Abstract
Objective:
While the short-term effects of disasters on health care utilization are well documented, less is known regarding potential longer-term effects. This study investigates the effects of Hurricane Katrina on the health care utilization of older individuals with diabetes.
Methods:
We examined Medicare claims and enrollment data for the 2002-2004 and 2006-2008 time periods for older individuals with diabetes. Our quasi-experimental design analyzed utilization across 2 treated and 3 control groups. We compared the proportion of individuals who received a screen related to diabetes before and after Katrina in the treated groups to the proportions in the control groups. Our regression analysis employs individual and year fixed effects to control for factors specific to a given individual or to a given year.
Results:
We found that utilization rates in the 2002-2004 period exhibited roughly parallel trends for the treated and control groups, which provides support for our research design. The 2006-2008 utilization rates were generally lower for the treated groups than they were for the control groups. The differences were especially pronounced for older age cohorts.
Conclusions:
Our study suggests that the effects of disasters on health care utilization may persist for years after the event. Recovery efforts may be improved by addressing both short-term and long-term health care interruptions.
Keywords: hurricane, Medicare, diabetes, administrative data, health care utilization
The potential short-term effects of disasters on health care utilization are often readily apparent. Disaster victims typically face daunting challenges in obtaining care, including being unable to travel to their provider or their provider’s facility being closed, perhaps permanently. Further, in the days after a disaster, concerns for self, family, friends, or property may supersede their perceived need for health care.
Screenings are an essential type of utilization for diabetics to keep their condition under control. Timely screenings can help prevent diabetic complications such as retinopathy, chronic kidney disease, and end-stage renal disease. The relatively few studies that examine changes in utilization by diabetics following disasters investigate short-term effects. Children displaced by Hurricane Katrina were generally able to maintain screens immediately following the storm.1 However, residents affected by Katrina experienced problems with dialysis patient care, dialysis unit function, and supplies.2 Studies following Hurricane Sandy found higher rates of emergency department utilization for all diabetics3 and seniors in particular.4 Studies of postdisaster utilization for other conditions also examine a relatively short period after the disaster.5-8
While less obvious, there may be long-term effects of disasters on utilization. Nonhealth concerns may persist for significant periods of time. Victims may be forced to find new providers and, even if they are able to do so, they may encounter logistical or emotional barriers to re-establishing their care patterns. Negative emotional reactions to the disaster may lead victims to feel less motivated in maintaining their health. In the extreme scenario of displacement, victims can face extensive impediments to obtaining routine care. These challenges can be magnified for seniors, as the effects of disasters on their health are generally greater and they are especially at risk of developing new medical conditions.
Several studies have investigated the effects of disasters on health outcomes for diabetes. A number of diabetes measures were found to have deteriorated for victims of Hurricane Katrina immediately following the storm, but measures had largely recovered within a year.9 Studies following earthquakes in Japan in 1995 and 2011 found differing changes in HbA1c levels,10,11 while an analysis of diabetics affected by the 2011 tsunami found that blood pressure and HbA1c worsened.12 While quality-adjusted life expectancy decreased for diabetics affected by Hurricane Katrina,13 there was no measured change in mortality risk for dialysis patients.14
In this paper, we analyze the relationship between disaster exposure and the frequency of important diabetes screenings for an extended period following the disaster in the context of Hurricane Katrina. Katrina struck the United States Gulf Coast in August 2005 and was responsible for approximately 1200 deaths and $108 billion in damages.15 Approximately 1.5 million people in the region were forced to evacuate.16
This study compares screening utilization data for senior diabetics for the 3 years prior to the storm to the 3 years following. We group individuals by their exposure to the storm to estimate the potential association between disaster exposure and utilization. We utilize individual-level insurance claims data to perform both group- and individual-level analyses.
Our analysis improves upon existing studies in a number of ways. By investigating longer-term outcomes, we fill a significant gap in the literature. Our use of multiple treated and control groups provides nuanced estimates of the effects that reflect differences in geography and demography. We also measure the differential effects for seniors who were displaced by Katrina. Finally, the administrative claims data that we use provides a detailed picture of utilization that is not subject to recall error and has rarely been used in previous disaster studies.4
METHODS
Data
Our sample period is 2002-2004 and 2006-2008. The year 2005 is excluded from the sample due to concerns regarding data accuracy in light of the destructive impact of Katrina. We employ data from the Medicare Master Beneficiary Summary File and Personal Summary file. The data include data for all claims paid for all Medicare beneficiaries enrolled in traditional, fee-for-service Medicare.
Our unrestricted sample consists of all Medicare beneficiaries in 2004 and 2005 who had a diabetes diagnosis at some point since 1999 and resided in either Alabama, Louisiana, Mississippi, or Texas. These states are chosen to include both those beneficiaries potentially affected by Katrina, as well as beneficiaries thought to be suitable controls. We restrict our sample to beneficiaries who were present in every year of our sample period. We further restrict the sample to beneficiaries who had Medicare Part A and Medicare Part B coverage in every month, were not enrolled in Medicare Advantage at any point, did not die prior to 2009, and whose eligibility was based on Old-Age and Survivors Insurance (OASI) and not due to end-stage renal disease or disability coverage. Additional restrictions include limiting the sample to beneficiaries who lived in the same county throughout 2002-2004 and who were less than 100 years old as of January 1, 2002. The resulting number of beneficiaries in our sample is 1 521 736.
Groups
We group the beneficiaries to account for the extent to which they were likely affected by Katrina. Our first grouping level is the beneficiary’s state of residence. This grouping accounts for any potential state-specific factors that may have affected their utilization, such as medical resource availability and geographic proximity to Hurricane Katrina’s path.
The second grouping level is based on the level of assistance designated by the Federal Emergency Management Agency (FEMA) to be provided to the beneficiary’s county of residence. The 2 primary assistance levels are individual assistance and public assistance. Individual assistance is intended for areas in which the damages are determined to be beyond the response capabilities of the state and local governments,17 while public assistance is intended for less-affected areas.18 Our groupings reflect FEMA designations for both Hurricane Katrina and Hurricane Rita (which made landfall roughly 1 month after Hurricane Katrina). Table 1 details the FEMA designations by state and indicates that roughly half of the counties in Alabama, Louisiana, and Mississippi were designated as individual assistance counties following Hurricane Katrina.
TABLE 1.
Number of FEMA-Declaration Counties by Hurricane and State
| Katrina | Rita | |||||
|---|---|---|---|---|---|---|
| Individual Assistance |
Public Assistance |
None | Individual Assistance |
Public Assistance |
None | |
| Alabama | 11 | 22 | 45 | 0 | 0 | 67 |
| Louisiana | 31 | 63 | 1 | 0 | 63 | 1 |
| Mississippi | 49 | 82 | 0 | 0 | 0 | 82 |
| Texas | 0 | 254 | 0 | 22 | 232 | 0 |
Notes: Based on the following FEMA designated areas websites. AL: https://www.fema.gov/disaster/1605/designated-areas. LA: https://www.fema.gov/disaster/1603/designated-areas, https://www.fema.gov/disaster/3260/designated-areas. MS: https://www.fema.gov/disaster/1604/designated-areas. TX: https://www.fema.gov/disaster/3216/designated-areas, https://www.fema.gov/disaster/1606/designated-areas.
As our interest is in the effects of Hurricane Katrina, our primary treated group (T1) consisted of beneficiaries who lived in a county in any state that was declared as an individual assistance county following Hurricane Katrina. Our secondary treated group (T2) consisted of beneficiaries who lived in a Louisiana county designated as a public assistance county.
We employ 3 control groups. Control group 1 (C1) consisted of beneficiaries who lived in a Mississippi county designated as a public assistance county, while control group 2 (C2) consisted of all residents in a Texas county designated as a public assistance county. Finally, control group 3 (C3) comprised all beneficiaries in an Alabama county not designated as either individual or public assistance.
While we use the term control groups to describe these last 3 groups, we readily admit that they are not perfectly “pure” control groups. Groups C1 and C2 are especially imperfect control groups given their residents were affected by either Hurricane Katrina and Rita, albeit somewhat indirectly given their public assistance status. Group C3 is likely the closest we have to a true control group.
Measures
The screenings analyzed are cholesterol, HbA1C, microalbumin, and retinal. Our outcome of interest is whether the beneficiary received at least 1 of the specified screenings in a given year. Current Procedural Terminology (CPT) codes are used to determine whether a specified screening was received. (See Appendix Table 1 for CPT codes used.)
Statistical Analysis
For the group-level analyses, the analysis consisted of descriptive measures of the proportion of beneficiaries in that group who received at least 1 screen in that year.
The individual-level analyses are based on linear regressions of samples based on observations at the level of beneficiary-year. Given that each beneficiary appeared in the data from each of the 6 sample years, the regressions contain 6 observations for each beneficiary. Separate regressions are estimated for each of the 4 screening types (HbA1c, retinal, cholesterol, and microalbumin).
The base regression equation is
| [1] |
where denotes the beneficiary, denotes the group, and denotes the year. is a binary variable that equals 1 if the beneficiary in group and year received the screening in question. are individual fixed effects that control for any factors that affected the baseline probability of screening that did not vary during the sample period. For instance, the individual fixed effects control for any racial differences in the probability of receiving a screen during the sample period. It is important to note that the inclusion of individual fixed effects implies that it is not possible to include explanatory variables that are constant throughout the sample period (eg, age, race). are year fixed effects that controlled for any factor common to all beneficiaries that were specific to a given year. For example, the 2007 year fixed effect controls for any national factors that affected the likelihood of individuals obtaining a screen in 2007.
The coefficients of interest are represented by . The terms following it in Equation 1 are the interactions of the year indicator variables with the group indicator variables. Thus, the coefficients measure the marginal effect on the probability of being screened for that year and group.
For instance, the coefficient on the interaction between the 2006 year indicator variable and the group T1 indicator variable measures the marginal effect on the probability of being screened for a beneficiary in group T1 in 2006. If this coefficient is negative, it implies that individuals in group T1 in 2006 were less likely to obtain the screening.
Given our research question, we are most interested in the coefficients for the 2 treated groups in the post-Katrina period. In other words, our focus is on the 2006, 2007, and 2008 interaction coefficients for groups T1 and T2. If these coefficients are less than the corresponding coefficients for the control groups, it would suggest that the treated groups were less likely to obtain screenings.
Additional regressions are estimated to assess whether the marginal effects for the treated groups differed across demographic characteristics. The inclusion of individual fixed effects implies that it is not possible to directly include in the regression variables that do not vary within individuals. However, it is possible to include the interaction of such variables with the year indicator variables and the group indicator variables. Thus, for instance, we are able to estimate the marginal effect for blacks in group T1 in 2007.
The regressions are estimated via ordinary least squares and the errors are clustered at the individual level. All calculations were performed in Stata 14.0. The study was approved on an expedited basis by the University of South Florida Institutional Review Board (IRB# CR2_Pro00024034).
RESULTS
Table 2 describes the demographic characteristics of the 2 treated and 3 control groups. The number of beneficiaries in each group ranged from 54 636 in group C1 to 712 815 in group C2. The gender and age proportions across the groups are relatively consistent. Differences are present across race/ethnic groups: groups T1, T2, and C1 have higher proportions of blacks, while group C2 has a much higher proportion of Hispanics. The variable “state buy-in” refers to individuals for whom the state Medicaid program paid the Medicare premium for the individual. As this is typically done for individuals at low income levels, this variable can be considered a rough proxy for low socioeconomic status. The 2 outliers for this proportion are group C2 at 16.7% and group C1 at 29.6%.
TABLE 2.
Demographic Characteristics
| Variable | Group T1 | Group T2 | Group C1 | Group C2 | Group C3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| N | 272 146 | 80 384 | 54 636 | 712 815 | 152 288 | |||||
| Gender | ||||||||||
| Female | 168 435 | 61.9 | 49 407 | 61.5 | 34 613 | 63.4 | 427 525 | 60.0 | 93 961 | 61.7 |
| Male | 103 711 | 38.1 | 30 977 | 38.5 | 20 023 | 36.6 | 285 290 | 40.0 | 58 327 | 38.3 |
| Race | ||||||||||
| Unknown | 218 | 0.1 | 81 | 0.1 | 31 | 0.1 | 377 | 0.1 | 97 | 0.1 |
| Non-Hispanic white | 219 662 | 80.7 | 64 062 | 79.7 | 43 607 | 79.8 | 549 673 | 77.1 | 133 632 | 87.7 |
| Black | 47 277 | 17.4 | 15 445 | 19.2 | 10 703 | 19.6 | 36 914 | 5.2 | 17 514 | 11.5 |
| Other | 429 | 0.2 | 140 | 0.2 | 60 | 0.1 | 1495 | 0.2 | 215 | 0.1 |
| Asian/Pacific Islander | 1108 | 0.4 | 140 | 0.2 | 136 | 0.2 | 6050 | 0.8 | 324 | 0.2 |
| Hispanic | 3161 | 1.2 | 456 | 0.6 | 89 | 0.2 | 117 335 | 16.5 | 417 | 0.3 |
| American Indian/Alaska Native | 291 | 0.1 | 60 | 0.1 | 10 | 0.0 | 971 | 0.1 | 89 | 0.1 |
| Age | ||||||||||
| 65-69 | 78 800 | 29.0 | 23 954 | 29.8 | 16 478 | 30.2 | 208 509 | 29.3 | 47 404 | 31.1 |
| 70-74 | 82 283 | 30.2 | 24 685 | 30.7 | 16 482 | 30.2 | 215 754 | 30.3 | 46 856 | 30.8 |
| 75-79 | 62 347 | 22.9 | 17 489 | 21.8 | 11 652 | 21.3 | 158 205 | 22.2 | 32 703 | 21.5 |
| 80-84 | 33 700 | 12.4 | 9789 | 12.2 | 6658 | 12.2 | 89 549 | 12.6 | 17 526 | 11.5 |
| 85+ | 15 016 | 5.5 | 4467 | 5.6 | 3 366 | 6.2 | 40 798 | 5.7 | 7799 | 5.1 |
| State buy-in | ||||||||||
| Yes | 52 310 | 19.2 | 18 029 | 22.4 | 16 157 | 29.6 | 119 138 | 16.7 | 31 411 | 20.6 |
| No | 219 836 | 80.8 | 62 355 | 77.6 | 38 479 | 70.4 | 593 677 | 83.3 | 120 877 | 79.4 |
Notes: Summary statistics of sample subjects are based on data from the 2004 Medicare personal summary file.
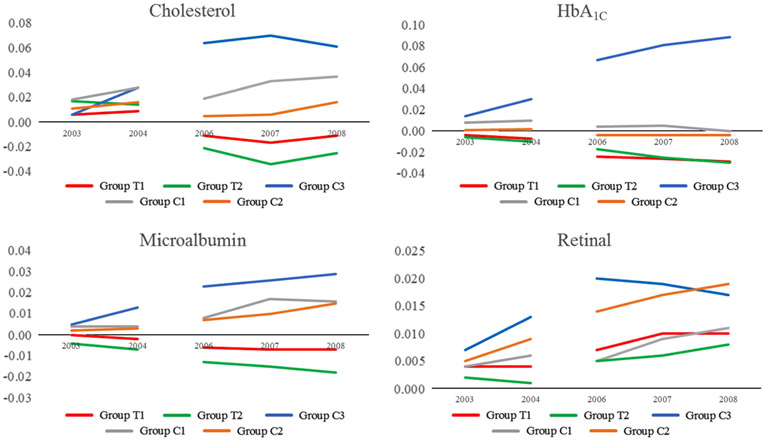
Figure 1 contains graphs that detail the group-level proportions of beneficiaries who received at least 1 of the specified screens in that year. Retinal and cholesterol screenings were the most commonly received, while microalbumin screenings were relatively rare. All of the screenings other than retinal display a generally upward trend during the sample period. Again, except for retinal, groups T1 and T2 generally have the lowest proportions. Further, the gaps between the control groups and the treated groups tend to increase significantly in the post-Katrina period. This divergence suggests that individuals in the treated groups may have experienced challenges to obtaining screenings after Katrina that individuals in the control group did not.
FIGURE 1. Screening Rates by Group.
Notes: Graphs depict the proportion of subjects in each group who received the indicated screening at least one time during the year.
A necessary condition for the regression analysis that we employ is the presence of parallel trends (or parallel slopes) in the pre-Katrina period. One way to assess this condition is to graphically examine the values of the outcome variables across the treated and control groups. Roughly parallel lines suggest that the parallel trends condition holds. While not definitive, the graphs in Figure 1 indicate that this condition may hold, in that the slopes of the lines in the 2002-2004 period are roughly similar. The most questionable case is for microalbumin screenings, where the pre-Katrina trends diverged somewhat.
The coefficients on the group-year interaction variables from the individual-level regressions are detailed in Figure 2. The omitted indicator variables are for the year 2002 and for group C1. Thus, the coefficients are to be interpreted as differences from 2002 screening rates for group C1. (The coefficients are provided in Appendix Table 3.)
FIGURE 2. Group-Year Interaction Coefficients.
Notes: The coefficients shown are based on regressions in which the dependent variable is a binary indicator of whether the individual received the specified screen in that year and are limited to interactions involving the T1 group.
The proximity of the pre-Katrina coefficients can be viewed as another indication of whether the parallel trends trend condition was likely to hold. The closer the values are in the 2003-2004 period, the more evidence is present in favor of parallel trends. The charts generally show a relatively tight bunching of coefficients in the pre-Katrina period, followed by more widely dispersed values post-Katrina, thus providing some evidence that the parallel trends condition is likely to hold.
Generally, the lines for the 2 treated groups are significantly lower than those for the control groups in the post-Katrina period. These gaps suggest lower screening rates for individuals in the treated groups after controlling for the other explanatory variables. The gap is especially large relative to group C3. (Recall that group C3 consisted of counties in Alabama that were not designated for assistance from FEMA and is arguably the “purest” of the 3 control groups.) For instance, the roughly 0.8 difference between T1 and C3 coefficients in the 2008 cholesterol figure correspond to an approximately 10% lower screening rate for T1 beneficiaries.
Table 3 compares the observed associations within each subgroup of T1 for the 4 screenings. Specifically, the reported values are the coefficients for each of the included group-year interactions. The omitted (or reference) subgroups are males, ages 65 to 69, whites, and no state buy-in. For instance, the top gender subsection of the table indicates that within the T1 group, in the 3 post-Katrina years, the probability of females receiving a cholesterol screen ranged from 1.2 to 1.5 percentage points higher than the probability of males receiving the same screening. The largest coefficients are present in the age group subsection, where the probability of receiving any of the 4 screens was significantly lower for the older age groups and where the difference increased over the 3 post-Katrina years. For screens other than HbA1c, blacks were more likely to receive a screen. Beneficiaries who received state Medicaid assistance to pay their Medicaid premiums were less likely to receive a HbA1c screen but more likely to receive a retinal screen.
TABLE 3.
Demographic-Group-Year Interaction Coefficient Estimates—Group T1
| Cholesterol | HbA1C | Microalbumin | Retinal | |||||
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Female | ||||||||
| 2006 | 0.015 | *** | −0.015 | *** | −0.002 | 0.027 | *** | |
| 2007 | 0.012 | *** | −0.016 | *** | −0.002 | 0.033 | *** | |
| 2008 | 0.012 | *** | −0.017 | *** | 0.001 | 0.039 | *** | |
| Age group | ||||||||
| 70-74 | ||||||||
| 2006 | −0.013 | *** | −0.027 | *** | −0.007 | *** | 0.023 | *** |
| 2007 | −0.02 | *** | −0.027 | *** | −0.007 | *** | 0.031 | *** |
| 2008 | −0.023 | *** | −0.028 | *** | −0.007 | *** | 0.037 | *** |
| 75-79 | ||||||||
| 2006 | −0.039 | *** | −0.034 | *** | −0.009 | *** | 0.006 | *** |
| 2007 | −0.05 | *** | −0.039 | *** | −0.012 | *** | 0.009 | *** |
| 2008 | −0.06 | *** | −0.04 | *** | −0.012 | *** | 0.009 | *** |
| 80-84 | ||||||||
| 2006 | −0.054 | *** | −0.042 | *** | −0.014 | *** | −0.008 | *** |
| 2007 | −0.069 | *** | −0.047 | *** | −0.017 | *** | −0.01 | *** |
| 2008 | −0.088 | *** | −0.056 | *** | −0.019 | *** | −0.016 | *** |
| 85-99 | ||||||||
| 2006 | −0.076 | *** | −0.052 | *** | −0.02 | *** | −0.034 | *** |
| 2007 | −0.101 | *** | −0.065 | *** | −0.025 | *** | −0.047 | *** |
| 2008 | −0.119 | *** | −0.068 | *** | −0.028 | *** | −0.071 | *** |
| Race/ethnicity | ||||||||
| Asian | ||||||||
| 2006 | 0.045 | ** | −0.0003 | 0.008 | 0.082 | *** | ||
| 2007 | 0.031 | −0.012 | 0.007 | 0.093 | *** | |||
| 2008 | 0.026 | 0.002 | 0.007 | 0.103 | *** | |||
| Black | ||||||||
| 2006 | 0.028 | *** | −0.005 | 0.005 | *** | 0.058 | *** | |
| 2007 | 0.025 | *** | −0.001 | 0.007 | *** | 0.079 | *** | |
| 2008 | 0.029 | *** | 0.0005 | 0.009 | *** | 0.095 | *** | |
| Hispanic | ||||||||
| 2006 | 0.002 | −0.002 | 0.009 | ** | 0.051 | *** | ||
| 2007 | 0.011 | −0.004 | 0.011 | *** | 0.058 | |||
| 2008 | 0.011 | −0.011 | 0.01 | ** | 0.07 | |||
| State buy-in | ||||||||
| Yes | ||||||||
| 2006 | −0.005 | −0.015 | *** | −0.004 | *** | 0.034 | *** | |
| 2007 | 0.003 | −0.011 | *** | −0.002 | 0.04 | *** | ||
| 2008 | 0.007 | * | −0.009 | *** | −0.003 | ** | 0.039 | *** |
Notes: *** P < .01, ** P < .05, * P < .10. The coefficients shown are based on regressions in which the dependent variable is a binary indicator of whether the individual received the specified screen in that year and are limited to interactions involving the T1 group.
DISCUSSION
Our goal was to assess the impact of Hurricane Katrina on long-term health care utilization for diabetic seniors, an especially vulnerable population. Our analysis was based on comparing utilization rates by those directly affected by Katrina to those in several geographically proximate groups. Our finding that the demographic profiles of the treated and control groups were roughly similar and that pre-Katrina screening rates exhibited parallel trends provided evidence that a difference-in-difference regression analysis was appropriate.
Our analysis indicated that there were large decreases in screening rates for the treated groups relative to the control groups in the post-Katrina period. However, the results for HbA1c, microalbumin, and retinal screenings were somewhat ambiguous given the post-Katrina coefficients largely followed the trends of the pre-Katrina coefficients. By contrast, in the cholesterol graphs, not only did the pre- and post-Katrina coefficient trends diverge for the treated groups, but the signs of the coefficients flipped from positive to negative. Based on comparisons to the C3 control group, the proportion of beneficiaries in the T1 group who received a cholesterol screening in 2007 was roughly 10% less. This association translated to roughly 27,000 unscreened beneficiaries.
We found that older beneficiaries in the treated groups were less likely to receive cholesterol screens during the post-Katrina period and that the difference increased over the 3 years. Compared to non-Hispanic whites, blacks in the treated groups were roughly 5% more likely to receive a screen. Surprisingly, we did not observe a shrinkage in the utilization gap between the treated and control groups towards the end of the sample period. This finding suggested that the effects of Katrina on utilization may have been at least somewhat permanent.
Our analysis is most closely related to earlier studies examining health care utilization of diabetics following disasters. Contrary to our findings, immediately after Hurricane Katrina children were largely able to continue their screens.1 However, consistent with our results, during the period immediately following Hurricane Katrina, older residents faced difficulties in obtaining dialysis care and supplies.2 The increased emergency department utilization by diabetics following Hurricane Sandy19,20 likely reflects the inability of those with diabetes to obtain care in the period immediately following the disaster.
Our findings are consistent with many earlier studies that showed decreased utilization of services to control chronic conditions following disasters. For instance, there were decreases in mental health utilization by US military veterans with posttraumatic stress disorder affected by Hurricane Katrina.6 Likewise, the rate of HIV health care services declined following the 2010 earthquake in Haiti.21,22 Asthmatic children affected by Katrina were less likely to get their asthma medications filled.8 These decreases in maintenance services may have contributed to a relatively high proportion of hospitalizations following Hurricane Katrina being due to chronic conditions.23
Limitations
Our study had a number of limitations. While we believed that our numerous groups provided nuanced insight into the effects of Hurricane Katrina, our “purest” control group (C3) was imperfect. While the counties in C3 did not have any FEMA declarations, it was likely that they experienced spillover effects from affected counties. As mentioned above, it is unclear whether the pre-Katrina parallel trends condition held for our regressions. For instance, the coefficients for the T1 and T2 groups were already trending downward before Katrina. Thus, our finding of screening reductions post-Katrina could have reflected the continuation of those trends. However, our findings regarding cholesterol screenings did not share this condition.
Our analysis also was susceptible to potential sample bias if the sample restrictions we imposed materially affected the comparability of the groups. For instance, it was possible that our restriction of having no Medicare Advantage months may have caused the resulting samples to be unrepresentative of the groups, as beneficiaries in Medicare Advantage tend to be healthier than those in traditional Medicare.24 It is also possible that our estimates may have been biased if there were group-wide changes in diabetic condition during the sample period that caused differences in screening rates. Also, Hurricane Katrina was an extreme weather event and may not be representative of other disasters.
Further, we are not able to control for the potential effects of Hurricane Katrina on the operations of health care organizations. Prior studies have found that previous experience with major incidents can have an important effect on the ability of organizations to provide care following a disaster.25 Our data did not allow us to control for this potentially significant aspect.
Implications
Communities often face an array of daunting challenges following a disaster. Their resources may be overwhelmed in the attempt to address immediate and short-term needs, and that may be very costly in terms of time and resources. Even in the best scenario, a successful recovery from short-time issues may lead to exhausted people and resources, and that can lead to long-term effects that may be neglected. Further, these effects may be especially pronounced for vulnerable populations.
Our findings indicate that health care utilization may be an example of a neglected long-term issue. Not addressing utilization challenges may have important negative consequences. Direct costs for the victim can include lower quality of life and potential death. The larger community may also suffer due to higher health care costs and lost productivity.
To mitigate these effects, policy makers and local governments should assess recovery efforts in the longer-term after disasters to determine if unaddressed needs remain. These efforts may include analyzing population health data to identify if any negative effects persist. Corrective steps may include establishing public health clinics in affected areas or working with medical providers to perform outreach to assist victims.
CONCLUSION
We conducted a unique study that utilized administrative data and a fixed-effects regression analysis to investigate the potential long-term effects of disasters on health care utilization. Our analysis of screening rates for seniors with diabetes suggests that those directly affected by Hurricane Katrina were less likely to obtain cholesterol screenings for the 3 years following the storm. In the context of diabetes, our findings suggest that medical care providers should pay special attention to those in disaster-affected areas to ensure that they do not experience disruptions in their preventive care screenings. More generally, our results highlight the potential challenges faced by those with a chronic condition in maintaining their care after a disaster. Future research should investigate other disasters, as well as other health conditions and populations.
Supplementary Material
Acknowledgment
This work was supported by the National Institute on Aging of the National Institutes of Health under award number R03AG050065. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2018.128
Contributor Information
Troy Quast, College of Public Health, University of South Florida, Tampa, Florida.
Lijuan Feng, Department of Economics, University of South Florida, Tampa, Florida.
REFERENCES
- 1.Quast T, Mortensen K. Diabetes care provided to children displaced by Hurricane Katrina. Disaster Med Public Health Prep. 2015;9(5):480–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopp JB, Ball LK, Cohen A, et al. Kidney patient care in disasters: lessons from the hurricanes and earthquake of 2005. CJASN. 2007;2(4):814–824. [DOI] [PubMed] [Google Scholar]
- 3.Velez-Valle EM, Shendell D, Echeverria S, et al. Type II diabetes emergency room visits associated with Hurricane Sandy in New Jersey: implications for preparedness. J Environ Health. 2016;79(2):30. [PubMed] [Google Scholar]
- 4.Lee DC, Gupta VK, Carr BG, et al. Acute post-disaster medical needs of patients with diabetes: emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Res Care. 2016;4(1):e000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polusny MA, Ries BJ, Schultz JR, et al. PTSD symptom clusters associated with physical health and health care utilization in rural primary care patients exposed to natural disaster. J Trauma Stress. 2008;21(1):75–82. [DOI] [PubMed] [Google Scholar]
- 6.Druss B, Henderson K, Rosenheck R. Swept away: use of general medical and mental health services among veterans displaced by Hurricane Katrina. Am J Psychiatry. 2007;164(1):154–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jhung M, Shehab N, Rohrallegrini C, et al. Chronic disease and disasters: medication demands of Hurricane Katrina evacuees. Am J Prev Med. 2007;33(3):207–210. [DOI] [PubMed] [Google Scholar]
- 8.Quast T. Healthcare utilization by children with asthma displaced by Hurricane Katrina. J Asthma. 2018;55(4):416–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thethi TK, Yau CL, Shi L, et al. Time to recovery in diabetes and comorbidities following Hurricane Katrina. Disaster Med Public Health Prep. 2010;4(suppl S1):S33–S38. [DOI] [PubMed] [Google Scholar]
- 10.Inui A, Kitaoka H, Majima M, et al. Effect of the Kobe earthquake on stress and glycemic control in patients with diabetes mellitus. Arch Intern Med. 1998;158(3):274–278. [DOI] [PubMed] [Google Scholar]
- 11.Nishikawa Y, Fukuda Y, Tsubokura M, et al. Managing type 2 diabetes mellitus through periodical hospital visits in the aftermath of the Great East Japan Earthquake disaster: a retrospective case series. PLoS One. 2015;10(5):e0125632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogawa S, Ishiki M, Nako K, et al. Effects of the Great East Japan Earthquake and huge tsunami on glycaemic control and blood pressure in patients with diabetes mellitus. BMJ Open. 2012;2(2):e000830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fonseca VA, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes exacerbation of disparities and long-term consequences. Dia Care. 2009;32(9):1632–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kutner NG, Muntner P, Huang Y, et al. Effect of Hurricane Katrina on the mortality of dialysis patients. Kidney Int. 2009;76(7):760–766. [DOI] [PubMed] [Google Scholar]
- 15.Blake ES, Landsea CW, Gibney EJ, et al. The deadliest, costliest, and most intense United States tropical cyclones from 1851 to 2006 (and other frequently requested hurricane facts). NOAA/National Weather Service, National Centers for Environmental Prediction, National Hurricane Center. http://www.srh.noaa.gov/www/images/tbw/1921/DeadliestHurricanes.pdf. Published 2007. Accessed May 27, 2017. [Google Scholar]
- 16.Groen J, Polivka A. Hurricane Katrina evacuees: who they are, where they are, and how they are faring. Mon Labor Rev Online. 2007;131:32–51. [Google Scholar]
- 17.Federal Emergency Management Agency. Fact Sheet: Individual Assistance Program. https://www.fema.gov/-media-library-data/1502462481273e60375f24bc71e1d3efd6fa18249c54e/FACTSHEET-IndividualAssistance.pdf. Published May 2007. Accessed September 19, 2017.
- 18.Federal Emergency Management Agency. Fact Sheet: Public Assistance Program. Undated. https://www.fema.gov/media-library-data/1497559657642-a01f6ee60e25394fa9a25cae2fd289d5/PublicAssistance-FactSheet-June2017.pdf. Accessed September 19, 2017.
- 19.Velez-Valle EM, Shendell D, Echeverria S, et al. Type II diabetes emergency room visits associated with Hurricane Sandy in New Jersey: implications for preparedness. J Environ Health. 2016;79(2):30. [PubMed] [Google Scholar]
- 20.Lee DC, Gupta VK, Carr BG, et al. Acute post-disaster medical needs of patients with diabetes: emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Res Care. 2016;4(1):e000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walldorf JA, Joseph P, Valles JS, et al. Recovery of HIV service provision post-earthquake. AIDS. 2012;26(11):1431–1436. [DOI] [PubMed] [Google Scholar]
- 22.Puttkammer NH, Zeliadt SB, Balan JG, et al. Before and after the earthquake: a case study of attrition from the HIV antiretroviral therapy program in Haiti. Global Health Action. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4124816/. Published 2014. Accessed April 26, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma AJ, Weiss EC, Young SL, et al. Chronic disease and related conditions at emergency treatment facilities in the New Orleans area after Hurricane Katrina. Disaster Med Public Health Prep. 2008;2(01):27–32. [DOI] [PubMed] [Google Scholar]
- 24.Jason B, Mark D, Ilyana K, et al. How does risk selection respond to risk adjustment? New evidence from the Medicare Advantage Program. Am Econ Rev. 2014;104(10):3335–3364. [DOI] [PubMed] [Google Scholar]
- 25.Seyedin H, Zaboli R, Raviaghi H. Major incident experience and preparedness in a developing country. Disaster Med Public Health Prep. 2013;7(3):313–318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.