Abstract
The transoral endoscopic thyroidectomy vestibular approach (TOETVA) is an innovative technique in thyroid surgery. This review compiles current research on TOETVA, covering its development, anatomical challenges, techniques, selection of suitable patients, results, complications, and future advancements. We performed a comprehensive literature review on PubMed, EMBASE, and Cochrane databases for articles published up to 15th March 2024. The search strategy included a combination of terms focused on “vestibular approach” and “thyroidectomy”. The review underscores the necessity for preoperative planning and careful patient selection to reduce risks and enhance outcomes. It discusses the unique anatomical challenges of TOETVA, such as avoiding mental nerve damage and the complexities involved in creating a subplatysmal space. Outcomes of TOETVA, including surgical duration, complication rates, and recovery times, are compared favorably to traditional methods. The approach is particularly noted for high patient satisfaction and superior cosmetic results. Complications specific to TOETVA, like infection, bleeding, and potential harm to the recurrent laryngeal nerve, are recognized. Future research directions are discussed as well. In summary, TOETVA is a promising alternative for thyroidectomy with excellent cosmetic outcomes and patient satisfaction. Success relies on selective patient criteria, surgical expertise, and continuous research to refine the approach.
Keywords: transoral, endoscopic, thyroidectomy, neck, minimally invasive
1. Introduction
In order to treat thyroid diseases, such as benign nodules, multinodular goiter, and cancers, thyroid surgery is a frequently performed treatment (1). Historically, a thyroidectomy necessitates a cervical incision, which can still be evident even after it is reasonably small and tucked into a skin fold to reduce visibility. This scar may cause psychological distress and unhappiness with the surgical result for certain patients, especially those who have a high concern for esthetic outcomes (2). There is a growing need for scarless surgical treatments, hence many systems for remote access have been developed. These include the retroauricular, transaxillary, and breast approaches, which, although minimizing scarring in the neck, may leave additional scars and can necessitate more extensive dissection (3). For thyroid surgery, the transoral vestibular approach (TOETVA) has emerged as a novel technique that offers a truly scar-free outcome by accessing the thyroid gland through natural orifices, specifically the oral cavity (4). This minimally invasive technique aligns with the principles of natural orifice transluminal endoscopic surgery (NOTES), aiming to reduce postoperative pain, improve cosmetic results, and potentially shorten recovery time (5). Initially introduced in Asia and subsequently adopted in various other regions, TOETVA has garnered attention for its innovative use of the oral vestibule as an entry point for endoscopic or robotic thyroid surgery (6). By avoiding external incisions, the technique provides an excellent cosmetic result, which is particularly appealing in cultures with a strong emphasis on aesthetic outcomes and in patients with a personal preference for avoiding neck scars (7). The transoral vestibular approach is not without challenges, however. It requires careful patient selection, meticulous surgical technique, and a comprehensive understanding of cervical anatomy from an unconventional perspective (8). Additionally, the approach has a distinct set of potential complications that surgeons must be adept at managing (9). This review will provide an in-depth analysis of the vestibular approach for thyroid surgery. It will explore the historical evolution of the technique, anatomical and technical considerations, patient selection criteria, clinical outcomes, complications, and the future direction of this surgical method. By synthesizing the current body of literature, this review aims to offer a valuable resource for surgeons considering the incorporation of TOETVA into their surgical practice and for patients seeking information on scarless thyroidectomy options.
2. Methods
We conducted a comprehensive literature search on PubMed, EMBASE, and Cochrane databases for articles published up to 15th March 2024. The search strategy included a combination of Medical Subject Headings (MeSH) and free-text terms to capture the concepts of “vestibular approach” and “thyroidectomy”. Search terms included “thyroid”, “surgery” “vestibular”, “thyroidectomy”, “minimally invasive”, “surgical”, “TOETVA”. Filters were applied to include articles in English and studies involving human subjects. Studies were included if they reported on the surgical procedure, patient selection, patient outcomes, during and after TOETVA. We considered observational studies, randomized controlled trials (RCTs), case-control studies, cohort studies, and cross-sectional studies. Reviews, meta-analyses, and clinical guidelines were also included to provide context and discuss current recommendations. Case reports, editorials, commentaries, and studies not specifically addressing TOETVA were excluded from the review. Two reviewers independently screened titles and abstracts for relevance, followed by a full-text review to determine eligibility. Discrepancies were resolved through discussion or consultation with a third reviewer.
3. Evolution of TOETVA
The development of the vestibular approach for thyroidectomy is a testament to the surgical community's ongoing effort to reduce the morbidity and improve the aesthetic outcomes associated with traditional thyroid surgery (10). The timeline of this evolution reflects advancements in surgical techniques, patient-centered care, and technological progress in medical instruments. The concept of performing thyroid surgery without a cervical scar was initially met with skepticism, given the complex anatomy and vital structures of the neck. However, the successful application of minimally invasive techniques in other surgical fields, particularly the NOTES procedures, inspired endocrine surgeons to explore similar approaches for thyroid surgery (11). The first documented TOETVA procedures originated in Asia, where there is a significant cultural emphasis on cosmetic outcomes and a preference for avoiding visible scars (12). Surgeons in South Korea and Thailand, led by Dr. W.Y. Chung and Dr. Angkoon Anuwong, respectively, were pioneers in developing and refining this technique (13). In 2016, Dr. Anuwong published the first series of TOETVA procedures, demonstrating the feasibility and safety of this approach (4). Early adopters of the vestibular approach reported on various aspects, including reduced postoperative pain, absence of visible scarring, and high levels of patient satisfaction with the cosmetic results (14). Following these initial successes, there was a concerted effort to standardize the technique, ensuring consistency and reproducibility of results (15). Key steps, such as incision placement in the oral vestibule, creation of the working space, and endoscopic dissection techniques, were meticulously defined (16). The use of specialized retractors and the adaptation of existing endoscopic equipment further refined the TOETVA procedure (17). The introduction of robotic surgery to TOETVA represented a significant milestone, allowing for enhanced dexterity, three-dimensional visualization, and improved ergonomics (18). Although robotic TOETVA is not as widespread due to cost and availability, it has demonstrated benefits in select cases, particularly for surgeons early in their learning curve (19). As the technique gained recognition, surgeons around the world began to adopt and adapt the TOETVA approach to their clinical practices (20). Variations emerged to accommodate different patient anatomies, surgical preferences, and healthcare settings (21). With the increasing number of TOETVA procedures being performed globally, a substantial body of evidence has accumulated, including comparative studies and meta-analyses (22). These studies have provided a more robust understanding of the indications, outcomes, and potential complications associated with the vestibular approach, contributing to its broader acceptance (23). The dissemination of the TOETVA technique has been facilitated by advancements in surgical training and simulation (24). Workshops, cadaveric courses, and virtual reality simulations have become valuable tools for training surgeons in the intricacies of the vestibular approach without compromising patient safety (25). Today, TOETVA is recognized as a viable and effective approach for select patients requiring thyroid surgery (26). Ongoing research focuses on extending the indications, refining patient selection criteria, and enhancing the safety profile of the procedure (15). Future directions also include the development of new instruments and technologies tailored to the unique requirements of transoral thyroid surgery (6). The benefit of transoral endoscopic thyroidectomy is the potential for scar-free surgery (27).
4. Surgical procedure
Before the initiation of the procedure, the patient is carefully evaluated and optimized (24) in order to prevent intraoperative hypotensive events (25, 26). Then, general anesthesia is induced, and the patient is intubated with a specially designed endotracheal tube that allows for intraoperative nerve monitoring. The patient's neck is extended to facilitate the approach to the thyroid gland, and the oral cavity is prepared with antiseptic solution to minimize the risk of infection (15). The TOETVA procedure begins with three incisions: two lateral and one central, all within the lower lip's inner aspect, hidden inside the oral vestibule (6). These incisions are typically less than 1 cm in length and are strategically placed to minimize trauma to oral structures and provide optimal access to the thyroid gland (27). These incisions are used for trocars placement: the 10 mm trocar is central and the two 5 mm trocars are lateral (Figure 1) (28). Blunt dissection is used to create a subplatysmal working space, which is expanded using dilators or insufflation with carbon dioxide to improve visibility and provide room for instrument manipulation. This working space extends from the chin to the sternal notch, and laterally to the sternocleidomastoid muscles on either side. The midline approach helps to minimize the risk of injury to the lateral neurovascular structures (29). The strap muscles are identified and separated along the midline raphe to expose the thyroid gland (16). Careful attention is paid to preserve the integrity and vascular supply of the strap muscles for re-approximation during closure (30). Using laparoscopic instruments through the vestibular incisions, the surgeon begins careful dissection of the thyroid gland (Figure 2) (19). Hemostasis is meticulously maintained using energy devices or clips to control blood vessels (17). The recurrent laryngeal nerve and parathyroid glands are identified and preserved (31). The thyroid lobectomy or total thyroidectomy is performed based on the preoperative indications (32). Dissection of the thyroid lobe began with the pyramidal lobe and continued inferiorly with the division of the isthmus close to the contralateral thyroid lobe using an ultrasonic device (32). After superior pole dissection, the recurrent laryngeal nerve is identified at the insertion and dissected parallel to the trachea and downwards perpendicular to the inferior thyroid artery, near the lower parathyroid gland (33). Then, the thyroid gland was cut close to the thyroid capsule in order to preserve the nerve and lower parathyroid gland (34). If a thyroidectomy is necessary, the same procedure is for the other lobe (35). The indocyanine green (ICG) is useful for locating the parathyroid glands or proofing of the viable glands (36). This could be applied to TOETVA for reducing the rate of hypoparathyroidism (12). Once the thyroid gland or lobes are dissected, they are placed in an endoscopic bag to avoid seeding of the working space and removed through one of the vestibular incisions (37). This may require the gland to be morcellated (cut into smaller pieces) inside the bag, to facilitate removal without enlarging the incision excessively (38). For papillary microcarcinoma patients, central neck lymph node level VI dissection was routinely performed (39). After ensuring complete hemostasis, the strap muscles are reapproximated, and the subplatysmal space is deflated (40). The oral vestibule incisions are then closed with absorbable sutures (41). A drain may be placed in the working space and brought out through the floor of the mouth in some cases, although this practice varies among surgeons (42). A gauze pressure dressing was placed around the chin for 24 h (22). Patients are typically monitored postoperatively for signs of bleeding, infection, or other complications (43). The oral cavity is maintained with antiseptic mouthwash to reduce the risk of infection (44). Postoperative analgesia is managed according to standard protocols (18). The TOETVA procedure requires a significant adjustment in surgical technique compared to traditional cervical thyroidectomy (45). Surgeons must be skilled in endoscopic surgery and familiar with the altered perspective and ergonomics of the transoral approach (13). Modifications to the standard technique may be necessary based on patient anatomy, the extent of the pathology, and intraoperative findings (3).
Figure 1.
Surgical incision for TOETVA.
Figure 2.
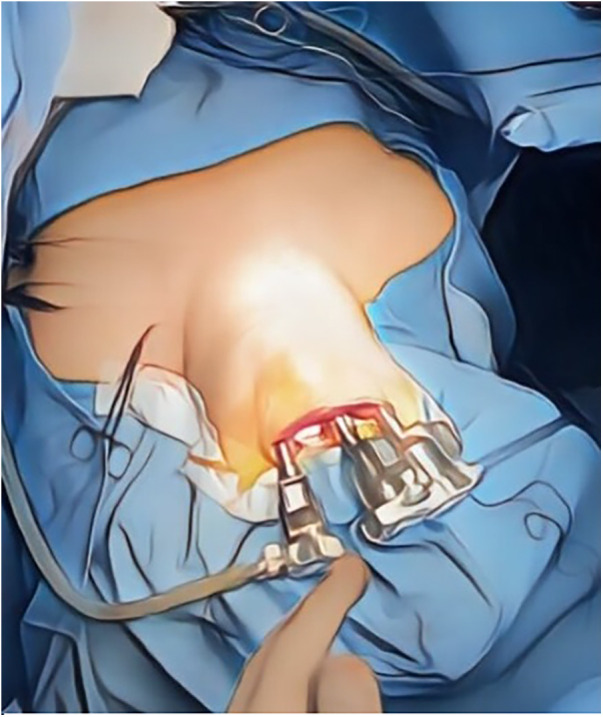
TOETVA procedure.
5. Patient selection
TOETVA is primarily indicated for patients with benign thyroid nodules, small to medium-sized goiters, Graves' disease, and in select cases of papillary thyroid carcinoma when the cancer is small (usually less than 2 cm), without evidence of local invasion or distant metastasis (Table 1) (15, 46).
Table 1.
Indications for TOETVA.
| Type of indication | Specific indication |
|---|---|
| Motivational | Patients must be motivated to avoid a skin incision or an anterior cervical scar |
| Clinical | History of hypertrophic scarring |
| Benign thyroid nodules | |
| Goiters (small to medium-size) | |
| Graves disease | |
| Papillary thyroid carcinoma (no evidence of local invasion or distant metastasis) |
Contraindications to TOETVA include, but are not limited to:
-
•
Large goiters that extend substernally or laterally beyond the neck's carotid sheath (47).
-
•
Previous neck surgery or radiation, which could result in altered anatomy and increased risk of complications due to scar tissue (9).
-
•
Advanced or aggressive cancers that involve surrounding tissues and require extensive resection beyond the gland, as reported in other settings (48).
-
•
Coagulopathy or other conditions that predispose patients to bleeding complications, such as anticoagulant therapy (49).
-
•
Morbid obesity or short neck, which may limit the operative working space and make the procedure technically challenging (50).
5.1. Preoperative assessment
A comprehensive preoperative assessment is crucial for patient selection:
-
•
Ultrasound Evaluation: To assess the size, location, and characteristics of the thyroid nodules or the extent of the goiter (51).
-
•
Fine-Needle Aspiration (FNA): If indicated, to rule out or confirm malignancy in thyroid nodules (52).
-
•
CT/MRI Scans: To further evaluate the thyroid's anatomy and any substernal extension or surrounding tissue involvement (53).
-
•
Laryngoscopy: To assess vocal cord function before surgery, as any preexisting palsy must be documented (32).
Cosmetic concerns are significant for many patients considering thyroid surgery. TOETVA is particularly suitable for patients who prioritize a scar-free neck, as long as they understand the potential risks and benefits of the procedure compared to conventional methods (4). Patients should be provided with detailed information about the TOETVA, including its novelty, the limited long-term data available compared to traditional approaches, potential risks, and postoperative care (33). Informed consent must be obtained after ensuring that the patient has a clear understanding of the information provided (54). The experience and skill level of the surgeon are also critical factors in patient selection. TOETVA should only be performed by surgeons who have undergone specialized training and have demonstrated proficiency in the technique (44). The healthcare facility must be equipped with the necessary endoscopic equipment and have staff trained in the specific perioperative care requirements of TOETVA patients (19).
6. Outcomes and possible complications
The primary measure of surgical success for TOETVA is the complete removal of the targeted thyroid tissue with preservation of vital structures such as the recurrent laryngeal nerves and parathyroid glands (4). Operative time is longer for TOETVA when compared to conventional thyroidectomy, particularly during the initial learning curve (44). As surgeons become more experienced, operative times tend to decrease (15). Complications are a critical metric for any surgical procedure. Despite the minimally invasive nature of the procedure, there is still a risk of bleeding that may require intervention (16). Also, since the oral cavity is not a sterile environment, there is a risk of surgical site infection despite prophylactic antibiotics (6). Moreover, transient or permanent hypoparathyroidism can occur if the parathyroid glands are inadvertently damaged or their blood supply is compromised (28). Lastly, recurrent laryngeal nerve injury and mental nerve injury can lead to temporary or permanent hoarseness or voice changes, as well as numbness or altered sensation in the chin and lower lip (55, 56). Conversion to open surgery is also possible due to difficulties encountered during the procedure (12). Postoperative pain may be less with TOETVA compared to traditional approaches, which can contribute to a quicker recovery and shorter hospital stay (57). Patients often report less discomfort due to the absence of a cervical incision (13). Cosmetic satisfaction is reported to be high among patients who undergo TOETVA, as the procedure leaves no visible neck scars (7). This is particularly significant for patients who place a high value on aesthetic outcomes (58). Patient satisfaction surveys and quality-of-life assessments post-surgery often reflect this positive aspect of the procedure (59). Voice and swallowing function are important considerations in thyroid surgery. TOETVA has been shown to have similar or improved functional outcomes when compared to traditional approaches, although more long-term data is required for a definitive assessment (43). In cases of thyroid cancer, the adequacy of oncologic resection is of utmost concern. A summary of the characteristics of the included studies and the outcomes considered is provided in Table 2. Early studies show promising results, with TOETVA providing similar rates of tumor-free margins compared to conventional thyroidectomy (60). Long-term follow-up is necessary to assess recurrence rates and survival (61). Several studies found the overall incidence of recurrent laryngeal nerve injury of 3.1%–5.9% for TOETVA to be comparable to the incidence of 2.1%–11.8% for open thyroidectomy (15, 62). The low incidence of recurrent laryngeal nerve injury in TOETVA can be explained by the reduced incidence of traction injury and the use of IONM (63). During TOETVA, the recurrent laryngeal nerve is usually identified at its insertion site and released first after division of the Berry's ligament (13). This reduces the risk of traction injury.
Table 2.
Characteristics of the included studies..
| Study | Year | Design | N. TOETVA patients | Outcomes |
|---|---|---|---|---|
| Chen et al. | 2021 | Retro PSM | 99 | 1–3, 5–9 |
| Lee et al. | 2023 | Retro PSM | 142 | 1, 3–6, 8, 9 |
| Anuwong et al. | 2018 | Retro PSM | 216 | 1, 2, 5–8 |
| Hong et al. | 2020 | Retro PSM | 82 | 1, 3–9 |
| Han et al. | 2020 | Retro PSM | 50 | 1, 3, 9 |
| Kasemsiri et al. | 2020 | Pro CST | 32 | 1, 2, 5, 7, 9, 10 |
| Wang et al. | 2020 | Retro PSM | 80 | 1–4, 9 |
| Liu et al. | 2021 | Retro PSM | 78 | 1–10 |
| Sun et al. | 2022 | Retro PSM | 28 | 1, 3–7, 9 |
| Nguyen et al. | 2022 | Pro CST | 60 | 1,2,6–10 |
| Li et al. | 2023 | Retro PSM | 101 | 1–9 |
| You et al. | 2021 | Retro PSM | 186 | 1, 3–9 |
| Lee et al. | 2023 | Retro PSM | 100 | 1, 3–7 |
PSM, retrospective propensity score-matched comparison; CST, prospective cross-sectional study. Outcomes: 1, operative time; 2, blood loss; 3, retrieved lymph nodes; 4, metastatic lymph nodes; 5, recurrent laryngeal nerve palsy; 6, hypoparathyroidism; 7, other complications (including mental nerve injury, surgical site infection, skin flap perforation, chyle leakage, seroma, hematoma, etc.); 8, postoperative pain; 9, postoperative hospital stay; 10, cosmetic satisfaction.
7. Future directions
-
•
Technological Advancements
Further development of specialized instruments and endoscopic equipment may enhance the precision and safety of TOETVA. Innovations such as flexible endoscopes or robotic systems with better ergonomics could allow for more delicate dissection and easier manipulation within the confined spaces of the neck.
-
•
Enhanced Visualization
Improvements in visualization technology, such as high-definition cameras and augmented reality (AR), could provide surgeons with more detailed views of the surgical field, potentially reducing the risk of complications and improving surgical accuracy.
-
•
Broadening Indications
As the technique becomes more refined and safety profiles are better understood, the indications for TOETVA may expand. This could include its application in larger goiters, more advanced thyroid cancers, or preoperative surgery in selected cases.
-
•
Training and Education
Establishing standardized training programs and certification processes will be essential to ensure that surgeons are adequately prepared to perform TOETVA. Simulation models, cadaveric workshops, and virtual reality training platforms may become more integral to the educational process.
-
•
Comparative Effectiveness Research
More rigorous comparative studies and randomized controlled trials are needed to evaluate the effectiveness of TOETVA against traditional and other minimally invasive approaches. Long-term outcomes, including recurrence rates in cancer patients and quality of life measures, will be important areas of investigation.
-
•
Patient-Reported Outcomes
Greater emphasis on patient-reported outcomes will help to understand the true impact of TOETVA from the patient's perspective. This includes assessing satisfaction with cosmetic results, pain, recovery time, and overall quality of life after surgery.
-
•
Cost-Effectiveness Analysis
Assessing the cost-effectiveness of TOETVA compared to traditional thyroidectomy and other minimally invasive approaches will be important, considering factors such as operative time, length of hospital stay, and the need for specialized equipment.
-
•
International Collaboration and Registries
Building international collaborations and establishing registries for TOETVA can facilitate the sharing of knowledge, techniques, and outcomes. This global approach can accelerate the accumulation of evidence and help standardize the procedure internationally.
-
•
Genomic and Personalized Medicine
Advancements in genomics and personalized medicine may influence the selection of patients for TOETVA, tailoring the approach based on individual tumor genetics or patient-specific anatomical considerations.
-
•
Artificial Intelligence (AI) and Machine Learning
AI and machine learning algorithms could be developed to assist in preoperative planning, intraoperative decision-making, and postoperative monitoring, potentially improving the precision and outcomes of TOETVA.
-
•
Non-Surgical Alternatives
Research into non-surgical alternatives, such as radiofrequency ablation or percutaneous ethanol injection for benign nodules, may also influence the role of TOETVA in the management of thyroid pathologies.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Author contributions
LL: Conceptualization, Supervision, Writing – original draft. AZ: Conceptualization, Supervision, Writing – original draft. AC: Investigation, Methodology, Writing – original draft. MD: Writing – original draft. AM: Investigation, Writing – review & editing. SC: Investigation, Writing – review & editing. AC: Investigation, Methodology, Writing – original draft, Writing – review & editing. SD: Conceptualization, Methodology, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Gharib H, Papini E, Garber JR, Duick DS, Harrell RM, Hegedüs L, et al. American Association of clinical endocrinologists, American college of endocrinology, and associazione medici endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules–2016 update. Endocr Pract. (2016) 22(5):622–39. 10.4158/EP161208.GL [DOI] [PubMed] [Google Scholar]
- 2.Arora A, Swords C, Garas G, Chaidas K, Prichard A, Budge J, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: a prospective cohort study. Int J Surg. (2016) 25:38–43. 10.1016/j.ijsu.2015.11.021 [DOI] [PubMed] [Google Scholar]
- 3.Berber E, Bernet V, Fahey TJ, III, Kebebew E, Shaha A, Stack BC, Jr, et al. American Thyroid association statement on remote-access thyroid surgery. Thyroid. (2016) 26(3):331–7. 10.1089/thy.2015.0407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg. (2016) 40(3):491–7. 10.1007/s00268-015-3320-1 [DOI] [PubMed] [Google Scholar]
- 5.Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. (2008) 22(8):1871–5. 10.1007/s00464-007-9734-6 [DOI] [PubMed] [Google Scholar]
- 6.Anuwong A, Sasanakietkul T, Jitpratoom P, Ketwong K, Kim HY, Dionigi G, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc. (2018) 32(1):456–65. 10.1007/s00464-017-5705-8 [DOI] [PubMed] [Google Scholar]
- 7.Shan L, Liu J. A systemic review of transoral thyroidectomy. Surg Laparosc Endosc Percutan Tech. (2018) 28(3):135–8. 10.1097/SLE.0000000000000512 [DOI] [PubMed] [Google Scholar]
- 8.Zhang D, Park D, Sun H, Anuwong A, Tufano R, Kim HY, et al. Indications, benefits and risks of transoral thyroidectomy. Best Pract Res Clin Endocrinol Metab. (2019) 33(4):101280. 10.1016/j.beem.2019.05.004 [DOI] [PubMed] [Google Scholar]
- 9.Camenzuli C, Schembri Wismayer P, Calleja Agius J. Transoral endoscopic thyroidectomy: a systematic review of the practice so far. JSLS. (2018) 22(3):e2018.00026. 10.4293/JSLS.2018.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dionigi G, Bacuzzi A, Lavazza M, Inversini D, Pappalardo V, Tufano RP, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): from A to Z. Surg Technol Int. (2017) 30:103–12. [PubMed] [Google Scholar]
- 11.Benhidjeb T, Wilhelm T, Harlaar J, Kleinrensink GJ, Schneider TA, Stark M. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc. (2009) 23(5):1119–20. 10.1007/s00464-009-0347-0 [DOI] [PubMed] [Google Scholar]
- 12.Chai YJ, Kim HY, Kim HK, Jun SH, Dionigi G, Anuwong A, et al. Comparative analysis of 2 robotic thyroidectomy procedures: transoral versus bilateral axillo-breast approach. Head Neck. (2017) 39(5):886–92. 10.1002/hed.24694 [DOI] [PubMed] [Google Scholar]
- 13.Anuwong A, Kim HY, Dionigi G. Transoral endoscopic thyroidectomy using vestibular approach: updates and evidences. Gland Surg. (2017) 6(3):277–84. 10.21037/gs.2017.03.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Razavi CR, Vasiliou E, Tufano RP, Russell JO. Learning curve for transoral endoscopic thyroid lobectomy. Otolaryngol Head Neck Surg. (2018) 159(4):625–9. 10.1177/0194599818795881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anuwong A, Ketwong K, Jitpratoom P, Sasanakietkul T, Duh QY. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg. (2018) 153(1):21–7. 10.1001/jamasurg.2017.3366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang D, Fu Y, Dionigi G, Pontin A, Caruso E, Pino A, et al. Human cadaveric model for studying the preservation of mental nerve during transoral endoscopic thyroidectomy. Surg Radiol Anat. (2020) 42(1):55–62. 10.1007/s00276-019-02306-8 [DOI] [PubMed] [Google Scholar]
- 17.Park JO, Park YJ, Kim MR, Sun DI, Kim MS, Koh YW, et al. Gasless transoral endoscopic thyroidectomy vestibular approach (gasless TOETVA). Surg Endosc. (2019) 33(9):3034–9. 10.1007/s00464-019-06826-7 [DOI] [PubMed] [Google Scholar]
- 18.Tartaglia N, Iadarola R, Di Lascia A, Cianci P, Fersini A, Ambrosi A. What is the preferred entry site for transoral robotic thyroidectomy? Updates Surg. (2020) 72(2):473–80. [Google Scholar]
- 19.Kim HK, Chai YJ, Dionigi G, Berber E, Tufano RP, Kim HY. Transoral robotic thyroidectomy for papillary thyroid carcinoma: perioperative outcomes of 100 consecutive patients. World J Surg. (2018) 42(6):1878–84. 10.1007/s00268-018-04877-w [DOI] [PubMed] [Google Scholar]
- 20.Russell JO, Razavi CR, Shaear M, Chen LW, Lee AH, Ranganath R, et al. Transoral vestibular thyroidectomy: current state of affairs and considerations for the future. J Clin Med. (2019) 8(9):1337. 10.3390/jcm8091337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dionigi G, Chai YJ, Tufano RP, Anuwong A, Kim HY. Transoral endoscopic thyroidectomy via a vestibular approach: why and how? Endocrine. (2018) 59(2):275–9. 10.1007/s12020-017-1451-x [DOI] [PubMed] [Google Scholar]
- 22.Jiang WJ, Yan PJ, Zhao CL, Si MB, Tian W, Zhang YX, et al. Comparison of transoral endoscopic thyroidectomy vestibular approach, total endoscopic thyroidectomy via areola approach, and conventional open thyroidectomy: a retrospective analysis of safety, trauma, and feasibility of central neck dissection in the treatment of papillary thyroid carcinoma. Surg Endosc. (2020) 34(1):268–74. 10.1007/s00464-019-06762-6 [DOI] [PubMed] [Google Scholar]
- 23.Lira RB, Ramos AT, Nogueira RM, de Carvalho GB, Russell JO, Tufano RP, et al. Transoral thyroidectomy (TOETVA): complications, surgical time, and learning curve. Oral Oncol. (2020) 110:104871. 10.1016/j.oraloncology.2020.104871 [DOI] [PubMed] [Google Scholar]
- 24.La Via L, Vasile F, Perna F, Zawadka M. Prediction of fluid responsiveness in critical care: current evidence and future perspective. Trends Anaesth Crit Care. (2024) 54:101316. 10.1016/j.tacc.2023.101316 [DOI] [Google Scholar]
- 25.La Via L, Santonocito C, Bartolotta N, Astuto M, Sanfilippo F. α-2 agonists vs. fentanyl as adjuvants for spinal anesthesia in elective cesarean section: a meta-analysis. Minerva Anestesiol. (2023) 89(5):445–54. 10.23736/S0375-9393.22.16969-5 [DOI] [PubMed] [Google Scholar]
- 26.Messina A, La Via L, Milani A, Astuto M, Cecconi M. Spinal anesthesia and hypotensive events in hip fracture surgical repair in elderly patients: a meta-analysis. J Anesth Analg Crit Care. (2022) 2(1):19. 10.1186/s44158-022-00047-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dionigi G, Rovera F, Boni L, Castano P. Commentary on transoral endoscopic thyroidectomy vestibular approach (TOETVA). Surg Technol Int. (2017) 31:1–3. [PubMed] [Google Scholar]
- 28.Fernandez-Ranvier G, Meknat A, Guevara DE, Taye A, Suh H, Inabnet WB, III. Transoral endoscopic thyroidectomy vestibular approach. JSLS. (2019) 23(4):e2019.00036. 10.4293/JSLS.2019.00036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tesseroli MAS, Spagnol M, Sanabria Á. Transoral endoscopic thyroidectomy by vestibular approach (TOETVA): initial experience in Brazil. Rev Col Bras Cir. (2018) 45(5):e1951. 10.1590/0100-6991e-20181951 [DOI] [PubMed] [Google Scholar]
- 30.Udelsman R, Anuwong A, Oprea AD, Rhodes A, Prasad M, Sansone M, et al. Trans-oral vestibular endocrine surgery: a new technique in the United States. Ann Surg. (2016) 264(6):e13–6. 10.1097/SLA.0000000000002001 [DOI] [PubMed] [Google Scholar]
- 31.Jitpratoom P, Ketwong K, Sasanakietkul T, Anuwong A. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves’ disease: a comparison of surgical results with open thyroidectomy. Gland Surg. (2016) 5(6):546. 10.21037/gs.2016.11.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dionigi G, Lavazza M, Bacuzzi A, Inversini D, Pappalardo V, Tufano RP, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): anatomical landmarks and minimally invasive surgical technique. Surg Technol Int. (2017) 30:34–8. [PubMed] [Google Scholar]
- 33.Dionigi G, Tufano RP, Russell J, Kim HY, Piantanida E, Anuwong A, et al. Transoral thyroidectomy: advantages and limitations. J Endocrinol Invest. (2020) 43(4):381–8. 10.1007/s40618-019-01124-4 [DOI] [PubMed] [Google Scholar]
- 34.Sasanakietkul T, Jitpratoom P, Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a case report of Graves’ disease. Gland Surg. (2019) 8(3):278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Celik S, Makay O, Yoruk MD, Yilmaz B, Ertan Y, Ozdemir M, et al. A comparison of complications in patients who underwent total thyroidectomy: conventional technique vs. transoral endoscopic thyroidectomy vestibular approach (TOETVA). Chirurgia (Bucur. (2020) 115(1):92–100. [Google Scholar]
- 36.Liu ZQ, Liu J, Xie QP, Huang TP, Zhang YF, Jiang J. The clinical value of indocyanine green fluorescence imaging in transoral endoscopic thyroidectomy via vestibular approach-monitored parathyroid protection technology. J Surg Oncol. (2019) 120(7):1296–9. [Google Scholar]
- 37.Wang M, Chen B, Zang C, Xu S, Wang K. The techniques in the specimen extraction of transoral endoscopic thyroidectomy vestibular approach (TOETVA): a systematic review. Eur Arch Otorhinolaryngol. (2019) 276(12):3279–84. [Google Scholar]
- 38.Chen YH, Kim HY, Anuwong A, Huang TS. Transoral endoscopic thyroidectomy vestibular approach versus open thyroidectomy: a case-matched study on long-term quality of life. Surg Endosc. (2019) 33(12):4271–7. [Google Scholar]
- 39.Sun H, Zheng H, Wang Z, Zeng Q, He G, Zhang Y, et al. Comparison of transoral endoscopic thyroidectomy vestibular approach, total endoscopic thyroidectomy via areola approach, and conventional open thyroidectomy: a propensity score matching analysis of surgical outcomes. Surg Endosc. (2020) 34(4):1837–45. [DOI] [PubMed] [Google Scholar]
- 40.Fu J, Luo Y, Chen Q, Lin F, Hong X, Kuang P, et al. Transoral endoscopic thyroidectomy: review of 81 cases in a single institute. J Laparoendosc Adv Surg Tech A. (2018) 28(3):286–91. 10.1089/lap.2017.0435 [DOI] [PubMed] [Google Scholar]
- 41.Park JO, Kim MR, Kim DH, Lee DK, Kim SH. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res. (2020) 98(2):73–9. 10.4174/astr.2016.91.5.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim HY, Chai YJ, Dionigi G, Anuwong A, Richmon JD. Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surg Endosc. (2018) 32(2):688–94. 10.1007/s00464-017-5724-5 [DOI] [PubMed] [Google Scholar]
- 43.Yi JW, Yoon SG, Kim HS, Yu HW, Kim SJ, Chai YJ, et al. Transoral endoscopic surgery for papillary thyroid carcinoma: initial experiences of a single surgeon in South Korea. Ann Surg Treat Res. (2018) 95(2):73–9. 10.4174/astr.2018.95.2.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sivakumar T, Amizhthu RA. Transoral endoscopic total thyroidectomy vestibular approach: a case series and literature review. J Minim Access Surg. (2018) 14(2):118. 10.4103/jmas.JMAS_3_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Razavi CR, Tufano RP. Transoral endoscopic thyroidectomy: nascent experimental technique or reality? In: Terris DJ, Singer MC, editors. Minimally Invasive and Robotic Thyroid and Parathyroid Surgery. Cham: Springer; (2019). p. 219–30. [Google Scholar]
- 46.Razavi CR, Russell JO, Tufano RP. Indications and contraindications to transoral thyroidectomy. Ann Thyroid. (2020) 5:3. 10.21037/aot.2020.03.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang TY, Chou SY, Chao WC, Lin YH, Cheng YC, Kim HY, et al. Indication and contraindication of transoral thyroidectomy. Formos J Surg. (2020) 53(1):1–7. 10.4103/fjs.fjs_29_19 [DOI] [Google Scholar]
- 48.Sartori E, Franchi M, Capelli G, Ratti M, Scambia G. Cancer in pregnancy: proposal of an Italian multicenter study. Gynecol Oncol Group Ital Soc Gynecol Obstet. (2018) 30(3):37–44. [Google Scholar]
- 49.Sanfilippo F, La Via L, Murabito P, Pappalardo F, Astuto M. More evidence available for the use of bivalirudin in patients supported by extracorporeal membrane oxygenation. Thromb Res. (2022) 211:148–9. 10.1016/j.thromres.2022.02.007 [DOI] [PubMed] [Google Scholar]
- 50.Pérez-Soto RH, Ponce de León-Ballesteros G, Montalvo-Hernández J, Sierra-Salazar M, Pantoja Millán JP, Herrera-Hernández MF, et al. Transoral endoscopic thyroidectomy by vestibular approach-initial experience and comparative analysis in the first reported Mexican cohort. J Laparoendosc Adv Surg Tech. (2019) 29(12):1526–31. 10.1089/lap.2019.0537 [DOI] [PubMed] [Google Scholar]
- 51.Chai YJ, Kim HY, Dionigi G, Anuwong A. Preoperative assessment of transoral approach for endoscopic thyroidectomy. J Endocr Surg. (2018) 18(3):132–41. [Google Scholar]
- 52.Dionigi G, Lavazza M. Transoral endoscopic thyroidectomy: indications, techniques, and safety. In: Townsend CM, Evers M, editors. Atlas of Endocrine Surgical Techniques. Cham: Springer; (2017). p. 17–26. [Google Scholar]
- 53.Park JO, Anuwong A, Kim MR, Sun DI, Kim MS, Dionigi G, et al. Transoral endoscopic thyroid surgery in a Korean population. Surg Endosc. (2019) 33:1–9. 10.1007/s00464-018-6481-9 [DOI] [PubMed] [Google Scholar]
- 54.Dionigi G, Boni L. Transoral endoscopic thyroidectomy: technique and outcomes (TOETO) study. In: Terris DJ, Singer MC, editors. Minimally Invasive and Robotic Thyroid and Parathyroid Surgery. Cham: Springer; (2019). p. 207–18. [Google Scholar]
- 55.Chai YJ, Chung JK, Anuwong A, Dionigi G, Kim HY, Hwang KT, et al. Transoral endoscopic thyroidectomy for papillary thyroid microcarcinoma: initial experience of a single surgeon. Ann Surg Treat Res. (2017) 93(2):70–5. 10.4174/astr.2017.93.2.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Park JO, Sun DI, Kim MS, Choi EC. Mental nerve injury after transoral thyroidectomy: a systematic review. Gland Surg. (2021) 10(3):1016. [Google Scholar]
- 57.Razavi CR, Khadem MGA, Fondong A, Nguyen TAV, Clark JH, Richmon J, et al. Early outcomes in transoral vestibular thyroidectomy: robotic versus endoscopic techniques. In: Ha P, editor. Head and Neck. Vol. 40. United States: Wiley; (2018). p. S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Inabnet WB, III. Robotic thyroidectomy: must we drive a luxury sedan to arrive at our destination safely? Thyroid. (2018) 28(8):973–4. 10.1089/thy.2012.2210.com2 [DOI] [PubMed] [Google Scholar]
- 59.Wang Y, Yu X, Wang P, Miao C, Xie Q, Yan H, et al. Implementation of intraoperative neuromonitoring for transoral endoscopic thyroid surgery: a preliminary report. J Laparoendosc Adv Surg Tech. (2020) 30(1):47–51. 10.1089/lap.2016.0291 [DOI] [PubMed] [Google Scholar]
- 60.Chen YH, Kim HY, Anuwong A, Huang TS. Transoral endoscopic thyroidectomy vestibular approach versus open thyroidectomy for differentiated thyroid cancer: a meta-analysis. Gland Surg. (2019) 8(6):646. [Google Scholar]
- 61.Dionigi G, Bacuzzi A, Lavazza M, Inversini D, Boni L, Rausei S, et al. Transoral endoscopic thyroidectomy: preliminary experience in Italy. Updates Surg. (2017) 69(2):225–34. 10.1007/s13304-017-0436-x [DOI] [PubMed] [Google Scholar]
- 62.Wang C, Feng Z, Li J, Yang W, Zhai H, Choi N, et al. Endoscopic thyroidectomy via a breast approach: a review of 1,026 cases. Surg Laparosc Endosc Percutan Tech. (2020) 30(5):388–93.32675753 [Google Scholar]
- 63.Barczynski M, Konturek A, Cichon S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. (2009) 96(3):240–6. 10.1002/bjs.6417 [DOI] [PubMed] [Google Scholar]



