Abstract
Formerly regarded as a rare disease, bronchiectasis is increasingly recognised. A renewed interest in this disease has led to significant progress in bronchiectasis research. Randomised clinical trials (RCTs) have demonstrated the benefits of airway clearance techniques, inhaled antibiotics and long-term macrolide therapy in bronchiectasis patients. However, the heterogeneity of bronchiectasis remains one of the most challenging aspects of management. Phenotypes and endotypes of bronchiectasis have been identified to help find “treatable traits” and partially overcome disease complexity. The goals of therapy for bronchiectasis are to reduce the symptom burden, improve quality of life, reduce exacerbations and prevent disease progression. We review the pharmacological and non-pharmacological treatments that can improve mucociliary clearance, reduce airway inflammation and tackle airway infection, the key pathophysiological features of bronchiectasis. There are also promising treatments in development for the management of bronchiectasis, including novel anti-inflammatory therapies. This review provides a critical update on the management of bronchiectasis focusing on treatable traits and recent RCTs.
Shareable abstract
Bronchiectasis is a rapidly developing field. This state of the art review highlights recent advancements in bronchiectasis management and emerging therapies. https://bit.ly/3yiipC0
Introduction
Bronchiectasis is defined radiographically by permanent dilatation of the bronchi and clinically by cough, sputum production and recurrent chest infections [1, 2]. Previously considered an orphan disease [3], bronchiectasis is now recognised to be a common disease. In 2013, it was reported that prevalence had increased by 40% since 2003 and was as high as 566 per 100 000 persons [4–7]. The increased prevalence potentially results from increased awareness among physicians and a wider application of chest computed tomography (CT) scans in clinical practice. Prevalence data from most European and non-European countries have not been updated since 2013. Thus, the prevalence is likely to be much higher at the present time. Bronchiectasis is associated with high medical costs and increased mortality rate [4, 8–10].
The improved awareness of this disease has stimulated marked progress in bronchiectasis research. Multinational, multicentre, prospective cohorts are now established worldwide [11–16], advancing our understanding of bronchiectasis. An increase in translational research has improved disease understanding in areas such as airway inflammation, the microbiome and mucociliary dysfunction. Furthermore, randomised controlled trials (RCTs) have provided a higher level of evidence for the clinical management of bronchiectasis. In this review, we provide a state of the art overview of recent advancements in bronchiectasis management, including therapies under development.
Search strategy
The authors conducted a systematic review of the PubMed database up to February 2024 using the search term “bronchiectasis” with “treatment”, “antibiotics”, “physiotherapy”, “macrolide”, “anti-inflammatory”, “inhaled”, “bronchodilators”, “mucolytics”, “Random*”, “management” and “exacerbation”. 5957 studies were initially identified, and eligibility was assessed by H. Choi and J.D. Chalmers. The search was supplemented by reviewing treatment options identified in the published international bronchiectasis guidelines and conducting updated searches for additional studies [17–21]. Developing treatment strategies were identified through searches of clinical trial registries.
Pathophysiology of bronchiectasis and goals of treatment
Traditionally, the pathophysiology of bronchiectasis has been explained by the “vicious cycle” model [22]. Impaired mucociliary clearance in dilated bronchi results in the accumulation of airway secretions that make an airway environment prone to chronic bacterial infection. In turn, this triggers an inflammatory response that causes abnormal airway remodelling and structural damage [23]. If the process occurs in a stepwise manner, it may be logical to stop the cycle by intervening with one of the three components: abnormal mucus, chronic infection or inflammation. However, treatment strategies targeting one component frequently fail in clinical practice.
In this regard, a “vicious vortex” model was proposed, and the model incorporated complex interactions among the three components of bronchiectasis [24]. For example, Pseudomonas infection does not only induce neutrophilic inflammation, but also directly affects mucociliary clearance through the action of ciliotoxins, such as pyocyanin, which slows down ciliary beat frequency [25, 26]. Bronchiectasis is an inflammatory disease and is associated with an imbalance between pro- and anti-inflammatory signalling, leading to the recruitment of inflammatory cells and, ultimately, a self-perpetuating cycle of inflammation [23, 27].
Treatment aims, therefore, are to improve mucus clearance from the airways, reduce inflammation and prevent and reduce the impact of infection. Successful treatment can mitigate the effects of lung damage, reduce airflow limitation, improve exercise capacity and reduce exacerbations.
Initial assessment
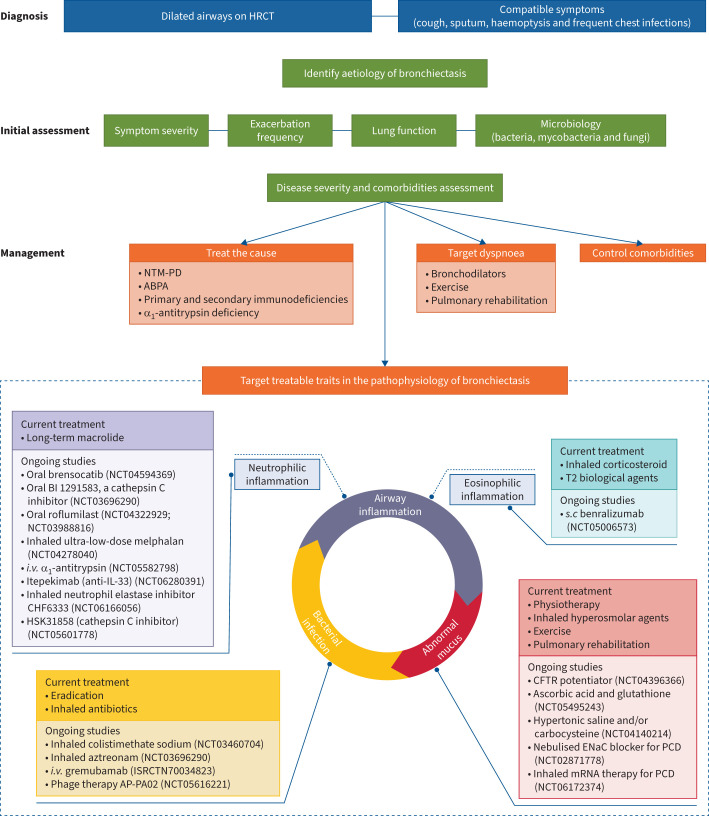
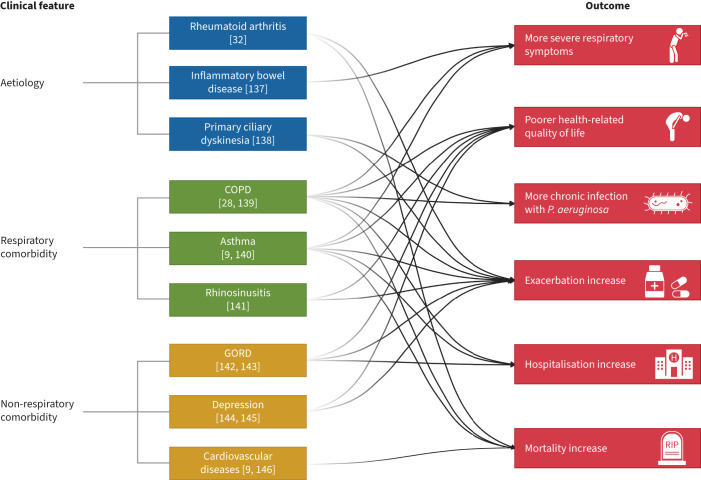
Patients with bronchiectasis are heterogeneous and, thus, their treatment must be individualised. Figure 1 summarises the principles of management of bronchiectasis. Following diagnosis based on high-resolution CT and the presence of the clinical syndrome [2], initial assessment of patients includes an assessment of the severity of symptoms, the frequency of exacerbations, lung function and microbiology, including bacterial, fungal and mycobacterial cultures. Patients with bronchiectasis frequently have comorbidities, with a median of four comorbidities per patient in one large international study. Comorbidities confer an increased risk of exacerbation or mortality [28]. Assessment of disease severity can include utilisation of validated severity tools such as the Bronchiectasis Severity Index and E-FACED [29, 30], but should also take into account parameters not included in the tools such as comorbidities, extent of symptoms and the underlying cause. Identifying patients at higher risk of deterioration is critical to guide initial therapy (figure 2).
FIGURE 1.
Summary of management points and ongoing studies (ClinicalTrials.gov and ISRCTN) in bronchiectasis. HRCT: high-resolution computed tomography; NTM-PD: non-tuberculous mycobacterial pulmonary disease; ABPA: allergic bronchopulmonary aspergillosis; IL: interleukin; i.v.: intravenous; T2: type 2; s.c.: subcutaneous; CFTR: cystic fibrosis transmembrane conductance regulator; ENaC: epithelial sodium channel; PCD: primary ciliary dyskinesia.
FIGURE 2.
Clinical conditions associated with worse outcomes in patients with bronchiectasis. GORD: gastro-oesophageal reflux disease; P. aeruginosa: Pseudomonas aeruginosa.
Identifying and treating the underlying cause
The first step in bronchiectasis management is to identify an aetiology that may be treatable or influence management. Non-tuberculous mycobacterial (NTM) pulmonary disease, allergic bronchopulmonary aspergillosis (ABPA) and primary and secondary immunodeficiency are examples of underlying causes with specific treatments [17, 18, 31], while rheumatoid arthritis and primary ciliary dyskinesia (PCD) are examples of conditions that are associated with worse outcomes and differences in clinical phenotype which require a change in management [32, 33]. Table 1 shows details on the diagnosis and treatment of NTM pulmonary disease, ABPA, immunodeficiency and α1-antitrypsin deficiency in bronchiectasis patients. Testing for other underlying causes arises from the detailed history. Patients with onset of disease during childhood or with specific clinical features such as infertility, severe rhinosinusitis/nasal polyps, severe disease accompanied by infection with Pseudomonas aeruginosa or Staphylococcus aureus or extrapulmonary features such as malabsorption may have a genetic cause of bronchiectasis such as PCD or cystic fibrosis (CF). A recent study reported that genome sequencing revealed an underdiagnosis of PCD in bronchiectasis where 12% of patients with severe bronchiectasis were found to have PCD [33]. Although specific treatment for PCD has not yet been established, its identification is important for more intensive airway clearance, management of upper airway disease, fertility counselling and cardiac investigations [34]. CF is infrequently diagnosed in adults but the availability of highly effective modulator therapy mandates that these cases are not missed. Although aetiological testing was performed by the treating clinician based on the testing recommended by consensus guidelines [17, 18], 38% of patients still had idiopathic bronchiectasis in a European multicentre cohort study [35]. Moreover, in a large proportion of aetiology, such as post-infective bronchiectasis, specific management targeting aetiology itself does not exist. Hence, the next step is to target the “treatable traits” of bronchiectasis: impaired mucociliary clearance, bacterial infection and airway inflammation (figure 1).
TABLE 1.
Diagnosis and treatment of treatable aetiologies in bronchiectasis
| Aetiology | Diagnosis | Treatment | Comments |
|---|---|---|---|
| NTM pulmonary disease [17, 18, 133, 134] | Sputum culture for mycobacteria Microbiological test results compatible with NTM pulmonary disease: 1) the same NTM species is isolated in ≥2 sputum cultures, 2) isolated in ≥1 bronchial wash or lavage or 3) biopsy with mycobacterial histopathological features plus positive culture for NTM (or ≥1 sputum or bronchial washings that are culture positive for NTM) |
Combination of antibiotics for 12 months after sputum culture conversion Decided based on clinical symptoms, progression of radiological signs and knowledge of the infecting NTM species |
ERS 2017 and BTS 2019 guidelines recommend mycobacterial sputum cultures in patients with bronchiectasis ATS/ERS/ESCMID/IDSA 2020 clinical practice guidelines for the treatment of NTM pulmonary disease |
| ABPA [17, 18, 135] | Total serum IgE test Aspergillus-specific IgG test Aspergillus-specific IgE test (or skin prick tests for Aspergillus) |
Systemic corticosteroids Antifungal agents |
ERS 2017 and BTS 2019 guidelines recommend ABPA testing in all patients with bronchiectasis |
| Immunodeficiency [17, 18] | Serum IgA, IgM and IgG Serum IgG subclass Peripheral blood lymphocyte subpopulations (including T-, B- and NK-cells) Pneumococcal IgG to vaccine response |
Immunoglobulin replacement | ERS 2017 and BTS 2019 guidelines recommend serum IgA, IgM and IgG testing in all patients with bronchiectasis BTS 2019 guideline recommends pneumococcal IgG to vaccine response |
| A1AT deficiency [17, 18, 136] | Serum A1AT A1AT genetic testing |
Intravenous augmentation of A1AT in countries where this is available | BTS 2019 guideline recommends A1AT deficiency testing in patients with coexisting basal panacinar emphysema ERS 2017 guideline states the presence of basal emphysema or early-onset airflow obstruction could suggest the need to exclude A1AT deficiency Portuguese 2016 guideline recommends A1AT deficiency testing in all patients with bronchiectasis (estimated prevalence is 1:2191 in Portugal) |
NTM: non-tuberculous mycobacterial; ERS: European Respiratory Society; BTS: British Thoracic Society; ATS: American Thoracic Society; ESCMID: European Society of Clinical Microbiology and Infectious Diseases; IDSA: Infectious Diseases Society of America; ABPA: allergic bronchopulmonary aspergillosis; NK: natural killer; A1AT: α1-antitrypsin.
Impaired mucociliary clearance
Airway clearance
The marked abnormalities in the mucus of bronchiectasis patients mandate that airway clearance is an absolute necessity in bronchiectasis management. Compared with healthy controls, mucus in bronchiectasis patients has higher mucin concentrations (both MUC5B and MUC5AC), and thus higher percent solids, higher osmotic pressure and increased elasticity and viscosity [36]. Furthermore, the abnormal mucus properties result in local hypoxia at the bronchial mucosa which further incites inflammation, increase in mucin concentration and worsen mucus properties [37]. Consequently, international guidelines recommend all patients with bronchiectasis receive instruction in airway clearance techniques taught by respiratory physiotherapists [17, 18, 38]. Unfortunately, evidence for this important aspect of care is somewhat lacking. Trials of airway clearance techniques are challenging to perform and as a result the majority of studies to date are small. Murray et al. [39] performed a randomised crossover trial in 20 patients who did not practice regular chest physiotherapy and compared 3 months of twice-daily airway clearance using an oscillatory positive expiratory pressure (PEP) device versus no physiotherapy. Upon study completion, regular airway clearance revealed significant improvements in the Leicester Cough Questionnaire (LCQ) score (median 1.3 improvement; p=0.002) and St George's Respiratory Questionnaire (SGRQ) total score (median 7.8 improvement; p=0.004), increased sputum volume and improved exercise capacity [39]. In addition, several small RCTs compared usual airway clearance, including the active cycle of breathing technique and autogenic drainage, with PEP devices, including Acapella (Smiths Medical, London, UK), Flutter (Scandipharm, Birmingham, AL, USA) and bubble-PEP [40–44]. Regular airway clearance resulted in increased sputum expectoration and improved health-related quality of life (HRQoL) in patients with bronchiectasis regardless of the clearance method.
A recent RCT provided more long-term evidence for airway clearance. Munoz et al. [45] performed an RCT comparing 22 patients who underwent ELTGOL (slow expiration with the glottis opened in a lateral posture) twice a day for 12 months and 22 who performed placebo exercises. Despite the small sample size, the ability to gather long-term data and the ability to have a placebo control make this an important study in the airway clearance field. The ELTGOL group showed higher sputum volume (primary outcome), clinically significant improvement in the SGRQ and LCQ scores (p<0.001 for both) and reduced exacerbation (p=0.042) compared with those in the placebo group [45]. Notably, the results of the study emphasise that long-term airway clearance can ameliorate the clinical course of patients with bronchiectasis, beyond reducing daily symptoms and improving HRQoL.
Overall, studies have shown mixed results regarding which airway clearance technique is superior. This is likely due to the heterogeneity of bronchiectasis patients with regard to varying airway calibre, unique sputum properties and individual respiratory strength. From this perspective, the authors recommend that airway clearance management be tailored to the patient's needs, as the most effective airway clearance technique is one the patient will use consistently and successfully over time.
Airway clearance alone may be sufficient to manage patients’ symptoms and improve their quality of life, but many patients have ongoing symptoms or exacerbations despite effective airway clearance. In this situation, it is recommended to add additional symptomatic and/or preventative treatments in a stepwise manner until disease control is achieved.
Inhaled hyperosmolar agents and mucolytics
Mucoactive agents improve mucus hydration, reduce sputum viscosity and/or stimulate cough to aid mucus clearance. Available agents include oral mucolytic agents and nebulised hyperosmolar agents (mannitol and hypertonic saline). Oral mucolytics such as N-acetylcysteine, carbocysteine and erdosteine have achieved some success in the management of COPD [46] and are now being studied in bronchiectasis patients. Regarding nebulised hyperosmolar agents, small RCTs have compared hypertonic and isotonic saline as adjuncts to physiotherapy and revealed that hypertonic saline was more likely to ease sputum expectoration, improve lung function and enhance HRQoL [47–49]. However, an RCT investigating their long-term effects showed that nebulised hypertonic and isotonic saline had similar effects on exacerbation, sputum colonisation, HRQoL and forced expiratory volume in 1 s (FEV1) over 12 months [50]. These results suggest that isotonic saline may benefit patients who cannot tolerate hypertonic saline. Notably, nebulised human recombinant DNase, although effective in CF, was poorly tolerated, ineffective and reduced FEV1 in an RCT of bronchiectasis patients [51].
Inhaled dry mannitol powder was examined in two double-blind RCTs. The first study compared 231 patients on 320 mg of mannitol twice daily and 112 on a placebo for 12 weeks, followed by an open-label extension over 52 weeks to assess safety [52]. The study showed increased sputum weight in favour of mannitol, but no significant difference in the SGRQ. Because it was unclear whether the differences in sputum weight resulted from higher antibiotic use in the control group, a subsequent RCT focusing on exacerbations was conducted. The second study set the rate of exacerbations over 1 year as the primary outcome and enrolled patients who had two or more exacerbations in the previous 12 months [53]. The 52-week study included 233 patients who received 400 mg of mannitol twice daily and 228 who received a placebo. However, its primary end-point was not met (rate ratio of exacerbation 0.92, 95% CI 0.78–1.08; p=0.3) [53]. Despite its failure to achieve the primary end-point, post hoc analysis provided some insights. Gao et al. [54] classified patients enrolled in the study according to symptom burden using the SGRQ (>70: high symptom burden; 40–70: moderate; <40: low). In highly symptomatic patients, the proportion of patients remaining exacerbation-free for 12 months of treatment was significantly higher in the mannitol group (32.7% versus 14.6%; rate ratio 2.84, 95% CI 1.40–5.76; p=0.003) than in the placebo group; however, no benefit was evident in those with lower symptom burden [54]. These results emphasise the importance of a personalised medicine treatment strategy in bronchiectasis. Therapies seem to have more measurable benefits in highly symptomatic patients than in a larger undifferentiated bronchiectasis cohort.
Pulmonary rehabilitation and exercise tolerance
Exercise improves shortness of breath, reduces fatigue and raises endurance in bronchiectasis patients. Patients with significant breathlessness and those who cannot exercise independently should be referred for pulmonary rehabilitation. As in airway clearance, randomised trials of pulmonary rehabilitation in bronchiectasis are small but show a benefit. An 8-week pilot RCT that compared 30 bronchiectasis patients randomised to either pulmonary rehabilitation plus chest physiotherapy or chest physiotherapy alone demonstrated significantly improved exercise tolerance, including incremental shuffle walk (56.7 m; p=0.03) and endurance walk (193.3 m; p=0.01) tests, and HRQoL, including SGRQ and LCQ (8 and 2.6, respectively; p<0.001 for both) in patients who received pulmonary rehabilitation [55]. Remarkably, the improved outcomes persisted for 12 weeks after the pulmonary rehabilitation concluded. A subsequent RCT included 85 bronchiectasis patients: 42 randomised to 8 weeks of exercise training versus 43 controls. Exercise training increased both incremental shuttle and 6-min walk distance compared with the controls, although these improvements were not sustained at 6 or 12 months [56]. Additionally, exercise training reduced the exacerbation frequency (median 1 versus 2; p=0.012) and prolonged the time to first exacerbation (8 versus 12 months; p=0.047) compared with the control group [56].
A recent prospective observational study reinforced the importance of physical activity in bronchiectasis; it enrolled 64 bronchiectasis patients and objectively monitored their activity using armbands [57]. Patients who walked ≤6290 steps per day or spent ≥7.8 h per day in sedentary behaviour at baseline had an increased risk of bronchiectasis-related hospitalisation at 1-year follow-up [57]. Taken together, exercise should be emphasised in bronchiectasis patients to extend their exercise capacity, improve HRQoL and reduce exacerbations. Exercise must be continued to maintain long-term benefits [38, 58, 59].
Bacterial infection
Rationale
The rational for short- and long-term antibiotics is based on two scientific findings: 1) high airway bacterial loads correlate with airway and systemic inflammation and a greater risk of exacerbation in bronchiectasis patients [60], and 2) short- and long-term antibiotic treatments are associated with reductions in bacterial load and airway and systemic inflammation [60]. Among pathogens of chronic bacterial infection, P. aeruginosa infection, in particular, is associated with significantly worse outcomes in bronchiectasis patients. In a meta-analysis of 21 observational cohort studies (n=3683), P. aeruginosa infection correlated with higher mortality (OR 2.95, 95% CI 1.98–4.40), increased hospitalisations (OR 6.57, 95% CI 3.19–13.51) and exacerbations (mean difference 0.97 year−1, 95% CI 0.64–1.30 year−1) compared with infection with other pathogens or none [61]. These results were replicated in a European multicentre bronchiectasis study (n=2596), in which the prevalence of chronic P. aeruginosa infection was 15% [62]. However, the study showed that P. aeruginosa infection was independently associated with mortality primarily in patients with frequent exacerbations (hazard ratio (HR) 2.03, 95% CI 1.36–3.03) [62]. The frequent exacerbator with chronic P. aeruginosa infection is one of the most severe clinical phenotypes in bronchiectasis and some RCTs on inhaled antibiotics targeted this population.
The roles of other bacteria have also been examined in bronchiectasis patients. In a retrospective observational study of 167 patients, chronic Stenotrophomonas maltophilia infection conferred more exacerbations (rate ratio 1.42, 95% CI 0.96–2.12) and hospitalisations (rate ratio 2.08, 95% CI 1.00–4.29) than in patients without the organism [63]. Staphylococcus aureus was examined in a US registry study involving 830 bronchiectasis patients in which the prevalence was 11% [64]. Patients with S. aureus had more frequent exacerbations and poorer lung function than those with no prior S. aureus or Gram-negative infection; however, they had less frequent exacerbations and better lung function than those with Gram-negative infection [64]. Thus, P. aeruginosa and other Gram-negative organisms are the most clinically important pathogens in bronchiectasis. Naturally, this has resulted in the development of eradication and inhaled antibiotic therapy for bronchiectasis. Regular sputum cultures during both clinical stability and at exacerbations are important to guide therapy and identify new infection with P. aeruginosa.
New methods of detecting bacterial infection
Microbiome studies using bacterial 16S rRNA gene sequencing have provided more insight into bronchiectasis by characterising the abundance and diversity of microbial species and demonstrating a diverse microbial environment, while such information cannot be provided by traditional culture-dependent microbiology. In a recent microbiome study of 281 bronchiectasis patients by Dicker et al. [65], individual patient microbiome profiles were relatively stable over time, during exacerbations and during disease stability, consistent with previous microbiome studies [66, 67]. The study revealed that patients with dominant Pseudomonas in the microbiome profiles were at increased risk of all-cause mortality (HR 3.12, 95% CI 1.33–7.36) and had more frequent exacerbations (incidence rate ratio (IRR) 1.69, 95% CI 1.07–2.67) than patients with other dominant genera. Furthermore, the reduced microbiome diversity, assessed by α diversity (within-sample microbiome differences), correlated with increased disease severity, lower FEV1 and more severe symptoms [65].
A recent study also used similarity network fusion approaches and metagenomics to integrate bacterial, fungal and viral data in sputum samples from 217 bronchiectasis patients [68]. In addition to reduced diversity, the study revealed that patients at the greatest risk of exacerbation have less complex microbial co-occurrence networks and a higher degree of antagonistic interactions in their airway microbiota [68]. These provocative results suggest that the relationships between bacteria in the bronchiectasis airway may be as, or more, important than the mere presence or absence of a single microbial group. Manipulating microbiomes by means other than antibiotics, probiotics and controlling host response in microbial environment [69, 70] will have therapeutic implications in the future.
Eradication
The European Respiratory Society (ERS) and British Thoracic Society (BTS) guidelines for adult bronchiectasis suggest that patients with a new isolation of P. aeruginosa should be offered eradication antibiotic treatment, despite low quality of evidence [17, 18, 71–73]. A recent systematic review and meta-analysis of observational studies reported that eradication treatment was associated with a 40% rate of clearing P. aeruginosa at 12 months. Efficacy was greater when systemic antibiotics were combined with an inhaled antibiotic (48% eradication rate) compared with systemic antibiotics alone (27% eradication rate) [74]. Therefore, current treatment recommendations suggest administration of a susceptibility guided oral fluoroquinolone or intravenous antipseudomonal antibiotics either with or followed by an inhaled antibiotic for 6 weeks to 3 months as an eradication regimen. A prospective randomised study of eradication therapy compared with no eradication treatment and testing of different eradication regimens is warranted.
Inhaled antibiotics
Long-term suppressive use of inhaled antibiotics has been the most actively investigated therapeutic agent strategy for bronchiectasis in clinical trials. Inhaled antibiotics have the advantage of delivering higher concentrations of drugs to the airway, reducing systemic absorption and side-effects compared with oral or i.v. antibiotics [75]. The current evidence for the use of inhaled antibiotics, including ciprofloxacin, aztreonam, tobramycin, gentamicin and colistin, in bronchiectasis is summarised in table 2 [76–88].
TABLE 2.
Summary of randomised controlled trials (RCTs) of inhaled antibiotics for bronchiectasis
| Agent and study | Subjects (n) | Study design | Primary outcome | Duration | Study population | Main results | Safety |
|---|---|---|---|---|---|---|---|
|
Ciprofloxacin DPI Wilson et al. (2013) [76] |
A: 60 P: 64 |
Phase 2 double-blind RCT | Bacterial load | 84 days (28-day treatment with follow-up) | ≥2 exacerbations in previous year; culture positive for target microorganisms | Mean difference in bacterial load −3.62 versus −0.27 log10CFU·mL−1 (p<0.001); no significant differences in proportion of patients with exacerbations (36.7% versus 39.1%; p=0.6) and SGRQ (mean difference −3.56; p=0.059) | 10% of patients developed resistance (MIC >4 mg·L−1) in the ciprofloxacin group; no difference in adverse events between groups |
|
Ciprofloxacin DPI De Soyza et al. (2018) RESPIRE 1 [77] |
14-day on/off A: 137 P: 68 28-day on/off A: 141 P: 70 |
Phase 3 double-blind RCT | Time to first exacerbation, frequency of exacerbations | 12 months (14- or 28-day on/off-treatment cycles) | ≥2 exacerbation in previous year; culture positive for predefined microorganisms | 14-day on/off cycle: significantly prolonged time to first exacerbation (median >336 versus 186 days; HR 0.53, 97.5% CI 0.36–0.80; p=0.0005); reduced frequency of exacerbation (IRR 0.61, 97.5% CI 0.40–0.91; p=0.0061); 28-day on/off cycle: no significant differences in primary end-points | No difference in adverse events between groups |
|
Ciprofloxacin DPI Asakamit et al. (2018) RESPIRE 2 [78] |
14-day on/off A: 176 P: 88 28-day on/off A: 171 P: 86 |
Phase 3 double-blind RCT | Time to first exacerbation, frequency of exacerbations | 12 months (28-day on/off-treatment cycles) | ≥2 exacerbations in previous year; culture positive for predefined microorganisms | Missed primary end-point: prolonged time to first exacerbation (HR 0.87, 95% CI 0.62–1.21; p=0.40 in 14-day on/off and HR 0.71, 99% CI 0.39–1.27; p=0.051 in 28-day on/off) and reduced frequency of exacerbations (IRR 0.83, 95% CI 0.59–1.17; p=0.29 in 14-day on/off and IRR 0.55, 99% CI 0.30–1.02; p=0.001 in 28-day on/off) | No difference in adverse events between groups |
|
Liposomal ciprofloxacin Serisier et al. (2013) ORBIT-2 [79] |
A: 20 P: 20 |
Phase 2 double-blind RCT | Bacterial load after first 28-day treatment cycle with intervening 28-day off periods | 24 weeks (three 28-day treatment cycles) | P. aeruginosa-colonised patients; ≥2 exacerbations in previous 12 months | Reduction in P. aeruginosa bacterial load −4.2 versus −0.08 log10CFU·mL−1 (p=0.002); reduced number of exacerbations in the active treatment group (OR 0.2, 95% CI 0.04–0.89; p=0.027) | No significant difference in MICs to ciprofloxacin at day 28; no increase in adverse events |
|
Liposomal ciprofloxacin Haworth et al. (2019) ORBIT-3 and ORBIT-4 [80] |
ORBIT-3 A: 183 P: 95 ORBIT-4 A: 206 P: 98 |
Phase 3 double-blind RCT | Time to first exacerbation | 48 weeks (six 28-day on/off-treatment cycles) | ≥2 exacerbations in previous year; chronic P. aeruginosa infection | Median time to first exacerbation: 230 versus 158 days (HR 0.72, 95% CI 0.53–0.97; p=0.032) in ORBIT-4; 214 versus 136 days (HR 0.99, 95% CI 0.71–1.38; p=0.97) in ORBIT-3; and 222 versus 157 days (HR 0.82, 95% CI 0.65–1.02; p=0.074) in a pooled analysis of both trials | No difference in adverse events between groups |
|
Aztreonam Barker et al. (2014) AIR-BX1 and AIR-BX2 [81] |
AIR-BX1 A: 134 P: 132 AIR-BX2 A: 136 P: 138 |
Two phase 3 double-blind RCTs | QOL-B score at week 4 | Two 28-day treatment courses with alternating 28 days off treatment | Positive sputum for P. aeruginosa or other Gram-negative organisms (excluding H. influenzae); FEV1 >20% predicted; chronic sputum production | No difference in QOL-B at week 4 (mean difference 0.8, 95% CI −3.1–4.7; p=0.7 in AIR-BX1 and 4.6, 95% CI 1.1–8.2; p=0.011 in AIR-BX2); no difference in QOL-B in both studies at week 12 (p=0.56 in both studies); no difference in time to first exacerbation | Adverse events leading to discontinuation: AIR-BX1 22% versus 6%; AIR-BX2 10% versus 5% |
|
Tobramycin Barker et al. (2000) [82] |
A: 37 P: 37 |
Phase 2 double-blind RCT | P. aeruginosa bacterial load at week 4 | 6 weeks (28-day treatment) | P. aeruginosa-colonised patients | Significant reduction in P. aeruginosa load (mean difference 4.56 log10CFU·mL−1; p<0.01); 13/37 cleared P. aeruginosa from sputum; no significant change in FEV1 (p=0.41) | Increased dyspnoea, chest pain and wheezing; new resistance to tobramycin in 4/36 |
|
Tobramycin Guan et al. (2022) TORNASOL [83] |
A: 167 P: 172 |
Phase 3 double-blind RCT | P. aeruginosa bacterial load and QOL-B Respiratory symptoms score on day 29 | 16 weeks (two cycles of 28 days on/off treatment) | ≥1 exacerbations in previous 2 years; chronic P. aeruginosa infection | P. aeruginosa bacterial load mean difference 1.74 log10CFU·mL−1 (p<0.001); QOL-B Respiratory symptom score mean difference 7.9 (p<0.001) | Adverse events leading to discontinuation: 6.2% (tobramycin) versus 2.8% (placebo) |
|
Tobramycin Terpstra et al. (2022) BATTLE [84] |
A: 26 P: 26 |
Phase 3 double-blind RCT | Frequency of exacerbation | 12 months | ≥2 exacerbations in previous year; culture positive for predefined microorganisms | Missed primary end-point: rate ratio 0.74, 95% CI 0.49–1.14 (p=0.15) | 8.8% of tobramycin group discontinued study due to respiratory symptoms in first 4 weeks |
|
Tobramycin inhalation powder Loebinger et al. (2021) iBEST [85] |
A: 86 P: 21 |
Phase 2 double-blind RCT | P. aeruginosa bacterial load on day 29 | Treatment for 16 weeks plus follow-up for 8 weeks | P. aeruginosa-colonised patients | Primary end-point was met in all three doses: P. aeruginosa bacterial load (log10CFU·mL−1) −2.5 at 84 mg (p=0.0004), −2.8 at 140 mg and −3.8 at 224 mg (p=0.0001 for all) | 8.8% of tobramycin group discontinued study due to respiratory symptoms in first 4 weeks |
|
Gentamicin Murray et al. (2011) [86] |
A: 27 P: 30 |
Single-blind RCT | Bacterial load | 12 months | Patients colonised with any pathogens in at least three sputum samples in the previous 12 months; 2 exacerbations in the previous year; able to tolerate test dose of gentamicin; FEV1 >30% predicted; ex-smokers of >1 year; not on long-term antibiotics | Significant difference in bacterial load at 12 months (2.69 versus 7.67 log10CFU·mL−1; p<0.0001); reduction in exacerbations (median 0 in gentamicin group versus 1.5 in saline group; p<0.0001); improved SGRQ and LCQ scores; reduced airway inflammation | Bronchospasm in 21.9%; two withdrawals; elevated serum gentamicin levels required dose reduction in one patient; no resistant isolates detected |
|
Colistin Haworth et al. (2014) [87] |
A: 73 P: 71 |
Phase 3 double-blind RCT | Time to first exacerbation | 6 months | P. aeruginosa-colonised patients (≥2 positive cultures in 12 months) and within 21 days of completing antipseudomonal antibiotics for exacerbation | Missed primary end-point (colistin 165 days versus placebo 111 days; p=0.11); improved SGRQ (mean difference −10.5; p=0.006); improved time to first exacerbation in patients taking >80% of doses | Five (7%) patients developed bronchoconstriction leading to discontinuation; no resistant strains at follow-up |
DPI: dry powder inhaler; A: active; P: placebo; SGRQ: St George's Respiratory Questionnaire; MIC: minimum inhibitory concentration; HR: hazard ratio; IRR: incident rate ratio; P. aeruginosa: Pseudomonas aeruginosa; QOL-B: Quality of Life Bronchiectasis; H. influenzae: Haemophilus influenzae; FEV1: forced expiratory volume in 1 s; LCQ: Leicester Cough Questionnaire.
A decade of phase 2 trials was followed by several large international phase 3 trials: AIR-BX, RESPIRE and ORBIT. The AIR-BX trial investigated aztreonam, an inhaled antibiotic licensed for CF treatment. AIR-BX1 (n=266) and AIR-BX2 (n=274) randomised patients to aztreonam or placebo over two treatment cycles of 28 days, with an off-treatment cycle in between [81]. The primary outcome was symptom improvement, measured using the Respiratory symptom domain of the Quality of Life Bronchiectasis (QOL-B) questionnaire after the first 28-day treatment. The primary outcome was only reached in AIR-BX2 (mean difference 4.6, 95% CI 1.1–8.2; p=0.011), and secondary end-points such as exacerbation were negative in both trials. Moreover, intolerance due to worsening dyspnoea and cough was a major issue. Active treatment was discontinued in 27 (20%) out of 134 aztreonam-treated patients in AIR-BX1 and in 10 (7%) out of 135 patients in AIR-BX2.
RESPIRE investigated a dry powder inhaled (DPI) formulation of ciprofloxacin in two identically designed trials: RESPIRE-1 (n=416) and RESPIRE-2 (n=521). Each trial studied 14- and 28-day on/off-treatment cycles of ciprofloxacin DPI administered twice daily versus placebo in a 2:1 allocation over a 48-week period [77, 78]. These trials included patients with P. aeruginosa and other bacteria, whereas most other inhaled antibiotic trials included only patients with P. aeruginosa. The primary outcomes were time to first exacerbation and frequency of exacerbations. Primary outcomes were only reached in the 14-day arm of RESPIRE-1: significantly prolonged time to first exacerbation (HR 0.53, 97.5% CI 0.36–0.80; p=0.0005) and reduced frequency of exacerbation (IRR 0.61, 97.5% CI 0.40–0.91; p=0.0061). However, these end-points were not met in the 28-day arm of RESPIRE-1 or in either arm of RESPIRE-2.
The ORBIT trials investigated liposomal formulations of ciprofloxacin, which aimed to improve tolerability through liposomal encapsulation of the drug, thus reducing the amount of free drug in contact with the pulmonary epithelium [79]. In phase 3 trials, ORBIT-3 (n=278) and ORBIT-4 (n=304) compared liposomal ciprofloxacin administered once daily with a placebo in a 2:1 ratio over 48 weeks [80]. The trials comprised six 56-day treatment cycles, with each cycle consisting of a 28 day on/off-treatment period. There was a significant prolongation of time to first exacerbation, a primary end-point, in ORBIT-4 (HR 0.72, 95% CI 0.53–0.97; p=0.032); however, this end-point was not met in either ORBIT-3 or pooled analysis of both trials.
More recently, three RCTs have investigated inhaled tobramycin in two different formulations: inhalation solution (TORNASOL and BATTLE studies) and dry powder (iBEST study). The TORNASOL trial (n=339), conducted in China, compared tobramycin inhalation solution and normal saline over 56 days (28 days on/off treatment) [83]. The study met its predefined co-primary end-point of a greater reduction in P. aeruginosa bacterial load (adjusted mean difference 1.74 log10CFU·mL−1; p<0.001) and greater improvement in the Respiratory symptom domain of the QOL-B questionnaire (adjusted mean difference 7.91; p<0.001) on day 29. The BATTLE study (n=58) also compared tobramycin inhalation solution and placebo for 1 year [84]. The primary end-point of exacerbation frequency was not met (rate ratio 0.74, 95% CI 0.49–1.14; p=0.15). The iBEST phase 2 trial (n=107) investigated the efficacy of tobramycin inhalation powder, delivered by TOBI Podhaler (Novartis, Basel, Switzerland), and showed a reduction in P. aeruginosa bacterial load at all three doses; the higher the dose, the greater the reduction in bacterial load from baseline to day 29 (−2.5 log10CFU·mL−1 at 84 mg, −2.8 log10CFU·mL−1 at 140 mg and −3.8 log10CFU·mL−1 at 224 mg) (p<0.0001 for all) [85]. Overall, inhaled tobramycin was well tolerated, with the majority of study patients in these three studies achieving 88–94% compliance. The finding that inhaled tobramycin was well tolerated conflicts with the early phase 2 trial by Barker et al. [82] which showed that although inhaled tobramycin significantly reduced P. aeruginosa bacterial load, it was poorly tolerated and decreased FEV1. The PROMIS trials of inhaled colistin have not yet been published but have been reported in abstract form, with PROMIS-I (ClinicalTrials.gov: NCT03093974) reporting a significant benefit of treatment [89] and PROMIS-II (ClinicalTrials.gov: NCT03460704) awaiting full results.
The inconsistent results of recent inhaled antibiotic trials may be due to differences in patient selection or a lack of statistical power. Several trial programmes have shown discordant results in replicating phase 3 studies. A secondary analysis of the AIR-BX trial revealed improved symptoms in patients with high bacterial loads [90], which may guide the commencement of inhaled antibiotics in the future. Additionally, symptoms worsen during “off periods” when antibiotics are administered 28 days on and 28 days off, suggesting continuous administration may achieve better disease control [91–93]. We have recently reported a meta-analysis of 20 studies including 3468 participants. Overall, inhaled antibiotics were shown to be efficacious with a significant reduction in exacerbation frequency (rate ratio 0.78, 95% CI 0.68–0.91) and a much larger estimated reduction in severe exacerbations (rate ratio 0.48, 95% CI 0.31–0.74). Inhaled antibiotics were also associated with an improvement in symptoms measured using the QOL-B questionnaire and SGRQ [88]. However, potential downsides of this treatment include an increased treatment burden, such as inhalation time, and a higher risk of emergent antibiotic resistance. In real-world practice, inhaled antibiotics were used in approximately 8% of the EMBARC registry cohort (n=16 963) and the rate varied between 2% and 9% according to different European regions [35]. Predictive clinical parameters and/or biomarkers are needed to identify which patients will best respond to inhaled antibiotics.
Airway inflammation
Rationale and new methods of measuring airway inflammation
Recent advancements in molecular techniques have shed light on airway inflammation, which is an important axis in the pathophysiology of bronchiectasis. An observational study measured sputum neutrophil elastase activity in 381 bronchiectasis patients at baseline and during exacerbations [94]. Neutrophil elastase activity was significantly increased during exacerbations (p=0.001) and correlated with a higher frequency of exacerbations over a 3-year follow-up period (p<0.001). The key role of neutrophilic inflammation was also demonstrated in a proteomic study showing neutrophil extracellular traps and their components are key mediators of disease severity and predictive of exacerbations [95]. The integral role that neutrophilic inflammation plays in bronchiectasis pathophysiology is the rationale for a novel drug class, cathepsin C/dipeptidyl peptidase-1 (DPP1) inhibitors, currently in clinical trial that directly targets neutrophilic inflammation [96]. With the optimism that such novel drugs will soon become clinically available, the need of a point-of-care neutrophil elastase assay comes to the forefront. A lateral flow neutrophil elastase activity assay device to rapidly identify patients with bronchiectasis at an increased risk of airway infection and future exacerbation is under development [97]. Additionally, a point-of-care test measuring sputum myeloperoxidase, an abundant protein in neutrophils, showed that myeloperoxidase reflected the exacerbation status of bronchiectasis [98].
Long-term macrolide
Macrolide therapy is highly effective in reducing the frequency of exacerbations in bronchiectasis, believed to be due to its anti-inflammatory properties, although it is also possible that macrolides affect other constituents of the microbiome or quorum sensing in P. aeruginosa [68, 99, 100]. Thus, both the ERS and BTS bronchiectasis guidelines recommend long-term macrolide therapy for frequent exacerbators and those with chronic P. aeruginosa infection who have not improved with inhaled antibiotics [17, 18]. The benefit of chronic macrolide therapy was shown in three double-blind RCTs: EMBRACE, BLESS and BAT [101–103]. Subsequently, an individual patient data meta-analysis of the three trials (n=341) showed that macrolides reduced the frequency of exacerbation (IRR 0.49, 95% CI 0.36–0.66; p<0.001) and prolonged the time to first exacerbation (HR 0.46, 95% CI 0.34–0.61; p<0.001). The effect of macrolides was observed in all subgroups; notably, an increased benefit was observed in patients with P. aeruginosa infection (IRR 0.36, 95% CI 0.18–0.72; p=0.004) [104].
A major concern regarding long-term macrolide use is its potential influence on the composition of the respiratory microbiota in bronchiectasis. A secondary analysis of the BLESS trial suggested that long-term macrolide therapy may increase the relative abundance of P. aeruginosa in the respiratory microbiota of patients with bronchiectasis. However, no patients were colonised with P. aeruginosa in culture; therefore, the clinical importance of this finding remains unclear [105]. Other concerns regarding macrolides are the need to monitor gastrointestinal side-effects, the QT interval, risk of hearing deficits and the development of resistant NTM [106, 107]. Baseline ECG and sputum acid-fast bacillus culture are recommended prior to the commencement of macrolide therapy. The risk of tinnitus and hearing deficits should be discussed with the patient and consideration given to baseline audiogram. Macrolide was more commonly used in approximately 17% of the EMBARC registry cohort (n=16 963) compared with inhaled antibiotics, but the rate substantially varied between 1% and 24% according to different European regions [35].
Inhaled corticosteroids and biologics targeting type 2 inflammation
In the absence of concomitant asthma and/or ABPA, inhaled corticosteroids (ICS) are not universally endorsed by the international guidelines [17, 18]. ICS have not been shown to reduce the frequency of bronchiectasis exacerbations and they do not properly address the predominant neutrophilic inflammation that is central to bronchiectasis pathophysiology. Recently, however, an eosinophilic endotype of bronchiectasis that is distinct from asthma has been described. Tsikrika et al. [108], in a small study of cell counts from Greece, were among the first to identify a subset of patients with elevated sputum eosinophils in bronchiectasis. Subsequently, Shoemark et al. [109] coined the entity “eosinophilic bronchiectasis” in a multicentre European cohort by identifying a subset of bronchiectasis patients with elevated T-helper cell type 2 (Th2) cytokines in sputum and then demonstrating approximately 20% of patients have blood eosinophil counts >300 cells·μL−1 or sputum eosinophils >3% after exclusion of asthma and ABPA. We have further characterised this patient group by showing that Th2 cytokines are typically elevated in association with Th1/neutrophil markers in a mixed inflammatory subtype. This mixed inflammatory subtype correlated with increased exacerbation risk compared with patients with milder inflammatory subtypes [110]. Thus, most bronchiectasis patients classified as “eosinophilic bronchiectasis” would have overlapping evidence of neutrophilic inflammation, which should be considered when deciding treatment by clinicians.
In a post hoc analysis of an RCT, ICS resulted in a statistically significant reduction of the SGRQ (≥4 points) in bronchiectasis patients with higher eosinophil counts (≥3% or ≥150 cells·µL−1), although the ICS effect was not observed in other eosinophil groups [111, 112]. Moreover, another pooled post hoc analysis of two RCTs showed that ICS led to lower rates of exacerbation and hospitalisations in bronchiectasis patients with high eosinophil counts (≥4%) [112–114]. These studies are limited by being post hoc with small sample sizes but are supported by extensive data showing eosinophils predict ICS response in other airway diseases.
The presence of an eosinophilic subtype of bronchiectasis raises the question of whether anti-Th2 biologics, which are highly effective in severe asthma, may have a role in eosinophilic bronchiectasis. The efficacy of anti-interleukin (IL)-5 or anti-IL-5 receptor monoclonal antibodies in severe eosinophilic bronchiectasis was reported in a case series (12 patients receiving mepolizumab and nine receiving benralizumab), which demonstrated marked improvements in exacerbation rate (median number of annual exacerbations, from 3 at baseline to 1 after 6 months of treatment) and lung function (median FEV1 % pred, from 53% to 68%) [115]. Moreover, other studies investigating the efficacy of Th2 inflammation-targeting biologics in patients with severe uncontrolled asthma and bronchiectasis [116–118] also support their use in patients with asthma and associated bronchiectasis. In the meantime, additional work is necessary to properly define eosinophilic bronchiectasis. This includes addressing the repeatability of circulating eosinophils over time and clarifying the role of fractional exhaled nitric oxide [119–121]. Moving forward, as precision medicine strategies become more common place in bronchiectasis management, guidelines may recommend ICS for eosinophilic subtypes of bronchiectasis.
Bronchodilators
A survey of over 700 European patients with bronchiectasis found that 70% of patients described breathlessness as either difficult or very difficult [122]. Approximately half of the EMBARC registry cohort of 16 963 patients have an FEV1 <80% predicted. Airflow obstruction is common and was reported in 35% of the patients [35]. A study performing detailed lung function in a cohort of 187 patients with bronchiectasis found airflow obstruction in 41%, but a higher proportion of patients also had air trapping reversibility and may respond to bronchodilator treatment even with “normal” spirometry [123]. Therefore, a trial of bronchodilators in patients with significant breathlessness is recommended by international guidelines [17, 18]. Randomised trials demonstrating efficacy are lacking.
Treating exacerbation
Definition of bronchiectasis exacerbation
Bronchiectasis exacerbations are watershed events in the natural history of the disease. Patients with frequent exacerbations have double the mortality rate compared with those who do not experience exacerbations [124]. In 2017, an international group of experts on bronchiectasis provided a uniform definition for clinical trials [125]. The consensus definition is: deterioration of three or more key symptoms for at least 48 h, in addition to a clinician's decision that a change in bronchiectasis treatment is required. The key symptoms are 1) cough, 2) sputum volume and/or consistency, 3) sputum purulence, 4) breathlessness and/or exercise intolerance, 5) fatigue and/or malaise, and 6) haemoptysis [125]. A clinician's decision to change treatment generally refers to the prescription of antibiotics.
Notably, the above definition was made for clinical trials, so a proportion of patients who are actually exacerbating do not meet those criteria in clinical practice. Research shows that a significant proportion of exacerbations are missed. In a study of 21 patients using a novel symptom diary, Artaraz et al. [126] showed that 23 out of 52 diary-detected exacerbations were not reported by the patients and were therefore not treated with antibiotics. Considering the detrimental effect of exacerbations in bronchiectasis patients [124, 127], widespread patient education to improve recognition of exacerbations is of paramount importance, particularly for those whose exacerbations are insufficiently severe to warrant hospital admission.
Antibiotic treatment for exacerbations
Bronchiectasis guidelines recommend antibiotics as the mainstay of treatment for bronchiectasis exacerbation. Based on expert opinion, the recommended duration of an antibiotic course is 14 days [17, 18]. However, shorter courses may be sufficient in cases of mild exacerbations or a rapid return to baseline condition, considering that an RCT demonstrated the non-inferiority of 10 versus 14 days in early responders to i.v. antibiotics in CF [128]. Additionally, the BTS guidelines recommend that suitable patients should have antibiotics to keep at home as part of their self-management plans [17]. This strategy guarantees prompt treatment of exacerbations but is not universally implemented because of concerns about antibiotic overuse. Exacerbation severity is typically determined by the site of care, with exacerbations requiring hospitalisation or home i.v. antibiotics regarded as severe and those managed as outpatients regarded as moderate. Severe exacerbations are usually managed with 14 days of i.v. antibiotics. Systemic corticosteroids are not recommended for bronchiectasis exacerbations in the absence of COPD or asthma [17, 18, 92].
A recent proof-of-concept study assessed the ability of bacterial load to guide the length of antibiotic administration during exacerbations. The study randomised 90 subjects to receive either a standard 14-day regimen or a flexible course guided by bacterial burden. 88% of patients whose length of antibiotic course was guided by bacterial load were able to stop treatment at day 8 [129]. The patients who received a standard 14-day course of antibiotics showed a non-significant trend for clinical improvement (improved HRQoL scores, reduced sputum volume and purulence) compared with the bacterial load-guided therapy. Paradoxically, despite receiving fewer days of antibiotics, the bacterial load-guided group had a longer time to next exacerbation compared with the patients who received a standard 14-day regimen [129]. A potential mechanism of such an effect is not known and may represent a chance finding. Therefore, more studies are needed to clarify the optimal duration of antibiotic treatment for bronchiectasis exacerbation. In fact, a singular recommendation is not likely to be appropriate for all patients given the overall heterogeneity of bronchiectasis patients. In addition, it is important to acknowledge that not all exacerbations require antibiotic treatment, as molecular methods do not identify bacteria in all cases. In some cases, exacerbations can be managed without antibiotics (i.e. by intensified airway clearance). Moving forward, this is an area of priority for future research.
A look to the future: new therapy, ongoing studies and precision medicine in bronchiectasis
A novel class of drugs that directly target neutrophilic inflammation in bronchiectasis has been developed. Neutrophil elastase and other neutrophil serine proteases are activated during neutrophil maturation in the bone marrow by cathepsin C/DPP1. Inhibitors of this enzyme are in advanced-phase clinical trial as novel anti-inflammatory treatments for bronchiectasis [130, 131]. The WILLOW phase 2 RCT of brensocatib, an oral reversible DPP1 inhibitor, enrolled patients with bronchiectasis in a 1:1:1 ratio to receive brensocatib 10 mg (n=82), 25 mg (n=87) or placebo (n=87) for 24 weeks. Brensocatib achieved the primary end-point of prolonged time to first exacerbation with 10 mg (HR 0.58, 95% CI 0.35–0.95; p=0.03) and 25 mg (HR 0.62, 95% CI 0.38–0.99; p=0.046) compared with that by placebo [96]. Brensocatib is currently in a phase 3 trial (ClinicalTrials.gov: NCT04594369). A similar compound, BI 1291583, is in a phase 2 clinical trial in bronchiectasis [132]. Randomised studies are also in progress testing biological treatments in eosinophilic (ClinicalTrials.gov: NCT05006573) and non-eosinophilic bronchiectasis (ClinicalTrials.gov: NCT06280391). Figure 1 summarises ongoing studies on other emerging treatments for bronchiectasis.
The heterogeneity of bronchiectasis precludes a one-size-fits-all management strategy. Post hoc analyses of previous clinical trials in bronchiectasis revealed clinically relevant subgroups of patients. For example, although both inhaled mannitol and inhaled aztreonam (AIR-BX) studies failed to meet their primary end-points [53, 81], post hoc analysis from each of the studies uncovered a subset of patients who benefitted from the study drug [54, 90]. Further analysis of such subsets may uncover “treatable traits”, or phenotypes and endotypes that may facilitate the recognition of patients who will benefit from certain therapies. Recent advancements in molecular techniques will make it possible to identify treatable traits. The objective of future bronchiectasis management is to employ targeted therapies toward specific treatable traits within mucus clearance, chronic bacterial infection and airway inflammation in accordance with the concept of precision medicine. There are many unanswered questions in the field of bronchiectasis. In 2016, the EMBARC consortium outlined 22 priority research topics [122]. Many have been addressed, such as the need for large-scale observational cohorts to study the natural history of bronchiectasis. Other areas still require further research. We have adapted these recommendations into 10 updated research recommendations: five on evidence for existing treatments and five related to novel treatments and disease understanding (table 3).
TABLE 3.
Suggested future research priorities in bronchiectasis (adapted from Aliberti et al. [122])
| Evidence for current treatments |
| 1) An RCT of Pseudomonas eradication therapy compared with symptomatic treatment |
| 2) An RCT to determine the optimal duration of antibiotic treatment for bronchiectasis exacerbations |
| 3) Biomarkers are needed to identify which patients respond optimally to inhaled antibiotics |
| 4) An RCT of inhaled corticosteroids in bronchiectasis, including determining whether biomarkers such as blood eosinophil counts can guide treatment |
| 5) Large-scale pragmatic trials of airway clearance techniques and pulmonary rehabilitation are required to establish a robust evidence base and the optimal mode of delivery for this intervention |
| Novel treatments and disease understanding |
| 6) Development of novel strategies to modify the microbiome as alternatives to broad-spectrum antibiotics (including antibodies/vaccines, phage therapy and probiotics) |
| 7) Development of novel therapeutics targeting neutrophilic inflammation/neutrophil extracellular traps to prevent exacerbations and improve symptoms |
| 8) A large-scale genetic study of unselected patients with bronchiectasis is needed to identify underlying causes, find new causes of “idiopathic bronchiectasis” and to identify new therapeutic targets |
| 9) Deep molecular endotyping of bronchiectasis incorporating proteomics, transcriptomics, microbiomics and other profiling is needed to understand the biological mechanisms underlying bronchiectasis and identify new biomarkers and targets |
| 10) Studies of early bronchiectasis, including syndromes such as persistent bacterial bronchitis and the early stages of diseases such as primary ciliary dyskinesia, are needed to understand the initial molecular mechanisms leading to the development and progression of bronchiectasis |
RCT: randomised controlled trial.
Conclusions
The fundamental goals of bronchiectasis treatment are to lessen the symptom burden, improve HRQoL, reduce exacerbations and prevent disease progression. With the increased awareness of the disease, bronchiectasis is finally receiving the attention that it deserves. Scientific research has improved our understanding of the pathophysiological mechanisms that drive the disease and there are an unprecedented number of clinical trials now available to our patients. With continued momentum, the concept of precision medicine in bronchiectasis will soon be a reality. Thus, the future for patients with bronchiectasis is promising.
Shareable PDF
Footnotes
Conflict of interest: H. Choi reports grants from the Basic Science Research Program of the Korean Ministry of Education (grant number 2021R1I1A3052416), and consulting and lecture fees from Boryung Pharmaceutical Co., Ltd and Kolon Pharma. P.J. McShane reports study funding (paid to institution) from Boehringer Ingelheim, Armata, Paratek, Renovian, Spero, AN2 Therapeutics and Insmed, and speaker fees from Insmed. S. Aliberti reports grants or contracts from Insmed Incorporated, Chiesi, Fisher & Paykel and GlaxoSmithKline, royalties or licences from McGraw Hill, consulting fees from Insmed Incorporated, Insmed Italy, Insmed Ireland Ltd, Zambon SpA, AstraZeneca UK Ltd, AstraZeneca Pharmaceutical LP, CSL Behring GmbH, Grifols, Fondazione Internazionale Menarini, Moderna, Chiesi, MSD Italia Srl, Brahms, Physioassist SAS and GlaxoSmithKline SpA, payment or honoraria for lectures, presentations, manuscript writing or educational events from GlaxoSmithKline SpA, Thermofisher Scientific, Insmed Italy, Insmed Ireland, Zambon and Fondazione Internazionale Menarini, and participation on a data safety monitoring board or advisory board for Insmed Incorporated, Insmed Italy, AstraZeneca UK Ltd and MSD Italia Srl. J.D. Chalmers reports grants or contracts from AstraZeneca, Boehringer Ingelheim, Genentech, Gilead Sciences, GlaxoSmithKline, Grifols, Insmed, LifeArc and Novartis, and consulting fees from AstraZeneca, Chiesi, GlaxoSmithKline, Insmed, Grifols, Novartis, Boehringer Ingelheim, Pfizer, Janssen, Antabio and Zambon.
Support statement: EMBARC3 is funded by the European Respiratory Society through the EMBARC3 Clinical Research Collaboration. EMBARC3 is supported by project partners Armata, AstraZeneca, Boehringer Ingelheim, Chiesi, CSL Behring, Grifols, Insmed, Janssen, LifeArc and Zambon. Supported by the Innovative Medicines Initiative and the European Federation of Pharmaceutical Industries and Associations companies under the European Commission-funded Horizon 2020 Framework Program and by Inhaled Antibiotic for Bronchiectasis and Cystic Fibrosis (grant 115721). J.D. Chalmers is supported by the GlaxoSmithKline/Asthma and Lung UK Chair of Respiratory Research.
References
- 1.Chalmers JD, Chang AB, Chotirmall SH, et al. Bronchiectasis. Nat Rev Dis Primers 2018; 4: 45. doi: 10.1038/s41572-018-0042-3 [DOI] [PubMed] [Google Scholar]
- 2.Aliberti S, Goeminne PC, O'Donnell AE, et al. Criteria and definitions for the radiological and clinical diagnosis of bronchiectasis in adults for use in clinical trials: international consensus recommendations. Lancet Respir Med 2022; 10: 298–306. doi: 10.1016/S2213-2600(21)00277-0 [DOI] [PubMed] [Google Scholar]
- 3.Keistinen T, Saynajakangas O, Tuuponen T, et al. Bronchiectasis: an orphan disease with a poorly-understood prognosis. Eur Respir J 1997; 10: 2784–2787. doi: 10.1183/09031936.97.10122784 [DOI] [PubMed] [Google Scholar]
- 4.Quint JK, Millett ER, Joshi M, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population-based cohort study. Eur Respir J 2016; 47: 186–193. doi: 10.1183/13993003.01033-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi H, Yang B, Nam H, et al. Population-based prevalence of bronchiectasis and associated comorbidities in South Korea. Eur Respir J 2019; 54: 1900194. doi: 10.1183/13993003.00194-2019 [DOI] [PubMed] [Google Scholar]
- 6.Ringshausen FC, de Roux A, Diel R, et al. Bronchiectasis in Germany: a population-based estimation of disease prevalence. Eur Respir J 2015; 46: 1805–1807. doi: 10.1183/13993003.00954-2015 [DOI] [PubMed] [Google Scholar]
- 7.Weycker D, Hansen GL, Seifer FD. Prevalence and incidence of noncystic fibrosis bronchiectasis among US adults in 2013. Chron Respir Dis 2017; 14: 377–384. doi: 10.1177/1479972317709649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diel R, Chalmers JD, Rabe KF, et al. Economic burden of bronchiectasis in Germany. Eur Respir J 2019; 53: 1802033. doi: 10.1183/13993003.02033-2018 [DOI] [PubMed] [Google Scholar]
- 9.Choi H, Yang B, Kim YJ, et al. Increased mortality in patients with non cystic fibrosis bronchiectasis with respiratory comorbidities. Sci Rep 2021; 11: 7126. doi: 10.1038/s41598-021-86407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts JM, Goyal V, Kularatna S, et al. The economic burden of bronchiectasis: a systematic review. Chest 2023; 164: 1396–1421. doi: 10.1016/j.chest.2023.06.040 [DOI] [PubMed] [Google Scholar]
- 11.Aksamit TR, O'Donnell AE, Barker A, et al. Adult patients with bronchiectasis: a first look at the US Bronchiectasis Research Registry. Chest 2017; 151: 982–992. doi: 10.1016/j.chest.2016.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chalmers JD, Aliberti S, Polverino E, et al. The EMBARC European Bronchiectasis Registry: protocol for an international observational study. ERJ Open Res 2016; 2: 00081-2015. doi: 10.1183/23120541.00081-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dhar R, Singh S, Talwar D, et al. Bronchiectasis in India: results from the European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC) and Respiratory Research Network of India Registry. Lancet Glob Health 2019; 7: e1269–e1279. doi: 10.1016/S2214-109X(19)30327-4 [DOI] [PubMed] [Google Scholar]
- 14.Lee H, Choi H, Chalmers JD, et al. Characteristics of bronchiectasis in Korea: first data from the Korean Multicentre Bronchiectasis Audit and Research Collaboration registry and comparison with other international registries. Respirology 2021; 26: 619–621. doi: 10.1111/resp.14059 [DOI] [PubMed] [Google Scholar]
- 15.Lee H, Choi H, Sim YS, et al. KMBARC registry: protocol for a multicentre observational cohort study on non-cystic fibrosis bronchiectasis in Korea. BMJ Open 2020; 10: e034090. doi: 10.1136/bmjopen-2019-034090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Visser SK, Bye PTP, Fox GJ, et al. Australian adults with bronchiectasis: the first report from the Australian Bronchiectasis Registry. Respir Med 2019; 155: 97–103. doi: 10.1016/j.rmed.2019.07.016 [DOI] [PubMed] [Google Scholar]
- 17.Hill AT, Sullivan AL, Chalmers JD, et al. British Thoracic Society Guideline for bronchiectasis in adults. Thorax 2019; 74: Suppl. 1, 1–69. doi: 10.1136/thoraxjnl-2018-212463 [DOI] [PubMed] [Google Scholar]
- 18.Polverino E, Goeminne PC, McDonnell MJ, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J 2017; 50: 1700629. doi: 10.1183/13993003.00629-2017 [DOI] [PubMed] [Google Scholar]
- 19.Martinez-Garcia MA, Maiz L, Olveira C, et al. Spanish guidelines on treatment of bronchiectasis in adults. Arch Bronconeumol 2018; 54: 88–98. doi: 10.1016/j.arbr.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 20.Chang AB, Bell SC, Byrnes CA, et al. Thoracic Society of Australia and New Zealand (TSANZ) position statement on chronic suppurative lung disease and bronchiectasis in children, adolescents and adults in Australia and New Zealand. Respirology 2023; 28: 339–349. doi: 10.1111/resp.14479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Jahdali H, Alshimemeri A, Mobeireek A, et al. The Saudi Thoracic Society guidelines for diagnosis and management of noncystic fibrosis bronchiectasis. Ann Thorac Med 2017; 12: 135–161. doi: 10.4103/atm.ATM_171_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cole PJ. Inflammation: a two-edged sword – the model of bronchiectasis. Eur J Respir Dis Suppl 1986; 147: 6–15. [PubMed] [Google Scholar]
- 23.Keir HR, Chalmers JD. Pathophysiology of bronchiectasis. Semin Respir Crit Care Med 2021; 42: 499–512. doi: 10.1055/s-0041-1730891 [DOI] [PubMed] [Google Scholar]
- 24.Flume PA, Chalmers JD, Olivier KN. Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneity. Lancet 2018; 392: 880–890. doi: 10.1016/S0140-6736(18)31767-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amitani R, Wilson R, Rutman A, et al. Effects of human neutrophil elastase and Pseudomonas aeruginosa proteinases on human respiratory epithelium. Am J Respir Cell Mol Biol 1991; 4: 26–32. doi: 10.1165/ajrcmb/4.1.26 [DOI] [PubMed] [Google Scholar]
- 26.Nair C, Shoemark A, Chan M, et al. Cyanide levels found in infected cystic fibrosis sputum inhibit airway ciliary function. Eur Respir J 2014; 44: 1253–1261. doi: 10.1183/09031936.00097014 [DOI] [PubMed] [Google Scholar]
- 27.Watt AP, Brown V, Courtney J, et al. Neutrophil apoptosis, proinflammatory mediators and cell counts in bronchiectasis. Thorax 2004; 59: 231–236. doi: 10.1136/thx.2003.008037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McDonnell MJ, Aliberti S, Goeminne PC, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med 2016; 4: 969–979. doi: 10.1016/S2213-2600(16)30320-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chalmers JD, Goeminne P, Aliberti S, et al. The Bronchiectasis Severity Index. An international derivation and validation study. Am J Respir Crit Care Med 2014; 189: 576–585. doi: 10.1164/rccm.201309-1575OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martinez-Garcia MA, Athanazio RA, Girón R, et al. Predicting high risk of exacerbations in bronchiectasis: the E-FACED score. Int J Chron Obstruct Pulmon Dis 2017; 12: 275–284. doi: 10.2147/COPD.S121943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amati F, Simonetta E, Pilocane T, et al. Diagnosis and initial investigation of bronchiectasis. Semin Respir Crit Care Med 2021; 42: 513–524. doi: 10.1055/s-0041-1730892 [DOI] [PubMed] [Google Scholar]
- 32.De Soyza A, McDonnell MJ, Goeminne PC, et al. Bronchiectasis rheumatoid overlap syndrome is an independent risk factor for mortality in patients with bronchiectasis: a multicenter cohort study. Chest 2017; 151: 1247–1254. doi: 10.1016/j.chest.2016.12.024 [DOI] [PubMed] [Google Scholar]
- 33.Shoemark A, Griffin H, Wheway G, et al. Genome sequencing reveals underdiagnosis of primary ciliary dyskinesia in bronchiectasis. Eur Respir J 2022; 60: 2200176. doi: 10.1183/13993003.00176-2022 [DOI] [PubMed] [Google Scholar]
- 34.Shapiro AJ, Zariwala MA, Ferkol T, et al. Diagnosis, monitoring, and treatment of primary ciliary dyskinesia: PCD Foundation consensus recommendations based on state of the art review. Pediatr Pulmonol 2016; 51: 115–132. doi: 10.1002/ppul.23304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chalmers JD, Polverino E, Crichton ML, et al. Bronchiectasis in Europe: data on disease characteristics from the European Bronchiectasis registry (EMBARC). Lancet Respir Med 2023; 11: 637–649. doi: 10.1016/S2213-2600(23)00093-0 [DOI] [PubMed] [Google Scholar]
- 36.Ramsey KA, Chen ACH, Radicioni G, et al. Airway mucus hyperconcentration in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med 2020; 201: 661–670. doi: 10.1164/rccm.201906-1219OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mikami Y, Grubb BR, Rogers TD, et al. Chronic airway epithelial hypoxia exacerbates injury in muco-obstructive lung disease through mucus hyperconcentration. Sci Transl Med 2023; 15: eabo7728. doi: 10.1126/scitranslmed.abo7728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herrero-Cortina B, Lee AL, Oliveira A, et al. European Respiratory Society statement on airway clearance techniques in adults with bronchiectasis. Eur Respir J 2023; 62: 2202053. doi: 10.1183/13993003.02053-2022 [DOI] [PubMed] [Google Scholar]
- 39.Murray MP, Pentland JL, Hill AT. A randomised crossover trial of chest physiotherapy in non-cystic fibrosis bronchiectasis. Eur Respir J 2009; 34: 1086–1092. doi: 10.1183/09031936.00055509 [DOI] [PubMed] [Google Scholar]
- 40.Livnat G, Yaari N, Stein N, et al. 4-week daily airway clearance using oscillating positive-end expiratory pressure versus autogenic drainage in bronchiectasis patients: a randomised controlled trial. ERJ Open Res 2021; 7: 00426-2021. doi: 10.1183/23120541.00426-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patterson JE, Bradley JM, Hewitt O, et al. Airway clearance in bronchiectasis: a randomized crossover trial of active cycle of breathing techniques versus Acapella. Respiration 2005; 72: 239–242. doi: 10.1159/000085363 [DOI] [PubMed] [Google Scholar]
- 42.Patterson JE, Hewitt O, Kent L, et al. Acapella versus ‘usual airway clearance’ during acute exacerbation in bronchiectasis: a randomized crossover trial. Chron Respir Dis 2007; 4: 67–74. doi: 10.1177/1479972306075483 [DOI] [PubMed] [Google Scholar]
- 43.Santos MD, Milross MA, McKenzie DK, et al. Bubble-positive expiratory pressure device and sputum clearance in bronchiectasis: a randomised cross-over study. Physiother Res Int 2020; 25: e1836. doi: 10.1002/pri.1836 [DOI] [PubMed] [Google Scholar]
- 44.Uzmezoglu B, Altiay G, Ozdemir L, et al. The efficacy of Flutter and active cycle of breathing techniques in patients with bronchiectasis: a prospective, randomized, comparative study. Turk Thorac J 2018; 19: 103–109. doi: 10.5152/TurkThoracJ.2018.17050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Munoz G, de Gracia J, Buxo M, et al. Long-term benefits of airway clearance in bronchiectasis: a randomised placebo-controlled trial. Eur Respir J 2018; 51: 1701926. doi: 10.1183/13993003.01926-2017 [DOI] [PubMed] [Google Scholar]
- 46.Tse HN, Raiteri L, Wong KY, et al. High-dose N-acetylcysteine in stable COPD: the 1-year, double-blind, randomized, placebo-controlled HIACE study. Chest 2013; 144: 106–118. doi: 10.1378/chest.12-2357 [DOI] [PubMed] [Google Scholar]
- 47.Kellett F, Redfern J, Niven RM. Evaluation of nebulised hypertonic saline (7%) as an adjunct to physiotherapy in patients with stable bronchiectasis. Respir Med 2005; 99: 27–31. doi: 10.1016/j.rmed.2004.05.006 [DOI] [PubMed] [Google Scholar]
- 48.Kellett F, Robert NM. Nebulised 7% hypertonic saline improves lung function and quality of life in bronchiectasis. Respir Med 2011; 105: 1831–1835. doi: 10.1016/j.rmed.2011.07.019 [DOI] [PubMed] [Google Scholar]
- 49.Herrero-Cortina B, Alcaraz V, Vilaro J, et al. Impact of hypertonic saline solutions on sputum expectoration and their safety profile in patients with bronchiectasis: a randomized crossover trial. J Aerosol Med Pulm Drug Deliv 2018; 31: 281–289. doi: 10.1089/jamp.2017.1443 [DOI] [PubMed] [Google Scholar]
- 50.Nicolson CH, Stirling RG, Borg BM, et al. The long term effect of inhaled hypertonic saline 6% in non-cystic fibrosis bronchiectasis. Respir Med 2012; 106: 661–667. doi: 10.1016/j.rmed.2011.12.021 [DOI] [PubMed] [Google Scholar]
- 51.O'Donnell AE, Barker AF, Ilowite JS, et al. Treatment of idiopathic bronchiectasis with aerosolized recombinant human DNase I. Chest 1998; 113: 1329–1334. doi: 10.1378/chest.113.5.1329 [DOI] [PubMed] [Google Scholar]
- 52.Bilton D, Daviskas E, Anderson SD, et al. Phase 3 randomized study of the efficacy and safety of inhaled dry powder mannitol for the symptomatic treatment of non-cystic fibrosis bronchiectasis. Chest 2013; 144: 215–225. doi: 10.1378/chest.12-1763 [DOI] [PubMed] [Google Scholar]
- 53.Bilton D, Tino G, Barker AF, et al. Inhaled mannitol for non-cystic fibrosis bronchiectasis: a randomised, controlled trial. Thorax 2014; 69: 1073–1079. doi: 10.1136/thoraxjnl-2014-205587 [DOI] [PubMed] [Google Scholar]
- 54.Gao YH, Abo Leyah H, Finch S, et al. Relationship between symptoms, exacerbations, and treatment response in bronchiectasis. Am J Respir Crit Care Med 2020; 201: 1499–1507. doi: 10.1164/rccm.201910-1972OC [DOI] [PubMed] [Google Scholar]
- 55.Mandal P, Sidhu MK, Kope L, et al. A pilot study of pulmonary rehabilitation and chest physiotherapy versus chest physiotherapy alone in bronchiectasis. Respir Med 2012; 106: 1647–1654. doi: 10.1016/j.rmed.2012.08.004 [DOI] [PubMed] [Google Scholar]
- 56.Lee AL, Hill CJ, Cecins N, et al. The short and long term effects of exercise training in non-cystic fibrosis bronchiectasis – a randomised controlled trial. Respir Res 2014; 15: 44. doi: 10.1186/1465-9921-15-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alcaraz-Serrano V, Gimeno-Santos E, Scioscia G, et al. Association between physical activity and risk of hospitalisation in bronchiectasis. Eur Respir J 2020; 55: 1902138. doi: 10.1183/13993003.02138-2019 [DOI] [PubMed] [Google Scholar]
- 58.Herrero-Cortina B, Spinou A, Oliveira A, et al. Airway clearance techniques and exercise in people with bronchiectasis: two different coins. Eur Respir J 2023; 62: 2300741. doi: 10.1183/13993003.00741-2023 [DOI] [PubMed] [Google Scholar]
- 59.Choi H, Kim SH, Han K, et al. Association between exercise and risk of cardiovascular diseases in patients with non-cystic fibrosis bronchiectasis. Respir Res 2022; 23: 288. doi: 10.1186/s12931-022-02202-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chalmers JD, Smith MP, McHugh BJ, et al. Short- and long-term antibiotic treatment reduces airway and systemic inflammation in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med 2012; 186: 657–665. doi: 10.1164/rccm.201203-0487OC [DOI] [PubMed] [Google Scholar]
- 61.Finch S, McDonnell MJ, Abo-Leyah H, et al. A comprehensive analysis of the impact of Pseudomonas aeruginosa colonization on prognosis in adult bronchiectasis. Ann Am Thorac Soc 2015; 12: 1602–1611. doi: 10.1513/AnnalsATS.201506-333OC [DOI] [PubMed] [Google Scholar]
- 62.Araujo D, Shteinberg M, Aliberti S, et al. The independent contribution of Pseudomonas aeruginosa infection to long-term clinical outcomes in bronchiectasis. Eur Respir J 2018; 51: 1701953. doi: 10.1183/13993003.01953-2017 [DOI] [PubMed] [Google Scholar]
- 63.Marra R, Sgalla G, Richeldi L, et al. Role of Stenotrophomonas maltophilia isolation in patients with non-CF bronchiectasis. QJM 2020; 113: 726–730. doi: 10.1093/qjmed/hcaa120 [DOI] [PubMed] [Google Scholar]
- 64.Metersky ML, Aksamit TR, Barker A, et al. The prevalence and significance of Staphylococcus aureus in patients with non-cystic fibrosis bronchiectasis. Ann Am Thorac Soc 2018; 15: 365–370. doi: 10.1513/AnnalsATS.201706-426OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dicker AJ, Lonergan M, Keir HR, et al. The sputum microbiome and clinical outcomes in patients with bronchiectasis: a prospective observational study. Lancet Respir Med 2021; 9: 885–896. doi: 10.1016/S2213-2600(20)30557-9 [DOI] [PubMed] [Google Scholar]
- 66.Byun MK, Chang J, Kim HJ, et al. Differences of lung microbiome in patients with clinically stable and exacerbated bronchiectasis. PLoS One 2017; 12: e0183553. doi: 10.1371/journal.pone.0183553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tunney MM, Einarsson GG, Wei L, et al. Lung microbiota and bacterial abundance in patients with bronchiectasis when clinically stable and during exacerbation. Am J Respir Crit Care Med 2013; 187: 1118–1126. doi: 10.1164/rccm.201210-1937OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mac Aogáin M, Narayana JK, Tiew PY, et al. Integrative microbiomics in bronchiectasis exacerbations. Nat Med 2021; 27: 688–699. doi: 10.1038/s41591-021-01289-7 [DOI] [PubMed] [Google Scholar]
- 69.Panigrahi P, Parida S, Nanda NC, et al. A randomized synbiotic trial to prevent sepsis among infants in rural India. Nature 2017; 548: 407–412. doi: 10.1038/nature23480 [DOI] [PubMed] [Google Scholar]
- 70.Durack J, Kimes NE, Lin DL, et al. Delayed gut microbiota development in high-risk for asthma infants is temporarily modifiable by Lactobacillus supplementation. Nat Commun 2018; 9: 707. doi: 10.1038/s41467-018-03157-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vallieres E, Tumelty K, Tunney MM, et al. Efficacy of Pseudomonas aeruginosa eradication regimens in bronchiectasis. Eur Respir J 2017; 49: 1600851. doi: 10.1183/13993003.00851-2016 [DOI] [PubMed] [Google Scholar]
- 72.Blanco-Aparicio M, Saleta Canosa JL, Valino Lopez P, et al. Eradication of Pseudomonas aeruginosa with inhaled colistin in adults with non-cystic fibrosis bronchiectasis. Chron Respir Dis 2019; 16: 1479973119872513. doi: 10.1177/1479973119872513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.White L, Mirrani G, Grover M, et al. Outcomes of Pseudomonas eradication therapy in patients with non-cystic fibrosis bronchiectasis. Respir Med 2012; 106: 356–360. doi: 10.1016/j.rmed.2011.11.018 [DOI] [PubMed] [Google Scholar]
- 74.Conceicao M, Shteinberg M, Goeminne P, et al. Eradication treatment for Pseudomonas aeruginosa infection in adults with bronchiectasis: a systematic review and meta-analysis. Eur Respir Rev 2024; 33: 230178. doi: 10.1183/16000617.0178-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Quon BS, Goss CH, Ramsey BW. Inhaled antibiotics for lower airway infections. Ann Am Thorac Soc 2014; 11: 425–434. doi: 10.1513/AnnalsATS.201311-395FR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wilson R, Welte T, Polverino E, et al. Ciprofloxacin dry powder for inhalation in non-cystic fibrosis bronchiectasis: a phase II randomised study. Eur Respir J 2013; 41: 1107–1115. doi: 10.1183/09031936.00071312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.De Soyza A, Aksamit T, Bandel TJ, et al. RESPIRE 1: a phase III placebo-controlled randomised trial of ciprofloxacin dry powder for inhalation in non-cystic fibrosis bronchiectasis. Eur Respir J 2018; 51: 1702052. doi: 10.1183/13993003.02052-2017 [DOI] [PubMed] [Google Scholar]
- 78.Aksamit T, De Soyza A, Bandel TJ, et al. RESPIRE 2: a phase III placebo-controlled randomised trial of ciprofloxacin dry powder for inhalation in non-cystic fibrosis bronchiectasis. Eur Respir J 2018; 51: 1702053. doi: 10.1183/13993003.02053-2017 [DOI] [PubMed] [Google Scholar]
- 79.Serisier DJ, Bilton D, De Soyza A, et al. Inhaled, dual release liposomal ciprofloxacin in non-cystic fibrosis bronchiectasis (ORBIT-2): a randomised, double-blind, placebo-controlled trial. Thorax 2013; 68: 812–817. doi: 10.1136/thoraxjnl-2013-203207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Haworth CS, Bilton D, Chalmers JD, et al. Inhaled liposomal ciprofloxacin in patients with non-cystic fibrosis bronchiectasis and chronic lung infection with Pseudomonas aeruginosa (ORBIT-3 and ORBIT-4): two phase 3, randomised controlled trials. Lancet Respir Med 2019; 7: 213–226. doi: 10.1016/S2213-2600(18)30427-2 [DOI] [PubMed] [Google Scholar]
- 81.Barker AF, O'Donnell AE, Flume P, et al. Aztreonam for inhalation solution in patients with non-cystic fibrosis bronchiectasis (AIR-BX1 and AIR-BX2): two randomised double-blind, placebo-controlled phase 3 trials. Lancet Respir Med 2014; 2: 738–749. doi: 10.1016/S2213-2600(14)70165-1 [DOI] [PubMed] [Google Scholar]
- 82.Barker AF, Couch L, Fiel SB, et al. Tobramycin solution for inhalation reduces sputum Pseudomonas aeruginosa density in bronchiectasis. Am J Respir Crit Care Med 2000; 162: 481–485. doi: 10.1164/ajrccm.162.2.9910086 [DOI] [PubMed] [Google Scholar]
- 83.Guan WJ, Xu JF, Luo H, et al. A double-blind randomized placebo-controlled phase 3 trial of tobramycin inhalation solution in adults with bronchiectasis with Pseudomonas aeruginosa infection. Chest 2023; 163: 64–76. doi: 10.1016/j.chest.2022.07.007 [DOI] [PubMed] [Google Scholar]
- 84.Terpstra LC, Altenburg J, Bronsveld I, et al. Effects of long-term tobramycin inhalation solution (TIS) once daily on exacerbation rate in patients with non-cystic fibrosis bronchiectasis. Respir Res 2022; 23: 330. doi: 10.1186/s12931-022-02243-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Loebinger MR, Polverino E, Chalmers JD, et al. Efficacy and safety of TOBI Podhaler in Pseudomonas aeruginosa-infected bronchiectasis patients: iBEST study. Eur Respir J 2021; 57: 2001451. doi: 10.1183/13993003.01451-2020 [DOI] [PubMed] [Google Scholar]
- 86.Murray MP, Govan JR, Doherty CJ, et al. A randomized controlled trial of nebulized gentamicin in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med 2011; 183: 491–499. doi: 10.1164/rccm.201005-0756OC [DOI] [PubMed] [Google Scholar]
- 87.Haworth CS, Foweraker JE, Wilkinson P, et al. Inhaled colistin in patients with bronchiectasis and chronic Pseudomonas aeruginosa infection. Am J Respir Crit Care Med 2014; 189: 975–982. doi: 10.1164/rccm.201312-2208OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cordeiro R, Choi H, Haworth CS, et al. The efficacy and safety of inhaled antibiotics for the treatment of bronchiectasis in adults: updated systematic review and meta-analysis. Chest 2024; in press [ 10.1016/j.chest.2024.01.045]. doi: 10.1016/j.chest.2024.01.045 [DOI] [PubMed] [Google Scholar]
- 89.Haworth CS, Shteinberg M, Winthrop KL, et al. RCT Abstract – the efficacy and safety of colistimethate sodium delivered via the I-neb in bronchiectasis: the PROMIS-I randomized controlled trial. Eur Respir J 2021; 58: Suppl. 65, RCT4267. doi: 10.1183/13993003.congress-2021.RCT4267 [DOI] [Google Scholar]
- 90.Sibila O, Laserna E, Shoemark A, et al. Airway bacterial load and inhaled antibiotic response in bronchiectasis. Am J Respir Crit Care Med 2019; 200: 33–41. doi: 10.1164/rccm.201809-1651OC [DOI] [PubMed] [Google Scholar]
- 91.Chalmers JD, Cipolla D, Thompson B, et al. Changes in respiratory symptoms during 48-week treatment with ARD-3150 (inhaled liposomal ciprofloxacin) in bronchiectasis: results from the ORBIT-3 and -4 studies. Eur Respir J 2020; 56: 2000110. doi: 10.1183/13993003.00110-2020 [DOI] [PubMed] [Google Scholar]
- 92.Choi H, Chalmers JD. Bronchiectasis exacerbation: a narrative review of causes, risk factors, management and prevention. Ann Transl Med 2023; 11: 25. doi: 10.21037/atm-22-3437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Crichton ML, Lonergan M, Barker AF, et al. Inhaled aztreonam improves symptoms of cough and sputum production in patients with bronchiectasis: a post hoc analysis of the AIR-BX studies. Eur Respir J 2020; 56: 2000608. doi: 10.1183/13993003.00608-2020 [DOI] [PubMed] [Google Scholar]
- 94.Chalmers JD, Moffitt KL, Suarez-Cuartin G, et al. Neutrophil elastase activity is associated with exacerbations and lung function decline in bronchiectasis. Am J Respir Crit Care Med 2017; 195: 1384–1393. doi: 10.1164/rccm.201605-1027OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Keir HR, Shoemark A, Dicker AJ, et al. Neutrophil extracellular traps, disease severity, and antibiotic response in bronchiectasis: an international, observational, multicohort study. Lancet Respir Med 2021; 9: 873–884. doi: 10.1016/S2213-2600(20)30504-X [DOI] [PubMed] [Google Scholar]
- 96.Chalmers JD, Haworth CS, Metersky ML, et al. Phase 2 trial of the DPP-1 inhibitor brensocatib in bronchiectasis. N Engl J Med 2020; 383: 2127–2137. doi: 10.1056/NEJMoa2021713 [DOI] [PubMed] [Google Scholar]
- 97.Shoemark A, Cant E, Carreto L, et al. A point-of-care neutrophil elastase activity assay identifies bronchiectasis severity, airway infection and risk of exacerbation. Eur Respir J 2019; 53: 1900303. doi: 10.1183/13993003.00303-2019 [DOI] [PubMed] [Google Scholar]
- 98.Yang B, Yun H, Seong C, et al. Association between sputum myeloperoxidase concentration and acute exacerbation of bronchiectasis. Pulmonology 2023; in press [ 10.1016/j.pulmoe.2023.10.006]. doi: 10.1016/j.pulmoe.2023.10.006 [DOI] [PubMed] [Google Scholar]
- 99.Burr LD, Rogers GB, Chen AC, et al. Macrolide treatment inhibits Pseudomonas aeruginosa quorum sensing in non-cystic fibrosis bronchiectasis. An analysis from the Bronchiectasis and Low-Dose Erythromycin Study trial. Ann Am Thorac Soc 2016; 13: 1697–1703. doi: 10.1513/AnnalsATS.201601-044OC [DOI] [PubMed] [Google Scholar]
- 100.Yang B, Ryu J, Kim T, et al. Impact of bronchiectasis on incident nontuberculous mycobacterial pulmonary disease: a 10-year national cohort study. Chest 2021; 159: 1807–1811. doi: 10.1016/j.chest.2020.12.020 [DOI] [PubMed] [Google Scholar]
- 101.Wong C, Jayaram L, Karalus N, et al. Azithromycin for prevention of exacerbations in non-cystic fibrosis bronchiectasis (EMBRACE): a randomised, double-blind, placebo-controlled trial. Lancet 2012; 380: 660–667. doi: 10.1016/S0140-6736(12)60953-2 [DOI] [PubMed] [Google Scholar]
- 102.Serisier DJ, Martin ML, McGuckin MA, et al. Effect of long-term, low-dose erythromycin on pulmonary exacerbations among patients with non-cystic fibrosis bronchiectasis: the BLESS randomized controlled trial. JAMA 2013; 309: 1260–1267. doi: 10.1001/jama.2013.2290 [DOI] [PubMed] [Google Scholar]
- 103.Altenburg J, de Graaff CS, Stienstra Y, et al. Effect of azithromycin maintenance treatment on infectious exacerbations among patients with non-cystic fibrosis bronchiectasis: the BAT randomized controlled trial. JAMA 2013; 309: 1251–1259. doi: 10.1001/jama.2013.1937 [DOI] [PubMed] [Google Scholar]
- 104.Chalmers JD, Boersma W, Lonergan M, et al. Long-term macrolide antibiotics for the treatment of bronchiectasis in adults: an individual participant data meta-analysis. Lancet Respir Med 2019; 7: 845–854. doi: 10.1016/S2213-2600(19)30191-2 [DOI] [PubMed] [Google Scholar]
- 105.Rogers GB, Bruce KD, Martin ML, et al. The effect of long-term macrolide treatment on respiratory microbiota composition in non-cystic fibrosis bronchiectasis: an analysis from the randomised, double-blind, placebo-controlled BLESS trial. Lancet Respir Med 2014; 2: 988–996. doi: 10.1016/S2213-2600(14)70213-9 [DOI] [PubMed] [Google Scholar]
- 106.Schembri S, Williamson PA, Short PM, et al. Cardiovascular events after clarithromycin use in lower respiratory tract infections: analysis of two prospective cohort studies. BMJ 2013; 346: f1235. doi: 10.1136/bmj.f1235 [DOI] [PubMed] [Google Scholar]
- 107.Choi H, Kim SY, Lee H, et al. Clinical characteristics and treatment outcomes of patients with macrolide-resistant Mycobacterium massiliense lung disease. Antimicrob Agents Chemother 2017; 61: e02189-16. doi: 10.1128/AAC.02189-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tsikrika S, Dimakou K, Papaioannou AI, et al. The role of non-invasive modalities for assessing inflammation in patients with non-cystic fibrosis bronchiectasis. Cytokine 2017; 99: 281–286. doi: 10.1016/j.cyto.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 109.Shoemark A, Shteinberg M, De Soyza A, et al. Characterization of eosinophilic bronchiectasis: a European multicohort study. Am J Respir Crit Care Med 2022; 205: 894–902. doi: 10.1164/rccm.202108-1889OC [DOI] [PubMed] [Google Scholar]
- 110.Choi H, Ryu S, Keir HR, et al. Inflammatory molecular endotypes in bronchiectasis: a European multicenter cohort study. Am J Respir Crit Care Med 2023; 208: 1166–1176. doi: 10.1164/rccm.202303-0499OC [DOI] [PubMed] [Google Scholar]
- 111.Aliberti S, Sotgiu G, Blasi F, et al. Blood eosinophils predict inhaled fluticasone response in bronchiectasis. Eur Respir J 2020; 56: 2000453. doi: 10.1183/13993003.00453-2020 [DOI] [PubMed] [Google Scholar]
- 112.Martinez-Garcia MA, Perpina-Tordera M, Roman-Sanchez P, et al. Inhaled steroids improve quality of life in patients with steady-state bronchiectasis. Respir Med 2006; 100: 1623–1632. doi: 10.1016/j.rmed.2005.12.002 [DOI] [PubMed] [Google Scholar]
- 113.Martínez-García MÁ, Soler-Cataluña JJ, Catalán-Serra P, et al. Clinical efficacy and safety of budesonide-formoterol in non-cystic fibrosis bronchiectasis. Chest 2012; 141: 461–468. doi: 10.1378/chest.11-0180 [DOI] [PubMed] [Google Scholar]
- 114.Martinez-Garcia MA, Posadas T, Sotgiu G, et al. Role of inhaled corticosteroids in reducing exacerbations in bronchiectasis patients with blood eosinophilia pooled post-hoc analysis of 2 randomized clinical trials. Respir Med 2020; 172: 106127. doi: 10.1016/j.rmed.2020.106127 [DOI] [PubMed] [Google Scholar]
- 115.Rademacher J, Konwert S, Fuge J, et al. Anti-IL5 and anti-IL5Rα therapy for clinically significant bronchiectasis with eosinophilic endotype: a case series. Eur Respir J 2020; 55: 1901333. doi: 10.1183/13993003.01333-2019 [DOI] [PubMed] [Google Scholar]
- 116.Kudlaty E, Patel GB, Prickett ML, et al. Efficacy of type 2-targeted biologics in patients with asthma and bronchiectasis. Ann Allergy Asthma Immunol 2021; 126: 302–304. doi: 10.1016/j.anai.2020.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Crimi C, Campisi R, Nolasco S, et al. Mepolizumab effectiveness in patients with severe eosinophilic asthma and co-presence of bronchiectasis: a real-world retrospective pilot study. Respir Med 2021; 185: 106491. doi: 10.1016/j.rmed.2021.106491 [DOI] [PubMed] [Google Scholar]
- 118.Carpagnano GE, Scioscia G, Lacedonia D, et al. Severe uncontrolled asthma with bronchiectasis: a pilot study of an emerging phenotype that responds to mepolizumab. J Asthma Allergy 2019; 12: 83–90. doi: 10.2147/JAA.S196200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Oriano M, Gramegna A, Amati F, et al. T2-high endotype and response to biological treatments in patients with bronchiectasis. Biomedicines 2021; 9: 772. doi: 10.3390/biomedicines9070772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Martinez-Garcia MA, Posadas T, Sotgiu G, et al. Repeteability of circulating eosinophil measures and inhaled corticosteroids effect in bronchiectasis. A post hoc analysis of a randomized clinical trial. Arch Bronconeumol 2020; 56: 681–683. doi: 10.1016/j.arbr.2020.06.003 [DOI] [PubMed] [Google Scholar]
- 121.Shoemark A, Devaraj A, Meister M, et al. Elevated peripheral airway nitric oxide in bronchiectasis reflects disease severity. Respir Med 2011; 105: 885–891. doi: 10.1016/j.rmed.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 122.Aliberti S, Masefield S, Polverino E, et al. Research priorities in bronchiectasis: a consensus statement from the EMBARC Clinical Research Collaboration. Eur Respir J 2016; 48: 632–647. doi: 10.1183/13993003.01888-2015 [DOI] [PubMed] [Google Scholar]
- 123.Radovanovic D, Santus P, Blasi F, et al. A comprehensive approach to lung function in bronchiectasis. Respir Med 2018; 145: 120–129. doi: 10.1016/j.rmed.2018.10.031 [DOI] [PubMed] [Google Scholar]
- 124.Chalmers JD, Aliberti S, Filonenko A, et al. Characterization of the “frequent exacerbator phenotype” in bronchiectasis. Am J Respir Crit Care Med 2018; 197: 1410–1420. doi: 10.1164/rccm.201711-2202OC [DOI] [PubMed] [Google Scholar]
- 125.Hill AT, Haworth CS, Aliberti S, et al. Pulmonary exacerbation in adults with bronchiectasis: a consensus definition for clinical research. Eur Respir J 2017; 49: 1700051. doi: 10.1183/13993003.00051-2017 [DOI] [PubMed] [Google Scholar]
- 126.Artaraz A, Crichton ML, Finch S, et al. Development and initial validation of the bronchiectasis exacerbation and symptom tool (BEST). Respir Res 2020; 21: 18. doi: 10.1186/s12931-019-1272-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Guan WJ, Gao YH, Xu G, et al. Inflammatory responses, spirometry, and quality of life in subjects with bronchiectasis exacerbations. Respir Care 2015; 60: 1180–1189. doi: 10.4187/respcare.04004 [DOI] [PubMed] [Google Scholar]
- 128.Goss CH, Heltshe SL, West NE, et al. A randomized clinical trial of antimicrobial duration for cystic fibrosis pulmonary exacerbation treatment. Am J Respir Crit Care Med 2021; 204: 1295–1305. doi: 10.1164/rccm.202102-0461OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bedi P, Cartlidge MK, Zhang Y, et al. Feasibility of shortening intravenous antibiotic therapy for bronchiectasis based on bacterial load: a proof-of-concept randomised controlled trial. Eur Respir J 2021; 58: 2004388. doi: 10.1183/13993003.04388-2020 [DOI] [PubMed] [Google Scholar]
- 130.Giam YH, Shoemark A, Chalmers JD. Neutrophil dysfunction in bronchiectasis: an emerging role for immunometabolism. Eur Respir J 2021; 58: 2003157. doi: 10.1183/13993003.03157-2020 [DOI] [PubMed] [Google Scholar]
- 131.Palmer R, Maenpaa J, Jauhiainen A, et al. Dipeptidyl peptidase 1 inhibitor AZD7986 induces a sustained, exposure-dependent reduction in neutrophil elastase activity in healthy subjects. Clin Pharmacol Ther 2018; 104: 1155–1164. doi: 10.1002/cpt.1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chalmers JD, Gupta A, Chotirmall SH, et al. A phase 2 randomised study to establish efficacy, safety and dosing of a novel oral cathepsin C inhibitor, BI 1291583, in adults with bronchiectasis: Airleaf. ERJ Open Res 2023; 9: 00633-2022. doi: 10.1183/23120541.00633-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Daley CL, Iaccarino JM, Lange C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis 2020; 71: e1–e36. doi: 10.1093/cid/ciaa241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 2007; 175: 367–416. doi: 10.1164/rccm.200604-571ST [DOI] [PubMed] [Google Scholar]
- 135.Agarwal R, Sehgal IS, Muthu V, et al. Revised ISHAM-ABPA working group clinical practice guidelines for diagnosing, classifying and treating allergic bronchopulmonary aspergillosis/mycoses. Eur Respir J 2024; 63: 2400061. doi: 10.1183/13993003.00061-2024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Pulmonology Portuguese Society Bronchiectasis Study Group . Recommendations for aetiological diagnosis of bronchiectasis. Rev Port Pneumol 2016; 22: 222–235. doi: 10.1016/j.rppnen.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 137.De Soyza A, Chalmers JD, Dimakou K, et al. Impact of inflammatory bowel disease in bronchiectasis (IBD-BR) data from the EMBARC registry. Eur Respir J 2018; 52: Suppl. 62, PA2678. doi: 10.1183/13993003.congress-2018.PA2678 [DOI] [Google Scholar]
- 138.Shoemark A, Polverino E, Blasi F, et al. Characteristics and outcomes of adults with primary ciliary dyskinesia (PCD): an EMBARC/BEAT-PCD analysis. Eur Respir J 2021; 58: Suppl. 65, PA2062. doi: 10.1183/13993003.congress-2021.PA2062 [DOI] [Google Scholar]
- 139.Sobala R, De Soyza A. Bronchiectasis and chronic obstructive pulmonary disease overlap syndrome. Clin Chest Med 2022; 43: 61–70. doi: 10.1016/j.ccm.2021.11.005 [DOI] [PubMed] [Google Scholar]
- 140.Mao B, Yang JW, Lu HW, et al. Asthma and bronchiectasis exacerbation. Eur Respir J 2016; 47: 1680–1686. doi: 10.1183/13993003.01862-2015 [DOI] [PubMed] [Google Scholar]
- 141.Handley E, Nicolson CH, Hew M, et al. Prevalence and clinical implications of chronic rhinosinusitis in people with bronchiectasis: a systematic review. J Allergy Clin Immunol Pract 2019; 7: 2004–2012. doi: 10.1016/j.jaip.2019.02.026 [DOI] [PubMed] [Google Scholar]
- 142.Mandal P, Morice AH, Chalmers JD, et al. Symptoms of airway reflux predict exacerbations and quality of life in bronchiectasis. Respir Med 2013; 107: 1008–1013. doi: 10.1016/j.rmed.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 143.Yoon JH, Kim SH, Ryu J, et al. Gastro-oesophageal reflux disease increases healthcare use and medical costs in patients with bronchiectasis: a Korean nationwide population-based study. Therap Adv Gastroenterol 2021; 14: 17562848211062801. doi: 10.1177/17562848211062801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lee JH, Lee WY, Yong SJ, et al. Prevalence of depression and its associated factors in bronchiectasis: findings from KMBARC registry. BMC Pulm Med 2021; 21: 306. doi: 10.1186/s12890-021-01675-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Olveira C, Olveira G, Gaspar I, et al. Depression and anxiety symptoms in bronchiectasis: associations with health-related quality of life. Qual Life Res 2013; 22: 597–605. doi: 10.1007/s11136-012-0188-5 [DOI] [PubMed] [Google Scholar]
- 146.Navaratnam V, Millett ER, Hurst JR, et al. Bronchiectasis and the risk of cardiovascular disease: a population-based study. Thorax 2017; 72: 161–166. doi: 10.1136/thoraxjnl-2015-208188 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-00518-2024.Shareable (375.8KB, pdf)