Abstract
Objectives
The author discusses current otolaryngological procedures employing the palatopharyngeus muscle, based on the surgical anatomy of the muscle and its neural supply. These techniques should be deeply revised for more conservative, anatomically-based maneuvers.
Methods
Revision of anatomical and surgical research and comments with the provision of a primary concept.
Results
The palatopharyngeus muscle is innervated by the pharyngeal plexus (the vagus and the accessory nerves) with additional fibers from the lesser palatine nerves. The innervation enters the muscle mainly through its lateral border.
Conclusions
The palatopharyngeus muscle has a fundamental role in swallowing and speech. The muscle helps other dilators to maintain upper airway patency. Sphincter pharyngoplasty should be revised as regards its role as a sphincter. Palatopharyngeal procedures for OSA employing the palatopharyngeus muscle should follow the conservative, anatomically-based, and non-neural ablation concept.
Level of evidence
4.
Keywords: Palatopharyngeus muscle, Sphincter pharyngoplasty, Obstructive sleep apnea
Introduction
The palatopharyngeus muscle (PPM) has a pivotal role in proper swallowing and phonation. The muscle contributes to the soft palate’s movement, the pharynx’s shortening, and the hyo-laryngeal complex’s upward elevation movement. PPM is considered the key muscle in pharyngeal surgeries for obstructive sleep apnea (OSA); it has a role in the maintenance of patency of the upper airway (UA) by its activation in response to negative pressure (evident during nose breathing in the supine posture) [1–4].
The importance of PPM in Otolaryngology practice is clear; the muscle has a definite role in many surgeries, including sphincter pharyngoplsty in cases of velopharyngeal insufficiency and various pharyngeal techniques in cases of OSA. Thus, it deserves anatomical, histological, and surgical attention. However, debates still exist as regards the feasibility of various surgical techniques based on the pattern of muscle innervation.
In this commentary, the author tried to discuss some current otolaryngological procedures employing PPM, based on the surgical anatomy of the muscle. The author believes the techniques should be revised for more conservative, anatomically-based maneuvers.
Methods
Anatomy of the palatopharyngeal muscle
A recent cadaver head dissection reported that PPM originated from palatine aponeurosis and then passed laterally and inferiorly to form the palatopharyngeal arch (the posterior tonsillar pillar). Then, the muscle spreads radially (on the inner aspect of the pharyngeal wall) to be inserted into the pharyngeal raphe, the epiglottis, the pyriform fossa, and the thyroid cartilage. It was noticed that the most inferior portion of PPM passed antero-medially, and extended to the inner surface of the cricopharyngeal component of the inferior constrictor muscle to cover its inner surface [1, 2]. Noticeably, there is no general agreement as regards the neural supply of PPM, and debates continue. Researchers reported that the muscle receives innervation from the pharyngeal plexus (PPL). Other reports provided that the muscle is doubly innervated by fibers from the lesser palatine nerves and PPL. This innervation enters the muscle mainly through its lateral border [5–7]. The muscle predominantly consists of type II (fast twitch) fibers; thus, it is characterized by quick contraction but is more fatigable if contracted for long periods. On contraction of PPM, the soft palate moves posteriorly (with adduction of the posterior tonsillar pillars), and the lateral pharyngeal walls move medially, with elevation of the larynx. Thus, PPM could increase the velum’s size, allowing a larger area to contact the posterior pharyngeal wall [2, 8–10]. Figure 1 illustrates the anatomy of the lateral wall of the pharynx.
Fig. 1.
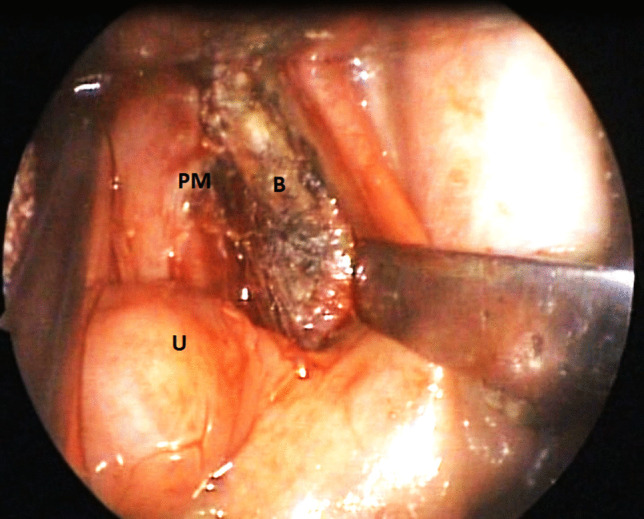
Lateral wall of the pharynx. PM palatopharyngeus muscle, U uvula, B bed of tonsil, the superior constrictor muscle of the pharynx
Discussion
Clinical applications
Swallowing
PPM was found to spread across the inner surface of the cricopharyngeal component of the inferior constrictor muscle, with dense fibrous tissue connecting them. In that way, the two PPMs could elevate the cricopharyngeal component of the inferior constrictor muscle supero-laterally, where the upper oesophageal sphincter (UES) is located. With this notice (and with the pulling forces of the suprahyoid muscles), the UES can be pulled in three different directions. Therefore, PPM might act directly on the UES [2, 8].
Phonation
Many authors believe that PPM acts to lower the soft palate and narrow the pharynx by the medial movement of the lateral pharyngeal walls during speech and swallowing. By its action of elevation of the larynx, the muscle could assist in the phonation of high-pitched sounds. PPM has a fundamental role in velopharyngeal closure. In addition, it has a role in the production of both oral and nasal speech sounds [1, 11–14].
By the middle of the last century, PPM was employed in cases of velopharyngeal insufficiency (VPI) in an operation called sphincter pharyngoplasty (SP). Since its presentation, SP (and its subsequent modifications) has been a cornerstone in the treatment of VPI. SP entails the creation of bilateral superiorly-based palatopharyngeal myo-mucosal flaps; flaps are transposed and sutured to the posterior pharyngeal wall or the soft palate. Postoperatively, the transposed muscle showed movements (perceived as contractions); hence the procedure was termed sphincteric pharyngoplasty. However, this assumption was not proved objectively by EMG studies and patients showed silent inactive flaps (on EMG). The noticed movements were only passive and seemed to result from the contraction of the superior pharyngeal muscles [15–18]. We assume that the primary problem (as regards SP) is that PPM is dissected from its lateral connections and is cut at its inferior ends; this means that the muscle is nearly denervated (the muscle is innervated through its lateral border) and the loss of action would be the result. So, SP would finally give only an inactive fibrous band at the velopharynx.
Role of PPM in OSA
Microscopic examination of PPM showed different muscle fibers in comparison with normal individuals. This change in the fibers’ properties and the disturbance of motor regulation might be important co-factors in abnormal upper airway collapse (allowing a retropalatal collapse) in patients with OSA [1–3].
The recent era of OSA surgery follows more conservative reconstructive techniques rather than aggressive radical soft tissue ablation, aiming at the preservation of pharyngeal function together with the control of OSA. PPM is involved in many palate-pharyngeal procedures and is considered a cornerstone in modern OSA surgeries. Currently, debates are still; a few authors suggest the inferior resection of PPM (superiorly-based flaps), while others favor muscle transposition without resection. Unfortunately, many basic questions would show up; could we resect PPM, how could it be resected, and how far can myofunctional therapy for OSA be effective? Although the resection of PPM might help OSA patients, it could jeopardize the beneficial functions of the muscle; therefore, PPM resection could be a “double-edged sword” in that issue. The author of the current paper follows the non-resection assumption aiming at the widening of the upper airway, with the maintenance of the muscle respiratory activities. Another important factor is that older individuals have a lower laryngeal position, which is independently a risk factor for OSA and might be associated with more severe OSA. Thus, we support the efficacy of myofunctional therapy of PPM in older individuals as it might guard against the descent of the larynx; hence, might prevent OSA in addition to its primary role in preventing dysphagia [2–5, 19–22].
Limitations and recommendations
This report has limitations. First, it presents the author’s assumption; this assumption was based on personal and other researchers’ efforts. However, the author believes that this assumption would open discussions that would eventually contribute to a better understanding of the anatomical and surgical applications of PPM. Second, no patients were included; we think that the idea was delivered without patients’ inclusion. More multi-center research is needed for a proper understanding of that issue.
Conclusion
The palatopharyngeus muscle has a fundamental role in swallowing and speech. The muscle helps other dilators to maintain upper airway patency. Sphincter pharyngoplasty should be revised as regards its role as a sphincter. Palatopharyngeal procedures for OSA employing the palatopharyngeus muscle should follow the conservative, anatomically-based, and non-neural ablation concept.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The author declares no financial support.
Data availability
Data is available upon reasonable request.
Declarations
Conflict of interest
The author declares no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by the author. All procedures performed in studies involving human participants were following the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ezzat AE, El-Shenawy HM. Palatopharyngeus the missing palatal muscles: anatomical and physiological review. Ann Maxillofac Surg. 2015;5(2):226–228. doi: 10.4103/2231-0746.175768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fukino K, Tsutsumi M, Nimura A, Miwa K, Ono T, Akita K. Anatomy of inferior end of palatopharyngeus: its contribution to upper esophageal sphincter opening. Eur Arch Otorhinolaryngol. 2021;278(3):749–754. doi: 10.1007/s00405-020-06437-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Casale M, Moffa A, Pignataro L, Rinaldi V. Palatopharyngeus muscle in pharyngoplasty surgery for OSAS: cut or not to cut? Eur Arch Otorhinolaryngol. 2021;278(7):2657–2658. doi: 10.1007/s00405-021-06761-1. [DOI] [PubMed] [Google Scholar]
- 4.Fukino K, Tsutsumi M, Nimura A, Miwa K, Ono T, Akita K. Reply to “Palatopharyngeus muscle in pharyngoplasty surgery for OSAS: cut or not to cut?”. Eur Arch Otorhinolaryngol. 2021;278(7):2659–2660. doi: 10.1007/s00405-021-06821-6. [DOI] [PubMed] [Google Scholar]
- 5.Shimokawa T, Yi S, Tanaka S. Nerve supply to the soft palate muscles with special reference to the distribution of the lesser palatine nerve. Cleft Palate Craniofac J. 2005;42(5):495–500. doi: 10.1597/04-142r.1. [DOI] [PubMed] [Google Scholar]
- 6.Broomhead IW. The nerve supply of the muscles of the soft palate. Br J Plast Surg. 1951;4:1–15. doi: 10.1016/S0007-1226(51)80002-X. [DOI] [PubMed] [Google Scholar]
- 7.Broomhead IW. The nerve supply of the soft palate. Br J Plast Surg. 1957;10:81–88. doi: 10.1016/S0007-1226(57)80017-4. [DOI] [PubMed] [Google Scholar]
- 8.Huang MH, Lee ST. Anatomic basis of cleft palate and velopharyngeal surgery: implications from a fresh cadaveric study. Plast Reconstr Surg. 1998;101:613–627. doi: 10.1097/00006534-199803000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Seikel JA, King DW, Drumright DG. Anatomy and physiology for speech, language and hearing. 3. New York: Thomson Delmar Learning; 2005. [Google Scholar]
- 10.Stal PS, Lindman R. Characterisation of human soft palate muscles with respect to fibre types, myosins, and capillary supply. J Anat. 2000;197:275–290. doi: 10.1046/j.1469-7580.2000.19720275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fritzell B. The velopharyngeal muscles in speech. Acta Otolaryngol. 1969;250:5–81. [PubMed] [Google Scholar]
- 12.Zemlin WR. Speech and hearing science. 4. Boston: Allyn and Bacon; 1998. [Google Scholar]
- 13.Dickson DR. Normal and cleft palate anatomy. Cleft Palate J. 1972;9:280–293. [PubMed] [Google Scholar]
- 14.Fritzell B. Electromyography in the study of the velopharyngeal function—a review. Folia Phoniatr. 1979;31:93–102. doi: 10.1159/000264155. [DOI] [PubMed] [Google Scholar]
- 15.Ysunza A, Pamplona M. Velopharyngeal function after two different types of pharyngoplasty. Int J Pediatr Otorhinolaryngol. 2006;70:1031–1037. doi: 10.1016/j.ijporl.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 16.Askar SM, Abou-Elsaad TS. A speech nasoendoscopy-based surgeon’s decision for correction of velopharyngeal insufficiency following adenotonsillectomy. Eur Arch Otorhinolaryngol. 2014;271(2):391–398. doi: 10.1007/s00405-013-2572-3. [DOI] [PubMed] [Google Scholar]
- 17.Ysunza A, Pamplona MC, Molina F, Chacón E, Collado M. Velopharyngeal motion after sphincter pharyngoplasty: a videonasopharyngoscopic and electromyographic study. Plast Reconstr Surg. 1999;104(4):905–910. doi: 10.1097/00006534-199909040-00002. [DOI] [PubMed] [Google Scholar]
- 18.Askar SM. Endoscopic-assisted sphincter pharyngoplasty (EASP) Int J Pediatr Otorhinolaryngol. 2013;77(2):170–174. doi: 10.1016/j.ijporl.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Askar SM, Al-Hussain OH, Abd El-Badea A, Abou-Sharkh AA, Awad AM. Suspension-expansion pharyngoplasty: a modified technique for oropharyngeal collapse in obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2023;280(3):1343–1351. doi: 10.1007/s00405-022-07688-x. [DOI] [PubMed] [Google Scholar]
- 20.Sorrenti G, Piccin O. Functional expansion pharyngoplasty in the treatment of obstructive sleep apnea. Laryngoscope. 2013;123(11):2905–2908. doi: 10.1002/lary.23911. [DOI] [PubMed] [Google Scholar]
- 21.Pang KP, Pang EB, Win MT, Pang KA, Woodson BT. Expansion sphincter pharyngoplasty for the treatment of OSA: a systemic review and meta-analysis. Eur Arch Otorhinolaryngol. 2016;273(9):2329–2333. doi: 10.1007/s00405-015-3831-2. [DOI] [PubMed] [Google Scholar]
- 22.Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 2003;113:1961–1968. doi: 10.1097/00005537-200311000-00020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available upon reasonable request.


