Abstract
Geographic variation in hardship, especially health-related hardship, was identified prior to and during the pandemic, but we do not know whether this variation is consistent among Veterans Health Administration (VHA)–enrolled veterans, who reported markedly high rates of financial hardship during the pandemic, despite general and veteran-specific federal policy efforts aimed at reducing hardship. In a nationwide, regionally stratified sample of VHA-enrolled veterans, we examined whether the prevalence of financial hardship during the pandemic varied by US Census region. We found veterans in the South, compared with those in other census regions, reported higher rates of severe-to-extreme financial strain, using up all or most of their savings, being unable to pay for necessities, being contacted by collections, and changing their employment due to the kind of work they could perform. Regional variation in veteran financial hardship demonstrates a need for further research about the role and interaction of federal and state financial-assistance policies in shaping risks for financial hardship as well as potential opportunities to mitigate risks among veterans and reduce variation across regions.
Keywords: financial hardship, veterans, census region, ADI, employment, COVID-19
Introduction
Many US veterans faced significant financial and material hardship1-4 prior to the COVID-19 pandemic, and veterans, regardless of infection status, also reported high rates of financial hardship5-7 during the pandemic. Numerous state and federal policies were enacted during the pandemic, such as expanded unemployment insurance, eviction moratoriums, restrictions on cost-sharing for COVID-19–related care, expanded child tax credits, economic impact payments, and paid medical and family leave.8,9 While some of these were shown to significantly reduce poverty and material hardship,10-13 and benefit veterans specifically,14 these programs varied across the country and largely expired when the COVID-19 national emergency declaration was withdrawn. Since government COVID-19–specific assistance has ended, evidence shows that material hardship is on the rise.15
There is also evidence of persistent regional variation in financial hardship, particularly health-related financial hardships, including during the COVID-19 pandemic.16-21 Geographic variation in financial and material hardship is also evident among veterans,2,22-24 with much of this literature focusing predominantly on food insecurity and homelessness. However, studies have yet to explore geographic variation in pandemic financial hardship among veterans, which may offer insight into the high rates of veteran-reported hardship and possible targets for intervention. We undertook the current study to examine geographic variation in pandemic-related financial hardship among VHA-enrolled veterans.
Data and methods
Study design and population
We conducted a cross-sectional survey to assess geographic variation in pandemic-related financial hardship among Veterans Health Administration (VHA)–enrolled veterans. As previously described, survey participants were sampled from an existing electronic health record–based cohort of VHA enrollees that was assembled and designed to assess the effect of COVID-19 on a broad range of long-term outcomes.25 The initial cohort included all VHA enrollees with a first SARS-CoV-2 infection between March 1, 2020, and April 30, 2021.
We used a stratified random-sampling scheme (stratified by month, census region, and COVID-19 hospitalization) to select, from the initial cohort, 600 veterans infected with COVID-19 between October–December 2020 and February–April 2021 (100 from each month).25 Surveys were completed 1.5 years after each veteran's initial infection date. After the sampled veterans with COVID-19 completed the survey, we invited up to 5 matched uninfected comparators to participate and complete surveys. Only veterans who were alive and residing in the United States at the time of survey initiation were eligible to participate. The survey instrument and study methods were approved by the Department of Veterans Affairs (VA) Institutional Review Board and all veterans provided verbal informed consent to participate. All participants were compensated $10 for their time. The survey did not include reference to infection or COVID-19 status so the same survey could be used for all participants regardless of COVID-19 status.
Measures
Financial hardship
The survey was designed to assess multiple post–COVID-19 outcomes, including financial hardship, measured using 10 items. The questions included 1 Likert scale question about perceived health-related financial strain26 and 9 indicator questions (yes/no) measuring specific financial hardships.27,28 Specifically, veterans were asked if they skipped or delayed needed medical care due to costs; took less prescribed medication due to costs; used up most or all savings; were contacted by collections; declared bankruptcy; were unable to pay for necessities like food, heat, or housing; lost a job; had to change the kind of work they could do; or had a loved one take time off work to care for them. We prefaced each question with “since the beginning of 2020” to capture the participant's experience of financial hardship during the pandemic. We report on all of these questions, as well as 1 composite outcome reporting any overall financial hardship (answering yes to any of the financial hardship indicators or reporting “severe” or “extreme” health-related financial strain).
Census region
Census region29 was our primary independent variables. We collected information on each participant's residential census region (Northeast, South, Midwest, and West) from the VHA's Corporate Data Warehouse.30
Statistical analyses
We applied survey sampling and nonresponse weights to all analyses to weight all measures to represent veterans in the parent cohort from which our study was sampled. We then fit survey-weighted logistic regression models with census region as the independent variable to assess their association with each financial hardship outcome (dependent variables). Region was modeled as a 4-level categorical variable with South as the reference region. We adjusted for participant age (years, continuous), sex, race, ethnicity, distance to nearest VA medical center (miles, continuous), and census block–level Area Deprivation Index (ADI)31 (continuous) and Gagne comorbidity index, which combines conditions in the Charlson and Elixhauser scales.32
Fitted models were used to estimate unadjusted and adjusted predicted probability and CIs of each outcome for comparison across region. Adjusted probabilities were standardized (ie, marginalized) to the sample distribution of covariates. To assess regional differences in the probability of each financial hardship outcome, we estimated average marginal effects with the South region as the reference.18 Average marginal effects with P values < .05 were considered statistically significant. All analyses were conducted in R (version 4.3.1; R Foundation for Statistical Computing, Vienna, Austria); marginal effects and probabilities were estimated using the “marginaleffects” package (version 0.16).
Results
Participant characteristics
Among the 600 veterans with COVID-19 sampled and invited to participate in the survey, 548 were alive and living in the United States; 194 (35.4%) completed surveys along with 194 of their matched comparators for a total analytic sample of 388. The survey sample was predominantly male (90.8%), non-Hispanic (91.4%), White (68.1%), and urban (67.5%), with a mean age of 60.9 years (SD = 13.8) (see Table S1). Most surveyed veterans were from the South census region (42.3%), followed by the Midwest (23.3%), West (19.8%), and Northeast (14.5%). In general, veterans’ demographic and health characteristics were consistent across census region, although we observed some variation in race and ethnicity.
Census region
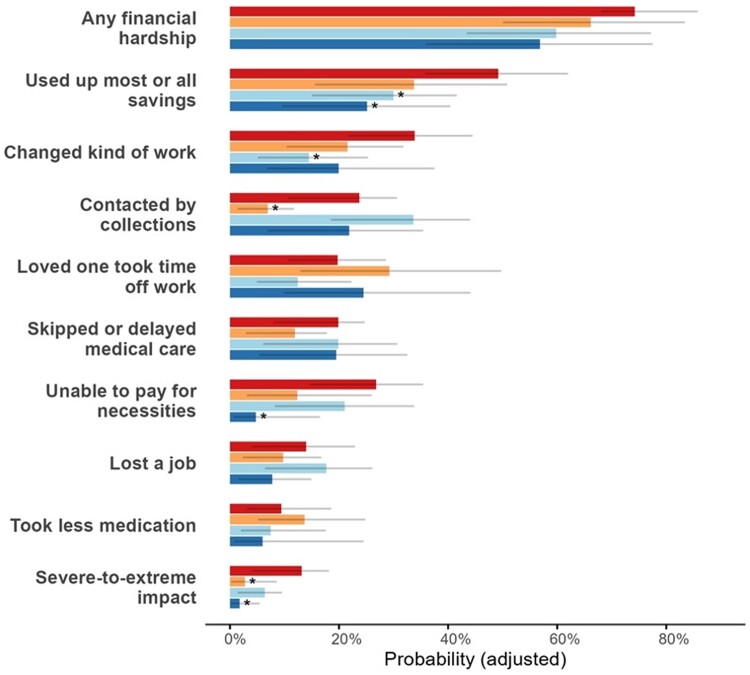
In unadjusted (see Table 1) and adjusted (see Figure 1, Table S2) analyses, veterans in the South had a significantly higher probability of experiencing 5 financial hardship outcomes than those in other regions. In unadjusted analyses, a significantly greater proportion of veterans in the South reported severe-to-extreme financial strain compared with veterans in the West and Northeast (Table S3); these differences remained significant in the adjusted analyses (South, 13.1%, 95% CI: 4.0%–18.14%; West, 2.7%, 95% CI: 0.2%–8.6%; and Northeast, 1.8%, 95% CI: 0.1%–5.4%).
Table 1.
Unadjusted probabilities of financial hardship outcomes overall by US Census region.
| Outcome | Unadjusted probability, % (95% CI) | ||||
|---|---|---|---|---|---|
| Overall | Census region | ||||
| South | Midwest | West | Northeast | ||
| Any financial hardship | 66.79 (59.34, 73.49) | 76.77 (66.62, 84.55) | 64.05 (49.69, 76.27) | 55.95 (39.01, 71.61) | 56.81 (34.56, 76.61) |
| Severe-to-extreme financial strain | 7.86 (4.85, 12.51) | 13.24 (7.17, 23.18) | 6.32 (2.55, 14.83) | 2.50 (0.78, 7.75) | 1.93 (0.41, 8.58) |
| Skipped or delayed medical care | 18.12 (13.06, 24.59) | 19.39 (11.84, 30.11) | 18.09 (8.57, 34.24) | 15.11 (7.03, 29.54) | 18.56 (7.97, 37.50) |
| Took less medication | 9.20 (5.67, 14.61) | 10.21 (4.99, 19.75) | 8.84 (3.03, 23.13) | 11.06 (4.19, 26.10) | 4.34 (0.66, 23.56) |
| Used up most or all savings | 38.27 (31.10, 45.98) | 52.14 (40.60, 63.45) | 33.49 (20.65, 49.34) | 24.49 (12.92, 41.49) | 24.19 (11.46, 44.02) |
| Contacted by collections | 22.81 (17.10, 29.76) | 25.28 (16.40, 36.86) | 32.89 (20.04, 48.95) | 6.11 (2.84, 12.64) | 22.08 (10.31, 41.13) |
| Declared bankruptcy | 2.22 (0.91, 5.27) | 4.11 (1.41, 11.40) | 1.04 (0.14, 7.11) | 1.16 (0.23, 5.58) | 0.00 (0.00, 0.00) |
| Unable to pay for necessities | 19.01 (13.50, 26.11) | 27.40 (17.47, 40.22) | 17.70 (9.23, 31.27) | 12.34 (5.01, 27.33) | 5.73 (1.26, 22.43) |
| Lost a job | 12.98 (8.58, 19.17) | 13.95 (7.30, 25.04) | 16.79 (7.49, 33.47) | 9.90 (4.35, 20.97) | 8.20 (2.52, 23.58) |
| Changed kind of work | 24.97 (19.05, 32.00) | 35.24 (24.76, 47.36) | 15.51 (7.31, 29.93) | 16.44 (9.44, 27.09) | 21.79 (9.90, 41.38) |
| Loved one took time off work | 20.28 (14.90, 26.99) | 20.31 (12.48, 31.29) | 13.62 (6.90, 25.13) | 24.80 (12.99, 42.15) | 24.78 (10.93, 46.94) |
Figure 1.
Adjusted probabilities of financial hardship outcomes by US Census region (included in Table S2). Census regions are represented by horizontal bars next to each outcome, from top to bottom (South, West, Midwest, Northeast) and by the following colors: red = South; orange = West; light blue = Midwest; dark blue = Northeast. Predicted probabilities are adjusted for age, sex, race/ethnicity, Gagne comorbidity index, distance to VA medical center; and ADI. *P ≤ .05 (compared with South region); based on z-test of average marginal effect. Abbreviations: ADI, Area Deprivation Index; VA, Department of Veterans Affairs.
In unadjusted analyses, over half of the veterans in the South reported using up most or all of their savings compared with less than one-quarter of those in the West and Northeast. In adjusted analyses, the probability of using up most or all savings was significantly higher in the South (49.2%, 95% CI: 35.8%–62.0%) than in the Midwest (30.0%, 95% CI: 15.0%–41.6%) and Northeast (25.1%, 95% CI: 9.5%–40.4%) regions.
In unadjusted analyses, veterans in the South were significantly more likely to report the kind of work they could do changed than those in the West and Midwest; differences between the South (33.9%, 95% CI: 21.7%–44.5%) and Midwest (14.5%, 95% CI: 5.1%–25.3%) remained significant after adjustment. In adjusted analyses, veterans in the South had a higher probability of being unable to pay for necessities than those in the Northeast (South, 26.8%, 95% CI: 14.6%–35.4%; Northeast: 4.8%, 95% CI: 0.6%–16.5%), and a higher probability of being contacted by collections than those in the West (South, 23.7%, 95% CI: 10.6%–30.6%; West: 6.9%, 95% CI: 1.4%–11.8%).
Discussion
In our study population, veterans residing in the South had greater risks of experiencing severe-to-extreme financial strain, as well as using up all or most of their savings, being unable to pay for necessities, being contacted by collections, and changing their kind of work. These differences persisted even when controlling for individual demographic characteristics and comorbidities and local social and economic conditions (ADI), suggesting that regional- and perhaps state-level factors and policies may have had a greater impact on pandemic-related hardship than pre-existing local conditions. There are numerous ways in which state-level COVID-19 conditions and policies, often mirrored within regions, varied across the country.8,12
Federal and state policies, aimed at mitigating individual pandemic-related financial hardships,8 as well as unique pandemic-assistance programs available to veterans, including VHA medical debt relief and state-specific emergency funds,33,34 were implemented between 2020 and 2022, and evidence suggests that veterans took advantage of some of these programs at high rates.14 However, the form and duration of assistance programs varied substantially between states.12,16 For example, some states enacted regulations requiring private insurers to waive or limit cost-sharing,35 which has been linked to greater testing, fewer COVID-19 deaths, and increased primary care use during the pandemic.36,37 Individuals in the South, Midwest, and West regions experienced greater out-of-pocket spending for COVID-19 hospitalizations.38 It is possible that regional variation in hardship among veterans reflects these more heterogenous state policies. Further, as most federal and state programs have ended, increases in financial hardship have been noted.15
Prior to and during the pandemic, rates of food insecurity, forgone medical care, and poverty have consistently been higher in the South census region,16-21,39 and while veterans throughout the country generally experience lower rates of poverty than the general public, they are not immune to state and regional variation in these outcomes.23,24 Pre-existing state-specific health care policies and programs (or lack thereof) have been linked to financial hardship,40,41 and may be a source of regional variation in subsequent pandemic- and COVID-19–related financial hardship among veterans. For example, state expansions of Medicaid have been associated with reductions in both nonmedical and medical financial hardship,42 yet many states in the US South have yet to expand Medicaid,43 and veterans, including those with low incomes,44 disproportionately reside in the South.45 Also in the South, half of states lack consumer protections from surprise medical bills.46
We acknowledge several limitations to our data and analyses. We lack information on veterans' individual finances, such as income or wealth, and rely on veteran self-report of financial hardships, rather that direct measures of health care costs. However, our self-reported outcomes center on how veterans experience financial burden and perceive it to impact their economic and health care decisions in varied ways. We also lack pre-pandemic data on hardship and are unable to examine temporal changes in hardship that may be attributable to the pandemic. The ADI and other composite measures of area social and economic conditions have strengths and weaknesses and may be a confounding factor.47-49 Our data are also underpowered to examine differences in financial hardship at the state level or to account for state-level differences in various public benefits.
Our findings demonstrate that some forms of pandemic-related financial hardship among veterans varied considerably across census regions. All of these findings point to the potential power of state-level policies and programs, in addition to VA and related federal programs, to impact veterans’ experiences of health-related financial hardship.44 The implementation of unique veterans’ assistance programs, particularly medical debt relief and state-specific emergency funds,33,34 and state-level variation in access to these programs are an important opportunity to explore possible policy solutions to decrease veterans’ experiences of disaster or pandemic financial hardships. Information on to what extent veterans accessed non-VA state- and federal-assistance programs would also shed light on potential access barriers unique to veterans. Although not specific to a single policy, our findings raise important questions about the role and interaction of federal and state policies in shaping the risk of, and mitigation strategies for, financial hardship among veterans and the general public.
Supplementary Material
Contributor Information
Katrina E Hauschildt, VA Center for Clinical Management Research, Ann Arbor VA, Ann Arbor, MI 48109, United States; Department of Medicine, School of Medicine, Johns Hopkins University, Baltimore, MD 21205, United States.
David P Bui, Center to Improve Veteran Involvement in Care, VA Portland Health Care System, Portland, OR 97239, United States.
Diana J Govier, Center to Improve Veteran Involvement in Care, VA Portland Health Care System, Portland, OR 97239, United States; Oregon Health & Science University—Portland State University School of Public Health, Portland, OR 97201, United States.
Tammy L Eaton, VA Center for Clinical Management Research, Ann Arbor VA, Ann Arbor, MI 48109, United States; University of Michigan Institute for Healthcare Policy & Innovation, Ann Arbor, MI 48109, United States; Division of Hospital Medicine, Department of Internal Medicine, University of Michigan, Ann Arbor, MI 48109, United States.
Elizabeth M Viglianti, VA Center for Clinical Management Research, Ann Arbor VA, Ann Arbor, MI 48109, United States; Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Michigan, Ann Arbor, MI 48109, United States.
Catherine K Ettman, School of Public Health, Johns Hopkins University, Baltimore, MD 21205, United States.
Holly McCready, Center to Improve Veteran Involvement in Care, VA Portland Health Care System, Portland, OR 97239, United States.
Valerie A Smith, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham Veterans Affairs Health Care System, Durham, NC 27705, United States; Department of Medicine, Duke University, Durham, NC 27710, United States; Department of Population Health Sciences, Duke University School of Medicine, Durham, NC 27710, United States.
Ann M O’Hare, Center of Innovation for Veteran-Centered and Value-Driven Care, Veterans Affairs Puget Sound Healthcare System, Seattle, WA 98108, United States; Hospital and Specialty Medicine Service, Veterans Affairs Puget Sound Health Care System, Seattle, WA 98108, United States; Department of Medicine, University of Washington, Seattle, WA 98195, United States.
Thomas F Osborne, VA Palo Alto Healthcare System, Palo Alto, CA 94304, United States; Department of Radiology, Stanford University School of Medicine, Stanford, CA 94305, United States.
Edward J Boyko, Seattle Epidemiologic Research and Information Center, VA Puget Sound Health Care System, Seattle, WA 98108, United States.
George N Ioannou, Center of Innovation for Veteran-Centered and Value-Driven Care, Veterans Affairs Puget Sound Healthcare System, Seattle, WA 98108, United States; Division of Gastroenterology, Department of Medicine, University of Washington, Seattle, WA 98195, United States.
Matthew L Maciejewski, Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), Durham Veterans Affairs Health Care System, Durham, NC 27705, United States; Department of Medicine, Duke University, Durham, NC 27710, United States; Department of Population Health Sciences, Duke University School of Medicine, Durham, NC 27710, United States.
Amy S B Bohnert, VA Center for Clinical Management Research, Ann Arbor VA, Ann Arbor, MI 48109, United States; Department of Anesthesiology, University of Michigan Medical School, Ann Arbor, MI 48109, United States.
Denise M Hynes, Center to Improve Veteran Involvement in Care, VA Portland Health Care System, Portland, OR 97239, United States; College of Health, and Center for Quantitative Life Sciences, Oregon State University, Corvallis, OR 97331, United States; School of Nursing, Oregon Health and Science University, Portland, OR 97201, United States.
Theodore J Iwashyna, VA Center for Clinical Management Research, Ann Arbor VA, Ann Arbor, MI 48109, United States; Department of Medicine, School of Medicine, Johns Hopkins University, Baltimore, MD 21205, United States; School of Public Health, Johns Hopkins University, Baltimore, MD 21205, United States; Department of Medicine, University of Michigan Medical School, Ann Arbor, MI 48109, United States.
for the VA COVID-19 Observational Research Collaboratory (CORC):
Wen Chai, Barrett Bowling, Matthew Maciejewski, James Womer, Theodore Iwashyna, Stacy Anderson, Taylor Bernstein, Aissa Cabrales, Katrina Hauschildt, Andrew Admon, Kaitland Byrd, Jennifer Cano, Jeffrey Curtis, Emily DelMonico, Dana Horowitz, Lee Kamphius, Peggy Korpela, Kyle Kumbier, Kenneth Langa, Hallie Prescott, Marylena Rouse, Sameer Saini, Sarah Seelye, Jeremy Sussman, Natalya Wawrin, Max Monahan, Amy Bohnert, Elizabeth Viglianti, Kathleen Akgun, Mihaela Aslan, Kei-Hoi Cheung, Yuli Li, Pradeep Mutalik, Nallakkandi Rajeevan, Lei Yan, Livia Anderson, Theodore Berkowitz, Joseph Bogdan, Hayden Bosworth, Nathan Boucher, Graham Cummin, Paul Dennis, Breana Floyd, Susan Nicole Hastings, Brystana Kaufman, Cassie Meyer, Amy Miles, Jennifer Naylor, Megan Shepherd-Banigan, Valerie Smith, Battista Smith, Christopher Woods, Aram Dobalian, Matthew Goetz, Kevin Ikuta, Michael Ong, Aasma Shaukat, Lisa Backus, Jacqueline Ferguson, Thomas Osborne, Troy Shahoumian, Zachary Veigulis, Donna Zulman, Kristina Bajema, David Bui, Jason Chen, Diana Govier, Mark Helfand, Alex Hickok, Catherine Hough, Holly McCready, Abby Moss, Summer Newell, Meike Niederhausen, Shannon Nugent, Somnath Saha, Christopher Slatore, Yumie Takata, Alan Teo, Anais Tuepker, Kelly Vranas, Kara Winchell, Denise Hynes, Edward Boyko, David Au, Aaron Baraff, Kristin Berry Wyatt, Joleen Borgerding, Nicholas Burwick, Kristina Crothers, Marie Davis, Jacob Doll, Jason Dominitz, McKenna Eastment, Vincent Fan, Alexandra Fox, Eric Hawkins, Paul Hebert, Elaine Hu, Anna Korpak, Daniel Morelli, Alexander Peterson, Ashok Reddy, Javeed Shah, Whitney Showalter, Nicholas Smith, Pradeep Suri, Eva Thomas, Aaron Turner, Elizabeth Vig, Katrina Wicks, Edwin Wong, Katherine Wysham, George Ioannou, Ann O'Hare, Barbara Jones, Makoto Jones, and Sara Knight
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Funding
This work was supported by grants C19-21-278, C19-21-279, SDR 02-237, and SDR 98-004 from the VA Health Services Research. All statements in this article, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the US Department of Veterans Affairs or the US government.
Notes
- 1. Anderson JK, Mackey KM, Beech EH, Young S, Parr NJ. Factors Associated with Homelessness Among US Veterans: A Systematic Review. Department of Veterans Affairs; 2023. Accessed April 11, 2024. http://www.ncbi.nlm.nih.gov/books/NBK593441/ [PubMed] [Google Scholar]
- 2. Heflin CM, Wilmoth JM, London AS. Veteran status and material hardship: the moderating influence of work-limiting disability. Social Serv Rev. 2012;86(1):119–142. 10.1086/665643 [DOI] [Google Scholar]
- 3. Robbins R, Porter Starr KN, Addison O, et al. Prevalence and socio-economic determinates of food insecurity in veterans: findings from National Health and Nutrition Examination Survey. Public Health Nutr. 2023;26(7):1478–1487. 10.1017/S1368980023000538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774–780. 10.1016/j.amepre.2020.12.012 [DOI] [PubMed] [Google Scholar]
- 5. Govier DJ, Bui D, Hauschildt KE, et al. COVID-19 & financial hardship: a national prospective veteran cohort study. Poster presented at: Academy Health Annual Research Meeting; July 1, 2024; Baltimore, MD.
- 6. Kelly JD, Bravata DM, Bent S, et al. Association of social and behavioral risk factors with mortality among US veterans with COVID-19. JAMA Netw Open. 2021;4(6):e2113031. 10.1001/jamanetworkopen.2021.13031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cohen RA, Boersma P. Financial burden of medical care among veterans aged 25-64, by health insurance coverage: United States, 2019-2021. Natl Health Stat Report. 2023;182:1–14. [PubMed] [Google Scholar]
- 8. Raifman J, Nocka K, Jones D, et al. COVID-19 US state policy database. Published online 2020. Accessed December 16, 2023. https://statepolicies.com/data/library/
- 9. Manoj M, Truong PP, Shiffman J, Shawar YR. The health justice policy tracker: COVID-19 policies to advance health justice for vulnerable populations: analysis examines the COVID-19 health justice policy tracker to examine policies using a health justice lens. Health Aff (Millwood). 2023;42(12):1689–1696. 10.1377/hlthaff.2023.00704 [DOI] [PubMed] [Google Scholar]
- 10. Cooney P, Shaefer HL, Jubaed S. Material Hardship and Well-Being of U.S. Households at the End of 2021. University of Michigan; 2022. Accessed December 16, 2023. https://sites.fordschool.umich.edu/poverty2021/files/2022/03/PovertySolutions-Material-Hardship-2021-March2022.pdf [Google Scholar]
- 11. Center on Budget and Policy Priorities . The COVID-19 economy's effects on food, housing, and employment hardships; 2022. Accessed December 16, 2023. https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-and
- 12. Boen CE, Keister LA, Gibson-Davis CM, Luck A. The buffering effect of state eviction and foreclosure policies for mental health during the COVID-19 pandemic in the United States. J Health Soc Behav. 2023. 10.1177/00221465231175939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Evangelist M, Wu P, Shaefer HL. Emergency unemployment benefits and health care spending during COVID. Health Serv Res. 2022;57(1):15–26. 10.1111/1475-6773.13772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tsai J, McCleery A, Wynn JK, Green MF. Unconditional cash transfers and association with clinical outcomes among U.S. veterans with psychosis or recent homelessness. Psychiatr Serv. 2023;74(11):1123–1131. 10.1176/appi.ps.20230021 [DOI] [PubMed] [Google Scholar]
- 15. Cooney P, Shaefer HL. Material hardship and well-being of U.S. households in 2022. University of Michigan; 2022. Accessed December 16, 2023. https://sites.fordschool.umich.edu/poverty2021/files/2022/10/Material-Hardship-PB-final.pdf
- 16. Wedeen S. Interactive Map Shows Geographic Variation in Pandemic Financial Pressures. Joint Center for Housing Studies, Harvard University; 2021. https://www.jchs.harvard.edu/blog/interactive-map-shows-geographic-variation-pandemic-financial-pressures [Google Scholar]
- 17. Towne SD, Probst JC, Hardin JW, Bell BA, Glover S. Health & access to care among working-age lower income adults in the great recession: disparities across race and ethnicity and geospatial factors. Soc Sci Med. 2017;182:30–44. 10.1016/j.socscimed.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 18. Peikes DN, Swankoski KE, Rastegar JS, Franklin SM, Pavliv DJ. Burden of health-related social needs among dual- and non-dual-eligible Medicare Advantage beneficiaries: study examines health-related social needs among dual- and non-dual-eligible Medicare Advantage beneficiaries. Health Aff (Millwood). 2023;42(7):899–908. 10.1377/hlthaff.2022.01574 [DOI] [PubMed] [Google Scholar]
- 19. Gertz AH, Pollack CC, Schultheiss MD, Brownstein JS. Delayed medical care and underlying health in the United States during the COVID-19 pandemic: a cross-sectional study. Prev Med Rep. 2022;28:101882. 10.1016/j.pmedr.2022.101882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bruch SK, Naald JVD, Gornick JC. Poverty reduction through federal and state policy mechanisms: variation over time and across the United States. Social Serv Rev. 2023;97(2):270–319. 10.1086/724556 [DOI] [Google Scholar]
- 21. Dhongde S, Glassman B. Multidimensional hardships in the U.S. during the COVID-19 pandemic. Soc Indic Res. 2023;169(3):883–905. 10.1007/s11205-023-03176-9 [DOI] [Google Scholar]
- 22. Fargo J, Metraux S, Byrne T, et al. Prevalence and risk of homelessness among US veterans. Prev Chronic Dis. 2012;9:E45. [PMC free article] [PubMed] [Google Scholar]
- 23. Tsai J, Hooshyar D. Prevalence of eviction, home foreclosure, and homelessness among low-income US veterans: the National Veteran Homeless and Other Poverty Experiences Study. Public Health. 2022;213:181–188. 10.1016/j.puhe.2022.10.017 [DOI] [PubMed] [Google Scholar]
- 24. London AS, Heflin CM. Supplemental Nutrition Assistance Program (SNAP) use among active-duty military personnel, veterans, and reservists. Popul Res Policy Rev. 2015;34(6):805–826. 10.1007/s11113-015-9373-x [DOI] [Google Scholar]
- 25. Iwashyna TJ, Smith VA, Seelye S, et al. Self-reported everyday functioning after COVID-19 infection. JAMA Netw Open. 2024;7(3):e240869. 10.1001/jamanetworkopen.2024.0869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Üstün T, Kostanjesek N, Chatterji S, Rehm J. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). World Health Organization; 2010. https://www.who.int/publications-detail-redirect/measuring-health-and-disability-manual-for-who-disability-assessment-schedule-(-whodas-2.0) [Google Scholar]
- 27. Iwashyna TJ, Kamphuis LA, Gundel SJ, et al. Continuing cardiopulmonary symptoms, disability, and financial toxicity 1 month after hospitalization for third-wave COVID-19: early results from a US nationwide cohort. J Hosp Med. 2021;16(9):531–537. 10.12788/jhm.3660 [DOI] [PubMed] [Google Scholar]
- 28. Hauschildt KE, Seigworth C, Kamphuis LA, et al. Financial toxicity after acute respiratory distress syndrome: a national qualitative cohort study. Crit Care Med. 2020;48(8):1103–1110. 10.1097/CCM.0000000000004378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. US Census Bureau . Census regions and divisions of the United States. Accessed January 24, 2024. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
- 30. Veterans Affairs Health Services Research and Development . Veterans Affairs Corporate Data Warehouse. http://www.hsrd.research.va.gov/for_researchers/vinci/cdw.cfm
- 31. University of Wisconsin School of Medicine and Public Health . 2015 Area Deprivation Index. Version 2.0. https://www.neighborhoodatlas.medicine.wisc.edu/
- 32. Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749–759. 10.1016/j.jclinepi.2010.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. National Veterans Legal Services Program . COVID-19 economic assistance for veterans. 2020. Accessed December 16, 2023. https://www.nvlsp.org/news-and-events/press-releases/covid-19-economic-assistance-information-for-veterans
- 34. US Department of Veterans Affairs . American rescue plan provides veterans seamless COVID-19 protections and monetary aid. Published March 12, 2021. Accessed December 16, 2023. https://news.va.gov/press-room/american-rescue-plan-provides-veterans-seamless-covid-19-protections-and-monetary-aid/
- 35. Norris L. COVID-19: state and federal efforts to improve access to testing, treatment, and health coverage. Published August 16, 2021. Accessed December 16, 2023. https://www.healthinsurance.org/obamacare/state-and-federal-efforts-to-improve-access-to-covid-19-testing-treatment/
- 36. Ritzwoller DP, Goodrich GW, Tavel HM, et al. Patient factors associated with use of adult primary care and virtual visits during the COVID-19 pandemic. Med Care. 2023;61(Suppl 1):S12–S20. 10.1097/MLR.0000000000001792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Almuqarrab A, Almuqamam A, Alhayki F, Alsultan F, Almuqamam M. The impact of waived cost-sharing policy on COVID-19 daily testing and deaths. Cureus. 2022;14(2):e21843. 10.7759/cureus.21843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chua KP, Conti RM, Becker NV. Trends in and factors associated with out-of-pocket spending for COVID-19 hospitalizations from March 2020 to March 2021. JAMA Netw Open. 2022;5(2):e2148237. 10.1001/jamanetworkopen.2021.48237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hernandez M, Wong R, Yu X, Mehta N. In the wake of a crisis: caught between housing and healthcare. SSM Popul Health. 2023;23:101453. 10.1016/j.ssmph.2023.101453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Guth M, Garfield R, Rudowitz R; Kaiser Family Foundation . The effects of Medicaid expansion under the ACA: updated findings from a literature review. Henry J. Kaiser Foundation; 2020. Accessed April 12, 2024. https://files.kff.org/attachment/Report-The-Effects-of-Medicaid-Expansion-under-the-ACA-Updated-Findings-from-a-Literature-Review.pdf
- 41. La Forgia A, Bond AM, Braun RT, Kjaer K, Zhang M, Casalino LP. Association of surprise-billing legislation with prices paid to in-network and out-of-network anesthesiologists in California, Florida, and New York: an economic analysis. JAMA Intern Med. 2021;181(10):1324–1331. 10.1001/jamainternmed.2021.4564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–1509. 10.1001/jamainternmed.2016.4419 [DOI] [PubMed] [Google Scholar]
- 43.Kaiser Family Foundation. Status of State Medicaid Expansion Decisions: Interactive Map. Published December 1, 2023. Accessed December 16, 2023. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
- 44. Govier DJ, Than CT, Chawla N, et al. Veterans Health Administration healthcare coverage and medical financial hardship in low-income veterans. Am J Prev Med. 2023;65(3):406–416. 10.1016/j.amepre.2023.03.004 [DOI] [PubMed] [Google Scholar]
- 45. US Census Bureau . American Community Survey: sex by age by veteran status for the civilian population 18 years and over, 2022. 2023. Accessed December 16, 2023. https://data.census.gov/table/ACSDT1Y2022.B21001? q=B21001&g=010XX00US$0400000&tp=true
- 46. Kona M. State balance-billing protections (map). Published online 2020. Accessed December 16, 2023. 10.26099/0X7J-7731 [DOI]
- 47. Trinidad S, Brokamp C, Mor Huertas A, et al. Use of area-based socioeconomic deprivation indices: a scoping review and qualitative analysis. Health Aff (Millwood). 2022;41(12):1804–1811. 10.1377/hlthaff.2022.00482 [DOI] [PubMed] [Google Scholar]
- 48. Hannan EL, Wu Y, Cozzens K, Anderson B. The neighborhood atlas Area Deprivation Index for measuring socioeconomic status: an overemphasis on home value: study examines the neighborhood atlas Area Deprivation Index as a tool to measure socioeconomic status. Health Aff (Millwood). 2023;42(5):702–709. 10.1377/hlthaff.2022.01406 [DOI] [PubMed] [Google Scholar]
- 49. Morenz AM, Liao JM, Au DH, Hayes SA. Area-level socioeconomic disadvantage and health care spending: a systematic review. JAMA Netw Open. 2024;7(2):e2356121. 10.1001/jamanetworkopen.2023.56121 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.