Abstract
BACKGROUND/OBJECTIVES:
To describe the use of home-based medical care (HBMC) among Medicaid beneficiaries.
DESIGN:
A systematic review of the peer-reviewed and gray literature of home-based primary care and palliative care programs among Medicaid beneficiaries including dual eligibles.
SETTING:
HBMC including home-based primary care and palliative care programs.
PARTICIPANTS:
Studies describing Medicaid beneficiaries receiving HBMC.
MEASUREMENTS:
Three groups of studies were included: those focused on HBMC specifically for Medicaid beneficiaries, studies that described the proportion of Medicaid patients receiving HBMC, and those that used Medicaid status as a dependent variable in studying HBMC.
RESULTS:
The peer-reviewed and gray literature searches revealed 574 unique studies of which only 16 met inclusion criteria. Few publications described HBMC as an integral care delivery model for Medicaid programs. Data from the programs described suggest the use of HBMC for Medicaid beneficiaries can reduce healthcare costs. The addition of social supports to HBMC appears to convey additional savings and benefits.
CONCLUSION:
This systematic literature review highlights the relative dearth of literature regarding the use and impact of HBMC in the Medicaid population. HBMC has great potential to reduce Medicaid costs, and innovative programs combining HBMC with social support systems need to be tested.
Keywords: home-based primary care, Medicaid, dual eligible, home-based medical care
At least 7.5 million fragile, vulnerable adults in the United States have difficulty obtaining or are completely unable to access office-based primary care because they are frail, functionally limited, and homebound. They are among the costliest patients to the U.S. healthcare system because of the impact of the powerful combination of multiple chronic conditions, functional impairment, frailty, and social stressors.1 Their needs and limited ability to access primary care result in unnecessary emergency department (ED) visits, hospitalizations, and downstream healthcare expenditure.
Home-based medical care (HBMC) that includes home-based primary care (HBPC) and home-based palliative care (HBPalC) provides a mechanism for such patients to access ongoing care in the community setting. HBMC was demonstrated to reduce the costs of health care in multiple studies2 and in the Centers for Medicare & Medicaid (CMS) Innovation Center Independence at Home Demonstration.3 However, although there are more than twice as many homebound adults as there are adults in nursing homes, about seven times more primary care providers made nursing home visits than home visits.
Most available data on HBMC focuses on Medicare beneficiaries.4 The role of HBMC for Medicaid beneficiaries is more opaque. Medicaid has traditionally been the safety-net healthcare program for the country and long-term care provider for most states.5 In 2015, it covered more than 70 million Americans with low incomes.6 Over time, Medicaid has also shifted from a predominantly fee-for-service system to managed care. By 2015, 48 states used some form of managed care to serve Medicaid beneficiaries. Concurrently, Medicaid long-term care benefits also shifted from institutional care to the home such that a larger portion of Medicaid spending is focused on care in the home. Although most of these benefits have been in the form of home and community long-term care based services that do not include HBMC, it stands to reason that persons previously eligible for nursing home care might benefit from medical care in the home. With the evolution of Medicaid payment strategies, HBMC, which was shown to reduce inpatient and long-term care utilization,2,7 offers a potentially attractive model for high-need homebound Medicaid populations.
There is a dearth of data on how HBMC is used in Medicaid populations or by state Medicaid plans. The aim of this study was to perform a scoping review of the literature to describe the use of HBMC among Medicaid beneficiaries and its impact on population and individual patient outcomes.
METHODS
Definitions
We defined our population as homebound Medicaid beneficiaries aged 18 and older. The intervention comprised receipt of HBPC or HBPalC that together make up HBMC. We defined HBPC as the delivery of primary longitudinal, often interdisciplinary, medical care by a physician, nurse practitioner (NP), or physician assistant to homebound individuals in their homes. We defined HBPalC as the delivery of palliative care focused on symptom management and quality of life delivered to patients with serious or life-limiting illness in their homes. Most studies describe the delivery of HBPC only.
Our comparison group (when applicable) included homebound Medicaid beneficiaries not receiving HBPC or HBPalC. Outcomes included cost, health service utilization (including inpatient admissions, hospital days, and skilled nursing facility use), quality of care, and patient/caregiver satisfaction with care, community survival, and mortality rate.
Data Sources and Search Strategies
We performed systematic searches of the peer-reviewed and gray literature on the use of HBPC and HBPalC among Medicaid beneficiaries. For the peer-reviewed literature search, we collaborated with a clinical informationist to identify search terms for Medline, the U.S. National Library of Medicine’s source of journal citations and abstracts for bio-medical literature. Search terms were adapted to facilitate searches of the Cumulative Index to Nursing & Allied Health, Embase, Web of Science, and Scopus libraries. Searches included all articles published in the English language before March 2019 (Figure 1).
Figure 1.
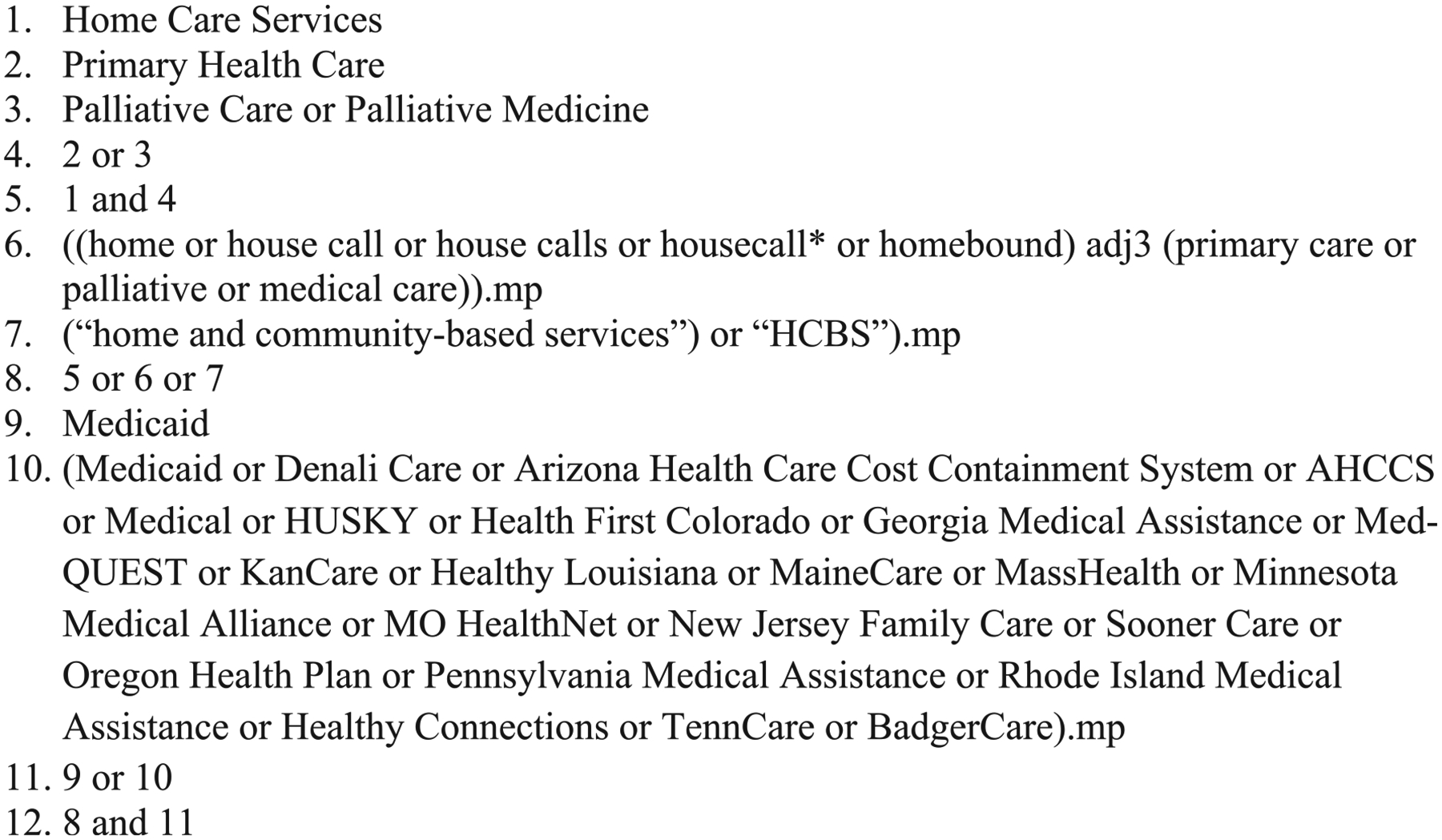
Embase search terms for peer-reviewed literature search.
Further, we conducted a search of relevant sources in the gray literature including databases of journalistic, academic, and mass publications including ProQuest, JSTOR, and LexisNexis using Boolean search terms adapted from those of the peer-reviewed medical literature review. We also searched publications from policy advisory groups, think tanks, and professional groups including Mathematica Policy Research, the Commonwealth Fund, the John A. Hartford Foundation, the Center for Health Care Strategies, the Home Centered Care Institute, and the American Academy of Home Care Medicine. Relevant online publications that may not be indexed in previously searched databases were also included, such as the Health Affairs Blog and the NEJM Catalyst. Finally, we sought to identify relevant documents, policy briefs, or research from CMS, the Agency for Healthcare Research and Quality, and the Center for Medicare & Medicaid Innovation. These sources were searched using the terms “home-based primary care” and “home-based palliative care” and subsequently screened for relevance to Medicaid beneficiaries.
Study Selection
We first examined studies that addressed the narrow question of the use and impact of HBPC or HBPalC on Medicaid beneficiaries. Inclusion criteria included only studies where provision of HBMC was delivered to Medicaid patients. We excluded care not delivered in the home by a billing/prescribing clinician, defined as a medical doctor, doctor of osteopathic medicine, physican assistant, or NP. Therefore, non-physician, non–advanced practice provider programs, such as the Community Aging in Place, Advancing Better Living for Elders (CAPABLE),8 were not included. Also excluded were interventions in which physicians oversaw the provision of care by nurses and ancillary staff in the home, such as the Promoting Effective Advance Care for Elders (PEACE) program.9
Home-based interventions consisting solely of home- and community-based services (HCBS) were excluded because they did not meet our definition of HBPC or HBPalC. Although some HCBS programs included care coordination services in the home with oversight from a primary care physician or geriatrician, these programs did not deliver medical care in the home. We also excluded studies focused on Program for All-inclusive Care of the Elderly (PACE) programs because these programs provide comprehensive services well beyond HBMC, such as primary and specialty medical care, nursing and social services, occupational and physical therapies, and day health center services.10
Additional Queries
Because studies of HBMC focused on Medicaid beneficiaries are relatively sparse, we also sought to understand whether Medicaid beneficiaries were included in studies of HBMC that cared for populations that included but were not focused solely on Medicaid beneficiaries. For this query, we included studies of HBMC where Medicaid beneficiaries or dual-eligible beneficiaries participated or were included as a subgroup of the broader study population (e.g., a study of outcomes and costs among patients of an HBPC program, some of whom were Medicaid beneficiaries). Limitations of data reporting from these studies precluded extracting outcomes for only Medicaid patients, but we deemed these studies worthy of inclusion because these home-based models did serve Medicaid patients.
Finally, we examined intervention studies in which some of the population studied were Medicaid beneficiaries to see if there was an association between Medicaid enrollment and outcomes. For this query, we included HBPC or HBPalC studies in which Medicaid was a studied covariate: for example, a study of the place of death for patients of an HBPC practice that found Medicaid enrollment was associated with a particular outcome.
Article Review
We screened all articles and sources identified through the peer-reviewed and gray literature searches for potential inclusion using the Covidence systematic review management system. We reviewed references of all included studies to check for additional articles, and when appropriate we reached out to researchers for information about unpublished data or other potentially relevant materials.
Two reviewers (R.Z. and O.S.) independently screened abstracts for potential inclusion. Discrepancies were resolved by consensus with the other two reviewers (B.L. and C.R.). Two reviewers (R.Z. and O.S.) then independently assessed the full text of potentially relevant articles. Both reviewers had to agree on eligibility. Discrepancies were discussed and consensus reached among the full research team. Data extraction for each article was performed by two researchers, and the results were compiled by a third member of the team. One researcher (R.Z.) reviewed the gray literature results in detail and compiled relevant sources for review by the whole team.
Data Quality
The quality of studies described in Table 1 was assessed where possible (commentaries and editorials excluded) using the Newcastle-Ottawa Scale for quality assessment.17
Table 1.
Articles Focused on Home-Based Medical Care for Medicaid Beneficiaries
| Study | Study design/Aim | Population studied (number in cohort) | % Medicaid | Outcomes assessed | Key findings |
|---|---|---|---|---|---|
| Master11 | Case study of the Community Medical Alliance, a clinical care system that contracts with Massachusetts Medicaid program on a fully capitated basis | Patients with advanced AIDS or severe disability (818) | 100 | Satisfaction, quality, cost | Most medical encounters were with NPs in the home setting; considerable cost reduction through reduced use of hospitals. |
| Fisher and Raphael12 | Case study of VNSNY CHOICE’s history, operating structure, and LTC service delivery model | Medicaid-eligible VNSNY CHOICE patients (2,509) | 100 | Utilization of capitated services, hospitalizations, nursing home utilization | Model includes enhanced clinical support (including home visits to members) and clinical consultations with nursing staff as well as education and training for staff. NPs serve as PCPs, working closely with physicians to achieve a shared understanding of a member’s needs, care planning, status changes, and joint visits with physicians when needed. Clinical, behavioral, social, and environmental resources available when needed; 24-hour, 7-day a week nurse-answered telephone triage system |
| Meyer13 | Description of the Commonwealth Care Alliance, a multidisciplinary PCP funded by Medicare and Medicaid | Two programs described: (1) Senior Care Options (homebound older persons) (2) Disability Care Program (2,965) |
100 | Cost, utilization, quality of care | Senior Care Options members: 45% fewer hospital days than comparable FFS dual-eligible patients; NH placement 30% lower than comparable Medicaid FFS persons. Growth rates for total medical spending were much lower for Senior Care Options members than FFS nursing home eligible. Total monthly cost for Disability Care Program patients was $3,601 in 2008 compared with $5,210 for Medicaid FFS patients with conditions of similar severity. |
| Trilla et al.14 | Retrospective chart review to describe NP-driven home-based intervention for high-risk, frail Medicaid population | Patients of an MCO (879) | 100 | Inpatient admissions, hospital days, total cost | 57.4% reduction in inpatient admissions per 1,000 members per year; 36.5% reduction in ED visits over 2 years; 19.1% decrease in total medical expenses per member per month. |
| Valluru et al.15 | Case-cohort study to determine effect of HBPC for frail older adults, operating under IAH incentive alignment, on LTI | Three IAH-participating HBPC sites in Philadelphia, PA; Richmond, VA; and Washington, DC (1,376) | Comparison group with HBPC: 36.6% Comparison group without HBPC: 38.9% | LTI rate, mortality rates, community survival, and LTSS costs | LTI rate at least 50% less than both comparison groups in all three programs; LTI for patients at each HBPC site declined over the 3 study years; HCBS costs nonsignificantly lower among integrated care patients; community residence extended by 12.8 mo compared with comparison group. |
| Davis et al.16 | Commentary on a policy proposal to finance home- and community-based services | 2012 Medicare beneficiaries | 18 | Not described | Adoption of HCBS benefit in Medicare would improve financial protection for beneficiaries with physical and/or cognitive impairment and provide the financing for health organizations to better integrate medical and social services. ICOs and delivery models of care emphasizing care at home would improve accessibility of care and avoid costly institutionalization. HCBS benefit in Medicare would also reduce beneficiary reliance on Medicaid. |
Abbreviations: AIDS, acquired immunodeficiency syndrome; ED, emergency department; FFS, fee for service; HBPC, home-based primary care; HCBS, home- and community-based services; IAH, Independence at Home; LTC, long-term care; LTI, long-term institutionalization; LTSS, long-term social supports; MCO, managed care organization; NH, nursing home; NP, nurse practitioner; PCP, primary care provider; VNSNY, Visiting Nurse Service of New York.
RESULTS
Identification of Eligible Studies
The search of the peer-reviewed literature yielded 529 unique studies for screening. Of these initial search results, 476 did not meet the inclusion criteria described earlier. Of the 53 studies deemed potentially relevant, 27 met inclusion criteria and underwent full review; 12 articles were deemed not in scope after full review, resulting in 15 peer-reviewed articles. The 12 studies were excluded because they were not about longitudinal HBMC (seven), they only described physician or author attitudes or opinions (three) and the study included Medicare beneficiaries only, not Medicaid (one), results were not yet available (one) (Figure 2).
Figure 2.
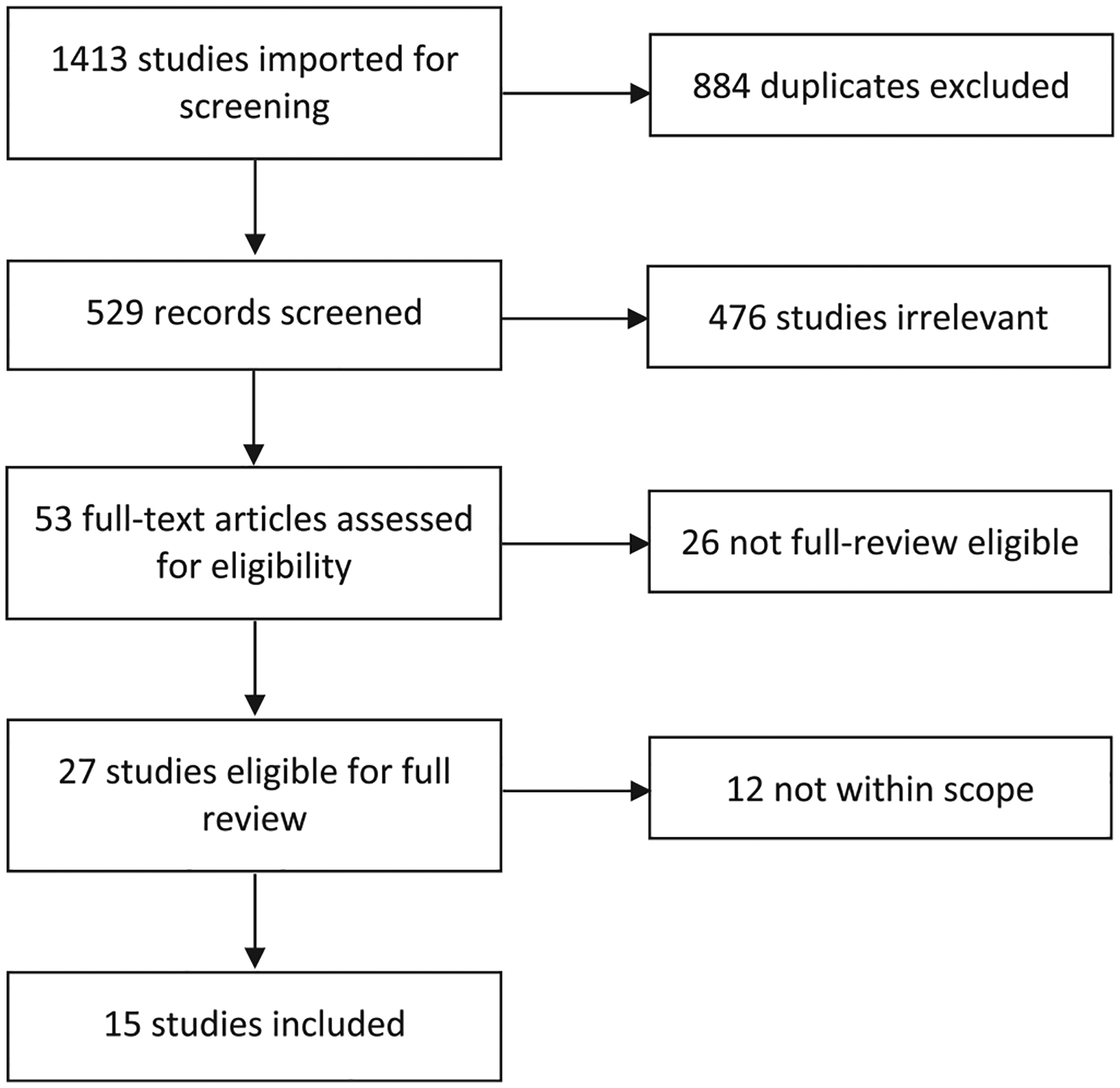
Flow diagram of peer-reviewed literature article selection.
The gray literature search identified 45 reports, briefs, articles, or other potentially relevant documents. Of these, only one article met inclusion criteria. From both the peer-reviewed and gray literature, a total of 16 articles were included in this review with six studies that focused on HBMC specifically for Medicaid beneficiaries, eight studies that described the proportion of Medicaid patients receiving HBMC, and two studies in which Medicaid status was a dependent variable in studying HBMC.
Articles Focused Specifically on Home-Based Medical Care for Medicaid Beneficiaries
Six articles published between 1998 and 2019 focused specifically on HBMC for Medicaid beneficiaries. None of these studies were clinical trials, and only three had a comparison group. No study achieved a high-quality rating.17 Table 1 describes the data from these studies.
Five articles evaluated specific programs. Master described the Community Medical Alliance (CMA), a Boston-based clinical care system that contracted with the Massachusetts Medicaid program on a fully capitated basis to treat patients with advanced acquired immunodeficiency disease or severe disability.11 Medical care in the home was delivered mostly by NPs. Costs for the CMA ranged between $219 and $1,021 lower than historical fee-for-service costs.
Fisher and Raphael described the Visiting Nurse Service of New York (VNSNY) CHOICE Health Plans, a managed long-term care integration model, provided to more than 2,500 Medicaid-eligible frail older adults with extensive functional and cognitive impairments as well as complex medical, psychosocial, and long-term care needs.12 Medical care in the home was provided mostly by NPs. The authors described nursing home admission and hospital admission rates of 11.6% and 41.2%, respectively, but they did not compare their rates with historical or concurrent controls.
Meyer et al. described the Massachusetts Commonwealth Care Alliance, a multidisciplinary primary care practice supporting dual-eligible homebound older persons (Senior Care Options) as well as severely disabled adults; 70% of the 2,965 members were nursing home eligible.13 The program, managed primarily by NPs, includes comprehensive in-home assessment and 24/7 access to clinical assistance. Senior Care Options’ hospital days were 55% of a comparable dual-eligible member cared for in a fee-for-service payment environment. Nursing home placements for eligible members was 30% of the comparable rate.
Trilla et al. described a NP-driven home-based intervention for high-risk frail Medicaid population in a New England managed care organization that involved an NP lead working in collaboration with a community health worker, pharmacist, and medical director. Like Senior Care Options, they had comprehensive assessments and 24/7 service. The comparison group included patients who met eligibility criteria for joining the program but were determined unsafe for home visits. Although the comparison group was not optimal given their likely more complex living environments, the authors found a 57% reduction in medical inpatient admissions, a 37% decrease in ED visits over 2 years, and a reduction in total medical expenses per member per month of 19%.14
In a case-cohort study using HBPC site information, Medicare administrative data, and National Health and Aging Trends Study benchmarks, Valluru and coauthors compared outcomes of three HBPC programs integrated with Medicaid long-term services with outcomes of similar cohorts not receiving HBPC by comparing HBPC outcomes with long-term institutionalization (LTI) and HCBS benchmarks. They found that Medicaid long-term services integrated with HBPC was associated with LTI at half the rate of the comparison benchmarks.15
Although not a study assessing outcomes of a HBPC program for Medicaid populations, Davis et al. argued that an integrated home-based medical and social care model would protect vulnerable patients, improve access to care, and avoid LTI that would otherwise be paid for by Medicaid.16
Articles Focused on HBMC Populations That Included Medicaid Patients
Table 2 provides details on eight articles focused on HBMC that included Medicaid beneficiaries as patients. Three of the studies were surveys of HBPC practices in the United States. In 2009, Landers et al. reported on 36 practices and found that 20% of practice patients were dual eligible and 6.5% of participants were Medicaid beneficiaries only.18 In 2015, Leff et al. reported on 272 HBPC practices with a mean daily census of 457, and they found that 9% had Medicaid as their primary insurance and 21% of practices reported that most of their patients were dual eligible.21 In 2018, in a survey of 101 HBMC practices, Norman et al. found that 26% of practices had practice panels composed of at least 50% dual-eligible patients.23
Table 2.
Articles Focused on Home-Based Medical Care That Included Medicaid Populations
| Study | Study design/Aim | Population studied (number in cohort) | % Medicaid | % Medicare | Outcomes assessed | Key findings |
|---|---|---|---|---|---|---|
| Landers et al.18 | Survey to describe characteristics of house call and home medical care practices in the United States | 36 HBPC practices | 20% dual eligible; 6% Medicaid only | 70% Medicare FFS; 7% Medicare Advantage | Patient and clinician characteristics |
|
| De Jonge et al.19 | Case-control study to examine effects of HBPC program on costs and survival | Newly enrolled patients (722 cases and 2,161 controls) | 36% | 100% | Medicare cost, mortality, healthcare utilization |
|
| Kronish et al.20 | Retrospective cross-sectional study to examine association between medication use and socioeconomic and disease factors | 417 patients of a New York–based HBPC practice | 64% | 61% | Medication use and medication expenditures |
|
| Left et al.21 | Survey to describe characteristics of HBPC practices | 272 HBPC practices | 9% Medicaid primary insurer; 47% dual eligible | 63% Medicare as primary insurer | Practice characteristics, percentage of practices using defined Ql protocols and associated factors |
|
| Kinosian et al.22 | Projections to estimate potential CMS savings if IAH was converted to a national program | 2,182,220 IAH-qualifying Medicare beneficiaries | 31.1% | 100% | Potential additional savings from avoiding LTI funded by Medicaid |
|
| Norman et al.23 | Survey to describe how nonmedical social needs of homebound older adults are assessed and addressed within HBPC practices, and identify barriers to coordinating HCBS for patients | AAHCM members (101 practices) | 26% of practices had >50% dual eligibles. Most common payment method for HCBS was Medicaid (40%) | NA | Barriers associated with HCBS coordination |
|
| Left et al.24 | Retrospective chart review to determine the prevalence, effectiveness, and predictors of planning the place of death | 125 homebound adults, patients of Baltimore-based HBPC practice | 3.2% Medicaid only; 11.2% dual eligible | 27.2% Medicare only; 11.2% dual eligible; 58.4% Medicare and private insurance | Presence of a plan to die in a specific place and concordance between planned and actual place of death |
|
| Klein et al25 | Expert perspectives using six case studies to describe effect of HBPC on outcomes and costs for Medicare and Medicaid beneficiaries with complex care needs | 6 HBPC practices (7–37,000 patients per practice) | 15–50% dual eligible | 100% | Optimized care processes and cost savings of home-based care models |
|
Abbreviations: AAHCM, American Academy of Home Care Medicine; CMS, Centers for Medicare & Medicaid Services; FFS, fee for service; HBPC, home-based primary care; HCBS, home- and community-based services; IAH, Independence At Home; LTI, long-term institutionalization; NA, not applicable; NP, nurse practitioner; PCP, primary care provider; QI, quality improvement.
Three studies of HBPC reported the proportion of patients in their study population that were Medicaid beneficiaries. In a case-control study, DeJonge and colleagues examined the effects of HBPC on Medicare cost and found that costs were 17% lower for HBPC patients, compared with controls; 36% of the study population were on Medicaid (mostly dual eligible).19 In a retrospective cross-sectional study of one HBPC practice, Kronish et al. found that increasing age was associated with less medication use; 64% of the patients in this study were Medicaid beneficiaries.20 In a retrospective chart review of 125 patients receiving HBMC, Leff et al. reviewed the charts of 125 patients (11.2% dually eligible) and found that 91% of those who made a plan to die in a specific place had that plan successfully executed.24 These studies provide signals that Medicaid beneficiaries are cared for in HBMCs, but considerable variability exists in the proportion of Medicaid beneficiaries served.
In a Commonwealth Fund Issue Brief, Klein and coauthors presented a qualitative synthesis of learnings from the field in the literature on HBPC.25 Dual-eligible beneficiaries accounted for 15% to 50% of practice panels of the six programs examined. Two practices served predominantly Black populations, and most practices had large populations of people with cognitive impairment.
A policy-focused article made projections of potential savings for the CMS through Medicare and Medicaid if the Independence at Home was converted to a national program.22 The study presumed a 31% Medicaid prevalence in the population, and projected total savings ranged from $12 to $53 billion.
HBMC Studies Reporting Outcome by Medicaid Status
Given the growing number of HBMC practices and of Medicare Advantage programs considering community-based interventions, we also sought to understand whether Medicaid status influenced outcomes in studies evaluating HBMC programs. Table 3 lists data extracted from two studies of HBPC that reported an outcome by Medicaid status. Kronhaus et al.26 studied the prevalence of dementia and prescribing patterns of patients in assisted living.
Table 3.
Studies of HBPC Reporting an Outcome by Medicaid Status
| Study | Study design/Aim | Population studied | Mean age, y | % Medicaid | Outcomes assessed | Key findings |
|---|---|---|---|---|---|---|
| Kronhaus et al.26 | Retrospective chart review to describe prevalence of dementia and prescribing patterns in ALRs | 3,175 ALR residents receiving HBPC in one state | 71.5 without dementia; 83.6 with dementia | 62% patients without dementia; 27.5% patients with dementia | Alzheimer medication use; antipsychotic medication use; other medication prescribing patterns |
|
| Prioleau et al.27 | Retrospective chart review to identify factors associated with place of death of patients in the Mount Sinai Visiting Doctors Program | 183 patients of New York–based HBPC practice | 47% aged ≥90 | 55.7% | Place of death (in or out of hospital) |
|
Abbreviations: ALR, assisted living residence; HBPC, home-based primary care.
Residents of assisted living facilities (ALFs) in one southeastern state were cared for through HBPC.26 Dementia medications were more likely to be prescribed to patients with dementia living in ALFs that had a memory care unit and also to patients who were not Medicaid beneficiaries. Prioleau et al. examined factors associated with death in the Mount Sinai Visiting Doctors Program and found that being White, aged 90 and older, non-Medicaid, or having recorded a preference for a nonhospital death increased the chance of death at home.27
DISCUSSION
This systematic review found 16 studies relevant to the use of HBMC among Medicaid beneficiaries. The studies suggest that at the practice level, the proportion of Medicaid patients served by HBMC varies from 26% to 64%. Although the populations served by HBMC practices include meaningful proportions of Medicaid beneficiaries, few publications described HBMC as an integral care delivery model for state or regional Medicaid programs. Three programs stand out: the Commonwealth Care Alliance and the CMA, in Boston, and VNSNY CHOICE, in New York State. Common components of these HBMC practices include the substantive involvement of NPs, the use of intensive case management, 24/7 availability, and the importance of primary care providers as part of the continuum of care. Data from these programs suggest that the use of HBMC for Medicaid beneficiaries can reduce healthcare costs.
This comprehensive review of peer-reviewed and gray literature on HBMC in Medicaid-eligible populations demonstrates a relative dearth of literature regarding the use and impact of HBMC in the Medicaid population. The reason for the scarcity of published data may relate to the divide between the Medicare and Medicaid programs and the associated divide between medical care and social care in the form of Medicaid HCBS. Most of the literature on Medicaid-supported home-based care focuses on HCBS rather than HBMC. HCBS tends to exist in parallel with HBPC (as with other medical services such as typical ambulatory-based primary care), rather than being integrated with HBPC. Further, although PACE models were specifically created for dually eligible beneficiaries, PACE programs are only available to 51,000 people in 31 states and require specific waivers.28
Available evidence suggests that HBMC warrants strong consideration by Medicaid programs, given its positive impact on person- and system-level outcomes. Studies of HBPC programs have demonstrated substantial reductions in ED visits, hospitalizations, hospital bed days, long-term-care admissions, long-term-care bed days, and costs of care; satisfaction and caregiver quality of life were better in HBPC than in usual care.2 An Agency for Healthcare Research and Quality (AHRQ) Comparative Effectiveness Review also found that “current research evidence is generally positive, providing moderate-strength evidence that HBPC reduces use of inpatient care.”29 The Veterans Affairs’ HBPC programs demonstrated approximately lower costs of care for both the Veterans Affairs health system and the Medicare program, without cost shifting.30
Recent trends suggest interest in the development and deployment of care delivery models that combine or integrate medical and social constructs, especially in the context of Medicaid managed care and special needs plans focused on dual-eligible beneficiaries. These models involve a growing number of for-profit organizations throughout the country. Researchers should collaborate with some of these innovative health service delivery entities that provide HBMC to Medicaid beneficiaries. State Medicaid agencies would benefit from a more detailed understanding of the services and supports provided to the Medicaid populations served by these companies. Understanding whether any of these programs care for pure Medicaid patients or whether all are aimed at dual-eligible populations will offer future insights as to why straight Medicaid patients are or are not able to receive HBMC. Underlying all of these questions for private entities is the approach to solvency and sustainability and whether they offer lessons for others interested in providing HBMC to Medicaid populations.
This review raises several important questions for how the Medicaid program might more effectively leverage HBMC to improve outcomes for their beneficiaries. How can state Medicaid programs promote the adoption or implementation of evidence-based models such as HBMC at scale? What are the best approaches to integrate and synergize HBMC with HCBS? What are the Medicaid-specific barriers to integrating HCBS with HBMC, and how can these be overcome? The Valluru et al. study included in this review suggests the potential for substantial reduction in LTI rates and more time in community when HCBS are integrated with HBMC. Evaluations of this type of care delivery model in Medicaid programs could guide state Medicaid programs in the future.
This review has several limitations. First, the literature on HBMC specifically for Medicaid beneficiaries is not robust, and the studies were mostly of Medicare beneficiaries that also cared for dual-eligible beneficiaries, making it difficult to understand model types that might be especially beneficial for Medicaid beneficiaries. Second, we were unable to assess which state Medicaid programs, if any, were testing HBMC nor what types of models they are testing. Future work could explore this through the use of Medicaid data made available for research through organizations such as the Research Data Assistance Center (ResDAC). Third, given that the studies identified were not clinical trials and did not define outcomes similarly, no results could be combined and no conclusions could be made about differences or similarities in outcomes. In general, none of these studies met criteria for a high-quality clinical trial, and only three had comparison groups. Finally, this review gathered available data but was unable to assess the current prevalence of HBMC in Medicaid.
In summary, HBMC has demonstrated positive impact on high-risk, high-cost populations. Studies to date suggest potential synergies between HBPC programs and HCBS; however, the quality of studies to date is poor, and it is unclear what components of HBPC or HCBS are most effective at improving patient outcomes. Creative integration between HBPC models and social care models for Medicaid beneficiaries is ripe for future testing and likely will be needed as Medicaid expands and our population ages.
ACKNOWLEDGMENTS
Financial Disclosure:
This work was supported by a grant from the California Healthcare Foundation.
Footnotes
Conflict of Interest: Bruce Leff is past president and former member of the board of directors of the American Academy of Home Care Medicine. The other authors have declared no conflicts of interest for this article.
REFERENCES
- 1.Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175(7):1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc. 2014;62(12):2243–2251. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Independence at home demonstration. https://innovation.cms.gov/innovation-models/independence-at-home. Accessed November 11, 2019.
- 4.Yao N, Ritchie C, Camacho F, Leff B. Geographic concentration of home-based medical care providers. Health Aff. 2016;35(8):1404–1409. [DOI] [PubMed] [Google Scholar]
- 5.Thompson FJ, Cantor JC, Farnham J. Medicaid long-term care: state variation and the intergovernmental lobby. J Health Polit Policy Law. 2016;41(4): 763–780. [DOI] [PubMed] [Google Scholar]
- 6.Snyder L Rudowitz R. Trends in state Medicaid programs: Looking back and looking ahead. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/trends-in-state-medicaid-programs-looking-back-and-looking-ahead/. Accessed November 11, 2019. [Google Scholar]
- 7.Beales JL, Edes T. Veteran’s affairs home based primary care. Clin Geriatr Med. 2009;25(1):149–154. viii–ix. [DOI] [PubMed] [Google Scholar]
- 8.Szanton SL, Wolff JW, Leff B, et al. CAPABLE trial: a randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: rationale and design. Contemp Clin Trials. 2014;38(1): 102–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen KR, Hazelett SE, Radwany S, Ertle D, Fosnight SM, Moore PS. The Promoting Effective Advance Care for Elders (PEACE) randomized pilot study: theoretical framework and study design. Popul Health Manag. 2012; 15(2):71–77. [DOI] [PubMed] [Google Scholar]
- 10.Hirth V, Baskins J, Dever-Bumba M. Program of all-inclusive care (PACE): past, present, and future. J Am Med Dir Assoc. 2009;10(3):155–160. [DOI] [PubMed] [Google Scholar]
- 11.Master RJ. Massachusetts Medicaid and the Community Medical Alliance: a new approach to contracting and care delivery for Medicaid-eligible populations with AIDS and severe physical disability. Am J Manag Care. 1998;4(suppl):SP90–SP98. [PubMed] [Google Scholar]
- 12.Fisher HM, Raphael TG. Managed long-term care: care integration through care coordination. J Aging Health. 2003;15(1):223–245. [DOI] [PubMed] [Google Scholar]
- 13.Meyer H A new care paradigm slashes hospital use and nursing home stays for the elderly and the physically and mentally disabled. Health Aff. 2011; 30(3):412–415. [DOI] [PubMed] [Google Scholar]
- 14.Trilla F, DeCastro T, Harrison N, et al. Nurse practitioner home-based primary care program improves patient outcomes. J Nurse Pract. 2018;14(9): E185–E188. [Google Scholar]
- 15.Valluru G, Yudin J, Patterson CL, et al. Integrated home- and community-based services improve community survival among Independence at home Medicare beneficiaries without increasing Medicaid costs. J Am Geriatr Soc. 2019;67(7):1495–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davis K, Willink A, Schoen C. Integrated care organizations: Medicare financing for care at home. Am J Manag Care. 2016;22(11):764–768. [PubMed] [Google Scholar]
- 17.Islam MM, Iqbal U, Walther B, et al. Benzodiazepine use and risk of dementia in the elderly population: a systematic review and meta-analysis. Neuroepidemiology. 2016;47(3–4):181–191. [DOI] [PubMed] [Google Scholar]
- 18.Landers SH, Gunn PW, Stange KC. An emerging model of primary care for older adults: the house call-home care practice. Care Manag J. 2009;10(3):110–114. [DOI] [PubMed] [Google Scholar]
- 19.De Jonge KE, Jamshed N, Gilden D, Kubisiak J, Bruce SR, Taler G. Effects of home-based primary care on Medicare costs in high-risk elders. J Am Geriatr Soc. 2014;62(10):1825–1831. [DOI] [PubMed] [Google Scholar]
- 20.Kronish IM, Federman AD, Morrison RS, Boal J. Medication utilization in an urban homebound population. J Gerontol A Biol Sci Med Sci. 2006; 61(4):411–415. [DOI] [PubMed] [Google Scholar]
- 21.Leff B, Weston CM, Garrigues S, Patel K, Ritchie C, the National Home-Based Primary Care and Palliative Care Network. Home-based primary care practices in the United States: current state and quality improvement approaches. J Am Geriatr Soc. 2015;63(5):963–969. [DOI] [PubMed] [Google Scholar]
- 22.Kinosian B, Taler G, Boling P, Gilden D. Independence at Home Learning Collaborative Writing Group. Projected savings and workforce transformation from converting Independence at home to a Medicare benefit. J Am Geriatr Soc. 2016;64(8):1531–1536. [DOI] [PubMed] [Google Scholar]
- 23.Norman GJ, Wade AJ, Morris AM, Slaboda JC. Home and community-based services coordination for homebound older adults in home-based primary care. BMC Geriatr. 2018;18(1):241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leff B, Kaffenbarger KP, Remsburg R. Prevalence, effectiveness, and predictors of planning the place of death among older persons followed in community-based long term care. J Am Geriatr Soc. 2000;48(8):943–948. [DOI] [PubMed] [Google Scholar]
- 25.Klein S, Hostetter M, McCarthy D. An overview of home-based primary care: learning from the field. Issue Brief (Commonw Fund). 2017;15:1–20. [PubMed] [Google Scholar]
- 26.Kronhaus A, Fuller S, Zimmerman S, Prevalence RD. medication management of dementia by a medical practice providing onsite care in assisted living. J Am Med Direct Assoc. 2016;17(7):673.e9–673.e15. [DOI] [PubMed] [Google Scholar]
- 27.Prioleau PG, Soones TN, Ornstein K, Zhang M, Smith CB, Wajnberg A. Predictors of place of death of individuals in a home-based primary and palliative care program. J Am Geriatr Soc. 2016;64(11):2317–2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National PACE Association. PACEFinder: Find a PACE program in your neighbohood. https://www.npaonline.org/pace-you/pacefinder-find-pace-program-your-neighborhood. Accessed May 20, 2020.
- 29.Totten AM, White-Chu EF, Wasson N, et al. Home-Based Primary Care Interventions. Comparative Effectiveness Reviews No. 164. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [PubMed] [Google Scholar]
- 30.Edes T, Kinosian B, Vuckovic NH, Nichols LO, Becker MM, Hossain M. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc. 2014;62(10):1954–1961. [DOI] [PubMed] [Google Scholar]


