Abstract
Transgender and gender diverse (TGD) adults are more likely to have obesity compared to cisgender peers. Based on surveys, the TGD population experiences disparities in healthy lifestyle behaviors (e.g., physical activity, screen time) compared to reference groups. They also face significant socioeconomic and healthcare barriers to accessing affirming care and gender minority stress, potentially contributing to increased weight. Gender-affirming hormone therapy is associated with changes in body composition and increased weight, which may impact cardiometabolic risk trajectory. Obesity can also be a barrier to gender-affirming surgeries, and affirming weight management services tailored to TGD patients are an important gap in healthcare to address. This Perspective briefly reviews current literature on the unique barriers experienced by TGD people and their identified needs regarding weight management interventions. It also suggests areas for future research to best fill this gap in healthcare and research while supporting the provision of lifesaving gender-affirming care.
In 2011, the U.S. Institute of Medicine identified obesity as an important health problem among gender and sexual minority people [1]. This includes transgender and gender diverse (TGD) individuals who have gender identities that differ from their sex assigned at birth. TGD adults are more like to have obesity compared to cisgender populations based on Veterans Health Administration records (adjusted odds ratio 1.58 [95% Cl 1.48–1.70]) and Medicare claims (31.3% vs. 17.2%, respectively) [2, 3]. Contemporaneously, lifetime prevalence of disordered eating is high among transgender men and women (10.6% and 8.1%, respectively), particularly anorexia and bulimia, due to internalized societal ideals of gender-specific body norms [4]. Thus, it is crucial for medical providers to become competent in culturally appropriate healthy weight management services to reduce the prevalence and comorbidities of overweight and obesity in this population.
TGD people’s higher prevalence of obesity is likely multifactorial (Fig. 1). Firstly, they less frequently access healthcare due to socioeconomic barriers and prejudice. In 2014, 40% of TGD adults in Colorado reported delaying medical care because of cost, inadequate insurance and/or fear of discrimination [5]. TGD patients often experience gender minority stress, the perceived or experienced stigmatization and social marginalization due to gender identity, leading many patients to avoid medical care due to concerns for social safety [6]. Secondly, they experience disparities in healthy lifestyle behaviors. For example, transgender college students are less likely to engage in ≥2 h of strenuous physical activity per week or any strengthening physical activity and more likely to engage in ≥14 h weekly of screen time compared to non-transgender peers [7]. This may be secondary to socioeconomic barriers and higher rates of certain health issues, particularly depression and anxiety, which provide additional mental and physical barriers to engaging in healthful behaviors [8].
Fig. 1.
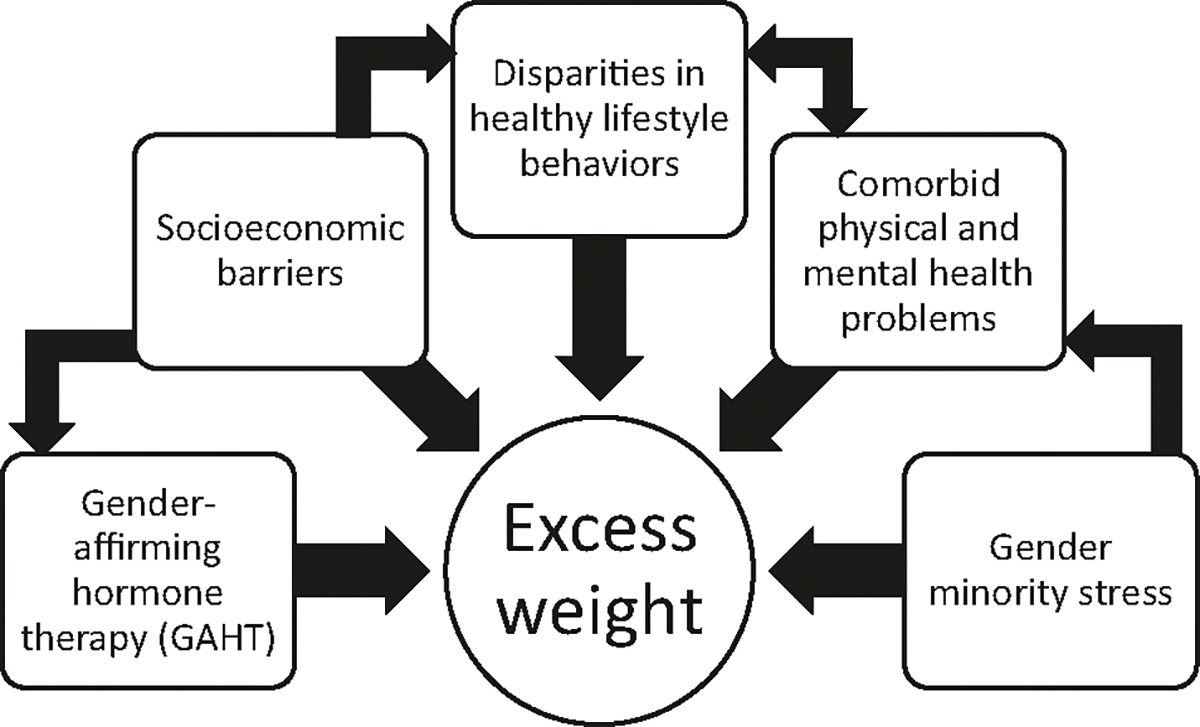
Contributors to excess weight for TGD people.
Additionally, gender-affirming hormone therapy (GAHT) has been associated with increases in body weight; masculinizing GAHT (i.e., testosterone) is associated with increased lean mass and decreased fat mass and feminizing GAHT (i.e., estrogen plus antiandrogens) is associated with the reverse changes, potentially impacting cardiometabolic risk trajectory [9]. In a recent longitudinal study of 470 TGD patients, ≥5 kg weight gain was experienced by 21% of patients on feminizing GAHT and 30% on masculinizing GAHT 11–21 months after initiation [10]. While transgender men gained a mean 2.35 kg within 2–4 months, transgender women did not gain weight until 21 months after initiating GAHT. Although the study did not account for confounders contributing to weight gain nor body composition changes, it suggests that many TGD patients gain weight with GAHT. The authors endorsed the need for more studies on the impact of different routes of GAHT administration on weight trajectory and whether these weight increases contribute to higher risk of cardiovascular disease and cancers.
In addition to increasing health risks, obesity is a barrier for many TGD people pursuing gender-affirming surgeries (GAS). While there is significant heterogeneity between surgical centers, many enforce body mass index (BMI) cutoffs for GAS, usually set at 30 or 35 kg/m2 based on the surgeon’s discretion. Increased perioperative complications and need for reoperation with increased BMI have been observed in cosmetic plastic surgery studies [11]; however, the merits of these concerns for GAS have recently been challenged given limited evidence that BMI significantly influences GAS outcomes [12]. Protocols to facilitate weight loss prior to GAS are lacking, but whether specific gender-affirming weight loss strategies are needed or desired is also yet to be determined. A recent retrospective study at Mount Sinai found that one-fourth of all patients presenting for an initial GAS consult had obesity and the prevalence of obesity did not change at subsequent follow-up with self-monitored weight management (i.e, unsupervised calorie restriction and increased physical activity) due to poor adherence [13]. These results suggest that affirming weight management programs may support the provision of lifesaving gender-affirming care such as healthy weight loss prior to GAS.
Addressing overweight and obesity in the TGD population requires understanding their unique barriers to care and listening to their needs and goals. According to the results of the Colorado Transgender Health Survey, transgender people who had providers that they perceived as inclusive were more likely to have received an annual routine exam within the past year, were almost half as likely to delay care due to fear of discrimination, and had lower rates of reported fair or poor overall health compared to people without an inclusive provider [5]. These results illustrate the need for inclusive providers who are knowledgeable about and able to address TGD-specific healthcare needs. Furthermore, many transgender women and men report improved social relations and decreased body uneasiness, respectively, with increased BMI after initiating GAHT [14, 15]. Thus, weight loss may not be consistent with TGD people’s goals; increases in weight may be affirming for TGD people in attaining desired body shape and should be considered prior to weight loss advice.
To our knowledge, there are no published needs assessments of TGD individuals regarding weight management strategies (self- or clinician-monitored) or perceptions about body weight, overweight and obesity. However, a nutritional needs assessment of 26 TGD university students in the U.S. Midwest, seven of whom had overweight or obesity, found that participants wanted interventions in spaces where they felt safe and comfortable and with TGD people on the intervention team [16]. Providing individual, group-based, and virtual options was preferred. They desired individually tailored nutritional guidance focusing on addressing food insecurity and targeting eating disorder prevention and treatment. Physical activity was a top concern for these students, and they expressed a need for inclusive exercise facilities that have accessible bathrooms and locker rooms and provide accommodations for physical disability. These students underutilized existing resources because they either were unaware of resources or questioned their inclusivity. Extrapolating from these results, providers should familiarize themselves with local and national resources that are inclusive to TGD people when creating or modifying existing patient care environments.
Addressing and eliminating barriers to behavior change among TGD individuals is necessary for weight management but may not be sufficient to achieve desired weight, whether for GAS or other reasons. As in studies in cisgender individuals in clinical practice, most TGD people with obesity will require adjunct treatment with medication and/or bariatric surgery to meet their weight loss goals. We are unaware of published studies on the effectiveness of weight loss medications in TGD patients. Given the significant socioeconomic barriers of TGD people and limited insurance coverage of weight loss medications, providers should consider off-label use of weight loss medications to increase access, when appropriate. Evidence for bariatric surgery in TGD patients is limited to a recent retrospective Dutch study of 15 patients who underwent bariatric surgery prior to GAS [17]. All participants weighed significantly less at the date of GAS compared to date of bariatric surgery, but the mean time between procedures was 3.4 years for transgender men and 3.0 years for transgender women. Overall, more evidence is needed regarding the efficacy and desirability of medical and surgical weight management treatments in TGD patients.
With increasing numbers of people identifying as TGD and the continued rise of the obesity epidemic, providers must prepare to manage obesity in this population in affirming ways. Interventions should be culturally appropriate, effective, and tailored to TGD individuals as informed by them. Providers should develop skills to better (1) assess for disordered eating and body shape goals when tailoring weight management recommendations; (2) assist patients in addressing barriers to healthful behaviors; and (3) consider offering anti-obesity medications or bariatric surgery when self-monitored weight management is insufficient. More research is necessary to better characterize the prevalence of overweight and obesity in TGD patients, to identify and meet TGD people’s needs regarding weight management services, and to determine the safety and effectiveness of weight loss medications and bariatric surgery in this population.
FUNDING
JMT has no financial disclosures. SJI receives funding through a Eunice Kennedy Shriver National Institute of Child Health & Human Development grant (The Colorado Building Interdisciplinary Research Careers in Women’s Health [BIRCWH] Program; supported by 5K12HD057022, PIs: Regensteiner JG and Santoro NF).
Footnotes
COMPETING INTERESTS
The authors declare no competing interests.
ADDITIONAL INFORMATION
Reprints and permission information is available at http://www.nature.com/reprints
REFERENCES
- 1.The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC) 2011. [PubMed] [Google Scholar]
- 2.Brown GR, Jones KT. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the veterans health administration: a case-control study. LGBT Health. 2016;3:122–31. [DOI] [PubMed] [Google Scholar]
- 3.Dragon CN, Guerino P, Ewald E, Laffan AM. Transgender medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT Health. 2017;4:404–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nagata JM, Ganson KT, Austin SB. Emerging trends in eating disorders among sexual and gender minorities. Curr Opin Psychiatry. 2020;33:562–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christian R, Mellies AA, Bui AG, Lee R, Kattari L, Gray C. Measuring the health of an invisible population: lessons from the Colorado Transgender health survey. J Gen Intern Med. 2018;33:1654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diamond LM, Alley J. Rethinking minority stress: a social safety perspective on the health effects of stigma in sexually-diverse and gender-diverse populations. Neurosci Biobehav Rev. 2022;138:104720. [DOI] [PubMed] [Google Scholar]
- 7.VanKim NA, Erickson DJ, Eisenberg ME, Lust K, Simon Rosser BR, Laska MN. Weight-related disparities for transgender college students. Health Behav Policy Rev. 2014;1:161–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newcomb ME, Hill R, Buehler K, Ryan DT, Whitton SW, Mustanski B. High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non-binary, and gender diverse youth and young adults. Arch Sex Behav. 2020;49:645–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klaver M, Dekker M, de Mutsert R, Twisk JWR, den Heijer M. Cross-sex hormone therapy in transgender persons affects total body weight, body fat and lean body mass: a meta-analysis. Andrologia. 2017;49:e12660. [DOI] [PubMed] [Google Scholar]
- 10.Kyinn M, Banks K, Leemaqz SY, Sarkodie E, Goldstein D, Irwig MS. Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy. Int J Obes (Lond). 2021;45:2562–9. [DOI] [PubMed] [Google Scholar]
- 11.Bigarella LG, Ballardin AC, Couto LS, de Avila ACP, Ballotin VR, Ingracio AR, et al. The impact of obesity on plastic surgery outcomes: a systematic review and meta-analysis. Aesthet Surg J. 2022;42:795–807. [DOI] [PubMed] [Google Scholar]
- 12.Brownstone LM, DeRieux J, Kelly DA, Sumlin LJ, Gaudiani JL. Body mass index requirements for gender-affirming surgeries are not empirically based. Transgend Health. 2021;6:121–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martinson TG, Ramachandran S, Lindner R, Reisman T, Safer JD. High body mass index is a significant barrier to gender-confirmation surgery for transgender and gender-nonbinary individuals. Endocr Pract. 2020;26:6–15. [DOI] [PubMed] [Google Scholar]
- 14.Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, et al. Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-year follow-up data. J Clin Endocrinol Metab. 2016;101:4260–9. [DOI] [PubMed] [Google Scholar]
- 15.Silva ED, Fighera TM, Allgayer RM, Lobato MIR, Spritzer PM. Physical and sociodemographic features associated with quality of life among transgender women and men using gender-affirming hormone therapy. Front Psychiatry. 2021;12:621075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirby SR, Linde JA. Understanding the nutritional needs of transgender and gender-nonconforming students at a large public midwestern university. Transgend Health. 2020;5:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Sluis WB, de Bruin RJM, Steensma TD, Bouman MB. Gender-affirmation surgery and bariatric surgery in transgender individuals in The Netherlands: Considerations, surgical techniques and outcomes. Int J Transgend Health. 2022;23:355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]


