. Gram negative organisms are the most common pathogens identified, especially non-typhoid Salmonella spp. Invasive pneumococcal disease is also frequent and may occur earlier than Gram negative infections. In some patients with advanced HIV disease, mycobacteraemia is detectable; this is much more frequently due to Mycobacterium tuberculosis than Mycobacterium avium intracellulare complex.
Diarrhoeal disease and HIV wasting syndrome
The best known clinical picture of AIDS in Africa is “slim”, the term given by people in rural Uganda to the HIV wasting syndrome. Profound wasting, chronic diarrhoea and fever are the typical features. About half the time no specific aetiology can be found for the diarrhoea: among identified causes, the most common are cryptosporidiosis, microsporidiosis, isosporiasis, and bacterial infections. The commonest autopsy finding in African patients with HIV wasting syndrome is disseminated tuberculosis, and undue emphasis may have been put on searching for a primary gastrointestinal cause of this whole syndrome. As with all medical causes of wasting, an important contributing factor to the HIV wasting syndrome is reduced food intake.
Neurological disease
Cerebral toxoplasmosis and cryptococcal meningitis are probably more frequent causes of severe HIV related disease in developing than industrialised countries, and their prevalence may vary by geographical region. Cerebral toxoplasmosis most often presents as a space occupying lesion of the brain, and cryptococcosis as a chronic meningitis.
Association with endemic tropical diseases
The association between endemic tropical diseases and HIV infection has only been studied to a limited degree. Theoretically, HIV infection could increase the incidence of tropical diseases, and alter their natural history, clinical expression, or response to treatment. Malaria is indirectly linked to HIV infection by causing anaemia in children, who may then be at risk of HIV infection transmitted through blood transfusion. HIV infected pregnant women experience greater frequency and severity of malarial parasitaemia, and increased frequency of placental malaria compared with HIV negative women. HIV infected people with Schistosoma mansoni excrete fewer eggs than those who are HIV negative, but it is not known whether the severity of schistosomiasis is affected by HIV infection, and response to treatment seems to be unaffected by HIV status. Amoebiasis and strongyloidiasis might be expected to be more frequent in HIV disease, but are not; on the basis of limited data, the same seems to be true of trypanosomiasis and leprosy. Little information is available concerning the influence of HIV infection on filariasis. Visceral leishmaniasis, often disseminated, appears to be increased in incidence in HIV infected people, although most reports have been from southern Europe rather than sub-Saharan Africa or South America. HIV infected people with leishmaniasis require maintenance treatment, as relapse is otherwise likely.
AIDS case definitions and staging of HIV disease
Case definitions of AIDS for epidemiological surveillance
For epidemiological surveillance, a practical case definition of severe HIV related disease is needed. The Centers for Disease Control (CDC) AIDS surveillance case definition is used in many industrialised countries, but cannot be used in most developing countries because it requires access to sophisticated laboratory investigations. For this reason, the World Health Organization (WHO) introduced a clinical case definition that could be used in settings where laboratory facilities are inaccessible. In 1994, this definition was expanded to incorporate HIV serology (thus increasing specificity) and to take account of revisions of the CDC case definition. If serological testing is unavailable or inaccessible, the clinical case definition should be used; if serological testing is available, the expanded case definition should be used.
WHO AIDS case definition for AIDS surveillance
For the purposes of AIDS surveillance an adult or adolescent (>12 years of age) is considered to have AIDS if at least two of the following major signs are present in combination with at least one of the minor signs listed below, and if these signs are not known to be due to a condition unrelated to HIV infection.
Major signs
Weight loss ⩾10% of body weight
Chronic diarrhoea for >1 month
Prolonged fever for >1 month (intermittent or constant)
Minor signs
Persistent cough for >1 month*
Generalised pruritic dermatitis
History of herpes zoster
Oropharyngeal candidiasis
Chronic progressive or disseminated herpes simplex infection
Generalised lymphadenopathy
The presence of either generalised Kaposi's sarcoma or cryptococcal meningitis is sufficient for the diagnosis of AIDS for surveillance purposes.
*For patients with tuberculosis, persistent cough for >1 month should not be considered as a minor sign.
Diagnosis and clinical staging of HIV disease in resource poor settings
Although advanced HIV disease may be easy to diagnose clinically, it is desirable to have HIV serology on patients with suspected HIV disease, particularly since HIV negative tuberculosis may be clinically indistinguishable from advanced HIV disease.
The case definitions in the boxes below were developed for epidemiological surveillance, and are not intended to be used for clinical staging of patients, for which they are neither sensitive nor specific. In order to estimate prognosis in individual patients, a clinical staging system is more useful than a case definition. The WHO's proposed staging system for HIV infection and disease, using clinical and laboratory data, can be used in developing countries. This system categorises patients into four stages based on clinical features of prognostic significance. The stages are interpreted as:
Stage 1: asymptomatic infection.
Stage 2: early (mild) disease.
Stage 3: intermediate (moderate) disease.
Stage 4: late (severe) disease.
The system can be refined using a laboratory axis: the CD4 count is the most useful laboratory marker for clinical staging, but is rarely available in developing countries. The total lymphocyte count can be used as a surrogate, although this is not ideal. Manifestations of HIV disease are rare at CD4 counts above 500 × 106 cells/l and severe illness and death are rare in patients with counts above 200 × 106/l. Tuberculosis and pneumococcal disease may occur at higher as well as lower CD4 counts. Once patients in developing countries have developed advanced HIV disease, they die with higher CD4 levels than in industrialised countries because of lack of access to high quality medical care; none the less, most patients die at the stage of advanced immunodeficiency.
Management of HIV infected people in developing countries
The general approach to treatment in developing countries should ideally be no different from that in the industrialised world, but is hampered by lack of infrastructure and resources for diagnosis and treatment. As for other diseases in resource poor countries, treatment must often be decided on the basis of very limited information. Patients should be counselled about HIV infection and prevention of its transmission.
Expanded WHO case definition for AIDS surveillance
For the purposes of AIDS surveillance an adult or adolescent (>12 years of age) is considered to have AIDS if a test for HIV antibody gives a positive result, and one or more of the following conditions are present:
⩾10% body weight loss or cachexia, with diarrhoea or fever, or both, intermittent or constant, for at least 1 month, not known to be due to a condition unrelated to HIV infection
Cryptococcal meningitis
Pulmonary or extrapulmonary tuberculosis
Kaposi's sarcoma
Neurological impairment that is sufficient to prevent independent daily activities, not known to be due to a condition unrelated to HIV infection (eg trauma or cerebrovascular accident)
Candidiasis of the oesophagus (which may be presumptively diagnosed based on the presence of oral candidiasis accompanied by dysphagia)
Clinically diagnosed life threatening or recurrent episodes of pneumonia, with or without aetiological confirmation
Invasive cervical cancer
Essential components of HIV/AIDS programmes
Prevention of new infections
Reduce sexual transmissionAwareness and life skills education, especially youthCondom promotionSTD control, including for commercial sex workersPartner notification
Blood safetyHIV testing of transfused bloodAvoid non-essential blood transfusionRecruitment of safe donor pool
Interventions to reduce transmission among injecting drug users (where necessary)
Reduce mother-child transmissionAntiretroviral therapyAvoidance of breast feeding (where safe): consider replacement feeding, or early weaning
Surveillance for HIV infections and AIDS
Voluntary counselling and testing
Mitigation of HIV related disease
Rational approach to care for HIV related disease, especially tuberculosis
Appropriate preventive therapies
Mitigating social impact
Minimising stigma: respect for confidentiality, protection against discrimination
Care for AIDS orphans
Antiretroviral therapy is currently available to only a very small minority of HIV infected people in developing countries. As antiretrovirals become less expensive, they will inevitably become more widely available and used. However, widespread implementation poses huge challenges in resource poor countries, including identifying HIV infected people before the stage of terminal disease; monitoring the response to therapy; continuity of drug supply; adherence, especially to complex regimens; and managing treatment failures. A priority will be to minimise the development of antiretroviral drug resistance by using rational and effective regimens, and maximising continuity of treatment and adherence. Resistance is probably inevitable unless triple drug regimens are used. Some populations will be easier to reach through existing infrastructures, such as occupational health schemes; tuberculosis programmes could also potentially be built upon if more resources were available.
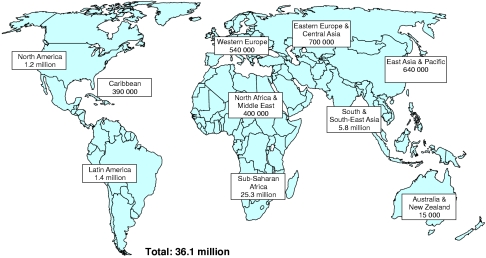
Figure.
Adults and children estimated to be living with HIV/AIDS at end of 2000. UNAIDS estimates that 95% of people living with HIV/AIDS are in developing countries
Figure.
A common clinical presentation of advanced HIV disease in African countries is marked wasting, known in Uganda as “slim” disease (courtesy of Professor Sebastian Lucas)
Figure.
Pruriginous dermatitis. This may be an early manifestation of HIV infection
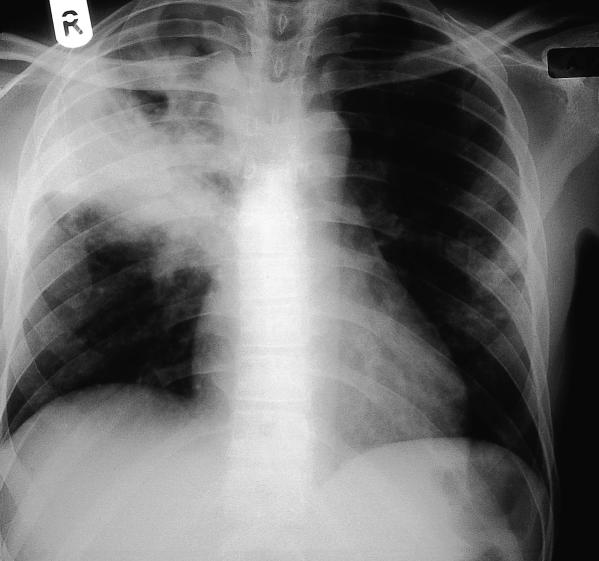
Figure.
Chest radiograph showing upper lobe cavitation typical of pulmonary tuberculosis. Appearances may also be atypical
Figure.
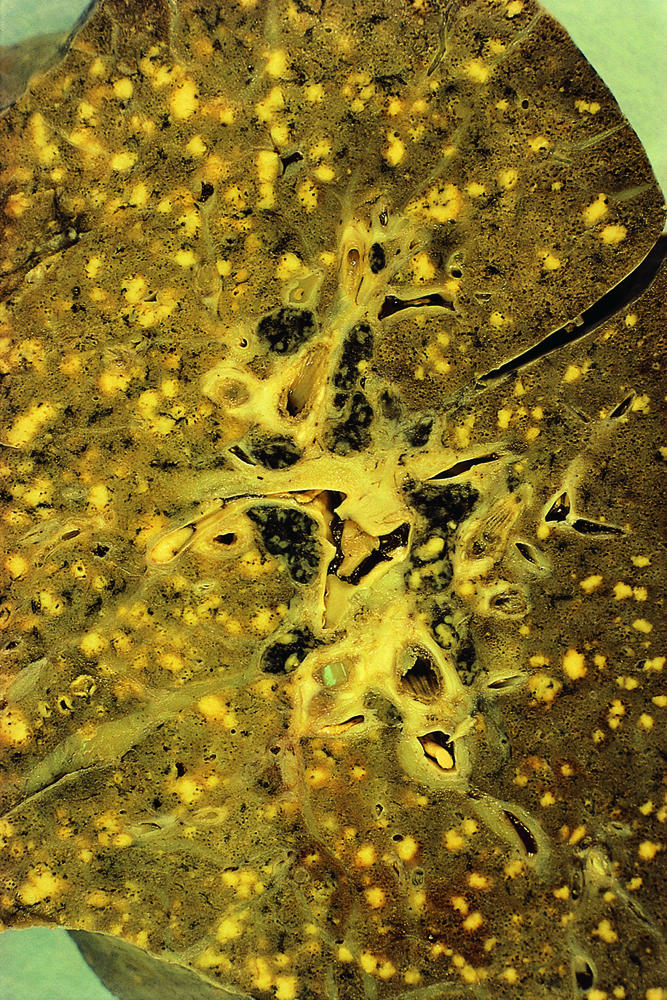
Postmortem section of lung showing miliarytuberculosis (courtesy of Professor Sebastian Lucas)
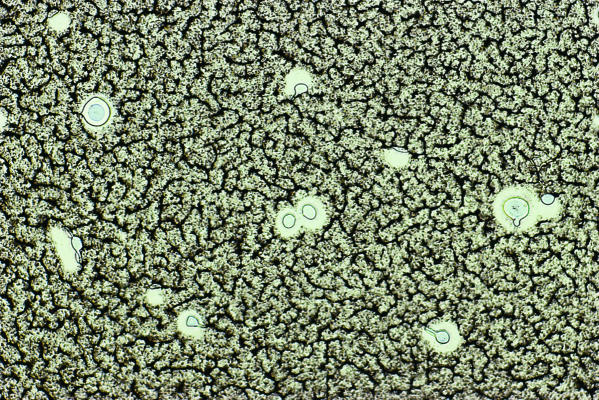
Figure.
Isospora belli, a treatable cause of diarrhoea in HIV infected people
Figure.
India ink stain of cerebrospinal fluid showing Cryptococcus neoformans, a common cause of meningitis (courtesy of Professor Sebastian Lucas)
Figure.
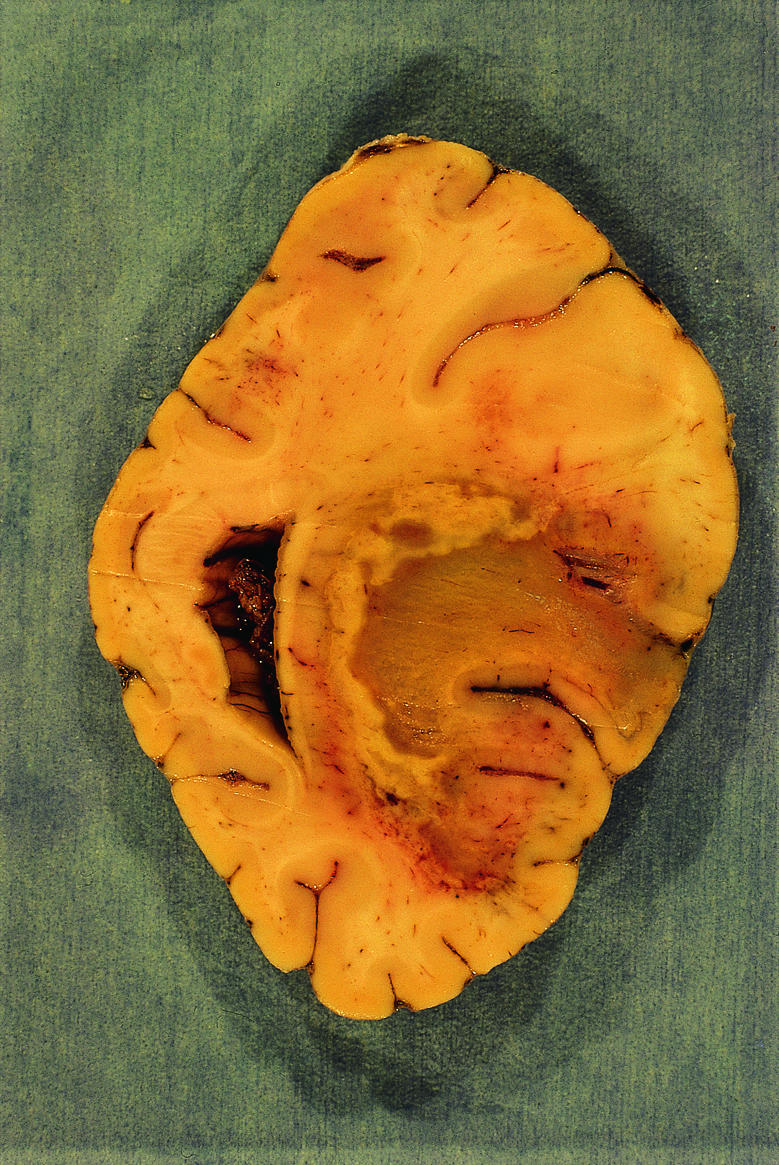
Cerebral toxoplasmosis: haemorrhagic andnecrotic mass in the occipital lobe (courtesy ofProfessor Sebastian Lucas)
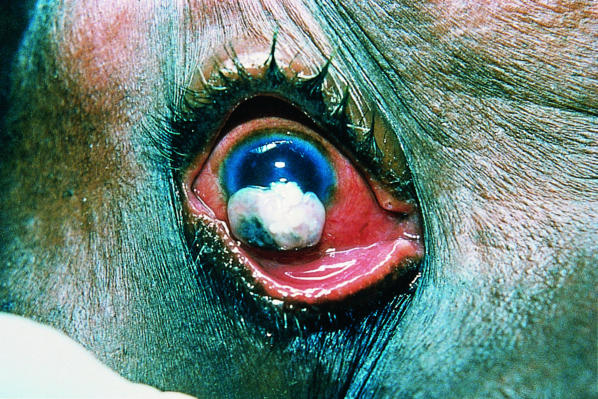
Figure.
Squamous cell carcinoma of the conjunctiva: an unusual cancer, strongly associated with HIV infection. Its incidence has increased markedly in Uganda and Rwanda (courtesy of Dr Keith Waddell)
Figure.

Kaposi's sarcoma: multiple skin nodules and plaques (courtesy of Dr A C Bayley)
Figure.

Kaposi's sarcoma: bilateral leg oedema and inguinal lymph node enlargement, without any evident skin lesions (courtesy of Dr A C Bayley)