ABSTRACT
Endoscopic retrograde cholangiopancreatography–guided transpapillary gallbladder drainage has emerged as an effective alternative for management of acute cholecystitis in nonoperable candidates. Delayed acute pancreatitis has not been previously described as an adverse event with this procedure. In this article, we describe 3 patients who developed acute pancreatitis between 2 and 6 weeks after stent insertion with no alternative inciting cause. Delayed acute pancreatitis may represent a rare and previously uncharacterized adverse event related to transpapillary gallbladder drainage.
KEYWORDS: pancreatitis, cholecystitis, ERCP-guided transpapillary gallbladder drainage
INTRODUCTION
Cholecystectomy is the gold standard for treatment of acute cholecystitis (AC).1 Endoscopic retrograde cholangiopancreatography (ERCP)-guided transpapillary gallbladder drainage (ET-GBD) is an effective technique to manage AC in patients who are poor operative candidates. Although it has been postulated that transpapillary stents might lead to delayed pancreatitis because of common bile duct (CBD) obstruction,2 this has not been reported as an adverse event of the procedure. In this study, we report 3 cases of delayed acute pancreatitis (AP) associated with ET-GBD.
METHODS
A search of the electronic medical record at Mayo Clinic was performed to identify patients with the International Classification of Diseases, Tenth Revision (ICD-10) codes for “pancreatitis” and “cholecystitis” along with the text entry of “transcystic” or “transpapillary” in either endoscopy procedure notes or clinical documentation. Patients were included in the study if they underwent ET-GBD and developed AP greater than 48 hours after the procedure with a transpapillary double-pigtail plastic stent (DPPS) in situ without a clear alternate cause of AP. Three patients met the inclusion criteria. The study was approved by the Mayo Clinic Rochester Institutional Review Board (IRB number 23-001960).
CASE 1
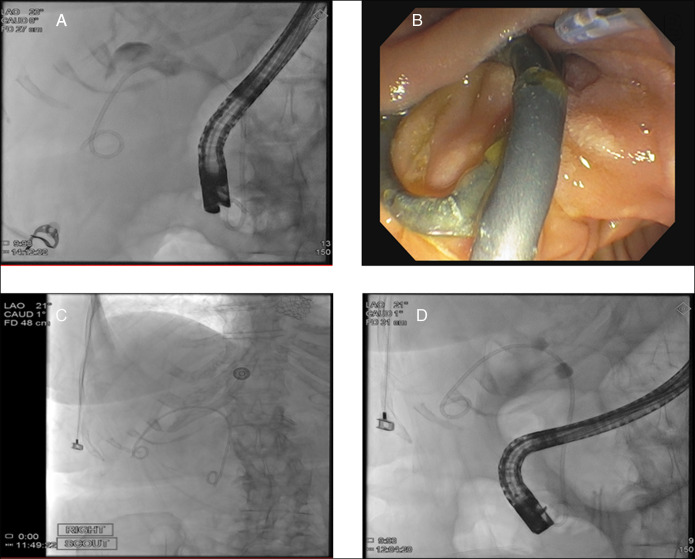
An 88-year-old woman with aortic stenosis underwent ET-GBD for AC. A sphincterotomy was performed along with a full cholangiogram showing brisk flow of contrast through the entire biliary tree followed by placement of a 7-French (Fr)-by-15-cm transpapillary DPPS into the gallbladder (Figure 1). Six weeks later, she developed sudden onset epigastric pain. Laboratory test results showed a lipase >3,000 U/L (normal range 13–60 U/L). Abdominal computed tomography (CT) scan showed edema in the pancreatic-duodenal groove, acute on chronic cholecystitis, as well as new moderate intrahepatic bile duct dilation and hyperenhancement. A repeat ERCP was performed, which noted a visibly occluded DPPS emerging from the ampulla (Figure 1) in appropriate position (Figure 1). The stent was removed, biliary tree was swept with a small amount of sludge seen, and a 7-Fr-by-15-cm DPPS was placed into the gallbladder with good bile flow noted endoscopically (Figure 1). Two weeks later, the patient had another episode of epigastric pain with a lipase >3,000 U/L (normal range 13–60 U/L). CT scan showed persistent peripancreatic edema and bile duct dilation. A percutaneous cholecystostomy tube was placed, which was complicated by a cholecystocolonic fistula. She was discharged to hospice and died shortly after.
Figure 1.
Case 1 fluoroscopy and endoscopy images. (A) Fluoroscopy image after initial ERCP-guided transpapillary gallbladder drainage. (B) Photograph of occluded transpapillary stent during second ERCP. (C) Scout image before second ERCP showing appropriate placement of initial transpapillary stent. (D) Fluoroscopy image after second ERCP confirming appropriate placement of transpapillary stent. ERCP, endoscopic retrograde cholangiopancreatography.
CASE 2
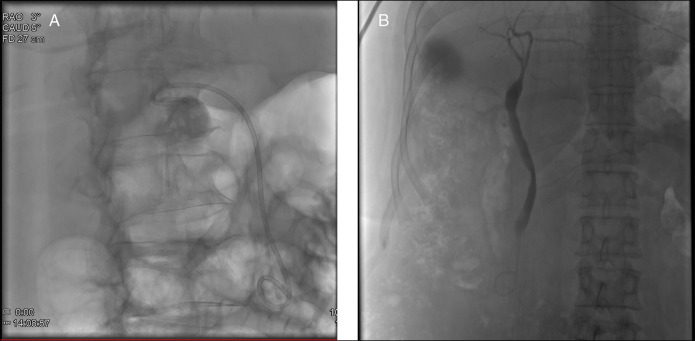
A 62-year-old woman with a history of cryptogenic cirrhosis complicated by esophageal varices underwent ET-GBD as destination therapy for AC. Three years later, she was found to have gallbladder dilation on ultrasonography performed to screen for hepatocellular carcinoma, despite the transpapillary stent being in appropriate position. Repeat ET-GBD was performed with a replacement 5-Fr-by-12-cm transpapillary DPPS inserted into the gallbladder in appropriate position (Figure 2). Thirteen days later, she presented with sudden-onset epigastric pain. CT scan showed fat stranding around the pancreatic head and mild chronic intrahepatic bile duct dilation. She was managed with intravenous hydration and discharged in stable condition.
Figure 2.
(A) Case 2 fluoroscopy image following second ET-GBD with replacement of blocked stent showing appropriate stent placement. (B) Case 3 fluoroscopy following ET-GBD showing appropriate positioning of transpapillary plastic stent.
CASE 3
A 64-year-old woman with rheumatic heart disease and mechanical aortic, tricuspid, and mitral valves was admitted with gallstone AP. ET-GBD was performed for prevention of cholecystitis, given poor operative candidacy. The pancreatic duct was stented. A sphincterotomy was performed, and a 7-Fr-by-10-cm plastic DPPS was placed into the gallbladder (Figure 2). Three weeks later, she returned to hospital with severe epigastric pain. Abdominal CT scan showed interstitial edematous pancreatitis and mild diffuse intrahepatic bile duct dilation. Lipase was elevated at 293 U/L (normal range 13–60 U/L). An open cholecystectomy was performed with removal of the transpapillary stent. She had no further episodes of AP.
DISCUSSION
In this article, we describe 3 cases of patients with delayed AP occurring between 2 and 6 weeks after ET-GBD. All 3 patients were female and older than 60 years at the time of AP. They were all former smokers; however, all had quit greater than 1 year before AP. All patients denied alcohol use, and triglycerides drawn around the time of AP were not significantly elevated. With the exception of case 3's index presentation of gallstone AP, none of the patients developed AP before ET-GBD or after stent removal. Apart from mildly elevated ALP, there were no acute derangement of liver enzymes at the time of presentation with AP. ET-GBD was performed without procedural complications in all cases.
There has been 1 case of late AP after ET-GBD reported previously. A patient developed AP 6 months after ET-GBD for AC after the transpapillary stent migrated distally and became fixed to the superior portion of the duodenum, thereby obstructing the pancreatic duct.3 Other than this report, delayed AP after ET-GBD has not been described previously. A cohort study following 158 patients for a mean duration of 3 years after ET-GBD found 9 cases of post-ERCP pancreatitis but no delayed AP.4 Another study following 51 patients for an average of 453 days found no cases of delayed AP after ET-GBD.5
With respect to possible causes, each case of AP in our study had their stents remain in appropriate position, suggesting an alternate mechanism to that described by Yane et al.3 Previous research has proposed that a larger-diameter plastic stent for ET-GBD might occlude the ampulla of Vater and predispose to AP.2 Although the transpapillary stents in our cases varied in diameter (ranging from 5 to 7 French), all patients showed biliary duct dilation on CT scans. Plastic stents used for ET-GBD primarily serve gallbladder drainage rather than relief of CBD obstruction. Despite having side-holes, these stents can lead to partial obstruction and sludge formation, potentially contributing to AP as a result. In addition, long-term transpapillary plastic stents may result in periampullary inflammation, leading to pancreatic duct obstruction and subsequent AP. Pancreatitis has been identified as an adverse event associated with CBD stent insertion for other indications. For malignant CBD obstruction, AP has been reported in 6% of cases after self-expanding metal stent insertion, likely because of increased axial force placed on the pancreatic duct from the stent.6 Plastic stents inserted into the CBD for malignant obstruction have also been associated with AP in 2.4% of cases,7 rising to 5.3% in stents retained greater than 1 year.8 Although the exact mechanism of AP remains unclear, the association with cholangitis in most cases8 suggests a contribution from biliary obstruction. Consequently, the mechanism contributing to AP in our cases may be similar.
Ultimately, the true incidence of delayed AP after ET-GBD remains unknown because most stents are routinely exchanged at predetermined intervals. Further studies are necessary to determine the precise mechanism and true incidence of the condition.
In summary, delayed AP after ET-GBD is a rare and previously unrecognized postprocedural adverse event. Further studies to identify the risk factors and outcomes of delayed ET-GBD are needed.
DISCLOSURES
Author contributions: ML Vincent: conceptualization, methodology, investigation, and writing (original draft). M. Aggarwal: conceptualization, writing (review and editing), and visualization. V. Chandrasekhara: writing (review and editing) and supervision. DS Pardi: conceptualization, writing (review and editing), supervision, and is the article guarantor. All authors have read the final version of the manuscript and agrees to be accountable for its accuracy and integrity.
Financial disclosure: V. Chandrasekhara is a consultant for Covidien LP and Boston Scientific and is a shareholder in Nevakar corporation. All other authors declare no conflicts of interest.
Previous presentation: The manuscript was presented at the 2023 American College of Gastroenterology Annual Meeting & Postgraduate Course; October 20–25, 2023; Vancouver, British Columba, Canada.
Informed consent was obtained for this case report.
Contributor Information
Manik Aggarwal, Email: aggarwal.manik@mayo.edu.
Vinay Chandrasekhara, Email: chandrasekhara.vinay@mayo.edu.
Darrell S. Pardi, Email: pardi.darrell@mayo.edu.
REFERENCES
- 1.Miura F, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: Initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci. 2018;25(1):31–40. [DOI] [PubMed] [Google Scholar]
- 2.Itoi T, Sofuni A, Itokawa F, et al. Endoscopic transpapillary gallbladder drainage in patients with acute cholecystitis in whom percutaneous transhepatic approach is contraindicated or anatomically impossible (with video). Gastrointest Endosc. 2008;68(3):455–60. [DOI] [PubMed] [Google Scholar]
- 3.Yane K, Katanuma A, Maguchi H. Late onset pancreatitis 6 months after endoscopic transpapillary gallbladder stenting for acute cholecystitis. Dig Endosc. 2014;26(3):494–5. [DOI] [PubMed] [Google Scholar]
- 4.Maruta A, Iwashita T, Iwata K, et al. Permanent endoscopic gallbladder stenting versus removal of gallbladder drainage, long-term outcomes after management of acute cholecystitis in high-risk surgical patients for cholecystectomy: Multi-center retrospective cohort study. J Hepatobiliary Pancreat Sci. 2021;28(12):1138–46. [DOI] [PubMed] [Google Scholar]
- 5.Storm AC, Vargas EJ, Chin JY, et al. Transpapillary gallbladder stent placement for long-term therapy of acute cholecystitis. Gastrointest Endosc. 2021;94(4):742–8.e1. [DOI] [PubMed] [Google Scholar]
- 6.Kawakubo K, Isayama H, Nakai Y, et al. Risk factors for pancreatitis following transpapillary self-expandable metal stent placement. Surg Endosc. 2012;26(3):771–6. [DOI] [PubMed] [Google Scholar]
- 7.Moses PL, Alnaamani KM, Barkun AN, et al. Randomized trial in malignant biliary obstruction: Plastic vs partially covered metal stents. World J Gastroenterol. 2013;19(46):8638–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sohn SH, Park JH, Kim KH, et al. Complications and management of forgotten long-term biliary stents. World J Gastroenterol. 2017;23(4):622–8. [DOI] [PMC free article] [PubMed] [Google Scholar]