There is no precise definition of dyspepsia. It can be defined pragmatically as upper abdominal or retrosternal pain, with or without other symptoms thought to be arising from the upper gastrointestinal tract—which is the approach that has been generally adopted by epidemiological studies.
It has been suggested that dyspeptic symptoms can be categorised as ulcer-like, reflux-like, and dysmotility-like as a guide to the underlying cause. These groups, however, overlap considerably, with mixed patterns being common. Symptom patterns are not strong predictors of underlying disease. Recently it has been proposed that if heartburn or acid regurgitation are the dominant symptoms then these are sufficiently accurate predictors of gastro-oesophageal reflux to make a safe and accurate diagnosis (see next article). Fewer than a fifth of sufferers have this symptom pattern, and the predictive accuracy needs confirmation.
Prevalence
Dyspepsia is common: in a recent UK survey 40% of adults reported having had one or more dyspeptic symptoms in the previous year, and about a half described these as being moderate to severe. Of this group, more than half were taking drugs for dyspepsia (40% of which were prescribed) and 22% had seen their general practitioner about dyspepsia in the previous year. Thus, 9% of all those interviewed reported consulting their doctor about dyspepsia in the previous year.
“Alarm” symptoms in patients with dyspepsia suggesting possibility of malignant disease
Anaemia
Loss of weight
Anorexia
Recent onset of progressive symptoms (<3 months)
Melaena or haematemesis
Dysphagia
Most dyspeptic patients have no clinically significant abnormalities on investigation. Up to 20% may have endoscopic reflux oesophagitis, and 15-20% may have peptic ulcer disease, including duodenitis. A declining proportion, currently around 2%, will have a gastric or oesophageal cancer, with other “alarm” symptoms such as dysphagia or weight loss usually being present.
Patients consulting with upper gastrointestinal disorders in general practitioner morbidity surveys
| No of patients (per 10 000/year) |
|||
|---|---|---|---|
| Condition (ICD code) | 1981-2 | 1991-2 | Change |
| Non-ulcer dyspepsia: | 178 | 330 | 85% |
| Oesophagus (530) | 24 | 103 | |
| Gastritis or duodenitis (535) | 27 | 74 | |
| Other disorders (536) | 127 | 153 | |
| Peptic ulcer (531-534) | 57 | 52 | −9% |
| All disorders | 720 | 866 | 20% |
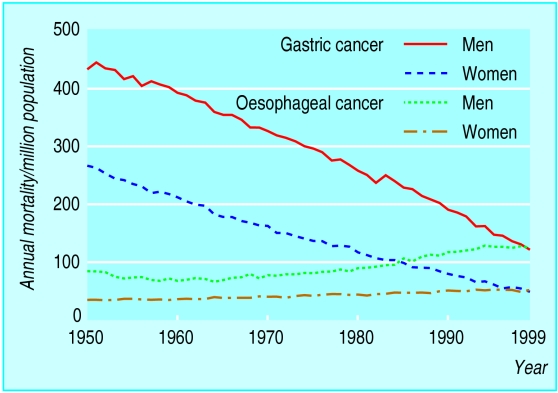
Whether dyspepsia is becoming more common is unclear, but general practice consultations for non-ulcer dyspepsia have been increasing. In contrast, morbidity and mortality resulting from peptic ulcer disease is declining; mortality from oesophageal cancer has now overtaken mortality from gastric cancer, which has declined steeply over the past 50 years.
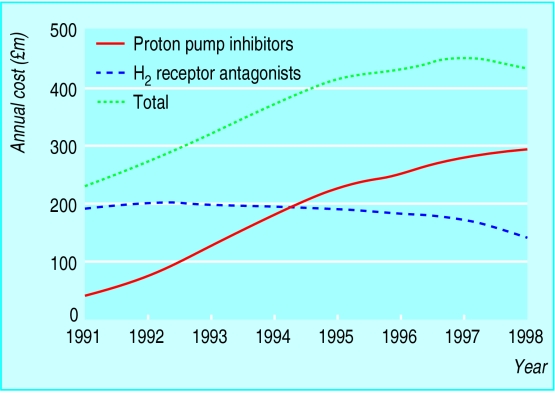
Cost to the NHS
The management of these patients has a considerable impact on the NHS. At any one time up to 4% of the population are thought to be taking prescribed drugs for dyspepsia. In the past few years the costs of these prescriptions have risen dramatically and now account for over 10% of drug expenditure in primary care (471m in 1999 in England and Wales), although this may now have peaked.
Investigation is also costly. The number of upper gastroscopies performed each year in the United Kingdom has been steadily increasing and was thought to be over 450 000 in 1996, a little over one endoscopy for every 100 adults in England and Wales. Endoscopy has been estimated to cost £80-£450 per procedure depending on the hospital (NHS Reference costs 1998). In addition, assessment of dyspepsia and abdominal pain is one of the commonest reasons for referral to hospital.
To these costs one might also add the costs of managing complications such as gastrointestinal bleeding from peptic ulceration and oesophagitis.
Managing dyspepsia in primary care
Why do patients consult with dyspepsia?
According to the health belief model, the decision to consult a general practitioner is determined by a person's perception of the likelihood of serious disease and the potential for cure.
Why do patients consult with dyspepsia?
Major factors
Patient's perception of the problem
Patient's peers' perception of the problem
Availability of medical care
Availability of non-medical treatments
Cost to the patient
Minor factors
Interference with work, personal life, or physical functioning
Medicalisation of symptoms
Five factors are thought to influence whether a patient consults a doctor: how the patient perceives the problem, how the patient's peers perceive the problem, the availability of medical care, the availability of non-medical treatments, and whether the patient can afford treatment. Other triggers—such as an interpersonal crisis; interference with personal relationships, work, or physical functioning; sanctioning; and setting of external time criteria—are required to force a medicalisation of the symptoms before they are perceived as illness.
Causes of dyspepsia
Findings from endoscopy in 2659 patients aged >40 years consulting their doctor for dyspepsia for the first time:
Hiatus hernia or oesophagitis 19%
Peptic ulcer: Gastric 6% Duodenal 10%
Duodenitis 4%
Gastric or oesophageal cancer 3%
Normal (including gastritis only) 59%
Qualitative studies have shown that patients with dyspepsia are concerned with finding causal relations between life events and their symptoms. “Stomach disease” is most commonly linked to stress and worry. No difference has been found between people who consult a doctor about their dyspepsia and those who do not in the frequency or subjective severity of their symptoms, but those who do consult have significantly more life events. People consulting with dyspepsia are more likely to believe that their symptoms are due to serious illness, heart disease, ulcers, or cancer in particular. The challenge for general practitioners is to maximise detection of serious and treatable conditions while minimising the cost and adverse effects of investigation.
Strategies for managing dyspepsia in primary care
Initial empiric treatment with antacids or anti-secretory drugs
A period of empiric treatment with antacids or H2 receptor antagonists has been the traditional strategy for managing patients with dyspepsia first consulting their doctor. This strategy recognises that most patients' symptoms are episodic and remit spontaneously and that the risk of peptic ulcer bleeding or perforation is extremely low. It also assumes that early diagnosis in the rare patient with malignant disease and no alarm symptoms has little effect on outcome.
However, this strategy has several major limitations. It takes little account of the fact that many dyspeptic people consult their doctor only after months, if not years, of symptoms and self medication. It also fails to meet the expectations of patients who are increasingly informed and often expect referral for investigation or prescription of more powerful drugs. It offers little reassurance to those patients who believe that their symptoms are due to more serious disease. In controlled trials empiric treatment results in the lowest scores for patient satisfaction.
Investigate all patients by early endoscopy
It has been argued that, as most dyspeptic patients end up having some investigation anyway, earlier investigation may prove more cost effective. However, cost effectiveness modelling has shown that if the incidence of peptic ulcer disease in dyspeptic patients is less than 10%, it would take more than five years for the costs of investigation to be recouped in savings from fewer prescriptions. Results of several large trials based in primary care of the cost effectiveness of this approach are expected soon.
A recent Cochrane review has shown that initial endoscopy may be associated with a 15% relative reduction in symptoms compared with empiric acid suppression. A primary care trial in patients aged over 50 years has shown that this small reduction in symptoms might be cost effective if the unit cost of endoscopy could be kept to £100.
Only investigate a proportion of dyspeptic patients
The rationale behind this proposal is to increase the diagnostic yield of endoscopy without missing any serious causes in those not investigated. Criteria involving age (related to gastric cancer risk), consumption of non-steroidal anti-inflammatory drugs, and “alarm” symptoms have been proposed.
More recently, non-invasive tests for Helicobacter pylori have been suggested: lack of H pylori infection is a good predictor of the absence of peptic ulcer or gastric cancer. A retrospective study examined the effect of screening for H pylori by serology before endoscopy in patients aged under 45 and not taking non-steroidal anti-inflammatory drugs. It found that positive serology was highly predictive of endoscopic abnormalities, and endoscopy workload would have been reduced by 23% if only the patients seropositive for H pylori had been investigated. However, recent prospective trials have suggested that in general practices near patient serology tests may lack sufficient accuracy and that the strategy might even increase endoscopic workload.
Test for H pylori and treat
Up to 15% (and higher in some areas such as Glasgow) of dyspeptic patients infected with H pylori may have peptic ulcer disease, so there is an argument for treating such patients, without first proving the presence of an ulcer by endoscopy. This may have the added advantage of preventing peptic ulcers or gastric cancer that might develop in the future as well as treating current disease.
Clinical summary
Patients aged under 55 presenting with dyspepsia for the first time should be managed initially with a short course of antacid or antisecretory drugs (based on consensus guidelines)
Patients still symptomatic should be tested for H pylori infection (by laboratory serum enzyme linked immunosorbent assay (ELISA), stool antigen test, or 13C-urea breath test) and, if positive, investigated by endoscopy or given eradication treatment
Treatment for H pylori infection without testing is not recommended as most patients treated will not be infected (cohort study)
Patients with gastric and duodenal ulceration, newly diagnosed or still requiring treatment, should receive H pylori eradication treatment (meta-analysis of randomised trials)
Unless a major complication has occurred (such as bleeding), cure should be taken as relief of symptoms without proceeding to a breath test (prospective cohort study)
Patients with persistent symptoms should have a 13C-urea breath test to confirm H pylori eradication (consensus guidelines)
Treatment of asymptomatic H pylori infection is not recommended
However, the successful eradication of H pylori requires combination therapy and carries a risk of increasing bacterial resistance. As the prevalence of H pylori infection in the developed world is steadily declining, treating patients without testing for infection is unlikely to be cost effective.
In contrast, decision analysis models suggest that testing for H pylori and treating those who test positive (“test and treat”) is likely to be one of the most cost effective approaches in primary care. Three randomised controlled trials have shown that testing for and treating H pylori was as effective as endoscopy based management in controlling symptoms in patients referred to secondary care, but cost less because many fewer endoscopies were performed. However, the long term effects of eradicating H pylori in patients without peptic ulcer disease are uncertain, and the effects on resource use compared with empiric acid suppression are unknown.
Role of hospitals
The appropriate management of dyspeptic patients in primary care relies on a combination of making a diagnosis to determine the most effective treatment and reducing the uncertainty experienced by both doctors and patients. In terms of potentially effective treatment two groups of patients should be actively sought— those with peptic ulcer disease, induced either by H pylori infection or non-steroidal anti-inflammatory drugs, and those with early gastric cancer.
Endoscopy is not the only investigation that may be used to support management: tests for H pylori infection, particularly the highly accurate 13C-urea breath tests and stool antigen tests, may be increasingly important in primary care. Specialists have an important role in coordinating local endoscopy services and in treating patients with difficult to manage dyspepsia.
Figure.
Dyspepsia is not new and has been known throughout history (Indigestion by Cruickshank (1792-1872))
Figure.
Mortality from gastric and oesophageal cancer in England and Wales 1950-99
Figure.
Cost of prescriptions for ulcer healing drugs in England and Wales
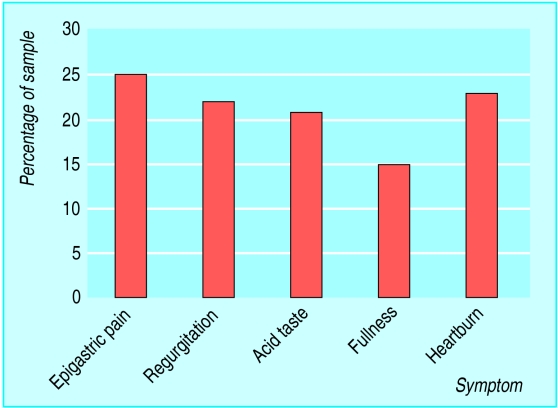
Figure.
Symptoms of dyspepsia reported by UK adults over the previous year
Figure.

Transmission electron micrograph of Helicobacter pylori
Acknowledgments
Indigestion is reproduced with permission of the Wellcome Library. The table of patients consulting with upper gastrointestinal disorders is derived from the Office of National Statistics Morbidity Statistics from General Practice—Fourth national study 1991-92. The graph of costs of drug prescriptions is based on data from the Prescription Pricing Authority. The table of causes of dyspepsia is adapted from Hallisey et al, BMJ 1990;301:513-5. The graph of prevalence of symptoms of dyspepsia is adapted from Penston and Pounder, Aliment Pharmacol Ther 1996;10:83-9. The electron micrograph of H pylori is reproduced with permission of Dr Linda Stannard and Science Photo Library.
Footnotes
Richard Logan is professor of clinical epidemiology, University Hospital, Nottingham. Brendan Delaney is reader in primary care and general practice, University of Birmingham, Birmingham.
The ABC of the upper gastrointestinal tract is edited by Robert Logan, senior lecturer in the division of gastroenterology, University Hospital, Nottingham, Adam Harris, consultant physician and gastroenterologist, Kent and Sussex Hospital, Tunbridge Wells, J J Misiewicz, honorary consultant physician and honorary joint director of the department of gastroenterology and nutrition, Central Middlesex Hospital, London, and J H Baron, honorary professorial lecturer at Mount Sinai School of Medicine, New York, USA, and former consultant gastroenterologist, St Mary's Hospital, London. The series will be published as a book in Spring 2002.