Abstract
Background: Research on the impact of reduced time to emergent surgery in trauma patients has yielded inconsistent results. Therefore, this study investigated the relationship between waiting emergent surgery time (WEST) and outcomes in trauma patients. Methods: This retrospective, multicenter study used data from the Tzu Chi Hospital trauma database. The primary clinical outcomes were in-hospital mortality, intensive care unit (ICU) admission, and prolonged hospital length of stay (LOS) of ≥30 days. Results: A total of 15,164 patients were analyzed. The median WEST was 444 min, with an interquartile range (IQR) of 248–848 min for all patients. Patients who died in the hospital had a shorter median WEST than did those who survived (240 vs. 446 min, p < 0.001). Among the trauma patients with a WEST of <2 h, the median time was 79 min (IQR = 50–100 min). No significant difference in WEST was observed between the survival and mortality groups for patients with a WEST of <120 min (median WEST: 85 vs. 78 min, p < 0.001). Multivariable logistic regression analysis revealed that WEST was not associated with an increased risk of in-hospital mortality (adjusted odds ratio [aOR] = 1.05, 95% confidence interval [CI] = 0.17–6.35 for 30 min ≤ WEST < 60 min; aOR = 1.12, 95% CI = 0.22–5.70 for 60 min ≤ WEST < 90 min; and aOR = 0.60, 95% CI = 0.13–2.74 for WEST ≥ 90 min). Conclusions: Our findings do not support the “golden hour” concept because no association was identified between the time to definitive care and in-hospital mortality, ICU admission, and prolonged hospital stay of ≥30 days.
Keywords: golden hour, time to definitive care, mortality, trauma
1. Introduction
Traumatic injuries present a substantial global threat; they contribute considerably to global morbidity and mortality. Early definite care is crucial for high-risk trauma patients, with interventions for such patients including surgery [1,2,3,4,5,6]. According to the “golden hour” concept, the first hour following a traumatic injury is the most crucial [7].
The term “golden hour” is often attributed to R. Adams Cowley, the founder of Baltimore’s Shock Trauma Institute. In a 1975 article, Cowley asserted that “the first hour after injury will largely determine a critically injured person’s chances for survival”. The golden hour concept emphasizes that critically injured patients must receive definitive care within 60 min of sustaining injuries. During this crucial period, immediate medical attention can profoundly influence a patient’s prognosis. Swift and effective intervention within this timeframe often determines whether a patient will live or die or will experience full recovery or lasting disability. Prompt assessment, stabilization, and transport to appropriate medical facilities during this hour are essential to reduce complications and improve survival and recovery outcomes. Providing medical care within the golden hour is imperative because delays can lead to worsened outcomes and increased mortality rates. The golden hour concept was proposed in the 1970s; it has not been supported by empirical data or research but has gained widespread acceptance because of its clinical plausibility. Therefore, its validity remains unclear.
Trauma patients requiring emergent surgery may benefit from prompt surgical intervention, as suggested by the golden hour concept, with such intervention potentially improving their prognosis. However, research on the relationship between the waiting emergent surgery time (WEST) and trauma patient outcomes has produced inconsistent findings. Most studies investigating the impact of reduced surgical wait times have focused on patients with hip fracture, and they have obtained varying results. Additionally, research efforts have often been limited by small sample sizes or a primary emphasis on reducing time intervals rather than improving patient outcomes.
Gaining a comprehensive understanding of the golden hour concept is imperative. In Taiwan, level 1 trauma centers, which are accredited on the basis of their emergency capacity, have attending surgeons available 24/7 for all major trauma resuscitations. These centers also provide resuscitation interventions such as transcatheter arterial embolization or surgery, even on weekends and holidays [6,8]. Although studies have reported the optimal time to definitive care to be 2 h for procedures such as exploratory laparotomy and craniotomy at level 1 hospitals, in Taiwan, the time limit for emergent trauma surgeries is typically 30 min [9,10]. The current study investigated the relationship between the time to definitive care and trauma patient outcomes.
2. Methods
2.1. Study Design and Setting
This study was a retrospective cohort analysis of data from the Tzu Chi Hospital trauma registry, and the study protocol was approved by the Institutional Review Board of Taipei Tzu Chi Hospital (IRB number: 12-XD-077). The trauma database of Tzu Chi Hospital is a collaborative effort among four hospitals within the Tzu Chi Hospital system, with the hospitals located in Hualien, Taipei, Taichung, and Dalin. This database includes the data of patients admitted with trauma-related conditions identified by International Classification of Diseases, Ninth Revision, Clinical Modification codes 800–959 (excluding 905–909 and 930–939) or International Classification of Diseases, Tenth Revision, Clinical Modification codes S00–T98 (excluding T15–T19 and T90–T98) as well as those with major traumatic injuries. The database includes information regarding a comprehensive set of 152 variables associated with trauma, covering aspects such as demographics, injury mechanisms, injury types, injury severity, vital signs, surgical interventions, and in-hospital mortality. The current study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplementary Table S1) [11].
2.2. Participant Selection
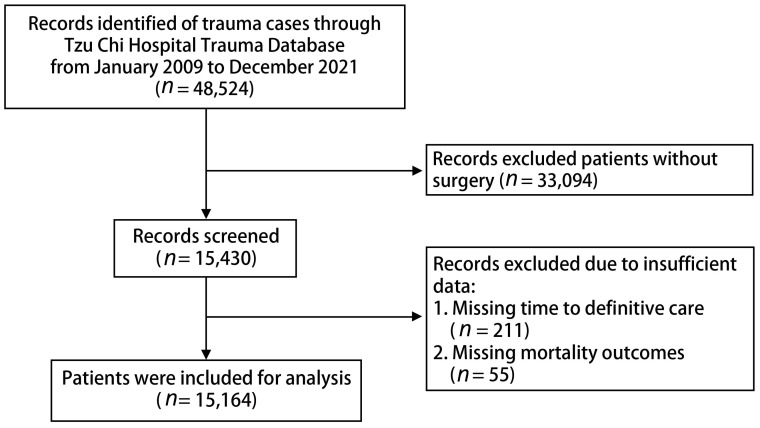
This study included patients listed on the Tzu Chi Hospital trauma database between January 2009 and December 2021. Initially, 48,524 patients were considered for analysis. However, patients who did not undergo surgery (n = 33,094), those without a recorded time to definitive care (n = 211), and those without data on mortality outcomes (n = 55) were excluded. Ultimately, 15,164 patients were included in the analysis. A detailed flow diagram of the participant selection process is presented in Figure 1.
Figure 1.
Flow diagram of participant selection.
2.3. Variable Measurements
The study analyzed the fundamental characteristics of the trauma cohort, including age, sex, pre-existing medical conditions, emergency triage classification, vital signs, injury etiology, and injury severity. Vital parameters, such as heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and respiratory rate (RR), were documented. Trauma severity was assessed using the injury severity score (ISS) and the revised trauma score (RTS). The ISS is used to evaluate the severity of multiple injuries, with scores from various body regions (head, chest, abdomen, extremities, and other areas) combined into a single value ranging from 0 to 75, with higher scores indicating more severe trauma [12]. The RTS is used to assess trauma severity on the basis of a patient’s physiological parameters, including SBP, RR, and level of consciousness [13]. These scoring systems are critical for the initial assessment and classification of trauma patients; they assist health-care providers in quickly assessing injury severity and developing appropriate treatment plans. Use of the ISS and RTS can help improve survival rates and patient outcomes as well as assist heal-care providers in effectively allocating emergency and medical resources. In the current study, patients with an ISS ≥ 16 or an RTS < 7 were defined as the major trauma population. The patients were categorized into two groups: those with traumatic brain injury (TBI, head Abbreviated Injury Score [AIS] ≥ 3) and those without TBI (head AIS score < 3). For the subgroup analysis, the geriatric population was defined as individuals aged ≥ 65 years. The mechanisms of injury included motor vehicle collision, low falls (falling from < 1 m), high falls (falling from ≥ 1 m), and others (such as drowning, burns, and cold injuries).
The primary variable in this study was each patient’s time to definitive care, defined as the time to surgical intervention for acute trauma injury. Time to emergent surgery was calculated as the interval from the patient’s arrival at the hospital to the start of surgical intervention. We categorized the WEST into 30 min intervals. Although emergency intervention is generally defined as that occurring within 1 h of injury, studies have indicated that the optimal time to definitive care for most emergent trauma interventions may extend up to 2 h, with this timeframe employed in some level 1 trauma centers [9,14]. To account for this, we conducted a sensitivity analysis focusing on patients who received emergent surgery within 2 h of injury.
2.4. Clinical Outcomes
We focused on three primary clinical outcomes: in-hospital mortality, admission to the intensive care unit (ICU), and extended hospitalization, defined as a length of stay (LOS) of ≥30 days. Additionally, we evaluated the frequency of ICU readmissions, the duration of ICU stays, extended ICU LOS (specified as an ICU stay exceeding 14 days), and the total duration of hospitalization for each patient.
2.5. Statistical Analysis
We conducted a comprehensive statistical analysis of all demographic information, injury details, and clinical outcomes by using SPSS software (version 20.0, SPSS, Chicago, IL, USA). The distribution patterns of continuous data were assessed using the Kolmogorov–Smirnov test. Continuous variables are presented as medians with interquartile ranges (IQRs), and categorical variables are presented as counts and percentages. Continuous data were analyzed using either nonparametric analysis of variance or the Mann–Whitney U test. Categorical and nominal data were evaluated using Pearson’s chi-square test or Fisher’s exact test. The relationship between the scoring systems and the three major trauma patient outcomes was determined using multivariable logistic regression. The factors considered in the regression analysis were variables with a p value < 0.10 in the chi-square or Mann–Whitney U tests or those of clinical significance, such as age, sex, injury type, and injury mechanism, by using a forced entry method. Sensitivity analyses were conducted to evaluate the associations across different groups, including categories of injury severity (minor injury: ISS < 16 or RTS ≥ 7 and major injury: ISS ≥ 16 or RTS < 7), age groups (nongeriatric: age < 65 years and geriatric: age ≥ 65 years), WEST durations (WEST < 30 min, 30 min ≤ WEST < 60 min, 60 min ≤ WEST < 90 min, and WEST ≥ 90 min), and major injury sites (head AIS ≥ 3, chest AIS ≥ 3, and abdominal AIS ≥ 3). All tests were two-sided, with significance set at p < 0.05.
3. Results
3.1. Characteristics of Study Participants
The in-hospital mortality rate, ICU admission rate, and rate of prolonged hospital LOS of ≥30 days were 1.0%, 12.0%, and 4.5%, respectively. Table 1 presents the demographic characteristics of all patients. The geriatric population (age ≥ 65 years) accounted for 41.4% and 63.4% of the mortality group. Patients in the in-hospital mortality group had higher triage levels, with 49.7% classified as triage level I. Penetrative injuries were present in only 5.3% of all patients. Cardiovascular disease was the most common chronic condition, accounting for 27.6% of the conditions, followed by diabetes (15.9%). Major injuries (ISS ≥ 16) were present in 7.4% of all patients and 67.6% of the in-hospital mortality group. Low falls were the most common injury mechanism, accounting for 39.9% of the injuries, followed by road traffic injuries, at 37.7%. TBI occurred in 6.7% of all patients and in 58.6% of the in-hospital mortality group.
Table 1.
Comparison of demographic characteristics of included patients.
| Characteristics | Total Patients | Survival | Mortality | p-Value |
|---|---|---|---|---|
| Patient number | 15,164 (100%) | 15,019 (99%) | 145 (1%) | |
| Age (years) | <0.001 | |||
| Age < 65 years old | 8890 (58.6%) | 8837 (58.8%) | 53 (36.6%) | |
| Age ≥ 65 years old | 6272 (41.4%) | 6180 (41.2%) | 92 (63.4%) | |
| Sex, n (%) | <0.001 | |||
| Female | 7520 (49.6%) | 7479 (49.8%) | 41 (28.3%) | |
| Male | 7644 (50.4%) | 7540 (50.2%) | 104 (71.7%) | |
| Vital sign | ||||
| SBP | 142 (124–161) | 142 (124–161) | 146 (109.5–174) | 0.864 |
| DBP | 83 (73–94) | 83 (73–94) | 84 (66–99) | 0.332 |
| RR | 18 (16–20) | 18 (16–20) | 18 (16–20) | 0.094 |
| HR | 84 (73–96) | 84 (73–96) | 89 (74–101) | 0.023 |
| Triage | <0.001 | |||
| 1 | 667 (4.4%) | 595 (4.0%) | 72 (49.7%) | |
| 2 | 5908 (39.0%) | 5866 (39.1%) | 42 (29.0%) | |
| 3 | 8444 (55.8%) | 8413 (56.1%) | 31 (21.4%) | |
| 4 and 5 | 125 (0.8%) | 125 (0.8%) | 0 (0.0%) | |
| Injury severity | ||||
| RTS | 7.84 (7.84–7.84) | 7.84 (7.84–7.84) | 6.90 (5.00–7.84) | <0.001 |
| RTS < 7 | 668 (4.4%) | 594 (4.0%) | 74 (51.4%) | <0.001 |
| ISS | 9 (4–9) | 9 (4–9) | 25 (9–29) | <0.001 |
| ISS ≥ 16 | 1125 (7.4%) | 1027 (6.8%) | 98 (67.6%) | <0.001 |
| Trauma team activation | 495 (3.3%) | 444 (3.0%) | 51 (35.2%) | <0.001 |
| Time for surgery | 444 (248–848) | 446 (251–850) | 240 (116.5–473) | <0.001 |
| Traumatic brain injury | <0.001 | |||
| Non-TBI | 14,151 (93.3%) | 14,091 (93.8%) | 60 (41.4%) | |
| TBI | 1013 (6.7%) | 928 (6.2%) | 85 (58.6%) | |
| Injury type | 0.080 | |||
| Penetrating injury | 807 (5.3%) | 804 (5.4%) | 3 (2.1%) | |
| Non-penetrating injury | 14,357 (94.7%) | 14,215 (94.6%) | 142 (97.9%) | |
| Mechanism of injury | 0.002 | |||
| Traffic road injury | 5112 (37.7%) | 5045 (37.6%) | 67 (51.5%) | |
| High fall | 1370 (10.1%) | 1353 (10.1%) | 17 (13.1%) | |
| Low fall | 5403 (39.9%) | 5362 (39.9%) | 41 (31.5%) | |
| Others | 3279 (21.6%) | 3259 (21.7%) | 20 (13.8%) | |
| Comorbidity | ||||
| CNS diseases | 672 (4.4%) | 66 (4.4%) | 6 (4.1%) | 0.863 |
| CVD | 3965 (26.1%) | 3925 (26.1%) | 40 (27.6%) | 0.692 |
| CKD | 351 (2.3%) | 339 (2.3%) | 12 (8.3%) | 0.003 |
| Diabetes mellitus | 1676 (11.1%) | 1653 (11.0%) | 23 (15.9%) | 0.250 |
| Hospitalization | ||||
| Total LOS days | 7 (4–10) | 7 (4–10) | 10 (4–22.5) | <0.001 |
| Total LOS ≥ 30 days | 687 (4.5%) | 661 (4.4%) | 26 (17.9%) | <0.001 |
| ICU admission | 1818 (12.0%) | 1695 (11.3%) | 123 (84.8%) | 0.040 |
| ICU LOS, days | 5 (3–11) | 5 (3–11) | 6 (3–19) | <0.001 |
| ICU LOS ≥ 14 days | 369 (22.0%) | 328 (21.1%) | 41 (33.3%) | 0.002 |
| In-hospital mortality | 145 | --- | 145 | ---- |
| Death within 24 h | 10 (6.9%) | ---- | 10 (6.9%) | ---- |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; RR, respiratory rate; HR, heart rate; CNS diseases, central nervous system diseases; CKD, chronic kidney disease; CVD, cardiovascular disease; ISS, injury severity score; RTS, revised trauma score; TBI, traumatic brain injury; LOS, length of stay; ICU, intensive care unit. The continuous variables are presented as median and interquartile range (IQR).
3.2. Time to Emergent Surgery in Subgroups
Table 2 presents the results of comparisons of the WEST among all patients across various subgroups. The median WEST for all patients was 444 min, with an IQR of 248–848 min. Patients who died in hospital had a notably shorter WEST than survivors did (median WEST: 240 vs. 446 min, p < 0.001). After stratification by other patient characteristics, a significantly shorter WEST was observed among patients younger than 65 years (median WEST: 419 vs. 478 min, p < 0.001), those with major injuries to the abdomen (median WEST in patients with abdominal AIS ≥ 3 vs. head AIS ≥ 3 vs. chest AIS ≥ 3: 353 vs. 413 vs. 492 min, p < 0.001), those with major injuries (ISS ≥ 16 or RTS < 7; median WEST in patients with RTS < 7 vs. RTS ≥ 7 and ISS ≥ 16 vs. ISS < 16: 301 vs. 450 min and 397 vs. 447 min, respectively, p < 0.001), and those with a hospital stay exceeding 30 days (median WEST: 446 vs. 406 min, p < 0.001).
Table 2.
Comparison of waiting emergent surgery times (WESTs) among all patients across various subgroups.
| Subgroup | Median (IQR) | p-Value |
|---|---|---|
| WEST per 30 min | ||
| WEST < 30 min | 16 (9–23) | <0.001 |
| 30 ≤ WEST < 60 min | 48 (38–55) | |
| 60 ≤ WEST < 90 min | 76 (70–84) | |
| WEST ≥ 90 min | 468 (275–873) | |
| Age | ||
| Age < 65 years old | 419 (231–802) | <0.001 |
| Age ≥ 65 years old | 478 (276–905) | |
| RTS | ||
| RTS < 7 | 301 (136–760) | <0.001 |
| RTS ≥ 7 | 450 (255–849) | |
| ISS | ||
| ISS < 16 | 447 (256–840) | <0.001 |
| ISS ≥ 16 | 397 (155–948) | |
| Major injury site | ||
| Head AIS ≥ 3 | 413 (157–956) | <0.001 |
| Chest AIS ≥ 3 | 492 (197–1077) | |
| Abdominal AIS ≥ 3 | 353 (156–946) | |
| Hospitalization | ||
| Total LOS < 30 days | 446 (252–847) | <0.001 |
| Total LOS ≥ 30 days | 406 (182–881) | |
| ICU admission | ||
| Yes | 432 (189–982) | 0.273 |
| No | 445 (256–830) | |
| In-hospital mortality | ||
| Yes | 240 (116–473) | <0.001 |
| No | 446 (251–850) |
Abbreviations: WEST, waiting emergent surgery time; SBP, systolic blood pressure; DBP, diastolic blood pressure; RR, respiratory rate; HR, heart rate; ISS, injury severity score; AIS, abbreviated injury scale; RTS, revised trauma score; TBI, traumatic brain injury; LOS, length of stay; ICU, intensive care unit.
3.3. Trauma Patients with WEST Less than 2 h
According to previous studies, many level 1 trauma centers have implemented the optimal time interval of 2 h for emergent trauma interventions [9,14]. Table 3 presents the results of sensitivity analyses for trauma patients who received emergent surgery within 2 h. Among the trauma patients with a WEST of <2 h, the median time was 79 min, with an IQR of 50–100 min. No significant difference in WEST was noted between the survival and mortality groups of patients with a WEST of <120 min (median WEST: 85 vs. 78 min, p < 0.001). The patients aged ≥ 65 years (median WEST: 81 vs. 72 min, p < 0.001), those with minor injuries (ISS < 16 or RTS ≥ 7; median WEST in patients with RTS ≥ 7 vs. RTS < 7 and ISS < 16 vs. ISS ≥ 16: 76 vs. 56 min and 88 vs. 76 min, respectively, p < 0.001), those with major injuries to the chest (median WEST in patients with chest AIS ≥ 3 vs. head AIS ≥ 3 vs. abdominal AIS ≥ 3: 77 vs. 91 vs. 81 min, p < 0.001), and those without ICU admission (median WEST: 76 vs. 87 min, p < 0.001) had a shorter WEST.
Table 3.
Comparison of waiting emergent surgery time (WEST) among trauma patients receiving emergent surgery within 2 h across various subgroups.
| Subgroup | Median (IQR) | p-Value |
|---|---|---|
| Age | ||
| Age < 65 years old | 81 (56–99.75) | <0.001 |
| Age ≥ 65 years old | 72 (40–99) | |
| RTS | ||
| RTS < 7 | 89 (70.5–102) | <0.001 |
| RTS ≥ 7 | 76 (48–99) | |
| ISS | ||
| ISS < 16 | 76 (47–99) | <0.001 |
| ISS ≥ 16 | 88 (64–103) | |
| Major injury site | ||
| Head AIS ≥ 3 | 91 (72–105) | <0.001 |
| Chest AIS ≥ 3 | 77 (53–93) | |
| Abdominal AIS ≥ 3 | 81 (60.5–96) | |
| Hospitalization | ||
| Total LOS < 30 days | 78 (49–99) | 0.174 |
| Total LOS ≥ 30 days | 87 (60–99) | |
| ICU admission | ||
| Yes | 87 (58.75–100) | <0.001 |
| No | 76 (48–99) | |
| In-hospital mortality | ||
| Yes | 85 (62–98) | 0.463 |
| No | 78 (50–99) |
Abbreviations: WEST, waiting emergent surgery time; SBP, systolic blood pressure; DBP, diastolic blood pressure; RR, respiratory rate; HR, heart rate; ISS, injury severity score; AIS, abbreviated injury scale; RTS, revised trauma score; TBI, traumatic brain injury; LOS, length of stay; ICU, intensive care unit.
3.4. Association between WEST and Clinical Outcomes
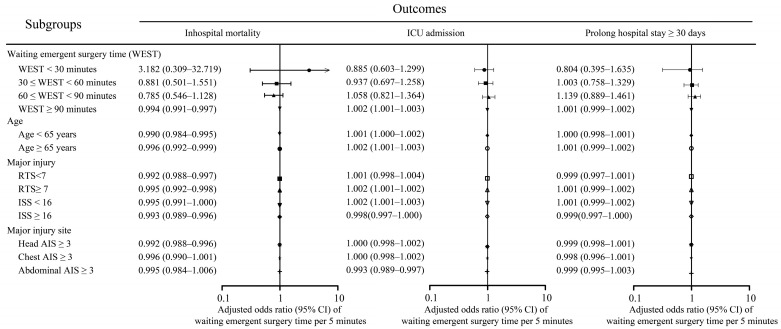
The results of the multivariable logistic regression in Table 4, which included all patient data, revealed several variables to be significantly associated with increased odds of mortality. These variables included age ≥ 65 years (adjusted odds ratio [aOR] = 3.62), male sex (aOR = 2.12), RTS < 7 (aOR = 5.15), and ISS ≥ 16 (aOR = 8.29). Notably, WEST was not correlated with an elevated risk of in-hospital mortality. Additionally, no significant association was noted between WEST and ICU admission or prolonged hospital stay of ≥30 days. The results of the subgroup analysis (Figure 2) indicated that a longer WEST was associated with a reduced risk of in-hospital mortality in patients with WEST ≥ 90 min (aOR = 0.994, 95% confidence interval [CI] = 0.991–0.997) in those aged < 65 years (aOR = 0.990, 95% CI = 0.984–0.995) and ≥65 years (aOR = 0.996, 95% CI = 0.992–0.999), as well as in those with minor injuries (RTS ≥ 7: aOR = 0.995, 95% CI = 0.992–0.998; ISS < 16: aOR = 0.995, 95% CI = 0.991–1.000) or major injuries (RTS < 7: aOR = 0.992, 95% CI = 0.988–0.997; ISS ≥ 16: aOR = 0.993, 95% CI = 0.989–0.996), and those with head AIS ≥ 3 (aOR = 0.992, 95% CI = 0.988–0.996).
Table 4.
Results of multivariable logistic regression analysis of in-hospital mortality, ICU admission, and prolonged hospital stay (≥30 days).
| Variables | In-Hospital Mortality | ICU Admission | Prolonged Hospital Stay ≥ 30 Days | |||
|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) |
p-Value | Adjusted OR (95% CI) |
p-Value | Adjusted OR (95% CI) |
p-Value | |
| WEST per 30 min | ||||||
| WEST < 30 min | Reference | --- | Reference | --- | Reference | --- |
| 30 ≤ WEST< 60 min | 1.05 (0.17–6.35) | 0.955 | 0.85 (0.41–1.80) | 0.678 | 2.93 (0.92–9.33) | 0.068 |
| 60 ≤ WEST< 90 min | 1.12 (0.22–5.70) | 0.890 | 0.62 (0.30–1.28) | 0.199 | 1.80 (0.58–5.53) | 0.307 |
| WEST ≥ 90 min | 0.60 (0.13–2.74) | 0.510 | 0.70 (0.40–1.24) | 0.225 | 1.69 (0.59–4.83) | 0.324 |
| Age | ||||||
| Age < 65 years old | Reference | --- | Reference | --- | Reference | --- |
| Age ≥ 65 years old | 3.62 (2.44–5.35) | <0.001 | 1.84 (1.59–2.13) | <0.001 | 1.22 (1.01–1.46) | 0.038 |
| Sex | ||||||
| Male | Reference | Ref | Reference | --- | Reference | Ref |
| Female | 0.47 (0.31–0.70) | <0.001 | 0.67 (0.58–0.77) | <0.001 | 0.83 (0.70–0.99) | 0.042 |
| Major injury or not | ||||||
| RTS score | ||||||
| RTS < 7 | 5.15 (3.32–7.99) | <0.001 | 5.97 (4.58–7.78) | <0.001 | 2.75 (2.16–3.51) | <0.001 |
| RTS ≥ 7 | Reference | --- | Reference | --- | Reference | --- |
| ISS score | ||||||
| ISS < 16 | Reference | --- | Reference | --- | Reference | --- |
| ISS ≥ 16 | 8.29 (4.54–15.1) | <0.001 | 20.3 (16.5–25.0) | <0.001 | 5.74 (4.39–7.50) | <0.001 |
| TBI status | ||||||
| No TBI | Reference | --- | Reference | --- | Reference | --- |
| TBI | 1.59 (0.91–2.81) | 0.106 | 9.63 (7.66–12.1) | <0.001 | 1.90 (1.43–2.52) | <0.001 |
| Injury type | ||||||
| Blunt injury | Reference | --- | Reference | --- | Reference | --- |
| Penetrating injury | 1.36 (0.38–4.90) | 0.636 | 0.48 (0.34–0.67) | <0.001 | 1.28 (0.86–1.90) | 0.223 |
| Mechanism | ||||||
| Road traffic injury | Reference | --- | Reference | --- | Reference | --- |
| High fall | 1.09 (0.61–1.93) | 0.776 | 0.77 (0.60–0.98) | 0.033 | 1.25 (0.95–1.63) | 0.106 |
| Low fall | 0.98 (0.61–1.55) | 0.920 | 0.55 (0.46–0.66) | <0.001 | 0.66 (0.52–0.84) | 0.001 |
| Others | 0.70 (0.39–1.26) | 0.234 | 1.78 (1.49–2.12) | <0.001 | 1.13 (0.89–1.44) | 0.304 |
Abbreviations: OR: odds ratio; CI: confidence interval; RTS: revised trauma score; ISS: injury severity score; TBI: traumatic brain injury.
Figure 2.
Subgroup analysis illustrating association between a 5 min increase in waiting emergent surgery time (WEST) and in-hospital mortality, ICU admission, and prolonged hospital stay (≥30 days) across various subgroups.
4. Discussion
Our findings revealed no association between WEST and in-hospital mortality, ICU admission, and prolonged hospital stay (≥30 days). However, the subgroup analysis indicated that a longer WEST (per 5 min) was associated with increased survival in patients with a WEST ≥ 90 min, those aged < 65 years, those aged ≥ 65 years, those with minor injuries (RTS ≥ 7 and ISS < 16), those with major injuries (RTS < 7 or ISS ≥ 16), and those with major injuries to the head (head AIS ≥ 3). Additionally, a longer WEST was associated with an increased risk of ICU admission in patients with a WEST ≥ 90 min, those aged ≥ 65 years, those with minor injuries, and those with major injuries in the abdomen.
Previous studies investigating the relationship between waiting time for surgery and mortality and functional outcomes have predominantly focused on fracture surgeries. For example, the TRON Study, a propensity score–matched multicenter investigation involving 779 patients who underwent ankle fracture surgery, revealed significantly longer operative times and higher infection rates in their delayed operation group compared with their early operation group [15]. Pincus et al. [16] analyzed 42,230 patients with hip fractures and revealed that prolonged wait times were associated with an increased risk of 30-day mortality and other complications. The time window for waiting for surgery is considerably narrower for complex fractures and major traumatic injuries than it is for simple fractures. Several studies have provided support for the golden hour concept with respect to emergent surgery. Hsieh et al. analyzed the data of 963 trauma patients from the Pan-Asian Trauma Outcome Study registry and revealed a positive association between a shorter time to definitive care within 2 h and patient survival and functional outcomes [14]. Another observational study that used data from the Trauma and Audit Research Network revealed that trauma patients who underwent secondary transfer experienced a prolonged time to urgent surgery and increased crude mortality rates [17]. However, our study did not obtain evidence supporting these associations, even among the subgroups with major trauma, TBI, major chest injuries, and torso injuries. The relationship between WEST and trauma outcomes might be influenced by presurgical treatments, which can attenuate the effect of WEST and render the effect nonsignificant. This underscores the importance of actively promoting recovery during the waiting period for surgery through interventions such as proactive blood and fluid transfusions, administration of hemostatic medications, maintenance of body temperature, and ensuring adequate ventilation to prevent acidosis [18,19]. Furthermore, the number and type of presurgical treatments can influence the time to emergent surgery. Surgeons and anesthesiologists generally consider stable baseline blood pressure and HR to be necessary for effective surgery. Conservative trauma practitioners may even advocate for ensuring acceptable blood pressure levels before surgery to avoid potential complications associated with operating on hemodynamically unstable patients. Therefore, patients with major trauma might experience a slightly higher WEST than those with minor injuries do; this extended WEST may be partially attributable to implementation of preoperative stabilization treatments and may reflect the greater complexity of injuries requiring more interventions. Nevertheless, studies investigating WEST and patient outcomes have failed to account for the potential confounding effect of presurgical treatments, which may have introduced bias into their results [14,17].
In our study, a subgroup analysis focusing on patients with major head, chest, and abdominal injuries revealed that longer intervals prior to surgical intervention did not increase the risk of mortality in the TBI population, nor did it have any association with the outcomes of patients with major chest or abdominal injuries. This finding contrasts with those of previous research primarily focused on TBIs [20,21]. A key reason for this inconsistency is that the location and severity of head trauma exert a more substantial influence on clinical outcomes than the timing of surgical procedures does. In clinical practice, neurosurgeons typically evaluate the prognoses of patients with head trauma and recommend surgery accordingly. For patients with severe injuries, surgical intervention may not significantly influence outcomes, whereas for those with less severe injuries, immediate surgery may not be required. Instead, the patient may be observed to determine whether surgical intervention is necessary as the condition evolves. Therefore, the inclusion of observation time in calculations of WEST for patients with TBI may introduce bias. Considering patients who are under observation before surgery in combination with those who require immediate surgery, such as those with epidural hematomas, may lead to findings indicating lower in-hospital mortality rates and longer intervals to definitive care. This underscores the influence of patient heterogeneity on outcomes and indicates that certain types of TBI may not require immediate intervention. Consistent with our findings, a meta-analysis of 16 studies revealed that patient outcomes were not significantly influenced by the timing of surgery in 68.7% of the included studies. Moreover, the effect of time to surgery on outcomes was not significant in the majority (75%) of studies focusing on patients with severe TBI [22]. In the current study, we considered different TBI severities (mild, moderate, and severe). The results indicated that shorter intervals to emergent surgery did not reduce in-hospital mortality in mild or severe TBI populations (mild TBI: aOR = 0.993, 95% CI = 0.987–0.999; moderate TBI: aOR = 0.997, 95% CI = 0.988–1.006; severe TBI: aOR = 0.992, 95% CI = 0.985–0.999). Future studies should conduct in-depth analyses of various traumatic intracranial hemorrhage types and include parameters such as the bleeding volume and brain herniation to minimize bias.
This study has several strengths. First, it validated the golden hour concept for surgical intervention in trauma patients. This finding holds clinical importance because it underscores the importance of timely stabilization of injury conditions and adequate resuscitation. Second, we conducted many subgroup analyses to investigate the association between WEST and clinical outcomes. These analyses confirmed that a shorter WEST did not significantly reduce the risk of mortality in trauma patients, even in those with major trauma injuries. This indicates that adequate resuscitation may be more crucial than shortening the WEST is.
This study has some limitations that should be considered. First, because this was a retrospective study, data may be missing, which may have introduced bias. The unmeasured variables in this study may also have influenced the study results. Moreover, our exclusion of unreasonable data points and outliers may have introduced selection bias into the final dataset. Although a randomized controlled trial could address these limitations, ethical considerations might render such a trial infeasible. The majority of the excluded patients lacked documentation for critical variables such as time to definitive care and mortality outcomes, which are crucial aspects of our analysis. Furthermore, imputing missing data for time to definitive care and mortality outcome data would be inappropriate because of the considerable variability in these measures related to factors such as hospital capacity, injury severity, and personalized treatment plans. Imputation under these circumstances could lead to inaccurate estimations. Additionally, imputing missing data for other variables would not notably improve the accuracy of the analysis. To mitigate these limitations, we compared the baseline characteristics between the included patients and patients excluded because of missing data (refer to Supplementary Table S2). Significant differences were noted between the two groups, particularly for outcome variables such as in-hospital mortality, ICU admission, and prolonged hospitalization. However, the in-hospital mortality rates were not statistically different between the included and excluded samples. Moreover, some missing data for time to definitive care may be considered “missing at random” because case managers may not have accurately predicted patient outcomes when documenting this variable. Second, emergency medical system dispatch times can considerably influence a patient’s WEST and clinical outcomes. However, because prehospital transport times in Taiwan are generally < 20 min, we excluded this variable from the analysis; in Taipei, the median transport interval is 7 min, and the median prehospital interval is 23 min, which are significantly shorter than those in other countries [23]. Third, our study excluded patients who did not receive surgical intervention. However, we were unable to determine the reasons for these patients ultimately not undergoing surgery. Possible reasons include ‘Do not resuscitate’ orders and poor prognosis leading to palliative care. Fourth, although the severity of injury is a major determinant of mortality among trauma patients, surgeons employing a proactive approach may also influence patient outcomes. Currently, no objective assessment method is available for this surgeon-specific factor. Fifth, missing data on resuscitation interventions for trauma patients, such as fluid resuscitation volume, blood transfusion, transcatheter arterial embolization, and emergent thoracotomy, may have influenced the study outcomes. These interventions can prolong the WEST, and accounting for them is crucial to accurately evaluating the effect of time to surgery. However, current studies supporting the golden hour concept often lack adjustment for these variables [14,24]. Finally, our findings may not be applicable to the general population. Major injuries were uncommon in our data (7.4%), with blunt injuries being the most prevalent (5.3%). Falls were the leading cause of injury (50%), with high falls accounting for 10.1% and lower falls accounting for 39.9% of the injuries. Further research involving broader populations and robustly controlling for confounding factors is required to validate our findings.
5. Conclusions
Our findings revealed no significant association between time to emergent surgery and in-hospital mortality, ICU admission, or prolonged hospital stays of ≥30 days, which contradicts the golden hour concept. Furthermore, our subgroup analysis revealed that a longer WEST (per 5 min) was associated with increased survival for patients with a WEST of ≥90 min, regardless of age group (<65 and ≥65 years), injury severity (minor injury with RTS ≥ 7 and ISS < 16 and major injury with RTS < 7 or ISS ≥ 16), and injury site (major injuries to the head, with head AIS ≥ 3).
Abbreviations
| WEST | Waiting emergent surgery time |
| ICU | Intensive care unit |
| LOS | Length of stay |
| IQR | Interquartile range |
| aOR | Adjusted odds ratio |
| CI | Confidence interval |
| HR | Heart rate |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| RR | Respiratory rate |
| ISS | Injury severity score |
| RTS | Revised trauma score |
| TBI | Traumatic brain injury |
| AIS | Abbreviated injury score |
| CNS diseases | Central nervous system diseases |
| CKD | Chronic kidney disease |
| CVD | Cardiovascular disease |
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/medicina60060960/s1, Table S1: STROBE Statement of current cohort study; Table S2: Comparison of demographic characteristics of included patients and patients with missing values.
Author Contributions
Study design: C.-H.T., M.-Y.W., D.-S.C., J.-Y.C. and P.-C.L.; data collection and analysis: C.-Y.L., I.-S.T. and Y.-T.H.; manuscript preparation: C.-H.T., M.-Y.W., Y.-L.C. and G.-T.Y.; writing—original draft preparation: C.-H.T., M.-Y.W., D.-S.C., J.-Y.C. and G.-T.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This retrospective cohort study was approved by Taipei Tzu Chi Hospital’s Institutional Review Board (number: 12-XD-077, approved date: 20 September 2023). The ethics committee waived the requirement for participant consent because of the retrospective nature of the study and the use of anonymized data.
Informed Consent Statement
Patient consent was waived due to retrospective nature of the study and the use of anonymized data by Taipei Tzu Chi Hospital’s Institutional Review Board.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare that they have no conflicts of interest with respect to the publication of this article.
Funding Statement
This research was supported by grants from Taipei Tzu Chi Hospital (TCRD-TPE-113-RT-4, TCRD-TPE-113-48).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Lin P.-C., Wu M.-Y., Chien D.-S., Chung J.-Y., Liu C.-Y., Tzeng I.-S., Hou Y.-T., Chen Y.-L., Yiang G.-T. Use of Reverse Shock Index Multiplied by Simplified Motor Score in a Five-Level Triage System: Identifying Trauma in Adult Patients at a High Risk of Mortality. Medicina. 2024;60:647. doi: 10.3390/medicina60040647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T.-H., Wu M.-Y., Shin S.D., Jamaluddin S.F., Son D.N., Hong K.J., Jen-Tang S., Tanaka H., Hsiao C.-H., Hsieh S.-L., et al. Discriminant ability of the shock index, modified shock index, and reverse shock index multiplied by the Glasgow coma scale on mortality in adult trauma patients: A PATOS retrospective cohort study. Int. J. Surg. 2023;109:1231–1238. doi: 10.1097/js9.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Y.-C., Lin P.-C., Liu C.-Y., Tzeng I.-S., Lee S.-J., Hou Y.-T., Chen Y.-L., Chien D.-S., Yiang G.-T., Wu M.-Y. Prehospital shock index multiplied by AVPU scale as a predictor of clinical outcomes in traumatic injury. Shock. 2022;58:524–533. doi: 10.1097/SHK.0000000000002018. [DOI] [PubMed] [Google Scholar]
- 4.Lin P.-C., Liu C.-Y., Tzeng I.-S., Hsieh T.-H., Chang C.-Y., Hou Y.-T., Chen Y.-L., Chien D.-S., Yiang G.-T., Wu M.-Y. Shock index, modified shock index, age shock index score, and reverse shock index multiplied by Glasgow Coma Scale predicting clinical outcomes in traumatic brain injury: Evidence from a 10-year analysis in a single center. Front. Med. 2022;9:3478. doi: 10.3389/fmed.2022.999481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang H.-K., Liu C.-Y., Tzeng I.-S., Hsieh T.-H., Chang C.-Y., Hou Y.-T., Lin P.-C., Chen Y.-L., Chien D.-S., Yiang G.-T., et al. The association between blood pressure and in-hospital mortality in traumatic brain injury: Evidence from a 10-year analysis in a single-center. Am. J. Emerg. Med. 2022;58:265–274. doi: 10.1016/j.ajem.2022.05.047. [DOI] [PubMed] [Google Scholar]
- 6.Chien D.-S., Yiang G.-T., Liu C.-Y., Tzeng I.-S., Chang C.-Y., Hou Y.-T., Chen Y.-L., Lin P.-C., Wu M.-Y. Association of In-Hospital Mortality and Trauma Team Activation: A 10-Year Study. Diagnostics. 2022;12:2334. doi: 10.3390/diagnostics12102334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forrester J.D., August A., Cai L.Z., Kushner A.L., Wren S.M. The Golden Hour After Injury Among Civilians Caught in Conflict Zones. Disaster Med. Public Health Prep. 2019;13:1074–1082. doi: 10.1017/dmp.2019.42. [DOI] [PubMed] [Google Scholar]
- 8.Wu M.-Y., Lin P.-C., Liu C.-Y., Tzeng I.-S., Hsieh T.-H., Chang C.-Y., Hou Y.-T., Chen Y.-L., Chien D.-S., Yiang G.-T. The impact of holiday season and weekend effect on traumatic injury mortality: Evidence from a 10-year analysis. Tzu-Chi Med. J. 2023;35:69. doi: 10.4103/tcmj.tcmj_20_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McIsaac D.I., Abdulla K., Yang H., Sundaresan S., Doering P., Vaswani S.G., Thavorn K., Forster A.J. Association of delay of urgent or emergency surgery with mortality and use of health care resources: A propensity score–matched observational cohort study. Can. Med. Assoc. J. 2017;189:E905–E912. doi: 10.1503/cmaj.160576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed K., Zygourakis C., Kalb S., Pennington Z., Molina C., Emerson T., Theodore N. Protocol for Urgent and Emergent Cases at a Large Academic Level 1 Trauma Center. Cureus. 2019;11:e3973. doi: 10.7759/cureus.3973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Baker S.P., O’Neill B., Haddon W., Jr., Long W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma. 1974;14:187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Champion H.R., Sacco W.J., Copes W.S., Gann D.S., Gennarelli T.A., Flanagan M.E. A revision of the Trauma Score. J. Trauma. 1989;29:623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Hsieh S.-L., Hsiao C.-H., Chiang W.-C., Shin S.D., Jamaluddin S.F., Son D.N., Hong K.J., Jen-Tang S., Tsai W., Chien D.-K., et al. Association between the time to definitive care and trauma patient outcomes: Every minute in the golden hour matters. Eur. J. Trauma Emerg. Surg. 2022;48:2709–2716. doi: 10.1007/s00068-021-01816-8. [DOI] [PubMed] [Google Scholar]
- 15.Sugino T., Takegami Y., Bando K., Sato T., Fujita T., Oka Y., Imagama S. The Wait Time for Surgery Following Injury Affects Functional Outcomes and Complications After an Ankle Fracture: A Propensity Score–Matched Multicenter Study, the TRON Study. Foot Ankle Spec. 2023 doi: 10.1177/19386400231164211. [DOI] [PubMed] [Google Scholar]
- 16.Pincus D., Ravi B., Wasserstein D., Huang A., Paterson J.M., Nathens A.B., Kreder H.J., Jenkinson R.J., Wodchis W.P. Association Between Wait Time and 30-Day Mortality in Adults Undergoing Hip Fracture Surgery. JAMA. 2017;318:1994–2003. doi: 10.1001/jama.2017.17606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haslam N.R., Bouamra O., Lawrence T., Moran C.G., Lockey D.J. Time to definitive care within major trauma networks in England. BJS Open. 2020;4:963–969. doi: 10.1002/bjs5.50316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galbraith C.M., Wagener B.M., Chalkias A., Siddiqui S., Douin D.J. Massive Trauma and Resuscitation Strategies. Anesthesiol. Clin. 2023;41:283–301. doi: 10.1016/j.anclin.2022.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cantle P.M., Cotton B.A. Balanced Resuscitation in Trauma Management. Surg. Clin. N. Am. 2017;97:999–1014. doi: 10.1016/j.suc.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Chockalingam K., A Rahman N.A., Idris Z., Theophilus S.C., Abdullah J.M., Ghani A.R.I., Ali A. Door-to-Skin Time in Patient Undergoing Emergency Trauma Craniotomy. Malays. J. Med. Sci. 2023;30:71–84. doi: 10.21315/mjms2023.30.4.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim Y.J. The Impact of Time from ED Arrival to Surgery on Mortality and Hospital Length of Stay in Patients with Traumatic Brain Injury. J. Emerg. Nurs. 2011;37:328–333. doi: 10.1016/j.jen.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 22.Kim Y.-J. The impact of time to surgery on outcomes in patients with traumatic brain injury: A literature review. Int. Emerg. Nurs. 2014;22:214–219. doi: 10.1016/j.ienj.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Shih J.Y.M., Shih J.J.M. Pre-Hospital Time Intervals among Trauma Patients in Northern Taiwan. Taiwan Crit. Care Med. 2011;12:166–174. [Google Scholar]
- 24.Mader M.M.-D., Rotermund R., Lefering R., Westphal M., Maegele M., Czorlich P., DGU The faster the better? Time to first CT scan after admission in moderate-to-severe traumatic brain injury and its association with mortality. Neurosurg. Rev. 2021;44:2697–2706. doi: 10.1007/s10143-020-01456-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.